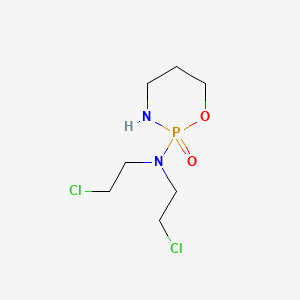
Cyclophosphamide
"Precursor of an alkylating nitrogen mustard antineoplastic and immunosuppressive agent that must be activated in the LIVER to form the active aldophosphamide. It has been used in the treatment of LYMPHOMA and LEUKEMIA. Its side effect, ALOPECIA, has been used for defleecing sheep. Cyclophosphamide may also cause sterility, birth defects, mutations, and cancer." (MeSH 2013)
Found this page useful?
 Web Resources: Cyclophosphamide
Web Resources: Cyclophosphamide Latest Research Publications
Latest Research PublicationsWeb Resources: Cyclophosphamide (6 links)
Cancer Research UK
Irish Cancer Society
Macmillan Cancer Support
NHS Evidence
 Cyclophosphamide - Substance Summary
Cyclophosphamide - Substance Summary
PubChem
MedlinePlus
Latest Research Publications
This list of publications is regularly updated (Source: PubMed).
Nishimura M, Onoe T, Sakai H, et al.
Safety and Relative Dose Intensity of Dose-dense Doxorubicin and Cyclophosphamide Followed by Dose-dense Paclitaxel.
Anticancer Res. 2019; 39(8):4379-4383 [PubMed] Related Publications
Safety and Relative Dose Intensity of Dose-dense Doxorubicin and Cyclophosphamide Followed by Dose-dense Paclitaxel.
Anticancer Res. 2019; 39(8):4379-4383 [PubMed] Related Publications
BACKGROUND/AIM: Dose-dense doxorubicin and cyclophosphamide (ddAC) followed by dose-dense paclitaxel (ddP) (ddAC-P) has improved disease-free survival of patients with breast cancer. The aim of this study was to evaluate the safety and relative dose intensity (RDI) of ddAC-P administered together with pegfilgrastim.
PATIENTS AND METHODS: Between May 2015 and Aug 2017, 44 patients were retrospectively reviewed; they were administered 4 cycles of ddAC, followed by 4 cycles of ddP. Pegfilgrastim (3.6 mg) was administered in every cycle.
RESULTS: The mean RDIs for ddAC-P, ddAC, and ddP were 95.0%, 94.5%, and 93.3%, respectively. The prevalence of high RDIs (≥85%) for ddAC-P, ddAC, and ddP was 90.9%, 84.1%, and 88.6%, respectively. Seven of the 10 patients with low RDIs experienced grade 1 or 2 fever.
CONCLUSION: DdAC-P administered together with pegfilgrastim (3.6 mg) appears to be feasible and maintains RDI in most of Japanese patients with breast cancer. Rapid evaluation and proper management of fever may prevent low RDI.
PATIENTS AND METHODS: Between May 2015 and Aug 2017, 44 patients were retrospectively reviewed; they were administered 4 cycles of ddAC, followed by 4 cycles of ddP. Pegfilgrastim (3.6 mg) was administered in every cycle.
RESULTS: The mean RDIs for ddAC-P, ddAC, and ddP were 95.0%, 94.5%, and 93.3%, respectively. The prevalence of high RDIs (≥85%) for ddAC-P, ddAC, and ddP was 90.9%, 84.1%, and 88.6%, respectively. Seven of the 10 patients with low RDIs experienced grade 1 or 2 fever.
CONCLUSION: DdAC-P administered together with pegfilgrastim (3.6 mg) appears to be feasible and maintains RDI in most of Japanese patients with breast cancer. Rapid evaluation and proper management of fever may prevent low RDI.
Li F, Yao FS, Zhu XJ, et al.
A randomized phase II, open-label and multicenter study of combination regimens of bortezomib at two doses by subcutaneous injection for newly diagnosed multiple myeloma patients.
J Cancer Res Clin Oncol. 2019; 145(9):2343-2355 [PubMed] Related Publications
A randomized phase II, open-label and multicenter study of combination regimens of bortezomib at two doses by subcutaneous injection for newly diagnosed multiple myeloma patients.
J Cancer Res Clin Oncol. 2019; 145(9):2343-2355 [PubMed] Related Publications
PURPOSE: Combinations of bortezomib (Velcade), cyclophosphamide and dexamethasone have shown significant efficacy and safety for patients of newly diagnosed multiple myeloma (NDMM). In this study, we compared the efficacy and safety of modified VCD regimens with novel changes in bortezomib dose and schedule for NDMM.
METHODS: Eighty-five NDMM patients from multiple centers were randomly assigned to a high-dose (1.6 mg/m
RESULTS: After four cycles, complete response (CR) or better in group A (43.6%) was higher than that in group B (12.8%) (P = 0.002). During induction, for patients with R-ISS stage III, the CR or better rate in group A was superior to that in group B (P = 0.01). Of patients < 65, the CR or better rate of group A was superior to that of group B (P = 0.004). Rapid onset of CR occurred in group A (P < 0.01). Meanwhile, rate of 3-4 diarrhea was higher in group A (P = 0.03), which caused higher rate of dose reduction for patients ≥ 65 (P = 0.041). No significant difference between the two groups in PFS and OS.
CONCLUSIONS: The studied high-dose VCD as induction regimen had an improved CR rate, especially in patients < 65 or with R-ISS stage III, and is feasible for young and high-risk patients. Trial registration ClinicalTrials.gov: NCT02086942.
METHODS: Eighty-five NDMM patients from multiple centers were randomly assigned to a high-dose (1.6 mg/m
RESULTS: After four cycles, complete response (CR) or better in group A (43.6%) was higher than that in group B (12.8%) (P = 0.002). During induction, for patients with R-ISS stage III, the CR or better rate in group A was superior to that in group B (P = 0.01). Of patients < 65, the CR or better rate of group A was superior to that of group B (P = 0.004). Rapid onset of CR occurred in group A (P < 0.01). Meanwhile, rate of 3-4 diarrhea was higher in group A (P = 0.03), which caused higher rate of dose reduction for patients ≥ 65 (P = 0.041). No significant difference between the two groups in PFS and OS.
CONCLUSIONS: The studied high-dose VCD as induction regimen had an improved CR rate, especially in patients < 65 or with R-ISS stage III, and is feasible for young and high-risk patients. Trial registration ClinicalTrials.gov: NCT02086942.
Nakamura Y, Tanaka Y, Tanaka M, et al.
Significance of Granulocyte Colony-Stimulating Factor-Combined High-Dose Cytarabine, Cyclophosphamide, and Total Body Irradiation in Allogeneic Hematopoietic Cell Transplantation for Myeloid Malignant Neoplasms.
Transplant Proc. 2019; 51(3):896-900 [PubMed] Related Publications
Significance of Granulocyte Colony-Stimulating Factor-Combined High-Dose Cytarabine, Cyclophosphamide, and Total Body Irradiation in Allogeneic Hematopoietic Cell Transplantation for Myeloid Malignant Neoplasms.
Transplant Proc. 2019; 51(3):896-900 [PubMed] Related Publications
Allogeneic hematopoietic cell transplant (HCT) is a curative procedure for myeloid malignant neoplasms, but relapse after HCT remains critical. A conditioning regimen involving granulocyte colony-stimulating factor-combined high-dose cytarabine, cyclophosphamide, and total body irradiation (G-CSF-combined high-dose cytarabine/cyclophosphamide/total-body irradiation [HDCA/CY/TBI]) was reported to improve outcomes after cord blood transplant (CBT) for myeloid malignant neoplasms, but this regimen was not previously evaluated among patients undergoing bone marrow transplant (BMT) or peripheral blood stem cell transplant (PBSCT).
METHODS: We retrospectively analyzed 28 patients who underwent allogeneic HCT including BMT from a related (1 patient) or unrelated donor (9 patients), PBSCT from a related donor (7 patients), or single-unit CBT from an unrelated donor (11 patients) after a G-CSF-combined HDCA/CY/TBI regimen.
RESULTS: All patients achieved neutrophil and platelet engraftment, which were significantly more rapid in the BMT/PBSCT group than in the CBT group. Eighteen patients were alive at a median follow-up of 54.3 months. The 3-year relapse and nonrelapse mortality rates were 28.6% and 7.1%, respectively, which were similar between the BMT/PBSCT and CBT groups. Overall survival and disease-free survival at 5 years after HCT were 62.6% and 64.3%, respectively, which were also similar between the BMT/PBSCT and CBT groups. Only disease status at HCT had a significant impact on overall survival and disease-free survival (86.7% with standard risk vs 38.5% with high risk and 86.7% with standard risk vs 38.5% with high risk, respectively).
CONCLUSION: A G-CSF-combined HDCA/CY/TBI regimen is a promising conditioning in patients with myeloid malignant neoplasms who undergo not only CBT but also BMT or PBSCT.
METHODS: We retrospectively analyzed 28 patients who underwent allogeneic HCT including BMT from a related (1 patient) or unrelated donor (9 patients), PBSCT from a related donor (7 patients), or single-unit CBT from an unrelated donor (11 patients) after a G-CSF-combined HDCA/CY/TBI regimen.
RESULTS: All patients achieved neutrophil and platelet engraftment, which were significantly more rapid in the BMT/PBSCT group than in the CBT group. Eighteen patients were alive at a median follow-up of 54.3 months. The 3-year relapse and nonrelapse mortality rates were 28.6% and 7.1%, respectively, which were similar between the BMT/PBSCT and CBT groups. Overall survival and disease-free survival at 5 years after HCT were 62.6% and 64.3%, respectively, which were also similar between the BMT/PBSCT and CBT groups. Only disease status at HCT had a significant impact on overall survival and disease-free survival (86.7% with standard risk vs 38.5% with high risk and 86.7% with standard risk vs 38.5% with high risk, respectively).
CONCLUSION: A G-CSF-combined HDCA/CY/TBI regimen is a promising conditioning in patients with myeloid malignant neoplasms who undergo not only CBT but also BMT or PBSCT.
Raciborska A, Bilska K, Rodriguez-Galindo C
Maintenance treatment with trofosfamide in patients with primary bone ewing sarcoma - single center experience.
Dev Period Med. 2019; 23(1):39-44 [PubMed] Related Publications
Maintenance treatment with trofosfamide in patients with primary bone ewing sarcoma - single center experience.
