Found this page useful?
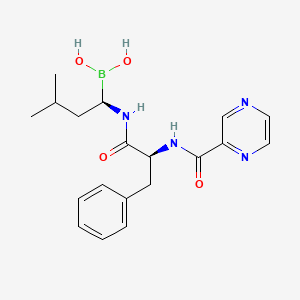
Bortezomib
 Web Resources: Bortezomib
Web Resources: Bortezomib Latest Research Publications
Latest Research PublicationsWeb Resources: Bortezomib (6 links)
MedlinePlus.gov
NHS Evidence
 Bortezomib - Substance Summary
Bortezomib - Substance Summary
PubChem
Macmillan Cancer Support
Cancer Research UK
Irish Cancer Society
Latest Research Publications
Jimenez-Zepeda VH, Duggan P, Neri P, et al.
Bortezomib-containing regimens (BCR) for the treatment of non-transplant eligible multiple myeloma.
Ann Hematol. 2017; 96(3):431-439 [PubMed] Related Publications
Bortezomib-containing regimens (BCR) for the treatment of non-transplant eligible multiple myeloma.
Ann Hematol. 2017; 96(3):431-439 [PubMed] Related Publications
In multiple myeloma (MM) patients ineligible for transplant, the selection of up-front therapy needs to balance efficacy and toxicity. Recently, regimens with bortezomib, a proteasome inhibitor with anti-myeloma effects, have been reported. We aimed to evaluate the impact of different bortezomib-containing regimens (BCR) for the treatment of transplant-ineligible MM. All- consecutive patients treated with BCR at our institution from 01/05 to 02/16 were evaluated. With a median of 6 cycles, an overall response rate of 95.2, 80.9, and 76.3% was observed for patients treated with cyclophosphamide-bortezomib-dexamethasone (CyBorD), bortezomib-melphalan-prednisone (VMP), and bortezomib-dexamethasone (VD), respectively (p = 0.03). The median overall survival was similar between the three different BCR, but a trend for better progression-free survival was noted in favor of CyBorD. BCR are efficacious in the treatment of transplant-ineligible MM. Patients receiving continuous therapy (CT) exhibited better outcomes, suggesting that strategies to prevent toxicity and increase the cumulative dose are warranted.
Zuo W, Zhu X, Yang J, et al.
Bortezomib combined with lenalidomide as the first-line treatment for the rare synchronous occurrence of multiple myeloma and pulmonary adenocarcinoma: A case report.
Medicine (Baltimore). 2017; 96(1):e5787 [PubMed] Free Access to Full Article Related Publications
Bortezomib combined with lenalidomide as the first-line treatment for the rare synchronous occurrence of multiple myeloma and pulmonary adenocarcinoma: A case report.
Medicine (Baltimore). 2017; 96(1):e5787 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Simultaneous multiple myeloma (MM) and pulmonary adenocarcinoma is a rare occurrence, and thus, treatment is a challenge. This study reports on 1 such case of MM with concurrent lung cancer, where an accurate diagnosis was made and the patient underwent treatment for both cancers.
CASE SUMMARY: A 68-year-old man presented with 2 months of progressive lower back pain. Visualization with magnetic resonance imaging (MRI) revealed multiple collapsed vertebrae from T12 to S3, as well as an altered signal intensity at the T3 vertebra. The patient was diagnosed with MM upon examination. A chest computed tomography (CT) scan revealed a round mass in the left lower lobe of the lungs, and a CT-guided needle biopsy uncovered a moderately differentiated adenocarcinoma. There were no additional notable findings in the left lung using positron emission tomography computed tomography (PET-CT). Therefore, a diagnosis of MM with pulmonary adenocarcinoma was made. Surgery was performed to excise the lung cancer. Bortezomib was used as first-line induction therapy against both tumors and lenalidomide was used for maintenance. The patient went into complete remission. Using this combined chemotherapy, the patient has survived for over 3 years since a diagnosis was made despite relapsing twice after the first year.
CONCLUSION: This report clearly delineates the diagnosis and treatment of a rare case of synchronous MM and pulmonary adenocarcinoma, as well as depicts a potentially positive outcome for the patient. It also overviews some diagnostic and therapeutic implications for clinicians.
CASE SUMMARY: A 68-year-old man presented with 2 months of progressive lower back pain. Visualization with magnetic resonance imaging (MRI) revealed multiple collapsed vertebrae from T12 to S3, as well as an altered signal intensity at the T3 vertebra. The patient was diagnosed with MM upon examination. A chest computed tomography (CT) scan revealed a round mass in the left lower lobe of the lungs, and a CT-guided needle biopsy uncovered a moderately differentiated adenocarcinoma. There were no additional notable findings in the left lung using positron emission tomography computed tomography (PET-CT). Therefore, a diagnosis of MM with pulmonary adenocarcinoma was made. Surgery was performed to excise the lung cancer. Bortezomib was used as first-line induction therapy against both tumors and lenalidomide was used for maintenance. The patient went into complete remission. Using this combined chemotherapy, the patient has survived for over 3 years since a diagnosis was made despite relapsing twice after the first year.
CONCLUSION: This report clearly delineates the diagnosis and treatment of a rare case of synchronous MM and pulmonary adenocarcinoma, as well as depicts a potentially positive outcome for the patient. It also overviews some diagnostic and therapeutic implications for clinicians.
Liu J, Li J, Chen M, Kuang L
Bortezomib followed by autologous stem cell transplantation in a patient with rheumatoid arthritis: A case report and review of the literature.
Medicine (Baltimore). 2016; 95(52):e5760 [PubMed] Free Access to Full Article Related Publications
Bortezomib followed by autologous stem cell transplantation in a patient with rheumatoid arthritis: A case report and review of the literature.
Medicine (Baltimore). 2016; 95(52):e5760 [PubMed] Free Access to Full Article Related Publications
RATIONALE AND PATIENTS CONCERNS: Despite the introduction of varied disease-modifying antirheumatic drugs and biological agents, a substantial proportion of patients remain untreatable. We report a 56-year-old Chinese female patient with a case of refractory rheumatoid arthritis (RA) complicated with multiple myeloma (MM) who was treated successfully with Bortezomib followed by autologous stem cell transplantation (ASCT).
DIAGNOSIS AND INTERVENTIONS: We report a 56-year-old Chinese female patient who was diagnosed as RA complicating with MM. She received 4 cycles of Bortezomib-based chemotherapy followed by ASCT. The response of her RA and MM were evaluated after every cycle of Bortezomib-based chemotherapy.
INTERVENTIONS AND OUTCOMES: After the first Bortezomib-based chemotherapy cycle, this patient's symptoms were significantly alleviated and thereafter the RA activity continued to improve. After the 4 courses of Bortezomib-based chemotherapy, the C-reactive protein was <0.5 mg/dL and the disease activity score 28-erythrocyte sedimentation rate was 2.0. No hematological or nonhematological side effects were observed during the treatment of Bortezomib.
LESSONS: Bortezomib might be a new safe and promising drug for refractory RA patients.
DIAGNOSIS AND INTERVENTIONS: We report a 56-year-old Chinese female patient who was diagnosed as RA complicating with MM. She received 4 cycles of Bortezomib-based chemotherapy followed by ASCT. The response of her RA and MM were evaluated after every cycle of Bortezomib-based chemotherapy.
INTERVENTIONS AND OUTCOMES: After the first Bortezomib-based chemotherapy cycle, this patient's symptoms were significantly alleviated and thereafter the RA activity continued to improve. After the 4 courses of Bortezomib-based chemotherapy, the C-reactive protein was <0.5 mg/dL and the disease activity score 28-erythrocyte sedimentation rate was 2.0. No hematological or nonhematological side effects were observed during the treatment of Bortezomib.
LESSONS: Bortezomib might be a new safe and promising drug for refractory RA patients.
Benyamini N, Avivi I, Dann EJ, et al.
Comparison of engraftment following different stem cell mobilization modalities in patients with multiple myeloma treated with a uniform induction regimen containing bortezomib, cyclophosphamide and dexamethasone.