Dev Period Med. 2019; 23(1):39-44 [PubMed] Related Publications
OBJECTIVE: Background: Patients with Ewing sarcoma have a dismal outcome. Maintenance treatment with trofosfamide has been proposed as an effective regimen for some paediatric malignancies. Aim: We sought to evaluate the schedule of trofosfamide for patients with high-risk primary bone Ewing sarcoma.
PATIENTS AND METHODS: Materials and methods: Fifteen patients with primary bone Ewing sarcoma received treatment with trofosfamide (150 mg/m2 p.o. days 1-10) every 28 days. All patients had standard tumour imaging and laboratory evaluation. All toxicities were documented.
RESULTS: Results: A total of 90 cycles (median 5 cycles/patient) were administered. A complete response was maintained in nine patients, while six patients had disease progression during treatment. Median time to progression was 1.9 months (range 1.8 to 4.6). Eleven patients (73.3%) are alive including nine with no evidence of disease with a median follow-up of 3.9 years (range 1.4 to 7.6). All patients with active disease at the start of the trofosfamide treatment died. There were no significant toxicities.
CONCLUSION: Conclusions: Treatment with trofosfamide is well-tolerated and could have a role to maintain response in patients with primary bone Ewing sarcoma. Further studies are needed to better define the use of this regimen in the upfront management of those patients.
PATIENTS AND METHODS: Materials and methods: Fifteen patients with primary bone Ewing sarcoma received treatment with trofosfamide (150 mg/m2 p.o. days 1-10) every 28 days. All patients had standard tumour imaging and laboratory evaluation. All toxicities were documented.
RESULTS: Results: A total of 90 cycles (median 5 cycles/patient) were administered. A complete response was maintained in nine patients, while six patients had disease progression during treatment. Median time to progression was 1.9 months (range 1.8 to 4.6). Eleven patients (73.3%) are alive including nine with no evidence of disease with a median follow-up of 3.9 years (range 1.4 to 7.6). All patients with active disease at the start of the trofosfamide treatment died. There were no significant toxicities.
CONCLUSION: Conclusions: Treatment with trofosfamide is well-tolerated and could have a role to maintain response in patients with primary bone Ewing sarcoma. Further studies are needed to better define the use of this regimen in the upfront management of those patients.
Boddu PC, Zeidan AM
Myeloid disorders after autoimmune disease.
Best Pract Res Clin Haematol. 2019; 32(1):74-88 [PubMed] Article available free on PMC after 01/03/2020 Related Publications
Myeloid disorders after autoimmune disease.
Best Pract Res Clin Haematol. 2019; 32(1):74-88 [PubMed] Article available free on PMC after 01/03/2020 Related Publications
Autoimmune diseases (ADs) are associated with an increased risk not only of lymphoproliferative disorders but also of myeloid malignancies. The excess risk of myelodysplastic syndromes and/or acute myeloid leukemia is observed across several AD types, including systemic lupus erythematosus, rheumatoid arthritis, inflammatory bowel disorders, multiple sclerosis, among others. The risk of developing myeloid neoplasms (MNs) is dependent on several variables, including the specific AD type, chronicity and severity of the AD, type and duration of exposure of disease modifying anti-rheumatic drugs or cytotoxics/immunosuppressives, and genetic predisposition risk. Putative triggering factors linking AD to elevated MN risk include AD-directed medications, shared genetic susceptibilities between the two disease entities, and chronic immune stimulation or bone marrow infiltration by the AD. Molecular mechanisms underpinning leukemogenesis remain largely speculative and warrant further investigation. Leukemias arising in patients with AD are not always 'therapy-related' in that MNs may develop in certain AD subtypes even among patients with no prior therapy exposure. Only a few studies have attempted to determine factors associated with MN development in AD but failed to demonstrate consistent characteristic clinical or paraclinical features. These reports have failed to demonstrate a clear correlation between individual agent exposure and subsequent leukemia development due to the low rates of therapy exposure compounded by the rarity of MN occurrence. Notwithstanding, the leukemogenic potential is best documented with agents such as azathioprine, cyclophosphamide, and mitoxantrone; this risk of MN development does not appear to be shared by biologic approaches such as anti-tumor necrosis factors-alpha inhibitors. In this article, we discuss plausible biologic mechanisms underlying MN pathogenesis in AD and review the data available on the development of MNs in patients with AD.
Soltermann Y, Heim D, Medinger M, et al.
Reduced dose of post-transplantation cyclophosphamide compared to ATG for graft-versus-host disease prophylaxis in recipients of mismatched unrelated donor hematopoietic cell transplantation: a single-center study.
Ann Hematol. 2019; 98(6):1485-1493 [PubMed] Related Publications
Reduced dose of post-transplantation cyclophosphamide compared to ATG for graft-versus-host disease prophylaxis in recipients of mismatched unrelated donor hematopoietic cell transplantation: a single-center study.
Ann Hematol. 2019; 98(6):1485-1493 [PubMed] Related Publications
Post-transplantation cyclophosphamide (PTCy) demonstrated effectiveness to prevent GVHD after haploidentical hematopoietic cell transplantation (HCT). Reducing toxicities with a maximized efficacy is still challenging in HCT. In this retrospective study, we analyzed the safety and efficacy of transplantation from a 1-antigen HLA-mismatched unrelated donor (9/10 MMUD) in 80 patients with hematological disorders between 2010 and 2018; 22 patients received PTCy with a reduced dose of 40 mg/kg, cyclosporine A, and mycophenolate mofetil (MMF); 58 patients received anti-thymocyte globulin (ATG), cyclosporine A, and either methotrexate or MMF for GVHD prophylaxis. Cumulative incidence (CI) of acute GVHD grades II-IV in the PTCy group was significantly lower (15% vs. 50%, p = 0.006); however, CI of chronic GVHD was (not significantly) lower in the PTCy group (26% vs. 35%, p = 0.137). One-year OS was significantly longer (p = 0.008) in the PTCy group with a similar 1-year PFS (p = 0.114) in both groups. Rates of 1-year relapse and non-relapse mortality were similar. Median time to neutrophil engraftment was comparable in both GVHD prophylaxis groups (14 days vs. 16 days, respectively, p = 0.107). Our results show that a lower dose of PTCy-based prophylaxis is an effective and safe strategy to prevent acute GVHD in HCT with 9/10 MMUD compared to ATG.
Sun G, Zhang W, Wang J
Integrating systemic module inference with attract method excavates attractor modules for cyclophosphamide contributing to prostate cancer.
J Cancer Res Ther. 2019; 15(Supplement):S153-S158 [PubMed] Related Publications
Integrating systemic module inference with attract method excavates attractor modules for cyclophosphamide contributing to prostate cancer.
J Cancer Res Ther. 2019; 15(Supplement):S153-S158 [PubMed] Related Publications
Objective: The complete molecular mechanism that cyclophosphamide (CPA) induces the cell death is still unknown. To further reveal the mechanism of CPA contributing to prostate cancer, we conducted analysis on gene expression profile of E-GEOD-42913 to identify attractor modules by integrating systemic module inference with attract method.
Methods: First, case and control protein-protein interaction (PPI) networks were inferred based on Spearman correlation coefficient; then clique merging algorithm was performed to explore modules in the reweighted PPI network, and these modules were compared with each other so as to select similar modules; in the following, attractor modules were identified via attract method; finally, pathway enrichment analysis of genes in attractor modules was carried out.
Results: A total of 11,535 genes were gained. A novel PPI network with 4698 nodes (20,541 interactions) was established via mapping the genes of the gene expression profile onto the original PPIs. Then, 1635 and 1487 interactions (P < 0.05) were selected to construct the destination network for CPA group and control group, respectively. Moreover, under the threshold value of overlap -threshold value of each two modules ≥ 0.5, 42 and 56 modules were separately determined for CPA group and control group. Twenty-six pairs of similar modules ([J (S
Conclusions: We predicted that during the process of chemotherapy, CPA mainly affected the pathways of DNA replication and nucleotide excision repair to induce the cancer cell's death.
Methods: First, case and control protein-protein interaction (PPI) networks were inferred based on Spearman correlation coefficient; then clique merging algorithm was performed to explore modules in the reweighted PPI network, and these modules were compared with each other so as to select similar modules; in the following, attractor modules were identified via attract method; finally, pathway enrichment analysis of genes in attractor modules was carried out.
Results: A total of 11,535 genes were gained. A novel PPI network with 4698 nodes (20,541 interactions) was established via mapping the genes of the gene expression profile onto the original PPIs. Then, 1635 and 1487 interactions (P < 0.05) were selected to construct the destination network for CPA group and control group, respectively. Moreover, under the threshold value of overlap -threshold value of each two modules ≥ 0.5, 42 and 56 modules were separately determined for CPA group and control group. Twenty-six pairs of similar modules ([J (S
Conclusions: We predicted that during the process of chemotherapy, CPA mainly affected the pathways of DNA replication and nucleotide excision repair to induce the cancer cell's death.
Caffo O, Facchini G, Biasco E, et al.
Activity and safety of metronomic cyclophosphamide in the modern era of metastatic castration-resistant prostate cancer.
Future Oncol. 2019; 15(10):1115-1123 [PubMed] Related Publications
Activity and safety of metronomic cyclophosphamide in the modern era of metastatic castration-resistant prostate cancer.
Future Oncol. 2019; 15(10):1115-1123 [PubMed] Related Publications
AIM: To evaluate activity of metronomic cyclophosphamide (mCTX) in heavily pretreated metastatic castration-resistant prostate cancer (mCRPC) patients.
PATIENTS & METHODS: We retrospectively evaluated a consecutive series of 74 mCRPC patients treated with at least one new agent after docetaxel failure, who received once-daily oral mCTX treatment at a fixed dose of 50 mg.
RESULTS: The treatment was well tolerated. Sixteen percent of the patients experienced a major biochemical response. Median progression-free survival was 4.0 months, and median overall survival was 8.1 months.
CONCLUSIONS: In the modern context of mCRPC, mCTX may represent a valuable and inexpensive alternative to new agents, which have shown similar activity in heavily pretreated patients.
PATIENTS & METHODS: We retrospectively evaluated a consecutive series of 74 mCRPC patients treated with at least one new agent after docetaxel failure, who received once-daily oral mCTX treatment at a fixed dose of 50 mg.
RESULTS: The treatment was well tolerated. Sixteen percent of the patients experienced a major biochemical response. Median progression-free survival was 4.0 months, and median overall survival was 8.1 months.
CONCLUSIONS: In the modern context of mCRPC, mCTX may represent a valuable and inexpensive alternative to new agents, which have shown similar activity in heavily pretreated patients.
Lim YC, Kim H, Lim SM, Kim JS
Genetic analysis of a novel antioxidant multi-target iron chelator, M30 protecting against chemotherapy-induced alopecia in mice.
BMC Cancer. 2019; 19(1):149 [PubMed] Article available free on PMC after 01/03/2020 Related Publications
Genetic analysis of a novel antioxidant multi-target iron chelator, M30 protecting against chemotherapy-induced alopecia in mice.
BMC Cancer. 2019; 19(1):149 [PubMed] Article available free on PMC after 01/03/2020 Related Publications
BACKGROUND: Chemotherapy-induced alopecia has been well documented as a cause of distress to patients undergoing cancer treatment. Almost all traditional chemotherapeutic agents cause severe alopecia. Despite advances in the treatment of chemotherapy-induced alopecia, there is no effective treatment for preventing chemotherapy-induced alopecia.
METHODS: In the present study, we investigated the potential role of a multi-target iron chelator, M30 in protecting against cyclophosphamide-induced alopecia in C57BL/6 mice implanted with an osmotic pump. M30 enhanced hair growth and prevented cyclophosphamide-induced abnormal hair in the mice. Furthermore, we examined the gene expression profiles derived from skin biopsy specimens of normal mice, cyclophosphamide-treated mice, and cyclophosphamide treated mice with M30 supplement.
RESULTS: The top genes namely Tnfrsf19, Ercc2, Lama5, Ctsl, and Per1 were identified by microarray analysis. These genes were found to be involved in the biological processes of hair cycle, hair cycle phase, hair cycle process, hair follicle development, hair follicle maturation, hair follicle morphogenesis, regulation of hair cycle.
CONCLUSION: Our study demonstrates that M30 treatment is a promising therapy for cyclophosphamide-induced alopecia and suggests that the top five genes have unique preventive effects in cyclophosphamide-induced transformation.
METHODS: In the present study, we investigated the potential role of a multi-target iron chelator, M30 in protecting against cyclophosphamide-induced alopecia in C57BL/6 mice implanted with an osmotic pump. M30 enhanced hair growth and prevented cyclophosphamide-induced abnormal hair in the mice. Furthermore, we examined the gene expression profiles derived from skin biopsy specimens of normal mice, cyclophosphamide-treated mice, and cyclophosphamide treated mice with M30 supplement.
RESULTS: The top genes namely Tnfrsf19, Ercc2, Lama5, Ctsl, and Per1 were identified by microarray analysis. These genes were found to be involved in the biological processes of hair cycle, hair cycle phase, hair cycle process, hair follicle development, hair follicle maturation, hair follicle morphogenesis, regulation of hair cycle.
CONCLUSION: Our study demonstrates that M30 treatment is a promising therapy for cyclophosphamide-induced alopecia and suggests that the top five genes have unique preventive effects in cyclophosphamide-induced transformation.
Werter IM, Huijts CM, Lougheed SM, et al.
Metronomic cyclophosphamide attenuates mTOR-mediated expansion of regulatory T cells, but does not impact clinical outcome in patients with metastatic renal cell cancer treated with everolimus.
Cancer Immunol Immunother. 2019; 68(5):787-798 [PubMed] Related Publications
Metronomic cyclophosphamide attenuates mTOR-mediated expansion of regulatory T cells, but does not impact clinical outcome in patients with metastatic renal cell cancer treated with everolimus.
Cancer Immunol Immunother. 2019; 68(5):787-798 [PubMed] Related Publications
INTRODUCTION: Metastatic renal cell cancer (mRCC) patients have a median overall survival (mOS) of approximately 28 months. Until recently, mammalian target of rapamycin (mTOR) inhibition with everolimus was the standard second-line treatment regimen for mRCC patients, improving median progression-free survival (mPFS). Treatment with everolimus supports the expansion of immunosuppressive regulatory T cells (Tregs), which exert a negative effect on antitumor immune responses. In a phase 1 dose-escalation study, we have recently demonstrated that a low dose of 50 mg oral cyclophosphamide once daily can be safely combined with everolimus in mRCC patients and prevents the everolimus-induced increase in Tregs.
MATERIALS AND METHODS: In a multicenter phase 2 study, performed in patients with mRCC not amenable to or progressive on a vascular endothelial growth factor (VEGF)-receptor tyrosine kinase inhibitor (TKI) containing treatment regimen, we assessed whether the addition of this metronomic dosing schedule of cyclophosphamide to therapy with everolimus could result in an improvement of progression-free survival (PFS) after 4 months of treatment.
RESULTS: Though results from this study confirmed that combination treatment effectively lowered circulating levels of Tregs, addition of cyclophosphamide did not improve the PFS rate at 4 months. For this reason, the study was abrogated at the predefined interim analysis.
CONCLUSION: Although the comprehensive immunomonitoring analysis performed in this study provides relevant information for the design of future immunotherapeutic approaches, the addition of metronomic cyclophosphamide to mRCC patients receiving everolimus cannot be recommended.
MATERIALS AND METHODS: In a multicenter phase 2 study, performed in patients with mRCC not amenable to or progressive on a vascular endothelial growth factor (VEGF)-receptor tyrosine kinase inhibitor (TKI) containing treatment regimen, we assessed whether the addition of this metronomic dosing schedule of cyclophosphamide to therapy with everolimus could result in an improvement of progression-free survival (PFS) after 4 months of treatment.
RESULTS: Though results from this study confirmed that combination treatment effectively lowered circulating levels of Tregs, addition of cyclophosphamide did not improve the PFS rate at 4 months. For this reason, the study was abrogated at the predefined interim analysis.
CONCLUSION: Although the comprehensive immunomonitoring analysis performed in this study provides relevant information for the design of future immunotherapeutic approaches, the addition of metronomic cyclophosphamide to mRCC patients receiving everolimus cannot be recommended.
Zhao YR, Song HM, Ni L
Cyclophosphamide for the treatment of acute lymphoblastic leukemia: A protocol for systematic review.
Medicine (Baltimore). 2019; 98(5):e14293 [PubMed] Article available free on PMC after 01/03/2020 Related Publications
Cyclophosphamide for the treatment of acute lymphoblastic leukemia: A protocol for systematic review.
Medicine (Baltimore). 2019; 98(5):e14293 [PubMed] Article available free on PMC after 01/03/2020 Related Publications
BACKGROUND: Previous clinical trials have reported that cyclophosphamide can be used for the treatment of acute lymphoblastic leukemia (ALL). However, its efficacy is still unclear. In this systematic review study, we aim to evaluate its efficacy and safety for ALL.
METHODS: The following 9 databases will be searched from their inception to the present: Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE, MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Allied and Complementary Medicine Database (AMED), and four Chinese databases. The randomized controlled trials or case control studies of cyclophosphamide that assess the clinical efficacy and safety in patients with ALL are included. The methodological quality of all eligible included studies will be assessed by the Cochrane risk of bias tool.The primary outcome measurement will be all-cause mortality at the period of treatment and follow-up. The secondary outcome measurements will include the health-related quality of life (HRQL), postinduction complete remission (CR) rate, event-free survival (EFS), relapse rate, and adverse events. Two authors will independently select eligible studies, exact data, and assess the methodological quality of included studies. RevMan 5.3 software will be used to synthesize the data. Reporting bias will be evaluated by the funnel plots, Begg, and Egger tests.
RESULTS: This systematic review will evaluate the clinical efficacy and safety of cyclophosphamide for ALL.
DISSEMINATION AND ETHICS: The findings of this review will summarize the present evidence of cyclophosphamide for ALL, and may provide guidance for clinical practice of cyclophosphamide for ALL. Its results will be published through peer-reviewed journals. This study does not need ethic approval, because it will not involve the individual data.
SYSTEMATIC REVIEW REGISTRATION: PROSPERO CRD42018119333.
METHODS: The following 9 databases will be searched from their inception to the present: Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE, MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Allied and Complementary Medicine Database (AMED), and four Chinese databases. The randomized controlled trials or case control studies of cyclophosphamide that assess the clinical efficacy and safety in patients with ALL are included. The methodological quality of all eligible included studies will be assessed by the Cochrane risk of bias tool.The primary outcome measurement will be all-cause mortality at the period of treatment and follow-up. The secondary outcome measurements will include the health-related quality of life (HRQL), postinduction complete remission (CR) rate, event-free survival (EFS), relapse rate, and adverse events. Two authors will independently select eligible studies, exact data, and assess the methodological quality of included studies. RevMan 5.3 software will be used to synthesize the data. Reporting bias will be evaluated by the funnel plots, Begg, and Egger tests.
RESULTS: This systematic review will evaluate the clinical efficacy and safety of cyclophosphamide for ALL.
DISSEMINATION AND ETHICS: The findings of this review will summarize the present evidence of cyclophosphamide for ALL, and may provide guidance for clinical practice of cyclophosphamide for ALL. Its results will be published through peer-reviewed journals. This study does not need ethic approval, because it will not involve the individual data.
SYSTEMATIC REVIEW REGISTRATION: PROSPERO CRD42018119333.
Gusdon AM, Malani R, Chen X
Clinical and EEG Characteristics of Ifosfamide-Related Encephalopathy.
J Clin Neurophysiol. 2019; 36(2):150-154 [PubMed] Related Publications
Clinical and EEG Characteristics of Ifosfamide-Related Encephalopathy.
J Clin Neurophysiol. 2019; 36(2):150-154 [PubMed] Related Publications
PURPOSE: Ifosfamide can lead to a syndrome of central nervous system toxicity. Here, we investigate the clinical and EEG characteristics of patients with ifosfamide-related encephalopathy.
METHODS: Retrospective data were collected on patients from Memorial Sloan Kettering Cancer Center, who developed encephalopathy associated with ifosfamide between 2007 and 2017. Patients who had an EEG performed were included. Clinical and laboratory data were retrospectively collected. Each EEG recording was reviewed and compared with the originally documented EEG report.
RESULTS: Sixteen patients with ifosfamide-related encephalopathy were included, with primary tumors consisting of lymphoma (N = 9), sarcoma (N = 4), poorly differentiated ovarian cancer (N = 1), neuroblastoma (N = 1), and papillary serous adenocarcinoma (N = 1). Laboratory results ruled out other etiologies of encephalopathy. Generalized periodic discharges with or without triphasic morphology were seen most commonly (N = 9), with a distinct pattern of interspersed intermittent background attenuation seen in five patients. Background slowing and intermittent rhythmic delta activity (N = 4), bursts of bilateral synchronized delta activity (N = 2), and frontal predominant intermittent delta activity (N = 1) were also seen. One patient demonstrated a pattern consistent with nonconvulsive status epilepticus. Although most patients experienced resolution of symptoms, those who died demonstrated a variety of EEG abnormalities. Abnormal movements were common, with six patients demonstrating characteristic orofacial myoclonus.