Ann Hematol. 2017; 96(3):461-467 [PubMed] Related Publications
Comparison of engraftment following different stem cell mobilization modalities in patients with multiple myeloma treated with a uniform induction regimen containing bortezomib, cyclophosphamide and dexamethasone.
Ann Hematol. 2017; 96(3):461-467 [PubMed] Related Publications
Bortezomib-based induction followed by autologous stem cell transplantation is a common treatment for multiple myeloma (MM). Stem cell (SC) mobilization with granulocyte-colony stimulating factor (G-CSF) alone has become an alternative to G-CSF combined with chemotherapeutic agents. This study aimed to compare the efficacy of the two mobilization modalities following induction with a uniform regimen containing bortezomib, cyclophosphamide and dexamethasone (VCD). We retrospectively evaluated results of SC mobilization using either G-CSF alone or combined with high-dose cyclophosphamide (HD-CY) in MM patients after VCD induction. The primary endpoints of the study were engraftment and mobilization-associated toxicity. Parameters of stem cell collection, transplantation and engraftment were assessed. Data of 92 patients were analyzed [56 (61%) mobilized with HD-CY + G-CSF and 36 (39%) with G-CSF only]. HD-CY + G-CSF provided a higher number of CD34 + cells (15.9 vs 8.1 × 10(6)/kg, p = 0.001) with fewer apheresis sessions. However, while no adverse events were observed in patients receiving G-CSF alone, nine patients (16%) receiving HD-CY + G-CSF developed neutropenic fever requiring hospitalization. Although a greater number of cells was transplanted following mobilization with HD-CY + G-CSF, neutrophil and platelet engraftment and duration of transplant-related hospitalization were similar in both cohorts. G-CSF alone provided a sufficient SC amount, without exposing patients to additional toxicity. While HD-CY + G-CSF resulted in a superior SC yield in MM patients induced with VCD, this advantage should be balanced against adverse effects of this mobilization regimen.
Berenson A, Vardanyan S, David M, et al.
Outcomes of multiple myeloma patients receiving bortezomib, lenalidomide, and carfilzomib.
Ann Hematol. 2017; 96(3):449-459 [PubMed] Related Publications
Outcomes of multiple myeloma patients receiving bortezomib, lenalidomide, and carfilzomib.
Ann Hematol. 2017; 96(3):449-459 [PubMed] Related Publications
New classes of drugs including the proteasome inhibitors (PI) bortezomib and, more recently, carfilzomib and the immunomodulatory agent lenalidomide have shown improved outcomes for multiple myeloma (MM) patients during the past decade. However, most of the studies reporting outcomes for patients receiving these drugs have relied on older data sets derived from large institutions that included patients not receiving their treatment at those facilities and represented only those eligible for clinical trials or were from sites where treatment options were limited. We have analyzed data from 258 MM patients who have received treatment with at least one of three agents: bortezomib, carfilzomib, and lenalidomide in a single clinic specializing in MM with respect to their responses and other outcomes to treatment regimens including these agents. Response rates were similar between these three drugs when used for the first time and again during subsequent treatment regimens. As expected, the clinical benefit rates (CBRs) were better for patients receiving their first treatment when compared to their use in subsequent treatment regimens. The CBRs were similar during their 2nd, 3rd, and 4th treatments containing these agents. Many patients refractory to these agents showed responses to regimens containing these same drugs when used in different combinations. In addition, patients refractory to one PI often responded to the other PI. The results of this study demonstrate that novel agents can be used repeatedly in novel combinations with significant clinical benefit for patients with MM.
Oiwa K, Morita M, Kishi S, et al.
High Risk of Tumor Lysis Syndrome in Symptomatic Patients with Multiple Myeloma with Renal Dysfunction Treated with Bortezomib.
Anticancer Res. 2016; 36(12):6655-6662 [PubMed] Related Publications
High Risk of Tumor Lysis Syndrome in Symptomatic Patients with Multiple Myeloma with Renal Dysfunction Treated with Bortezomib.
Anticancer Res. 2016; 36(12):6655-6662 [PubMed] Related Publications
BACKGROUND/AIM: Tumor lysis syndrome (TLS) is a life-threatening complication associated with cancer chemotherapy. We retrospectively evaluated the risk of developing TLS in patients with symptomatic multiple myeloma undergoing chemotherapy.
PATIENTS AND METHODS: Sixty-four patients (median age=71 years, range=48-87 years, 35 males/29 females) who were treated at our Institution between April 2006 and December 2015 were evaluated.
RESULTS: A total of 124 chemotherapy courses were administered, of which 63 courses were bortezomib-based regimens and 34 courses were immunomodulatory drug (IMiD)-based regimens. TLS occurred in 13 (10.5%) out of 124 chemotherapy courses with five (4.0%) cases of laboratory TLS and eight (6.5%) cases of clinical TLS. The incidences of TLS were 17.5% for bortezomib-containing regimens and 3.2% for non-bortezomib-based regimens. No TLS occurred in the patients treated with IMiD-containing regimens. TLS occurred more frequently in the patients with elevated uric acid, creatinine, or beta-2-microglobulin levels at baseline. The patients with disease classified as advanced International Staging System also developed TLS more frequently. All the patients who developed clinical TLS received bortezomib-containing regimens (8/63, 12.7%). Among them, patients with elevated values of uric acid or creatinine developed clinical TLS more often than those without such elevation. The incidence of clinical TLS was 33.3% if the patients had renal dysfunction at baseline and were subsequently treated with bortezomib-based regimens (8/24 cases).
CONCLUSION: Patients with renal dysfunction or a high uric acid level receiving bortezomib-based chemotherapy have a high risk of developing TLS.
PATIENTS AND METHODS: Sixty-four patients (median age=71 years, range=48-87 years, 35 males/29 females) who were treated at our Institution between April 2006 and December 2015 were evaluated.
RESULTS: A total of 124 chemotherapy courses were administered, of which 63 courses were bortezomib-based regimens and 34 courses were immunomodulatory drug (IMiD)-based regimens. TLS occurred in 13 (10.5%) out of 124 chemotherapy courses with five (4.0%) cases of laboratory TLS and eight (6.5%) cases of clinical TLS. The incidences of TLS were 17.5% for bortezomib-containing regimens and 3.2% for non-bortezomib-based regimens. No TLS occurred in the patients treated with IMiD-containing regimens. TLS occurred more frequently in the patients with elevated uric acid, creatinine, or beta-2-microglobulin levels at baseline. The patients with disease classified as advanced International Staging System also developed TLS more frequently. All the patients who developed clinical TLS received bortezomib-containing regimens (8/63, 12.7%). Among them, patients with elevated values of uric acid or creatinine developed clinical TLS more often than those without such elevation. The incidence of clinical TLS was 33.3% if the patients had renal dysfunction at baseline and were subsequently treated with bortezomib-based regimens (8/24 cases).
CONCLUSION: Patients with renal dysfunction or a high uric acid level receiving bortezomib-based chemotherapy have a high risk of developing TLS.
Berenson A, Vardanyan S, David M, et al.
Improved clinical outcomes for multiple myeloma patients treated at a single specialty clinic.
Ann Hematol. 2017; 96(3):441-448 [PubMed] Related Publications
Improved clinical outcomes for multiple myeloma patients treated at a single specialty clinic.
Ann Hematol. 2017; 96(3):441-448 [PubMed] Related Publications
Despite recent advances made in its treatment, multiple myeloma (MM) remains an incurable B cell malignancy. Thus, the objective for treating these patients is to prolong overall survival (OS) and preserve patients' quality of life. We have analyzed data from 264 consecutive MM patients who had their initial visit between July 1, 2004 and December 1, 2014 and have received treatment in a single clinic specializing in MM. We determined their progression-free survival (PFS, OS, and 5-year OS). The PFS for frontline (n = 165 treatments), salvage (n = 980), and all treatments (n = 1145) were 13.9, 4.6, and 5.5 months, respectively. The median OS of all patients was 98 months with a 5-year survival of 74%. The results of this study show a marked improvement in OS for unselected MM patients compared with historical data. There were no significant differences in OS between patients with different International Staging System (ISS) stages. Younger patients (<65 years old) showed a longer OS. The results of this study should help physicians predict outcomes for MM patients and be encouraging for patients with this B cell malignancy.