CONCLUSIONS: Ifosfamide-related encephalopathy commonly results in a distinct pattern of generalized periodic discharges admixed with intermittent background attenuation on EEG. Abnormal movements, in particular orofacial myoclonus, are also common. Recognizing these clinical and EEG features might lead to early detection of ifosfamide-related encephalopathy.
METHODS: Retrospective data were collected on patients from Memorial Sloan Kettering Cancer Center, who developed encephalopathy associated with ifosfamide between 2007 and 2017. Patients who had an EEG performed were included. Clinical and laboratory data were retrospectively collected. Each EEG recording was reviewed and compared with the originally documented EEG report.
RESULTS: Sixteen patients with ifosfamide-related encephalopathy were included, with primary tumors consisting of lymphoma (N = 9), sarcoma (N = 4), poorly differentiated ovarian cancer (N = 1), neuroblastoma (N = 1), and papillary serous adenocarcinoma (N = 1). Laboratory results ruled out other etiologies of encephalopathy. Generalized periodic discharges with or without triphasic morphology were seen most commonly (N = 9), with a distinct pattern of interspersed intermittent background attenuation seen in five patients. Background slowing and intermittent rhythmic delta activity (N = 4), bursts of bilateral synchronized delta activity (N = 2), and frontal predominant intermittent delta activity (N = 1) were also seen. One patient demonstrated a pattern consistent with nonconvulsive status epilepticus. Although most patients experienced resolution of symptoms, those who died demonstrated a variety of EEG abnormalities. Abnormal movements were common, with six patients demonstrating characteristic orofacial myoclonus.
CONCLUSIONS: Ifosfamide-related encephalopathy commonly results in a distinct pattern of generalized periodic discharges admixed with intermittent background attenuation on EEG. Abnormal movements, in particular orofacial myoclonus, are also common. Recognizing these clinical and EEG features might lead to early detection of ifosfamide-related encephalopathy.
Huijts CM, Lougheed SM, Bodalal Z, et al.
The effect of everolimus and low-dose cyclophosphamide on immune cell subsets in patients with metastatic renal cell carcinoma: results from a phase I clinical trial.
Cancer Immunol Immunother. 2019; 68(3):503-515 [PubMed] Article available free on PMC after 01/03/2020 Related Publications
The effect of everolimus and low-dose cyclophosphamide on immune cell subsets in patients with metastatic renal cell carcinoma: results from a phase I clinical trial.
Cancer Immunol Immunother. 2019; 68(3):503-515 [PubMed] Article available free on PMC after 01/03/2020 Related Publications
For the treatment of metastatic renal cell cancer several strategies are used among which the mTOR inhibitor everolimus. As mTOR plays an important role in the immune system, e.g., by controlling the expression of the transcription factor FoxP3 thereby regulating regulatory T cells (Tregs), it plays a key role in the balance between tolerance and inflammation. Previous reports showed stimulatory effects of mTOR inhibition on the expansion of Tregs, an effect that can be considered detrimental in terms of cancer control. Since metronomic cyclophosphamide (CTX) was shown to selectively deplete Tregs, a phase 1 clinical trial was conducted to comprehensively investigate the immune-modulating effects of several dosages and schedules of CTX in combination with the standard dose of everolimus, with the explicit aim to achieve selective Treg depletion. Our data show that 50 mg of CTX once daily and continuously administered, in combination with the standard dose of 10 mg everolimus once daily, not only results in depletion of Tregs, but also leads to a reduction in MDSC, a sustained level of the CD8
Ramirez DA, Collins KP, Aradi AE, et al.
Kinetics of Cyclophosphamide Metabolism in Humans, Dogs, Cats, and Mice and Relationship to Cytotoxic Activity and Pharmacokinetics.
Drug Metab Dispos. 2019; 47(3):257-268 [PubMed] Related Publications
Kinetics of Cyclophosphamide Metabolism in Humans, Dogs, Cats, and Mice and Relationship to Cytotoxic Activity and Pharmacokinetics.
Drug Metab Dispos. 2019; 47(3):257-268 [PubMed] Related Publications
Cyclophosphamide (CP), a prodrug that is enzymatically converted to the cytotoxic 4-hydroxycyclophosphamide (4OHCP) by hepatic enzymes, is commonly used in both human and veterinary medicine to treat cancers and modulate the immune system. We investigated the metabolism of CP in humans, dogs, cats, and mice using liver microsomes; apparent
Li H, Hu B, Guo Z, et al.
Correlation of UGT2B7 Polymorphism with Cardiotoxicity in Breast Cancer Patients Undergoing Epirubicin/Cyclophosphamide-Docetaxel Adjuvant Chemotherapy.
Yonsei Med J. 2019; 60(1):30-37 [PubMed] Article available free on PMC after 01/03/2020 Related Publications
Correlation of UGT2B7 Polymorphism with Cardiotoxicity in Breast Cancer Patients Undergoing Epirubicin/Cyclophosphamide-Docetaxel Adjuvant Chemotherapy.
Yonsei Med J. 2019; 60(1):30-37 [PubMed] Article available free on PMC after 01/03/2020 Related Publications
PURPOSE: The present study aimed to investigate correlations between uridine glucuronosyltransferase 2B7 (UGT2B7) -161 single nucleotide polymorphism C to T (C>T) and the occurrence of cardiotoxicity in Chinese breast cancer (BC) patients undergoing epirubicin/cyclophosphamide-docetaxel (EC-D) adjuvant chemotherapy.
MATERIALS AND METHODS: 427 BC patients who had underwent surgery were consecutively enrolled in this prospective cohort study. All patients were scheduled to receive EC-D adjuvant chemotherapy regimen, and they were divided into UGT2B7 -161 CC (n=141), UGT2B7 -161 CT (n=196), and UGT2B7 -161 TT (n=90) groups according to their genotypes. Polymerase chain reaction was performed for determination of UGT2B7 -161 genotypes. Cardiotoxicity was defined as an absolute decline in left ventricular ejection fraction (LVEF) of at least 10% points from baseline to a value less than 53%, heart failure, acute coronary artery syndrome, or fatal arrhythmia.
RESULTS: LVEF values were lower at cycle (C) 4, C8, 3 months after chemotherapy (M3), M6, M9, and M12 compared to C0 (all
CONCLUSION: A UGT2B7 -161 T allele serves as a potential biomarker for predicting a low occurrence of cardiotoxicity in BC patients undergoing EC-D adjuvant chemotherapy.
MATERIALS AND METHODS: 427 BC patients who had underwent surgery were consecutively enrolled in this prospective cohort study. All patients were scheduled to receive EC-D adjuvant chemotherapy regimen, and they were divided into UGT2B7 -161 CC (n=141), UGT2B7 -161 CT (n=196), and UGT2B7 -161 TT (n=90) groups according to their genotypes. Polymerase chain reaction was performed for determination of UGT2B7 -161 genotypes. Cardiotoxicity was defined as an absolute decline in left ventricular ejection fraction (LVEF) of at least 10% points from baseline to a value less than 53%, heart failure, acute coronary artery syndrome, or fatal arrhythmia.
RESULTS: LVEF values were lower at cycle (C) 4, C8, 3 months after chemotherapy (M3), M6, M9, and M12 compared to C0 (all
CONCLUSION: A UGT2B7 -161 T allele serves as a potential biomarker for predicting a low occurrence of cardiotoxicity in BC patients undergoing EC-D adjuvant chemotherapy.
Iqubal A, Iqubal MK, Sharma S, et al.
Molecular mechanism involved in cyclophosphamide-induced cardiotoxicity: Old drug with a new vision.
Life Sci. 2019; 218:112-131 [PubMed] Related Publications
Molecular mechanism involved in cyclophosphamide-induced cardiotoxicity: Old drug with a new vision.
Life Sci. 2019; 218:112-131 [PubMed] Related Publications
Cyclophosphamide (CP) is an important anticancer drug which belongs to the class of alkylating agent. Cyclophosphamide is mostly used in bone marrow transplantation, rheumatoid arthritis, lupus erythematosus, multiple sclerosis, neuroblastoma and other types of cancer. Dose-related cardiotoxicity is a limiting factor for its use. CP-induced cardiotoxicity ranges from 7 to 28% and mortality ranges from 11 to 43% at the therapeutic dose of 170-180 mg/kg, i.v. CP undergoes hepatic metabolism that results in the production of aldophosphamide. Aldophosphamide decomposes into phosphoramide mustard & acrolein. Phosphoramide is an active neoplastic agent, and acrolein is a toxic metabolite which acts on the myocardium and endothelial cells. This is the first review article that talks about cyclophosphamide-induced cardiotoxicity and the different signaling pathways involved in its pathogenicity. Based on the available literature, CP is accountable for cardiomyocytes energy pool alteration by affecting the heart fatty acid binding proteins (H-FABP). CP has been found associated with cardiomyocytes apoptosis, inflammation, endothelial dysfunction, calcium dysregulation, endoplasmic reticulum damage, and mitochondrial damage. Molecular mechanism of cardiotoxicity has been discussed in detail through crosstalk of Nrf2/ARE, Akt/GSK-3β/NFAT/calcineurin, p53/p38MAPK, NF-kB/TLR-4, and Phospholamban/SERCA-2a signaling pathway. Based on the available literature we support the fact that metabolites of CP are responsible for cardiotoxicity due to depletion of antioxidants/ATP level, altered contractility, damaged endothelium and enhanced pro-inflammatory/pro-apoptotic activities resulting into cardiomyopathy, myocardial infarction, and heart failure. Dose adjustment, elimination/excretion of acrolein and maintenance of endogenous antioxidant pool could be the therapeutic approach to mitigate the toxicities.
Nanni O, Amadori D, De Censi A, et al.
Metformin plus chemotherapy versus chemotherapy alone in the first-line treatment of HER2-negative metastatic breast cancer. The MYME randomized, phase 2 clinical trial.
Breast Cancer Res Treat. 2019; 174(2):433-442 [PubMed] Related Publications
Metformin plus chemotherapy versus chemotherapy alone in the first-line treatment of HER2-negative metastatic breast cancer. The MYME randomized, phase 2 clinical trial.
Breast Cancer Res Treat. 2019; 174(2):433-442 [PubMed] Related Publications
PURPOSE: To investigate the efficacy of metformin (M) plus chemotherapy versus chemotherapy alone in metastatic breast cancer (MBC).
METHODS: Non-diabetic women with HER2-negative MBC were randomized to receive non-pegylated liposomal doxorubicin (NPLD) 60 mg/m
RESULTS: One-hundred-twenty-two patients were evaluable for PFS. At a median follow-up of 39.6 months (interquartile range [IQR] 24.6-50.7 months), 112 PFS events and 71 deaths have been registered. Median PFS was 9.4 months (95% CI 7.8-10.4) in arm A and 9.9 (95% CI 7.4-11.5) in arm B (P = 0.651). In patients with HOMA index < 2.5, median PFS was 10.4 months (95% CI 9.6-11.7) versus 8.5 (95% CI 5.8-9.7) in those with HOMA index ≥ 2.5 (P = 0.034). Grade 3/4 neutropenia was the most common toxicity, occurring in 54.4% of arm A patients and 72.3% of the arm B group (P = 0.019). M induced diarrhea (G2) was observed in 8.8% of patients in Arm A. The effect of M was similar in patients with HOMA index < 2.5 and ≥ 2.5, for PFS and OS.
CONCLUSIONS: The MYME trial failed to provide evidence in support of an anticancer activity of M in combination with first line CT in MBC. A significantly shorter PFS was observed in insulin-resistant patients (HOMA ≥ 2.5). Noteworthy, M had a significant effect on CT induced severe neutropenia. Further development of M in combination with CT in the setting of MBC is not warranted.
METHODS: Non-diabetic women with HER2-negative MBC were randomized to receive non-pegylated liposomal doxorubicin (NPLD) 60 mg/m
RESULTS: One-hundred-twenty-two patients were evaluable for PFS. At a median follow-up of 39.6 months (interquartile range [IQR] 24.6-50.7 months), 112 PFS events and 71 deaths have been registered. Median PFS was 9.4 months (95% CI 7.8-10.4) in arm A and 9.9 (95% CI 7.4-11.5) in arm B (P = 0.651). In patients with HOMA index < 2.5, median PFS was 10.4 months (95% CI 9.6-11.7) versus 8.5 (95% CI 5.8-9.7) in those with HOMA index ≥ 2.5 (P = 0.034). Grade 3/4 neutropenia was the most common toxicity, occurring in 54.4% of arm A patients and 72.3% of the arm B group (P = 0.019). M induced diarrhea (G2) was observed in 8.8% of patients in Arm A. The effect of M was similar in patients with HOMA index < 2.5 and ≥ 2.5, for PFS and OS.
CONCLUSIONS: The MYME trial failed to provide evidence in support of an anticancer activity of M in combination with first line CT in MBC. A significantly shorter PFS was observed in insulin-resistant patients (HOMA ≥ 2.5). Noteworthy, M had a significant effect on CT induced severe neutropenia. Further development of M in combination with CT in the setting of MBC is not warranted.
Ito T, Koyama S, Iwamoto S, et al.
Acquired Platythorax, or Anteroposterior Flattening of the Chest Wall, as a Late Complication of Cyclophosphamide Treatment for Childhood Acute Lymphoblastic Leukemia, Presenting in a Young Man with Respiratory Failure.
Am J Case Rep. 2018; 19:1317-1323 [PubMed] Article available free on PMC after 01/03/2020 Related Publications
Acquired Platythorax, or Anteroposterior Flattening of the Chest Wall, as a Late Complication of Cyclophosphamide Treatment for Childhood Acute Lymphoblastic Leukemia, Presenting in a Young Man with Respiratory Failure.
Am J Case Rep. 2018; 19:1317-1323 [PubMed] Article available free on PMC after 01/03/2020 Related Publications
BACKGROUND Acquired platythorax, or flattening of the chest with a reduction in the anteroposterior (AP) diameter, is very rare and the prognosis depends on the degree of the deformity, respiratory function, and on any underlying disease. Drug-induced pulmonary fibrosis is associated with pulmonary hypoplasia. A case of acquired platythorax is presented in a young man previously treated with cyclophosphamide in childhood. CASE REPORT A 20-year-old man began to experience cough, chest pain, and mild exertional dyspnea. He was admitted to the hospital at 23 years of age with respiratory failure. Chest imaging showed pleural thickening and platythorax. He had been successfully treated for acute lymphoblastic leukemia (ALL), at 3 years of age, with chemotherapy that included a cumulative dose of cyclophosphamide of 15.6 g/m². His ALL relapsed six years later and he was the treated again with cyclophosphamide and underwent a second and complete remission. A clinical diagnosis of late-onset cyclophosphamide-induced lung disease with progressive platythorax was made on the basis of his clinical history and on imaging findings of the ratio of the AP to lateral chest wall diameter when compared with age-matched controls. Despite continued remission of his ALL, he died of progressive cardiopulmonary failure at 25 years of age. CONCLUSIONS This report described a rare case of acquired platythorax, or flattening of the chest, in a young adult. The use of the ratio of the chest wall AP diameter to lateral diameter may be used in the early detection of this rare chemotherapy-induced complication in children and adults.
Chen F, Li X, Wang J, et al.
Combination of Ginsenoside H dripping pills and cyclophosphamide improve paraneoplastic syndrome and inhibit postoperative recurrence via the reversion of Th1/Th2 shift.
Biomed Pharmacother. 2018; 108:865-875 [PubMed] Related Publications
Combination of Ginsenoside H dripping pills and cyclophosphamide improve paraneoplastic syndrome and inhibit postoperative recurrence via the reversion of Th1/Th2 shift.
Biomed Pharmacother. 2018; 108:865-875 [PubMed] Related Publications
Non-small-cell lung cancer (NSCLC) is recognized as the most common malignant disease worldwide and combination treatment is recommended as its first line therapy. As a Ph2 clinical product, Ginsenoside H dripping pills (GH) is proposed as an adjuvant of chemotherapy. In the present study, we utilized a postoperative model to evaluate the efficacy of GH on the functions of anti-recurrence and improvement of life quality when combined with chemotherapeutic drug cyclophosphamide (CTX). Specifically, the anti-recurrence effect was evaluated by tumor inhibiting rate and the improvement of life quality was evaluated by the remission of splenomegaly and emaciation. The underlying mechanisms were explored via quantitative real time-PCR, Elisa and IHC staining. Results showed that GH had a synergy when combined with CTX against tumor recurrence, significantly improved the life quality of postoperative patients via remitting splenomegaly and emaciation. H&E staining showed that GH could increase the number of splenic T cells, which were inhibited after CTX administration. Furthermore, the reversion of Th1/Th2 shift, which had been verified by different methods, may account for one of the mechanisms of the synergy. All these results indicated Ginsenoside H dripping pills as a promising adjuvant for postoperative chemotherapy of NSCLC.
Munster P, Krop IE, LoRusso P, et al.
Safety and pharmacokinetics of MM-302, a HER2-targeted antibody-liposomal doxorubicin conjugate, in patients with advanced HER2-positive breast cancer: a phase 1 dose-escalation study.
Br J Cancer. 2018; 119(9):1086-1093 [PubMed] Article available free on PMC after 30/10/2019 Related Publications
Safety and pharmacokinetics of MM-302, a HER2-targeted antibody-liposomal doxorubicin conjugate, in patients with advanced HER2-positive breast cancer: a phase 1 dose-escalation study.
Br J Cancer. 2018; 119(9):1086-1093 [PubMed] Article available free on PMC after 30/10/2019 Related Publications
BACKGROUND: This phase 1 dose-escalation trial studied MM-302, a novel HER2-targeted PEGylated antibody-liposomal doxorubicin conjugate, in HER2-positive locally advanced/metastatic breast cancer.
METHODS: Patients were enrolled in four cohorts: MM-302 monotherapy (8, 16, 30, 40, and 50 mg/m
RESULTS: Sixty-nine patients were treated. The most common adverse events (AEs) were fatigue and nausea. Grade 3/4 AEs of special interest included neutropenia, fatigue, mucosal inflammation, anemia, thrombocytopenia, febrile neutropenia, and palmar-plantar erythrodysesthesia. The MTD was not reached. With MM-302 ≥ 30 mg/m
CONCLUSION: MM-302 monotherapy, in combination with trastuzumab, or trastuzumab plus cyclophosphamide, was well tolerated and showed promising efficacy. The selected phase 2 MM-302 dose was 30 mg/m
METHODS: Patients were enrolled in four cohorts: MM-302 monotherapy (8, 16, 30, 40, and 50 mg/m
RESULTS: Sixty-nine patients were treated. The most common adverse events (AEs) were fatigue and nausea. Grade 3/4 AEs of special interest included neutropenia, fatigue, mucosal inflammation, anemia, thrombocytopenia, febrile neutropenia, and palmar-plantar erythrodysesthesia. The MTD was not reached. With MM-302 ≥ 30 mg/m
CONCLUSION: MM-302 monotherapy, in combination with trastuzumab, or trastuzumab plus cyclophosphamide, was well tolerated and showed promising efficacy. The selected phase 2 MM-302 dose was 30 mg/m
Schelker RC, Herr W, Reichle A, Vogelhuber M
Low-dose trofosfamide plus rituximab is an effective and safe treatment for diffuse large B-cell lymphoma of the elderly: a single center experience.
BMC Cancer. 2018; 18(1):1000 [PubMed] Article available free on PMC after 30/10/2019 Related Publications
Low-dose trofosfamide plus rituximab is an effective and safe treatment for diffuse large B-cell lymphoma of the elderly: a single center experience.
BMC Cancer. 2018; 18(1):1000 [PubMed] Article available free on PMC after 30/10/2019 Related Publications
BACKGROUND: Rituximab plus combination chemotherapy with cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) is broadly accepted as standard for the treatment of diffuse large B-cell lymphoma (DLBCL). Nevertheless, there is sparsely data concerning the management of elderly patients.
METHODS: We performed a retrospective study of treatment with rituximab and low-dose trofosfamide in elderly patients (≥ 75 years) with DLBCL who were not suitable for R-CHOP or R-CHOP-like regimens or who did not consent to aggressive treatment. The choice regarding the qualification for R-CHOP or R-CHOP-like regimen was left to the estimation of the treating physicians.
RESULTS: Eleven patients with a median age of 83 years (range, 75-90 years) were included. The age-adjusted international prognostic index was low risk in one patient, low-intermediate in four patients, high-intermediate in three patients, and high risk in 3 patients. All patients were evaluable for response. Five patients (45%) achieved a complete response, three (27%) a partial response, one (9%) stable disease, and two (18%) progressive disease. The estimated 1-yr overall survival was 54.5%, and the estimated 1-yr progression-free survival 45.5%, however, three patients (27%) were alive without evidence of disease at 16-20 months from start of treatment. Main toxicity was leukopenia (36% grade III or IV), whereas grade III/IV non-hematological adverse events did not occur.