Xia C, Ribeiro M, Scott S, Lonial S
Daratumumab: monoclonal antibody therapy to treat multiple myeloma.
Drugs Today (Barc). 2016; 52(10):551-560 [PubMed] Related Publications
Daratumumab: monoclonal antibody therapy to treat multiple myeloma.
Drugs Today (Barc). 2016; 52(10):551-560 [PubMed] Related Publications
Daratumumab (Darzalex[TM]) is a human monoclonal antibody (MAb) that targets CD38; a surface protein highly expressed across multiple myeloma (MM) cells. Preclinical studies have shown daratumumab induces MM cell death through several mechanisms, including complement-dependent cytotoxicity (CDC) antibody-dependent cell-mediated cytotoxicity (ADCC), antibody-dependent cellular phagocytosis (ADCP), apoptosis upon secondary crosslinking and immunomodulatory effects via a decrease in immune suppressive cells. Daratumumab has a favorable toxicity profile and encouraging clinical activity as a single agent and in combination with lenalidomide in heavily pretreated, relapsed patients in whom other novel agents (such as bortezomib, thalidomide and lenalidomide) and stem cell transplant have already failed. Given the encouraging efficacy and acceptable safety profile, daratumumab has emerged as a novel treatment option for MM both as a monotherapy and in combination with conventional and novel anti-MM agents. This review will focus on preclinical pharmacology, pharmacokinetics, safety and clinical development of daratumumab in MM.
Offidani M, Corvatta L, Bringhen S, et al.
Salvage therapy in first relapse: a retrospective study in a large patient population with multiple myeloma.
Eur J Haematol. 2017; 98(3):289-295 [PubMed] Related Publications
Salvage therapy in first relapse: a retrospective study in a large patient population with multiple myeloma.
Eur J Haematol. 2017; 98(3):289-295 [PubMed] Related Publications
OBJECTIVE: There is no strong evidence to guide therapeutic approach to multiple myeloma (MM) patients who experience first relapse. The treatment choice can be difficult since currently all patients are exposed to novel agents as thalidomide, bortezomib and lenalidomide.
METHODS: In this retrospective analysis, we evaluated the best therapeutic sequence, the role of retreatment, and the most beneficial cutoff of first remission in order to choose retreatment, analyzing 476 patients relapsed after first-line therapy.
RESULTS: Bortezomib-based regimens upfront followed by lenalidomide-based regimens at first relapse resulted in significantly better second progression-free survival (2ndPFS), PFS2, and overall survival (OS) compared to the opposite sequence. Changing therapy resulted in significantly better 2ndPFS in the whole population, whereas PFS2 was significantly longer only in patients who underwent maintenance therapy. Moreover, until PFS1 was shorter than 27 months, changing therapy at first relapse significantly extended 2ndPFS and PFS2 compared to retreatment, whereas similar outcomes were observed between the two strategies, when PFS1 was longer than 27 months.
CONCLUSION: Lacking randomized trials, our study could help to choose the most appropriate therapy algorithm in patients with MM.
METHODS: In this retrospective analysis, we evaluated the best therapeutic sequence, the role of retreatment, and the most beneficial cutoff of first remission in order to choose retreatment, analyzing 476 patients relapsed after first-line therapy.
RESULTS: Bortezomib-based regimens upfront followed by lenalidomide-based regimens at first relapse resulted in significantly better second progression-free survival (2ndPFS), PFS2, and overall survival (OS) compared to the opposite sequence. Changing therapy resulted in significantly better 2ndPFS in the whole population, whereas PFS2 was significantly longer only in patients who underwent maintenance therapy. Moreover, until PFS1 was shorter than 27 months, changing therapy at first relapse significantly extended 2ndPFS and PFS2 compared to retreatment, whereas similar outcomes were observed between the two strategies, when PFS1 was longer than 27 months.
CONCLUSION: Lacking randomized trials, our study could help to choose the most appropriate therapy algorithm in patients with MM.
Zhu W, Chen W
Bortezomib-based treatment for multiple myeloma patients with renal impairment: A systematic review and meta-analysis of observational studies.
Medicine (Baltimore). 2016; 95(46):e5202 [PubMed] Free Access to Full Article Related Publications
Bortezomib-based treatment for multiple myeloma patients with renal impairment: A systematic review and meta-analysis of observational studies.
Medicine (Baltimore). 2016; 95(46):e5202 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Renal insufficiency is a common and severe complication of patients with multiple myeloma. The aim of this study was to evaluate bortezomib-based treatment for multiple myeloma patients with renal insufficiency.
METHODS: The Cochrane Library, Embase, PubMed, ISI, China National Knowledge Infrastructure, Chinese Biomedical Literature Service System, Chongqing VIP Database, and Wan Fang Data were systematically searched to identify observational studies from January 1, 2001, to December 31, 2015. Myeloma response rate and renal remission rate were pooled by using risk ratio and 95% confidence interval (CI). The Cochran Q and I statistics were used to assess heterogeneity. Sensitivity analysis was performed to test the feasibility of pooled results. Publication bias was conducted when included studies were ≥9. Furthermore, grades of evidence were performed to evaluate study quality.
RESULTS: Eleven retrospective cohort studies were included in the final analysis. The number of available studies and risk ratios (95% CI) were, respectively, 10 and 1.48 (95% CI: 1.28-1.71) for myeloma overall response, 6 and 3.69 (95% CI: 2.22-6.13) for myeloma complete response, 9 and 1.47 (95% CI: 1.28-1.69) for renal overall remission, and 8 and 1.49 (95% CI: 1.26-1.75) for renal complete remission. No significant publication bias was observed and sensitivity analysis confirmed the stability of results. The overall qualities of evidence were high for myeloma complete response and medium for the other 3 outcomes based on the Grading of Recommendations, Assessment, Development and Evaluation system.
CONCLUSION: Current evidence indicated that bortezomib-based treatment could improve myeloma overall response (especially myeloma complete response) and renal overall remission (including renal complete remission).
METHODS: The Cochrane Library, Embase, PubMed, ISI, China National Knowledge Infrastructure, Chinese Biomedical Literature Service System, Chongqing VIP Database, and Wan Fang Data were systematically searched to identify observational studies from January 1, 2001, to December 31, 2015. Myeloma response rate and renal remission rate were pooled by using risk ratio and 95% confidence interval (CI). The Cochran Q and I statistics were used to assess heterogeneity. Sensitivity analysis was performed to test the feasibility of pooled results. Publication bias was conducted when included studies were ≥9. Furthermore, grades of evidence were performed to evaluate study quality.
RESULTS: Eleven retrospective cohort studies were included in the final analysis. The number of available studies and risk ratios (95% CI) were, respectively, 10 and 1.48 (95% CI: 1.28-1.71) for myeloma overall response, 6 and 3.69 (95% CI: 2.22-6.13) for myeloma complete response, 9 and 1.47 (95% CI: 1.28-1.69) for renal overall remission, and 8 and 1.49 (95% CI: 1.26-1.75) for renal complete remission. No significant publication bias was observed and sensitivity analysis confirmed the stability of results. The overall qualities of evidence were high for myeloma complete response and medium for the other 3 outcomes based on the Grading of Recommendations, Assessment, Development and Evaluation system.
CONCLUSION: Current evidence indicated that bortezomib-based treatment could improve myeloma overall response (especially myeloma complete response) and renal overall remission (including renal complete remission).
van de Velde H, Londhe A, Ataman O, et al.
Association between complete response and outcomes in transplant-eligible myeloma patients in the era of novel agents.
Eur J Haematol. 2017; 98(3):269-279 [PubMed] Related Publications
Association between complete response and outcomes in transplant-eligible myeloma patients in the era of novel agents.
Eur J Haematol. 2017; 98(3):269-279 [PubMed] Related Publications
OBJECTIVES: Achieving complete response (CR) has been linked to improved progression-free (PFS) and overall (OS) survival in myeloma. A meta-analysis was conducted to investigate whether this holds true in the era of novel agents (bortezomib, lenalidomide, thalidomide).
METHODS: A total of 24 studies in newly diagnosed patients undergoing autologous stem cell transplantation (ASCT) that reported associations between responses and long-term outcomes (PFS/OS rates post-ASCT by response, or hazard ratios with 95% confidence intervals from Cox models) were identified and analyzed.
RESULTS: Achievement of CR vs.CONCLUSIONS: Achieving CR during first-line therapy remains important in the novel-agent era; magnitude of association between achieving CR and outcomes appears higher for CR obtained using novel vs. non-novel agents.
METHODS: A total of 24 studies in newly diagnosed patients undergoing autologous stem cell transplantation (ASCT) that reported associations between responses and long-term outcomes (PFS/OS rates post-ASCT by response, or hazard ratios with 95% confidence intervals from Cox models) were identified and analyzed.
RESULTS: Achievement of CR vs.
Schabel C, Horger M, Kum S, et al.
Simplified response monitoring criteria for multiple myeloma in patients undergoing therapy with novel agents using computed tomography.
Eur J Radiol. 2016; 85(12):2195-2199 [PubMed] Related Publications
Simplified response monitoring criteria for multiple myeloma in patients undergoing therapy with novel agents using computed tomography.
Eur J Radiol. 2016; 85(12):2195-2199 [PubMed] Related Publications
INTRODUCTION: Multiple myeloma is a malignant hematological disorder of the mature B-cell lymphocytes originating in the bone marrow. While therapy monitoring is still mainly based on laboratory biomarkers, the additional use of imaging has been advocated due to inaccuracies of serological biomarkers or in a-secretory myelomas. Non-enhanced CT and MRI have similar sensitivities for lesions in yellow marrow-rich bone marrow cavities with a favourable risk and cost-effectiveness profile of CT. Nevertheless, these methods are still limited by frequently high numbers of medullary lesions and its time consumption for proper evaluation.
OBJECTIVE: To establish simplified response criteria by correlating size and CT attenuation changes of medullary multiple myeloma lesions in the appendicular skeleton with the course of lytic bone lesions in the entire skeleton. Furthermore to evaluate these criteria with respect to established hematological myeloma-specific parameters for the prediction of treatment response to bortezomib or lenalidomide.
MATERIALS AND METHODS: Non-enhanced reduced-dose whole-body CT examinations of 78 consecutive patients (43 male, 35 female, mean age 63.69±9.2years) with stage III multiple myeloma were retrospectively re-evaluated. On per patient basis, size and mean CT attenuation of 2-4 representative lesions in the limbs were measured at baseline and at a follow-up after a mean of 8 months. Results were compared with the course of lytical bone lesions as well with that of specific hematological biomarkers. Myeloma response was assessed according to the International Myeloma Working Group (IMWG) uniform response criteria. Testing for correlation between response of medullary lesions (Respmed) and response of all myeloma manifestations including osteolyses (Resptotal) was performed using the corrected contingency coefficient (Ccorr).
RESULTS: The correlation between Respmed based on length diameter and transverse diameter and Resptotal was perfect (Ccorr=1.0; p<0.0001) whereas the correlation based on density was moderate (Ccorr=0.54; p<0.0001). The evaluation of simplified response criteria with a measurement of only 2 medullary lesions yielded the best sensitivity and specificity valued for treatment-induced changes for the length diameter evaluation with 94.4%/95.7% for prediction of progressive disease and 78.6%/93.3% for prediction of therapy response. There were no significant differences between patients treated with bortezomib and lenalidomide (p>0.05).
CONCLUSION: Measurements of size of a minimum of two medullary lesions is sufficient for response assessment and correlates very well with the course of lytic bone lesions and that of hematologic parameters.
OBJECTIVE: To establish simplified response criteria by correlating size and CT attenuation changes of medullary multiple myeloma lesions in the appendicular skeleton with the course of lytic bone lesions in the entire skeleton. Furthermore to evaluate these criteria with respect to established hematological myeloma-specific parameters for the prediction of treatment response to bortezomib or lenalidomide.
MATERIALS AND METHODS: Non-enhanced reduced-dose whole-body CT examinations of 78 consecutive patients (43 male, 35 female, mean age 63.69±9.2years) with stage III multiple myeloma were retrospectively re-evaluated. On per patient basis, size and mean CT attenuation of 2-4 representative lesions in the limbs were measured at baseline and at a follow-up after a mean of 8 months. Results were compared with the course of lytical bone lesions as well with that of specific hematological biomarkers. Myeloma response was assessed according to the International Myeloma Working Group (IMWG) uniform response criteria. Testing for correlation between response of medullary lesions (Respmed) and response of all myeloma manifestations including osteolyses (Resptotal) was performed using the corrected contingency coefficient (Ccorr).
RESULTS: The correlation between Respmed based on length diameter and transverse diameter and Resptotal was perfect (Ccorr=1.0; p<0.0001) whereas the correlation based on density was moderate (Ccorr=0.54; p<0.0001). The evaluation of simplified response criteria with a measurement of only 2 medullary lesions yielded the best sensitivity and specificity valued for treatment-induced changes for the length diameter evaluation with 94.4%/95.7% for prediction of progressive disease and 78.6%/93.3% for prediction of therapy response. There were no significant differences between patients treated with bortezomib and lenalidomide (p>0.05).
CONCLUSION: Measurements of size of a minimum of two medullary lesions is sufficient for response assessment and correlates very well with the course of lytic bone lesions and that of hematologic parameters.
Bari A, Marcheselli R, Marcheselli L, et al.
A Multicenter Phase II Study of Twice-Weekly Bortezomib plus Rituximab in Patients with Relapsed Follicular Lymphoma: Long-Term Follow-Up.
Acta Haematol. 2017; 137(1):7-14 [PubMed] Related Publications
A Multicenter Phase II Study of Twice-Weekly Bortezomib plus Rituximab in Patients with Relapsed Follicular Lymphoma: Long-Term Follow-Up.
Acta Haematol. 2017; 137(1):7-14 [PubMed] Related Publications
Single-agent bortezomib (B) has shown activity in heavily pretreated patients with relapsed/refractory indolent lymphoma. On the basis of these findings, we performed a phase II study of B combined with rituximab (R) in patients with relapsed follicular lymphoma (FL). Forty-five patients with fairly good prognostic profiles were enrolled from 2007 to 2011 and received a total of 6 cycles of the B+R combination. The endpoints were the overall response rate (ORR), progression-free survival (PFS), duration of remission (DoR), overall survival (OS), and toxicity evaluation. When considering all the enrolled patients the ORR was 64%. At 5 years, the estimated PFS, DoR, and OS were 34, 49, and 70%, respectively. After excluding the 7 R-naïve patients, the ORR was 58%, with a PFS of 19 months. The most common grade >2 toxicities were thrombocytopenia (18%), peripheral neuropathy (13%), and neutropenia (2%). Our study shows the feasibility, long-term efficacy, and excellent tolerability of the B+R combination. We are aware that our study has specific limitations, such as the small sample size consisting of patients with a relatively good prognostic profile. However, because FL patients will be treated with subsequent chemotherapy regimens, a well-tolerated and effective chemotherapy-free therapy could be considered an additional tool for long-term disease control.
Winkelmann N, Desole M, Hilgendorf I, et al.
Comparison of two dose levels of cyclophosphamide for successful stem cell mobilization in myeloma patients.
J Cancer Res Clin Oncol. 2016; 142(12):2603-2610 [PubMed] Related Publications
Comparison of two dose levels of cyclophosphamide for successful stem cell mobilization in myeloma patients.
J Cancer Res Clin Oncol. 2016; 142(12):2603-2610 [PubMed] Related Publications
INTRODUCTION: Even in the era of proteasome inhibitors and immunomodulatory drugs, the autologous stem cell transplantation after high-dose melphalan continues to represent a standard approach for myeloma patients in first-line therapy. Different mobilization chemotherapies before stem cell apheresis have been published while cyclophosphamide at a dose level of up to 4 g/m(2) has been evaluated and is commonly applied. In contrast, lower dose levels of cyclophosphamide (e.g., 1.5 g/m(2)) did not result in a sufficient collection of stem cells.