CONCLUSIONS: Due to its potency and low toxicity, trofosfamide/rituximab might represent an alternative therapy for DLBCL of elderly patients not suitable for R-CHOP. This observation, however, should be confirmed in a larger patient population within a prospective clinical trial.
METHODS: We performed a retrospective study of treatment with rituximab and low-dose trofosfamide in elderly patients (≥ 75 years) with DLBCL who were not suitable for R-CHOP or R-CHOP-like regimens or who did not consent to aggressive treatment. The choice regarding the qualification for R-CHOP or R-CHOP-like regimen was left to the estimation of the treating physicians.
RESULTS: Eleven patients with a median age of 83 years (range, 75-90 years) were included. The age-adjusted international prognostic index was low risk in one patient, low-intermediate in four patients, high-intermediate in three patients, and high risk in 3 patients. All patients were evaluable for response. Five patients (45%) achieved a complete response, three (27%) a partial response, one (9%) stable disease, and two (18%) progressive disease. The estimated 1-yr overall survival was 54.5%, and the estimated 1-yr progression-free survival 45.5%, however, three patients (27%) were alive without evidence of disease at 16-20 months from start of treatment. Main toxicity was leukopenia (36% grade III or IV), whereas grade III/IV non-hematological adverse events did not occur.
CONCLUSIONS: Due to its potency and low toxicity, trofosfamide/rituximab might represent an alternative therapy for DLBCL of elderly patients not suitable for R-CHOP. This observation, however, should be confirmed in a larger patient population within a prospective clinical trial.
Ding W, Li Z, Wang C, et al.
Anthracycline versus nonanthracycline adjuvant therapy for early breast cancer: A systematic review and meta-analysis.
Medicine (Baltimore). 2018; 97(42):e12908 [PubMed] Article available free on PMC after 30/10/2019 Related Publications
Anthracycline versus nonanthracycline adjuvant therapy for early breast cancer: A systematic review and meta-analysis.
Medicine (Baltimore). 2018; 97(42):e12908 [PubMed] Article available free on PMC after 30/10/2019 Related Publications
PURPOSE: The clinical benefits provided by using anthracycline-contained regimens in patients with early breast cancer (EBC) remain uncertain. This meta-analysis used data from all relevant trials to compare treatment outcomes for patients with EBC receiving adjuvant chemotherapy with non-anthracycline-contained regimens or anthracycline-contained regimens.
PATIENTS AND METHODS: Individual patient data were collected on 7 randomized trials comparing non-anthracycline-contained regimens with anthracycline-contained regimens, a total of 14,451 women were analyzed. The hazard ratios (HR) of disease-free survival (DFS) and overall survival (OS), and the risk ratios for grades 3 to 4 toxicities were extracted from the retrieved studies and analyzed using various statistical methods. A pooled analysis was accomplished and HR with 95% confidence intervals (95% CIs) was derived. The significant differences in DFS and OS were explored. A heterogeneity test was applied as well.
RESULTS: Among 7 eligible trials, significant differences in favor of anthracycline-contained regimens were seen in DFS (HR: 0.86; 95% CI: 0.78-0.95; P = .003) and in OS (HR: 0.85; 95% CI: 0.75-0.97; P = .01). Subgroup analyses of DFS showed similar treatment effects by hormone-receptor status and nodal status, but differential effects by human epidermal growth factor receptor 2 status, menopausal status, and malignancy grade. Sensitive analysis showed that the DFS of taxanes and cyclophosphamide (TC) was noninferior to anthracycline-contained regiments.
CONCLUSION: Despite failing to show noninferior to the anthracycline-contained regimens in patients with EBC, it provides evidence that both regimens significantly improved the DFS and OS, and TC regimen may be noninferior to anthracycline-contained regimens.
PATIENTS AND METHODS: Individual patient data were collected on 7 randomized trials comparing non-anthracycline-contained regimens with anthracycline-contained regimens, a total of 14,451 women were analyzed. The hazard ratios (HR) of disease-free survival (DFS) and overall survival (OS), and the risk ratios for grades 3 to 4 toxicities were extracted from the retrieved studies and analyzed using various statistical methods. A pooled analysis was accomplished and HR with 95% confidence intervals (95% CIs) was derived. The significant differences in DFS and OS were explored. A heterogeneity test was applied as well.
RESULTS: Among 7 eligible trials, significant differences in favor of anthracycline-contained regimens were seen in DFS (HR: 0.86; 95% CI: 0.78-0.95; P = .003) and in OS (HR: 0.85; 95% CI: 0.75-0.97; P = .01). Subgroup analyses of DFS showed similar treatment effects by hormone-receptor status and nodal status, but differential effects by human epidermal growth factor receptor 2 status, menopausal status, and malignancy grade. Sensitive analysis showed that the DFS of taxanes and cyclophosphamide (TC) was noninferior to anthracycline-contained regiments.
CONCLUSION: Despite failing to show noninferior to the anthracycline-contained regimens in patients with EBC, it provides evidence that both regimens significantly improved the DFS and OS, and TC regimen may be noninferior to anthracycline-contained regimens.
Witte HM, Riecke A, Mayer T, et al.
Trofosfamide in the treatment of elderly or frail patients with diffuse large B-cell lymphoma.
J Cancer Res Clin Oncol. 2019; 145(1):129-136 [PubMed] Related Publications
Trofosfamide in the treatment of elderly or frail patients with diffuse large B-cell lymphoma.
J Cancer Res Clin Oncol. 2019; 145(1):129-136 [PubMed] Related Publications
PURPOSE: The introduction of immunochemotherapy has led to a significant improvement in treatment results and prognosis of diffuse large B-cell non-Hodgkins lymphoma (DLBCL) both at initial diagnosis and in relapse. Trofosfamide, an oxazaphosphorine derivative, has been utilized as alternative treatment option for patients with lymphoproliferative diseases unsuitable for conventional chemotherapy agents and protocols because of age, comorbidity, or poor performance score. While data on the activity and safety of single-agent trofosfamide have been published, the potential value of this agent in immunochemotherapy in combination with anti-CD20 antibodies such as rituximab has not been investigated to our knowledge.
METHODS: Safety and therapeutic effectiveness of trofosfamide given orally at a dose of 50 mg twice daily alone, or in combination with standard-dose rituximab, was investigated in a cohort of elderly and/or highly comorbid patients with histologically confirmed primary or secondary DLBCL.
RESULTS: Treatment with trofosfamide in this combination setting was generally well tolerated with no treatment-related deaths and manageable side effects, most of which were WHO class I-II; the most clinically relevant toxicity was cytopenia. 19 of 21 examined patients responded to therapy with 11 of 21 (52.4%) achieving a complete remission (CR). Median overall and progression-free survival (OS and PFS) in the CR-group was 14 and 9 months, respectively. In the subgroup with trofosfamide-based first-line therapy, 7 of 10 (70%) achieved CR and median PFS was not reached.
CONCLUSIONS: Immunochemotherapy with rituximab and trofosfamide (RT) is safe and effective in elderly and poor-performance patients with DLBCL. Response rates are comparable to most commonly used primary and salvage treatment protocols. The potential value of TR regimen in both first-line and relapsed/refractory DLCBL merits further investigation and is probably underestimated.
METHODS: Safety and therapeutic effectiveness of trofosfamide given orally at a dose of 50 mg twice daily alone, or in combination with standard-dose rituximab, was investigated in a cohort of elderly and/or highly comorbid patients with histologically confirmed primary or secondary DLBCL.
RESULTS: Treatment with trofosfamide in this combination setting was generally well tolerated with no treatment-related deaths and manageable side effects, most of which were WHO class I-II; the most clinically relevant toxicity was cytopenia. 19 of 21 examined patients responded to therapy with 11 of 21 (52.4%) achieving a complete remission (CR). Median overall and progression-free survival (OS and PFS) in the CR-group was 14 and 9 months, respectively. In the subgroup with trofosfamide-based first-line therapy, 7 of 10 (70%) achieved CR and median PFS was not reached.
CONCLUSIONS: Immunochemotherapy with rituximab and trofosfamide (RT) is safe and effective in elderly and poor-performance patients with DLBCL. Response rates are comparable to most commonly used primary and salvage treatment protocols. The potential value of TR regimen in both first-line and relapsed/refractory DLCBL merits further investigation and is probably underestimated.
Hamidieh AA, Eslami Shahre Babaki A, Rostami T, et al.
A Single-Center Experience With Hematopoietic Stem Cell Transplantation for Pediatric Acute Lymphoblastic Leukemia: A Modest Pitch for Non-Total Body Irradiation Conditioning Regimens.
Exp Clin Transplant. 2019; 17(2):243-250 [PubMed] Related Publications
A Single-Center Experience With Hematopoietic Stem Cell Transplantation for Pediatric Acute Lymphoblastic Leukemia: A Modest Pitch for Non-Total Body Irradiation Conditioning Regimens.
Exp Clin Transplant. 2019; 17(2):243-250 [PubMed] Related Publications
OBJECTIVES: Allogeneic hematopoietic stem cell transplantation has been used for several decades to treat patients with acute lymphoblastic leukemia. Total body irradiation has been promoted as an important component of conditioning regimens for this process; however, recent reports of chemotherapy-based conditioning regimens have shown comparable outcomes.
MATERIALS AND METHODS: We report our experience with radiation-free conditioning using busulfan and cyclophosphamide in 127 pediatric patients with acute lymphoblastic leukemia who were treated between 1997 and 2014. The median age was 11 years (range, < 1 to 15 y), 70% of patients were male, 81.1% received transplants from HLA-matched siblings, 83% received peripheral blood stem cells, 41% were in second complete remission at the time of transplant, and 83% had B-lineage immunophenotype.
RESULTS: In patients who were in complete remission at the time of transplant, 5-year overall survival, leukemia-free survival, and relapse rates were 62.48% (95% confidence interval, 52.29-71.09%), 49.43% (95% confidence interval, 39.57-58.53%), and 45.64% (95% confidence interval, 35.85-54.88%), respectively. We observed significant differences between outcomes in patients by time of transplant, presence of chronic graft-versus-host disease, and remission status.