METHODS: We retrospectively analyzed the impact of "intermediate-dose" (ID-CY, 2.5 g/m(2)) versus "high-dose" (HD-CY, 4 g/m(2)) cyclophosphamide in 101 (48 vs. 53) consecutively evaluable myeloma patients (median age 59 years, range 32-72 years) who underwent stem cell mobilization after induction chemotherapy. Successful stem cell harvest was defined as a stem cell yield of at least 5 million CD34 cells per kg bodyweight. Evaluation of toxicity especially considered infectious complications and hematological toxicity in both subgroups.
RESULTS: Successful stem cell mobilization was achieved in 40 of 48 (83 %) and 44 of 53 (83 %) patients, respectively. The median time to apheresis (11 vs. 12 days) and the median CD34 content of stem cell harvest (8.3 vs. 7.6 million CD34 cells per kg bodyweight) did not differ significantly between both groups. There was a significant difference of WBC nadir in favor of the cyclophosphamide regimen with 2.5 g/m(2) (0.8 vs. 0.3 Gpt/L, p = 0.021), and neutropenic fever was more often observed in patients who received 4 g/m(2) cyclophosphamide (34 vs. 15 %, p = 0.078). Importantly, after induction chemotherapy using the VCD regimen (bortezomib, cyclophosphamide, dexamethasone), successful stem cell mobilization was achieved in 26 of 29 (90 %) patients treated with 2.5 g/m(2) and 21 of 25 (84 %) patients receiving 4 g/m(2) cyclophosphamide, respectively.
CONCLUSIONS: ID-CY is safe and highly effective for stem cell mobilization in patients with newly diagnosed myeloma and associated with a reduced toxicity compared to HD-CY.
METHODS: We retrospectively analyzed the impact of "intermediate-dose" (ID-CY, 2.5 g/m(2)) versus "high-dose" (HD-CY, 4 g/m(2)) cyclophosphamide in 101 (48 vs. 53) consecutively evaluable myeloma patients (median age 59 years, range 32-72 years) who underwent stem cell mobilization after induction chemotherapy. Successful stem cell harvest was defined as a stem cell yield of at least 5 million CD34 cells per kg bodyweight. Evaluation of toxicity especially considered infectious complications and hematological toxicity in both subgroups.
RESULTS: Successful stem cell mobilization was achieved in 40 of 48 (83 %) and 44 of 53 (83 %) patients, respectively. The median time to apheresis (11 vs. 12 days) and the median CD34 content of stem cell harvest (8.3 vs. 7.6 million CD34 cells per kg bodyweight) did not differ significantly between both groups. There was a significant difference of WBC nadir in favor of the cyclophosphamide regimen with 2.5 g/m(2) (0.8 vs. 0.3 Gpt/L, p = 0.021), and neutropenic fever was more often observed in patients who received 4 g/m(2) cyclophosphamide (34 vs. 15 %, p = 0.078). Importantly, after induction chemotherapy using the VCD regimen (bortezomib, cyclophosphamide, dexamethasone), successful stem cell mobilization was achieved in 26 of 29 (90 %) patients treated with 2.5 g/m(2) and 21 of 25 (84 %) patients receiving 4 g/m(2) cyclophosphamide, respectively.
CONCLUSIONS: ID-CY is safe and highly effective for stem cell mobilization in patients with newly diagnosed myeloma and associated with a reduced toxicity compared to HD-CY.
Mateos MV, Oriol A, Martínez-López J, et al.
Outcomes with two different schedules of bortezomib, melphalan, and prednisone (VMP) for previously untreated multiple myeloma: matched pair analysis using long-term follow-up data from the phase 3 VISTA and PETHEMA/GEM05 trials.
Ann Hematol. 2016; 95(12):2033-2041 [PubMed] Related Publications
Outcomes with two different schedules of bortezomib, melphalan, and prednisone (VMP) for previously untreated multiple myeloma: matched pair analysis using long-term follow-up data from the phase 3 VISTA and PETHEMA/GEM05 trials.
Ann Hematol. 2016; 95(12):2033-2041 [PubMed] Related Publications
Bortezomib-melphalan-prednisone (VMP) is a standard-of-care for previously untreated, transplant-ineligible multiple myeloma (MM). Here, we compared outcomes between VMP regimens in the VISTA trial (9-cycle VMP schedule, including 4 cycles of twice weekly bortezomib) and the PETHEMA/GEM05 trial (less intensive 6-cycle VMP schedule with 1 cycle of twice weekly and 5 cycles of weekly bortezomib, then bortezomib-based maintenance). A total of 113 patient pairs matched by propensity score (estimated using logistic regression and incorporating eight exposure/outcome-related parameters) were included in this retrospective analysis. Median cumulative bortezomib dose was higher in PETHEMA/GEM05 than VISTA (49.6 vs 37.0 mg/m(2)); median dose intensity was lower (2.0 vs 5.1 mg/m(2)/month). Median progression-free survival (PFS) and time-to-progression (TTP) were significantly longer in PETHEMA/GEM05 than VISTA (PFS, 30.5 vs 20.0 months, p = 0.0265; TTP, 33.8 vs 24.2 months, p = 0.0049) after a median follow-up of 77.2 and 26.0 months, respectively. Median overall survival (OS) was similar (61.3 vs 61.0 months, p = 0.6528; median follow-up, 77.6 vs 60.1 months). Post-induction complete response rate was lower in PETHEMA/GEM05 than VISTA (19 vs 31 %; p = 0.03318); on-study (including maintenance) rate was similar (30 vs 31 %; p = 0.89437). This analysis suggests that the less-intensive PETHEMA/GEM05 VMP regimen plus maintenance may improve PFS and TTP, but not OS, compared with the VISTA VMP regimen.
TRIAL REGISTRATIONS: NCT00111319, NCT00443235.
TRIAL REGISTRATIONS: NCT00111319, NCT00443235.
Sasaki M
Current treatment of refractory and relapsed multiple myeloma.
Rinsho Ketsueki. 2016; 57(10):2084-2095 [PubMed] Related Publications
Current treatment of refractory and relapsed multiple myeloma.
Rinsho Ketsueki. 2016; 57(10):2084-2095 [PubMed] Related Publications
In the past decade, previously approved novel agents, such as proteasome inhibitors (bortezomib) and immunomodulatory drugs ([IMiDs]; e.g., lenalidomide), have led to significant improvement in the treatment of multiple myeloma in Japan. However, almost all patients will ultimately relapse, even when they have achieved a deep and prolonged therapeutic response with initial treatment. Next-generation IMiDs (pomalidomide) and deacetylase inhibitors (panobinostat) were approved for use as salvage therapy for refractory and relapsed multiple myeloma [RRMM] within the last year. Long-term chemotherapy could result in the emergence of drug-resistant clones due to "intraclonal heterogeneity" and "clonal evolution by Darwinian selection." Though some recommendations on the management of RRMM have been detailed, no uniform treatment has yet been established for these patients. Relapse situations are heterogeneous. Therefore, relapse management requires an individual approach based on assessments of patient-, disease-, and treatment-related factors. The primary considerations when selecting an appropriate treatment are patient-related factors such as frailty, comorbidity, disability, quality of life, and the overall goals of care. We hope that these novel agents that appear promising in Japan, such as monoclonal antibodies (e.g., elotuzumab, daratumumab) and next-generation proteasome inhibitors (e.g., carfilzomib, ixazomib) will improve the outcomes of patients with this incurable disease in the near future.
Tamura H
Treatment strategy for transplant-ineligible patients with newly diagnosed multiple myeloma.
Rinsho Ketsueki. 2016; 57(10):2074-2083 [PubMed] Related Publications
Treatment strategy for transplant-ineligible patients with newly diagnosed multiple myeloma.