CONCLUSIONS: Our relapse rates were comparable to those shown in recent studies, although the transplant-related mortality rate was lower. The results of our study showed that a busulfan/cyclophosphamide conditioning regimen has acceptable outcomes without the undesirable adverse effects of total body irradiation, particularly in pediatric patients. Large multicenter studies are needed to assess less toxic conditioning regimens with fewer adverse effects in these patients.
MATERIALS AND METHODS: We report our experience with radiation-free conditioning using busulfan and cyclophosphamide in 127 pediatric patients with acute lymphoblastic leukemia who were treated between 1997 and 2014. The median age was 11 years (range, < 1 to 15 y), 70% of patients were male, 81.1% received transplants from HLA-matched siblings, 83% received peripheral blood stem cells, 41% were in second complete remission at the time of transplant, and 83% had B-lineage immunophenotype.
RESULTS: In patients who were in complete remission at the time of transplant, 5-year overall survival, leukemia-free survival, and relapse rates were 62.48% (95% confidence interval, 52.29-71.09%), 49.43% (95% confidence interval, 39.57-58.53%), and 45.64% (95% confidence interval, 35.85-54.88%), respectively. We observed significant differences between outcomes in patients by time of transplant, presence of chronic graft-versus-host disease, and remission status.
CONCLUSIONS: Our relapse rates were comparable to those shown in recent studies, although the transplant-related mortality rate was lower. The results of our study showed that a busulfan/cyclophosphamide conditioning regimen has acceptable outcomes without the undesirable adverse effects of total body irradiation, particularly in pediatric patients. Large multicenter studies are needed to assess less toxic conditioning regimens with fewer adverse effects in these patients.
Souza CA, Simões R, Borges KBG, et al.
Arterial Stiffness Use for Early Monitoring of Cardiovascular Adverse Events due to Anthracycline Chemotherapy in Breast Cancer Patients. A Pilot Study.
Arq Bras Cardiol. 2018; 111(5):721-728 [PubMed] Article available free on PMC after 30/10/2019 Related Publications
Arterial Stiffness Use for Early Monitoring of Cardiovascular Adverse Events due to Anthracycline Chemotherapy in Breast Cancer Patients. A Pilot Study.
Arq Bras Cardiol. 2018; 111(5):721-728 [PubMed] Article available free on PMC after 30/10/2019 Related Publications
BACKGROUND: Chemotherapy with doxorubicin and cyclophosphamide, although efficient for treating breast cancer, is associated with cardiovascular complications. Recent studies seek to identify methods that can early detect cardiological and vascular changes as a strategy to decrease the incidence of cardiovascular comorbidities.
OBJECTIVE: To evaluate the role of arterial stiffness measurement in the monitoring of doxorubicin and cyclophosphamide-induced cardiotoxicity in breast cancer patients.
METHODS: Prospective longitudinal study in 24 breast cancer patients undergoing treatment with doxorubicin and cyclophosphamide. Patients underwent an indirect evaluation of arterial stiffness through non-invasive measurement of hemodynamic parameters such as pulse wave velocity with the Mobil-O-Graph® 24H PWA device at three different times of the chemotherapy treatment (pre-chemotherapy, after the first and the fourth cycle). The left ventricular ejection fraction was also evaluated by Doppler echocardiography (pre-chemotherapy and after the fourth chemotherapy cycle). Data were considered significant when p ≤ 0.05.
RESULTS: Patients had a mean age of 52.33 ± 8.85 years and body mass index of 31 ± 5.87 kg/m2. There was no significant difference between the hemodynamic parameters evaluated by the oscillometric method or in the left ventricular ejection fraction in the different evaluated periods.
CONCLUSION: Evaluations of arterial stiffness by oscillometry and measurement of left ventricular ejection fraction by Doppler echocardiography showed equivalence in the values found, suggesting that the evaluation method of arterial stiffness studied could be used as a marker for cardiovascular adverse events associated with doxorrubicin-based chemotherapy drugs.
OBJECTIVE: To evaluate the role of arterial stiffness measurement in the monitoring of doxorubicin and cyclophosphamide-induced cardiotoxicity in breast cancer patients.
METHODS: Prospective longitudinal study in 24 breast cancer patients undergoing treatment with doxorubicin and cyclophosphamide. Patients underwent an indirect evaluation of arterial stiffness through non-invasive measurement of hemodynamic parameters such as pulse wave velocity with the Mobil-O-Graph® 24H PWA device at three different times of the chemotherapy treatment (pre-chemotherapy, after the first and the fourth cycle). The left ventricular ejection fraction was also evaluated by Doppler echocardiography (pre-chemotherapy and after the fourth chemotherapy cycle). Data were considered significant when p ≤ 0.05.
RESULTS: Patients had a mean age of 52.33 ± 8.85 years and body mass index of 31 ± 5.87 kg/m2. There was no significant difference between the hemodynamic parameters evaluated by the oscillometric method or in the left ventricular ejection fraction in the different evaluated periods.
CONCLUSION: Evaluations of arterial stiffness by oscillometry and measurement of left ventricular ejection fraction by Doppler echocardiography showed equivalence in the values found, suggesting that the evaluation method of arterial stiffness studied could be used as a marker for cardiovascular adverse events associated with doxorrubicin-based chemotherapy drugs.
Campone M, Lacroix-Triki M, Roca L, et al.
UCBG 2-08: 5-year efficacy results from the UNICANCER-PACS08 randomised phase III trial of adjuvant treatment with FEC100 and then either docetaxel or ixabepilone in patients with early-stage, poor prognosis breast cancer.
Eur J Cancer. 2018; 103:184-194 [PubMed] Related Publications
UCBG 2-08: 5-year efficacy results from the UNICANCER-PACS08 randomised phase III trial of adjuvant treatment with FEC100 and then either docetaxel or ixabepilone in patients with early-stage, poor prognosis breast cancer.
Eur J Cancer. 2018; 103:184-194 [PubMed] Related Publications
PURPOSE: UNICANCER-PACS08 compared adjuvant FEC (5-FU; epirubicin; cyclophosphamide) then docetaxel to FEC then ixabepilone in poor prognosis early breast cancer (BC). We evaluated whether replacing docetaxel with ixabepilone would increase 5-year disease-free survival (DFS).
PATIENTS AND METHODS: Triple-negative breast cancer (TNBC) or oestrogen receptor (ER)+/progesterone receptor (PR)-/HER2- BC patients were randomised to receive standard FEC (3 cycles) followed by 3 cycles of either docetaxel (100 mg/m
RESULTS: Seven hundred sixty-two patients were enrolled between October 2007 and September 2010. Baseline characteristics were balanced between arms. Median follow-up was 66.7 months. Median DFS was not reached; 5-year DFS rate was 76% with docetaxel and 79% with ixabepilone (hazard ratio [HR] = 0.80; 95% confidence interval [CI] = 0.58-1.10; p = 0.175). Median overall survival (OS) was not reached; 5-year OS rate was 86% versus 84% (HR = 0.97; 95% CI = 0.66-1.42; p = 0.897). TNBC patients treated with ixabepilone had a 23% lower risk of relapse compared to docetaxel (HR for DFS = 0.77; 95% CI = 0.53-1.11; p = 0.168). DFS was longer with ixabepilone than docetaxel in patients with grade II-III lymphocytic infiltration (HR = 0.55; 95% CI = 0.29-1.05; p = 0.063). All patients experienced ≥1 adverse events (AEs): 75% reported grade III-IV AEs and two (<1%) had grade V AEs (both with neutropenia and infection receiving ixabepilone).
CONCLUSION: After adjuvant FEC, ixabepilone was comparable to docetaxel for treating poor prognosis early BC patients. The benefit of ixabepilone in subgroups (patients with TNBC and grade II-III lymphocytic infiltration) requires further evaluation.
PATIENTS AND METHODS: Triple-negative breast cancer (TNBC) or oestrogen receptor (ER)+/progesterone receptor (PR)-/HER2- BC patients were randomised to receive standard FEC (3 cycles) followed by 3 cycles of either docetaxel (100 mg/m
RESULTS: Seven hundred sixty-two patients were enrolled between October 2007 and September 2010. Baseline characteristics were balanced between arms. Median follow-up was 66.7 months. Median DFS was not reached; 5-year DFS rate was 76% with docetaxel and 79% with ixabepilone (hazard ratio [HR] = 0.80; 95% confidence interval [CI] = 0.58-1.10; p = 0.175). Median overall survival (OS) was not reached; 5-year OS rate was 86% versus 84% (HR = 0.97; 95% CI = 0.66-1.42; p = 0.897). TNBC patients treated with ixabepilone had a 23% lower risk of relapse compared to docetaxel (HR for DFS = 0.77; 95% CI = 0.53-1.11; p = 0.168). DFS was longer with ixabepilone than docetaxel in patients with grade II-III lymphocytic infiltration (HR = 0.55; 95% CI = 0.29-1.05; p = 0.063). All patients experienced ≥1 adverse events (AEs): 75% reported grade III-IV AEs and two (<1%) had grade V AEs (both with neutropenia and infection receiving ixabepilone).
CONCLUSION: After adjuvant FEC, ixabepilone was comparable to docetaxel for treating poor prognosis early BC patients. The benefit of ixabepilone in subgroups (patients with TNBC and grade II-III lymphocytic infiltration) requires further evaluation.
Schiavetti A, Pedetti V, Varrasso G, et al.
Long-term renal function and hypertension in adult survivors of childhood sarcoma: Single center experience.
Pediatr Hematol Oncol. 2018; 35(3):167-176 [PubMed] Related Publications
Long-term renal function and hypertension in adult survivors of childhood sarcoma: Single center experience.
Pediatr Hematol Oncol. 2018; 35(3):167-176 [PubMed] Related Publications
AIM: Little data is available on long-term renal impairment in survivors from childhood sarcoma. We investigated the prevalence of renal impairment and hypertension after very long-term follow-up in survivors who reached adulthood after treatment for childhood sarcoma.
METHODS: A cross-sectional single center study was performed. Outcomes included estimating glomerular filtration rate (eGFR), albuminuria, glycosuria, serum phosphate and magnesium, tubular reabsorption phosphate (TRP), chronic kidney disease (CKD) according to the "Kidney Disease: Improving Global Outcomes" (KDIGO) guidelines and blood pressure (BP).
RESULTS: Out of 87 > 5-year sarcoma survivors, 30 adults (10F/20M, median age at diagnosis 9 years, median age at investigation 26 years, median follow-up 16 years, mean 19 years) were identified. Renal impairment was detected in four cases (13.3%); three of these fulfilled the criteria for CKD. Among the adult survivors, a subgroup of 15 cases (50%) had received ifosfamide without confounding factors such as a diagnosis of genito-urinary rhabdomyosarcoma or administration of other potentially nephrotoxic chemotherapy (platinum-based drugs or methotrexate); no renal dysfunction was detected in this subgroup. In the whole cohort of sarcoma survivors, hypertension was diagnosed in four cases (13.3%); BP was significantly correlated with body mass index [p .014].