Rinsho Ketsueki. 2016; 57(10):2074-2083 [PubMed] Related Publications
The current therapeutic strategy for multiple myeloma has improved dramatically due to the use of novel agents. In newly diagnosed transplant-ineligible myeloma patients, the standard therapy until the 1990s had long been melphalan and prednisolone (MP), but the recent recommendation is the proteasome inhibitor bortezomib plus MP (MPB), the immunomodulatory drug thalidomide plus MP (MPT), and the thalidomide derivative lenalidomide (LEN)-based regimens such as LEN plus low-dose dexamethasone (Ld) and LEN plus MP (MPL). The overall response rate in patients treated with Ld, MPL, or MPB was reported to be approximately 70%. Achieving complete remission (CR) is important in elderly as well as younger patients. Therefore, MPB administration appears to be the most appropriate initial therapy because the MPB regimen results in high CR rates. However, in elderly patients, especially in those 75 years of age and older and those who are frail or with comorbidities, it is important to balance efficacy and toxicity as well as to maintain quality of life. Furthermore, continuous treatment results in longer survival than a fixed-duration regimen in this population.
Sunami K
Treatment strategy in untreated transplant-eligible multiple myeloma patients.
Rinsho Ketsueki. 2016; 57(10):2064-2073 [PubMed] Related Publications
Treatment strategy in untreated transplant-eligible multiple myeloma patients.
Rinsho Ketsueki. 2016; 57(10):2064-2073 [PubMed] Related Publications
Autologous stem cell transplantation (ASCT) is known to be superior to conventional chemotherapies and has been established as a standard of care for young patients with multiple myeloma. In the first decade of this century, novel agents such as thalidomide, bortezomib, and lenalidomide became clinically available, and several clinical trials using these drugs as induction therapies, conditioning regimens, and post-transplant consolidation and maintenance therapies have been reported, leading to increasing improvement in treatment results as compared to conventional therapies. Future changes in therapeutic strategies using these novel agents are anticipated to increase the complete response rate and prolong progression free survival and overall survival. This article describes the optimal treatment strategy for ASCT-eligible patients in Japan.
Matsuoka A, Mitsuma A, Maeda O, et al.
Quantitative assessment of chemotherapy-induced peripheral neurotoxicity using a point-of-care nerve conduction device.
Cancer Sci. 2016; 107(10):1453-1457 [PubMed] Free Access to Full Article Related Publications
Quantitative assessment of chemotherapy-induced peripheral neurotoxicity using a point-of-care nerve conduction device.
Cancer Sci. 2016; 107(10):1453-1457 [PubMed] Free Access to Full Article Related Publications
Chemotherapy-induced peripheral neurotoxicity (CIPN) seriously impairs patients' quality of life cumulatively and dose-dependently. Because assessment of CIPN usually depends on patients' subjective evaluation of symptoms, objective and quantitative measures are needed. We evaluated a point-of-care nerve conduction device (POCD), previously validated for the assessment of diabetic peripheral neuropathy. Sensory nerve action potential (SNAP) amplitude and sensory nerve conduction velocity (SNCV) of the sural nerve were measured using a portable, automated POCD (DPNCheck; NeuroMetrix Inc., Waltham, MA, USA) in patients with a clinical diagnosis of CIPN of grade 1 or higher. We compared SNAP and SNCV among patients with different grades of CIPN according to the Common Terminology Criteria for Adverse Events. A total of 50 patients (22 men, 28 women; median age, 64 years; grade 1/2/3, 21/18/11) were evaluated. Anticancer drugs responsible for CIPN were cisplatin in five patients, oxaliplatin in 15, carboplatin in 5, paclitaxel in 16, docetaxel in 14, nab-paclitaxel in 7, vincristine in 6, and bortezomib in 3. Unadjusted SNAP was 8.45 ± 3.67 μV (mean ± SD) in patients with grade 1 CIPN, 5.42 ± 2.68 μV with grade 2, and 2.45 ± 1.52 μV with grade 3. Unadjusted SNCV was 49.71 ± 4.77 m/s in patients with grade 1 CIPN, 48.78 ± 6.33 m/s with grade 2, and 44.14 ± 7.31 m/s with grade 3. The adjusted SNAP after controlling for age significantly differed between each CTCAE grade (P < 0.001, ancova). The adjusted SNCV after controlling for age and height also differed significantly (P = 0.027). Differences in the severity of CIPN could be detected objectively and quantitatively using this POCD.
Sivaraj D, Green MM, Gasparetto C
Panobinostat for the management of multiple myeloma.
Future Oncol. 2017; 13(6):477-488 [PubMed] Related Publications
Panobinostat for the management of multiple myeloma.
Future Oncol. 2017; 13(6):477-488 [PubMed] Related Publications
Multiple myeloma (MM) is the second most common blood cancer following non-Hodgkin's lymphoma. While the treatments for MM have improved over the past decade, for the most part, it remains an incurable disease. For this reason newer therapeutic agents are needed to combat this malignancy. Panobinostat is a pan-deacetylase inhibitor that impedes protein destruction by disturbing the enzymatic activity of deacetylases. It was US FDA approved in February 2015 for the management of relapsed/refractory MM in combination with bortezomib and dexamethasone. Several trials are ongoing, exploring the utility of panobinostat in various other settings for the management of MM. This review will detail the biology, clinical efficacy and potential future applications of panobinostat in the treatment of MM.
Mangiacavalli S, Pompa A, Ferretti V, et al.
The possible role of burden of therapy on the risk of myeloma extramedullary spread.
Ann Hematol. 2017; 96(1):73-80 [PubMed] Related Publications
The possible role of burden of therapy on the risk of myeloma extramedullary spread.
Ann Hematol. 2017; 96(1):73-80 [PubMed] Related Publications
Extramedullary relapse (EMR) represents a poor prognostic marker in the course of multiple myeloma (MM). We reviewed data from 329 patients, diagnosed between 2000 and 2010, without extramedullary disease at onset to explore possible risk factors for EMR. The median overall survival of our study cohort was 6.4 years. The risk of EMR was 28 % with a median time from diagnosis to first EMR of 2.2 years (0.2-9.1 years). Patients with soft tissue masses located in extra-osseous organs (EMR-S) showed the worst outcome, compared to those with tumor masses arising from adjacent bone (EMR-B) (median OS 1.6 vs 2.4 years, p = 0.006). In addition, patients with EMR-S showed a significant trend for further development of extramedullary masses in a very short time (3.7 vs 5.7 months for EMR-B, p = 0.043). Multivariate analysis failed to identify any clinically presenting features predictive for EMR. The occurrence of EMR was higher in patients with more complex treatment history, defined on the basis of longer treatment duration (≥6 vs <6 months) and on elevated number of treatment lines administered (>2 vs ≤2 lines) (HR = 4.5, p < 0.001 and HR = 9.0, p < 0.001, respectively, when one or both factors are present).In conclusion, increasing burden of treatment might be a possible risk factor for EMR. MM patients with multiple relapses should be comprehensively investigated including, when possible, a whole-body-targeted radiologic technique to accurately detect EMR. Treatment choice should take into account the very poor outcome for patients with soft tissue involvement.
Gavriatopoulou M, Terpos E, Kastritis E, Dimopoulos MA
Current treatments for renal failure due to multiple myeloma.
Expert Opin Pharmacother. 2016; 17(16):2165-2177 [PubMed] Related Publications
Current treatments for renal failure due to multiple myeloma.
Expert Opin Pharmacother. 2016; 17(16):2165-2177 [PubMed] Related Publications
INTRODUCTION: Renal impairment (RI) is one of the most common complication of multiple myeloma (MM). RI is present in almost 20% of MM patients at diagnosis and in 40%-50% of patients during the course of their disease. Areas covered: Biology along with tools for diagnosis and management of RI are reported in this paper. Papers published in PubMed and reported abstracts up to May 2016 were used. Expert opinion: Moderate and severe RI increases the risk of early death; thus rapid intervention and initiation of anti-myeloma treatment is essential and improves renal outcomes in RI patients. Bortezomib and dexamethasone triplet combinations are the current standard of therapy for MM patients with acute kidney injury due to cast nephropathy; they offer high rates of both anti-myeloma response and renal recovery. Thalidomide and lenalidomide may be used in bortezomib refractory patients. In the relapsed/refractory setting additional treatment options such as carfilzomib, pomalidomide and monoclonal antibodies are available; however, there is limited data for their effects on patients with RI. High dose melphalan with autologous stem cell transplantation should be considered in otherwise eligible patients with RI. Finally, high cut-off hemodialysis membranes do not seem to offer significant additive effects on anti-myeloma therapies.
Hashimoto S, Kuroha T, Yano T, et al.
The Addition of Low-dose Thalidomide to Bortezomib and Dexamethasone for Refractory Multiple Myeloma.
Intern Med. 2016; 55(20):3025-3028 [PubMed] Free Access to Full Article Related Publications
The Addition of Low-dose Thalidomide to Bortezomib and Dexamethasone for Refractory Multiple Myeloma.
Intern Med. 2016; 55(20):3025-3028 [PubMed] Free Access to Full Article Related Publications
Five cases were treated by adding daily low-dose thalidomide (50 mg) to bortezomib and dexamethasone therapy for refractory multiple myeloma. This therapy was effective in four cases, with an improvement of bone pain and regression of M-protein. One case was treated with cyclophosphamide, thalidomide, and dexamethasone, adding bortezomib after starting the three-drug combination therapy. This patient has remained in a stable disease state since the beginning of this therapy. Regarding the other four cases, a partial response and a prolonged survival for approximately one year were noted. Peripheral neuropathy did not increase after thalidomide addition. Adding low-dose thalidomide may safely improve the responses for multiple myeloma refractory to bortezomib and dexamethasone.
Voorhees PM, Usmani SZ
The role of high-dose melphalan and autologous stem cell transplant in the rapidly evolving era of modern multiple myeloma therapy.
Clin Adv Hematol Oncol. 2016; 14(9):719-28 [PubMed] Related Publications
The role of high-dose melphalan and autologous stem cell transplant in the rapidly evolving era of modern multiple myeloma therapy.
Clin Adv Hematol Oncol. 2016; 14(9):719-28 [PubMed] Related Publications
The advent of the immunomodulatory drugs thalido-mide, lenalidomide, and pomalidomide; the proteasome inhib-itors bortezomib, carfilzomib, and ixazomib; the histone deacet-ylase inhibitor panobinostat; and the monoclonal antibodies elotuzumab and daratumumab has led to dramatic improvements in outcomes for patients with multiple myeloma. Along with progress in nontransplant therapy have come questions regarding the continued role of high-dose melphalan (HDM) supported by autologous stem cell transplant (ASCT) in the treatment of multiple myeloma. Emerging evidence from phase 3 studies demonstrates that consolidation therapy with HDM/ASCT further improves depth of response and progression-free survival in the context of modern therapy for multiple myeloma. Moreover, unprecedented survival data from ongoing phase 3 studies of patients treated with modern myeloma therapy followed by HDM/ASCT in first-line or second-line therapy reaffirm single and tandem HDM/ASCT as important standards of care for eligible patients. Herein, we review the evolving role of HDM/ASCT for the treatment of patients with newly diagnosed or relapsed multiple myeloma.
Palumbo A, Chanan-Khan A, Weisel K, et al.
Daratumumab, Bortezomib, and Dexamethasone for Multiple Myeloma.
N Engl J Med. 2016; 375(8):754-66 [PubMed] Related Publications
Daratumumab, Bortezomib, and Dexamethasone for Multiple Myeloma.
N Engl J Med. 2016; 375(8):754-66 [PubMed] Related Publications
BACKGROUND: Daratumumab, a human IgGκ monoclonal antibody that targets CD38, induces direct and indirect antimyeloma activity and has shown substantial efficacy as monotherapy in heavily pretreated patients with multiple myeloma, as well as in combination with bortezomib in patients with newly diagnosed multiple myeloma.
METHODS: In this phase 3 trial, we randomly assigned 498 patients with relapsed or relapsed and refractory multiple myeloma to receive bortezomib (1.3 mg per square meter of body-surface area) and dexamethasone (20 mg) alone (control group) or in combination with daratumumab (16 mg per kilogram of body weight) (daratumumab group). The primary end point was progression-free survival.
RESULTS: A prespecified interim analysis showed that the rate of progression-free survival was significantly higher in the daratumumab group than in the control group; the 12-month rate of progression-free survival was 60.7% in the daratumumab group versus 26.9% in the control group. After a median follow-up period of 7.4 months, the median progression-free survival was not reached in the daratumumab group and was 7.2 months in the control group (hazard ratio for progression or death with daratumumab vs. control, 0.39; 95% confidence interval, 0.28 to 0.53; P<0.001). The rate of overall response was higher in the daratumumab group than in the control group (82.9% vs. 63.2%, P<0.001), as were the rates of very good partial response or better (59.2% vs. 29.1%, P<0.001) and complete response or better (19.2% vs. 9.0%, P=0.001). Three of the most common grade 3 or 4 adverse events reported in the daratumumab group and the control group were thrombocytopenia (45.3% and 32.9%, respectively), anemia (14.4% and 16.0%, respectively), and neutropenia (12.8% and 4.2%, respectively). Infusion-related reactions that were associated with daratumumab treatment were reported in 45.3% of the patients in the daratumumab group; these reactions were mostly grade 1 or 2 (grade 3 in 8.6% of the patients), and in 98.2% of these patients, they occurred during the first infusion.
CONCLUSIONS: Among patients with relapsed or relapsed and refractory multiple myeloma, daratumumab in combination with bortezomib and dexamethasone resulted in significantly longer progression-free survival than bortezomib and dexamethasone alone and was associated with infusion-related reactions and higher rates of thrombocytopenia and neutropenia than bortezomib and dexamethasone alone. (Funded by Janssen Research and Development; ClinicalTrials.gov number, NCT02136134.).
METHODS: In this phase 3 trial, we randomly assigned 498 patients with relapsed or relapsed and refractory multiple myeloma to receive bortezomib (1.3 mg per square meter of body-surface area) and dexamethasone (20 mg) alone (control group) or in combination with daratumumab (16 mg per kilogram of body weight) (daratumumab group). The primary end point was progression-free survival.
RESULTS: A prespecified interim analysis showed that the rate of progression-free survival was significantly higher in the daratumumab group than in the control group; the 12-month rate of progression-free survival was 60.7% in the daratumumab group versus 26.9% in the control group. After a median follow-up period of 7.4 months, the median progression-free survival was not reached in the daratumumab group and was 7.2 months in the control group (hazard ratio for progression or death with daratumumab vs. control, 0.39; 95% confidence interval, 0.28 to 0.53; P<0.001). The rate of overall response was higher in the daratumumab group than in the control group (82.9% vs. 63.2%, P<0.001), as were the rates of very good partial response or better (59.2% vs. 29.1%, P<0.001) and complete response or better (19.2% vs. 9.0%, P=0.001). Three of the most common grade 3 or 4 adverse events reported in the daratumumab group and the control group were thrombocytopenia (45.3% and 32.9%, respectively), anemia (14.4% and 16.0%, respectively), and neutropenia (12.8% and 4.2%, respectively). Infusion-related reactions that were associated with daratumumab treatment were reported in 45.3% of the patients in the daratumumab group; these reactions were mostly grade 1 or 2 (grade 3 in 8.6% of the patients), and in 98.2% of these patients, they occurred during the first infusion.
CONCLUSIONS: Among patients with relapsed or relapsed and refractory multiple myeloma, daratumumab in combination with bortezomib and dexamethasone resulted in significantly longer progression-free survival than bortezomib and dexamethasone alone and was associated with infusion-related reactions and higher rates of thrombocytopenia and neutropenia than bortezomib and dexamethasone alone. (Funded by Janssen Research and Development; ClinicalTrials.gov number, NCT02136134.).
Imai Y, Maru Y, Tanaka J
Action mechanisms of histone deacetylase inhibitors in the treatment of hematological malignancies.
Cancer Sci. 2016; 107(11):1543-1549 [PubMed] Free Access to Full Article Related Publications
Action mechanisms of histone deacetylase inhibitors in the treatment of hematological malignancies.