CONCLUSION: In our series of adult survivors treated for a diagnosis of sarcoma in their childhood, the prevalence of CKD was 10%. We found survivors treated with ifosfamide as the only nephrotoxic agent did not present glomerular or tubular toxicity at long term follow-up, but further studies including a larger number of cases are required to confirm it.
METHODS: A cross-sectional single center study was performed. Outcomes included estimating glomerular filtration rate (eGFR), albuminuria, glycosuria, serum phosphate and magnesium, tubular reabsorption phosphate (TRP), chronic kidney disease (CKD) according to the "Kidney Disease: Improving Global Outcomes" (KDIGO) guidelines and blood pressure (BP).
RESULTS: Out of 87 > 5-year sarcoma survivors, 30 adults (10F/20M, median age at diagnosis 9 years, median age at investigation 26 years, median follow-up 16 years, mean 19 years) were identified. Renal impairment was detected in four cases (13.3%); three of these fulfilled the criteria for CKD. Among the adult survivors, a subgroup of 15 cases (50%) had received ifosfamide without confounding factors such as a diagnosis of genito-urinary rhabdomyosarcoma or administration of other potentially nephrotoxic chemotherapy (platinum-based drugs or methotrexate); no renal dysfunction was detected in this subgroup. In the whole cohort of sarcoma survivors, hypertension was diagnosed in four cases (13.3%); BP was significantly correlated with body mass index [p .014].
CONCLUSION: In our series of adult survivors treated for a diagnosis of sarcoma in their childhood, the prevalence of CKD was 10%. We found survivors treated with ifosfamide as the only nephrotoxic agent did not present glomerular or tubular toxicity at long term follow-up, but further studies including a larger number of cases are required to confirm it.
Dabkara D, Ganguly S, Biswas B, Ghosh J
Metronomic therapy in metastatic castrate-resistant prostate cancer: Experience from a tertiary cancer care center.
Indian J Cancer. 2018 Jan-Mar; 55(1):94-97 [PubMed] Related Publications
Metronomic therapy in metastatic castrate-resistant prostate cancer: Experience from a tertiary cancer care center.
Indian J Cancer. 2018 Jan-Mar; 55(1):94-97 [PubMed] Related Publications
Background: Many agents have shown survival advantage in metastatic castrate-resistant prostate cancer (mCRPC). Despite this improvement, survival is poor, especially in subgroup of elderly patients who are not fit for cytotoxic chemotherapy.
Materials and Methods: This is a single-institutional data review of mCRPC treated between December 2012 and May 2016 with oral cyclophosphamide (50-100 mg/day) ± oral prednisolone. mCRPCs failed or not fit for docetaxel and/or abiraterone were included in this study. Monthly prostate-specific antigen (PSA) was monitored, and toxicity of cyclophosphamide was recorded. PSA response was defined as ≥50% reduction from precyclophosphamide value. The median follow-up was calculated from the day of starting cyclophosphamide and the last date of follow-up or death, whichever is later.
Results: Eighteen patients were included with a median age of 74.5 years (range: 59-83). The site of metastasis was bone in 15, bone and distant lymph nodes in 2, and rectum in 1 patient. The median duration of androgen deprivation was 21 months (range: 3-42.9 months). The median cyclophosphamide exposure was 2 months (range: 0.9-13.5 months) after a median follow-up of 5.8 months. Overall PSA response rate was 44%. The median PSA progression-free survival with cyclophosphamide was 4.7 months (range: 0.9-13.5 months). Five patients had durable PSA response of 9.9, 10.1, 10.5, 12.1, and 13.5 months, respectively. No Grade 3 or 4 toxicity was observed with cyclophosphamide.
Conclusion: Oral metronomic cyclophosphamide was found to be an effective and well-tolerated therapy in mCRPC after failure or not fit for docetaxel and/or abiraterone. In few patients, cyclophosphamide induced durable PSA response. This finding needs further evaluation in a prospective manner.
Materials and Methods: This is a single-institutional data review of mCRPC treated between December 2012 and May 2016 with oral cyclophosphamide (50-100 mg/day) ± oral prednisolone. mCRPCs failed or not fit for docetaxel and/or abiraterone were included in this study. Monthly prostate-specific antigen (PSA) was monitored, and toxicity of cyclophosphamide was recorded. PSA response was defined as ≥50% reduction from precyclophosphamide value. The median follow-up was calculated from the day of starting cyclophosphamide and the last date of follow-up or death, whichever is later.
Results: Eighteen patients were included with a median age of 74.5 years (range: 59-83). The site of metastasis was bone in 15, bone and distant lymph nodes in 2, and rectum in 1 patient. The median duration of androgen deprivation was 21 months (range: 3-42.9 months). The median cyclophosphamide exposure was 2 months (range: 0.9-13.5 months) after a median follow-up of 5.8 months. Overall PSA response rate was 44%. The median PSA progression-free survival with cyclophosphamide was 4.7 months (range: 0.9-13.5 months). Five patients had durable PSA response of 9.9, 10.1, 10.5, 12.1, and 13.5 months, respectively. No Grade 3 or 4 toxicity was observed with cyclophosphamide.
Conclusion: Oral metronomic cyclophosphamide was found to be an effective and well-tolerated therapy in mCRPC after failure or not fit for docetaxel and/or abiraterone. In few patients, cyclophosphamide induced durable PSA response. This finding needs further evaluation in a prospective manner.
van Rossum AGJ, Kok M, van Werkhoven E, et al.
Adjuvant dose-dense doxorubicin-cyclophosphamide versus docetaxel-doxorubicin-cyclophosphamide for high-risk breast cancer: First results of the randomised MATADOR trial (BOOG 2004-04).
Eur J Cancer. 2018; 102:40-48 [PubMed] Related Publications
Adjuvant dose-dense doxorubicin-cyclophosphamide versus docetaxel-doxorubicin-cyclophosphamide for high-risk breast cancer: First results of the randomised MATADOR trial (BOOG 2004-04).
Eur J Cancer. 2018; 102:40-48 [PubMed] Related Publications
BACKGROUND: Dose-dense administration of chemotherapy and the addition of taxanes to anthracycline-based adjuvant chemotherapy have improved breast cancer survival substantially. However, clinical trials directly comparing the additive value of taxanes with dose-dense anthracycline-based chemotherapy are lacking.
PATIENTS AND METHODS: In the multicentre, randomised, biomarker discovery Microarray Analysis in breast cancer to Tailor Adjuvant Drugs Or Regimens (MATADOR) trial, patients with pT1-3, pN0-3 breast cancer were randomised (1:1) between six adjuvant cycles of doxorubicin 60 mg/m
RESULTS: Between 2004 and 2012, 664 patients were randomised. At 5 years, RFS was 87% (95% confidence interval [CI] 83%-91%) in the ddAC-treated patients and 88% (84-92%) in the TAC-treated subgroup (hazard ratio [HR] 0.89, 95% CI 0.62-1.28, P = 0.53). OS at 5 years was 93% (90%-96%) in the ddAC-treated and 94% (91%-97%) in the TAC-treated patients (HR 0.89, 95% CI 0.57-1.39, P = 0.61). Anaemia was more frequent in ddAC-treated patients (62/327 patients [18.9%] versus 15/319 patients [4.7%], P < 0.001) and diarrhoea (21 [6.4%] versus 53 [16.6%], P<0.001) and peripheral neuropathy (15 [4.6%] versus 46 [14.4%], P < 0.001) were observed more often in TAC-treated patients.
CONCLUSIONS: With a median follow-up of 7 years, no significant differences in RFS and OS were observed between six adjuvant cycles of ddAC and TAC in high-risk breast cancer patients.
TRIAL REGISTRATION NUMBERS: ISRCTN61893718 and BOOG 2004-04.
PATIENTS AND METHODS: In the multicentre, randomised, biomarker discovery Microarray Analysis in breast cancer to Tailor Adjuvant Drugs Or Regimens (MATADOR) trial, patients with pT1-3, pN0-3 breast cancer were randomised (1:1) between six adjuvant cycles of doxorubicin 60 mg/m
RESULTS: Between 2004 and 2012, 664 patients were randomised. At 5 years, RFS was 87% (95% confidence interval [CI] 83%-91%) in the ddAC-treated patients and 88% (84-92%) in the TAC-treated subgroup (hazard ratio [HR] 0.89, 95% CI 0.62-1.28, P = 0.53). OS at 5 years was 93% (90%-96%) in the ddAC-treated and 94% (91%-97%) in the TAC-treated patients (HR 0.89, 95% CI 0.57-1.39, P = 0.61). Anaemia was more frequent in ddAC-treated patients (62/327 patients [18.9%] versus 15/319 patients [4.7%], P < 0.001) and diarrhoea (21 [6.4%] versus 53 [16.6%], P<0.001) and peripheral neuropathy (15 [4.6%] versus 46 [14.4%], P < 0.001) were observed more often in TAC-treated patients.
CONCLUSIONS: With a median follow-up of 7 years, no significant differences in RFS and OS were observed between six adjuvant cycles of ddAC and TAC in high-risk breast cancer patients.
TRIAL REGISTRATION NUMBERS: ISRCTN61893718 and BOOG 2004-04.
Valdez BC, Tang X, Li Y, et al.
Epigenetic modification enhances the cytotoxicity of busulfan and4-hydroperoxycyclophosphamide in AML cells.
Exp Hematol. 2018; 67:49-59.e1 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
Epigenetic modification enhances the cytotoxicity of busulfan and4-hydroperoxycyclophosphamide in AML cells.
Exp Hematol. 2018; 67:49-59.e1 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
The combination of the DNA-alkylating agents busulfan (Bu) and cyclophosphamide is the most commonly used myeloablative pretransplantation conditioning therapy for myeloid leukemias. However, it is associated with significant nonrelapse mortality, which prohibits dose escalation to control relapse. We hypothesized that combining these two drugs with an epigenetic modifier would increase antileukemic efficacy without jeopardizing patient safety. A preclinical study was performed to determine the synergistic cytotoxicity of Bu, 4-hydroperoxycyclophosphamide (4HC), and the hypomethylating agent decitabine (DAC) in human acute myeloid leukemia (AML) cell lines. Exposure of KBM3/Bu250


 Breast Cancer
Breast Cancer