Cancer Sci. 2016; 107(11):1543-1549 [PubMed] Free Access to Full Article Related Publications
Histone deacetylases (HDACs) critically regulate gene expression by determining the acetylation status of histones. Studies have increasingly focused on the activities of HDACs, especially involving non-histone proteins, and their various biological effects. Aberrant HDAC expression observed in several kinds of human tumors makes HDACs potential targets for cancer treatment. Several preclinical studies have suggested that HDAC inhibitors show some efficacy in the treatment of acute myelogenous leukemia with AML1-ETO, which mediates transcriptional repression through its interaction with a complex including HDAC1. Recurrent mutations in epigenetic regulators are found in T-cell lymphomas (TCLs), and HDAC inhibitors and hypomethylating agents were shown to act cooperatively in the treatment of TCLs. Preclinical modeling has suggested that persistent activation of the signal transducer and activator of transcription signaling pathway could serve as a useful biomarker of resistance to HDAC inhibitor in patients with cutaneous TCL. Panobinostat, a pan-HDAC inhibitor, in combination with bortezomib and dexamethasone, has achieved longer progression-free survival in patients with relapsed/refractory multiple myeloma (MM) than the placebo in combination with bortezomib and dexamethasone. Panobinostat inhibited MM cell growth by degrading protein phosphatase 3 catalytic subunit α (PPP3CA), a catalytic subunit of calcineurin. This degradation was suggested to be mediated by the blockade of the chaperone function of heat shock protein 90 due to HDAC6 inhibition. Aberrant PPP3CA expression in advanced MM indicated a possible correlation between high PPP3CA expression and the pathogenesis of MM. Furthermore, PPP3CA was suggested as a common target of panobinostat and bortezomib.
Vaiou M, Pangou E, Liakos P, et al.
Endothelin-1 (ET-1) induces resistance to bortezomib in human multiple myeloma cells via a pathway involving the ETB receptor and upregulation of proteasomal activity.
J Cancer Res Clin Oncol. 2016; 142(10):2141-58 [PubMed] Related Publications
Endothelin-1 (ET-1) induces resistance to bortezomib in human multiple myeloma cells via a pathway involving the ETB receptor and upregulation of proteasomal activity.
J Cancer Res Clin Oncol. 2016; 142(10):2141-58 [PubMed] Related Publications
PURPOSE: Bortezomib (BTZ) is used for the treatment of multiple myeloma (MM). However, a significant proportion of patients may be refractory to the drug. This study aimed to investigate whether the endothelin (ET-1) axis may act as an escape mechanism to treatment with bortezomib in MM cells.
METHODS: NCI-H929 and RPMI-8226 (human MM cell lines) were cultured with or without ET-1, BTZ, and inhibitors of the endothelin receptors. ET-1 levels were determined by ELISA, while the protein levels of its receptors and of the PI3K and MAPK pathways' components by western blot. Effects of ET-1 on cell proliferation were studied by MTT and on the ubiquitin proteasome pathway by assessing the chymotryptic activity of the 20S proteasome in cell lysates.
RESULTS: Endothelin receptors A and B (ETAR and ETBR, respectively) were found to be expressed in both cell lines, with the RPMI-8226 cells that are considered resistant to BTZ, expressing higher levels of ETBR and in addition secreting ET-1. Treatment of the NCI-H929 cells with ET-1 increased proliferation, while co-incubation of these cells with ET-1 and BTZ decreased BTZ efficacy with concomitant upregulation of 20S proteasomal activity. Si-RNA silencing or chemical blockade of ETBR abrogated the protective effects of ET-1. Finally, data suggest that the predominant signaling pathway involved in ET-1/ETBR-induced BTZ resistance in MM cells may be the MAPK pathway.
CONCLUSION: Our data suggest a possible role of the ET-1/ETBR axis in regulating the sensitivity of MM cells to BTZ. Thus, combining bortezomib with strategies to target the ET-1 axis could prove to be a novel promising therapeutic approach in MM.
METHODS: NCI-H929 and RPMI-8226 (human MM cell lines) were cultured with or without ET-1, BTZ, and inhibitors of the endothelin receptors. ET-1 levels were determined by ELISA, while the protein levels of its receptors and of the PI3K and MAPK pathways' components by western blot. Effects of ET-1 on cell proliferation were studied by MTT and on the ubiquitin proteasome pathway by assessing the chymotryptic activity of the 20S proteasome in cell lysates.
RESULTS: Endothelin receptors A and B (ETAR and ETBR, respectively) were found to be expressed in both cell lines, with the RPMI-8226 cells that are considered resistant to BTZ, expressing higher levels of ETBR and in addition secreting ET-1. Treatment of the NCI-H929 cells with ET-1 increased proliferation, while co-incubation of these cells with ET-1 and BTZ decreased BTZ efficacy with concomitant upregulation of 20S proteasomal activity. Si-RNA silencing or chemical blockade of ETBR abrogated the protective effects of ET-1. Finally, data suggest that the predominant signaling pathway involved in ET-1/ETBR-induced BTZ resistance in MM cells may be the MAPK pathway.
CONCLUSION: Our data suggest a possible role of the ET-1/ETBR axis in regulating the sensitivity of MM cells to BTZ. Thus, combining bortezomib with strategies to target the ET-1 axis could prove to be a novel promising therapeutic approach in MM.
Iqbal N, Tariq MU, Shaikh MU, Majid H
Pleural effusion as a manifestation of multiple myeloma.
BMJ Case Rep. 2016; 2016 [PubMed] Related Publications
Pleural effusion as a manifestation of multiple myeloma.
BMJ Case Rep. 2016; 2016 [PubMed] Related Publications
Multiple myeloma is a clonal B-cell malignancy, characterised by proliferation of plasma cells and secretion of paraproteins. These plasma cells accumulate predominantly in the bone marrow; rarely, they invade other areas, especially the thorax. Myeloma presenting with a pleural effusion is rare and reported in only 6% of patients with myeloma. Such patients generally present late and have a poor prognosis. Here, we describe a patient presenting with a lung mass, renal failure and a massive unilateral pleural effusion due to multiple myeloma who was treated successfully.
Gonsalves WI, Milani P, Derudas D, Buadi FK
The next generation of novel therapies for the management of relapsed multiple myeloma.
Future Oncol. 2017; 13(1):63-75 [PubMed] Article available free on PMC after 01/01/2018 Related Publications
The next generation of novel therapies for the management of relapsed multiple myeloma.
Future Oncol. 2017; 13(1):63-75 [PubMed] Article available free on PMC after 01/01/2018 Related Publications
The advent of various novel therapies such as immunomodulators and proteasome inhibitors has transformed the treatment paradigm for patients with multiple myeloma (MM). As a result, the overall survival has improved dramatically over the last decade. Despite these advances, MM remains mostly incurable and most patients experience disease relapse after enjoying a period of disease control or remission. Fortunately, the scientific community continues to make strides in developing 'next-generation' therapies for the management of patients with relapsed MM. This review will summarize the efficacy of some of the newest therapeutic agents available for the treatment of patients with relapsed MM after their upfront treatment with the original novel agents such as thalidomide, lenalidomide and bortezomib.
Esaki M, Ishii K, Azuma Y, et al.
Rapid improvement of hyperammonemic encephalopathy by bortezomib treatment in IgD-type multiple myeloma.
Rinsho Ketsueki. 2016; 57(7):854-8 [PubMed] Related Publications
Rapid improvement of hyperammonemic encephalopathy by bortezomib treatment in IgD-type multiple myeloma.
Rinsho Ketsueki. 2016; 57(7):854-8 [PubMed] Related Publications
A 74-year-old man visited our hospital with complaints of anorexia, weight loss, and impaired activities of daily living. He presented mild consciousness disturbance at the first visit, but specific causes were identified. The IgD level was>2,000 mg/dl and bone marrow biopsy was performed after aspiration failed due to excessive density. He was diagnosed with IgD/λ multiple myeloma (MM). He lapsed into a coma with an extremely high ammonia level of 484 μg/dl on day 8 after admission. His diagnosis was established as hyperammonemic encephalopathy (HE). He was treated with dexamethasone (Dex) pulse therapy and continuous hemodiafiltration. Minor improvement of hyperammonemia was achieved. Combination therapy with bortezomib and Dex was commenced. His ammonia level rapidly decreased and his mental state improved. HE accompanied by MM is rare and further studies are needed to clarify outcomes in response to treatment using the novel agent Bor. Although HE is potentially fatal, we found Bor to be rapidly effective against HE.


 Myeloma
Myeloma