Found this page useful?
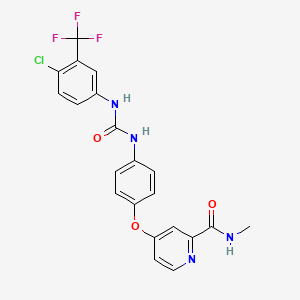
Sorafenib (Nexavar)
 Web Resources: Sorafenib (Nexavar)
Web Resources: Sorafenib (Nexavar) Latest Research Publications
Latest Research PublicationsWeb Resources: Sorafenib (Nexavar) (6 links)
Irish Cancer Society
MedlinePlus.gov
NHS Evidence
PubChem
Macmillan Cancer Support
Cancer Research UK
Latest Research Publications
Atkin C, Earwaker P, Pallan A, et al.
Exceptional serological and radiological response to sorafenib in 2 patients with advanced hepatocellular carcinoma and chronic hepatitis C viral infection: case report and review of the literature.
BMC Gastroenterol. 2017; 17(1):30 [PubMed] Free Access to Full Article Related Publications
Exceptional serological and radiological response to sorafenib in 2 patients with advanced hepatocellular carcinoma and chronic hepatitis C viral infection: case report and review of the literature.
BMC Gastroenterol. 2017; 17(1):30 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: In patients with advanced hepatocellular carcinoma (HCC), the multikinase inhibitor sorafenib is the only systemic treatment that has been shown to increase overall survival. However, similar to other tyrosine kinase inhibitors, most patients achieve disease stabilisation radiologically, and only 2-3% of patients achieve a partial response. Recent exploratory subgroup analyses of the large phase 3 trials have demonstrated that patients with chronic hepatitis C virus (HCV) infection associated HCC survive longer than those who are negative for HCV. The mechanism underlying this currently remains unknown. A small number of cases of complete response to sorafenib treatment have now been reported worldwide, however a prolonged response has only been reported in 2 cases, both of whom had HCV-related HCC.
CASE PRESENTATION: A 55 year old gentleman was diagnosed with hepatocellular carcinoma and concomitant chronic hepatitis C viral infection. He progressed following transarterial chemoemoblisation treatment and was commenced on sorafenib treatment. His serum alphafetoprotein level normalised within 2 months of treatment and he achieved an almost complete radiological response. This response was maintained for 20 months before the patient progressed. A 75 year old lady was diagnosed with advanced hepatocellular carcinoma and concomitant chronic hepatitis C viral infection. She was commenced on sorafenib treatment but required early dose reductions due to palmar plantar erythrodysesthesia, and liver decompensation. Despite this she achieved an excellent serological and radiological response that was maintained for 24 months.
CONCLUSIONS: Our two cases show that patients with HCV-associated HCC can attain excellent responses to sorafenib treatment that is durable. Furthermore, such exceptional responses can be achieved even with dose reductions and treatment breaks.
CASE PRESENTATION: A 55 year old gentleman was diagnosed with hepatocellular carcinoma and concomitant chronic hepatitis C viral infection. He progressed following transarterial chemoemoblisation treatment and was commenced on sorafenib treatment. His serum alphafetoprotein level normalised within 2 months of treatment and he achieved an almost complete radiological response. This response was maintained for 20 months before the patient progressed. A 75 year old lady was diagnosed with advanced hepatocellular carcinoma and concomitant chronic hepatitis C viral infection. She was commenced on sorafenib treatment but required early dose reductions due to palmar plantar erythrodysesthesia, and liver decompensation. Despite this she achieved an excellent serological and radiological response that was maintained for 24 months.
CONCLUSIONS: Our two cases show that patients with HCV-associated HCC can attain excellent responses to sorafenib treatment that is durable. Furthermore, such exceptional responses can be achieved even with dose reductions and treatment breaks.
Nass N, Streit S, Wybranski C, et al.
Validation of VX2 as a Hepatocellular Carcinoma Model: Comparison of the Molecular Reaction of VX2 and HepG2 Tumor Cells to Sorafenib In Vitro.
Anticancer Res. 2017; 37(1):87-93 [PubMed] Related Publications
Validation of VX2 as a Hepatocellular Carcinoma Model: Comparison of the Molecular Reaction of VX2 and HepG2 Tumor Cells to Sorafenib In Vitro.
Anticancer Res. 2017; 37(1):87-93 [PubMed] Related Publications
As there is currently no superior hepatocellular carcinoma (HCC) model with percutaneous vascular access for transarterial treatments available, the VX2 rabbit model is frequently used for in vivo investigations on liver carcinoma. However, the VX2 cell line was derived from a virus-induced skin papilloma that can form carcinosarcoma in liver of rabbits and the transferability of obtained results to HCC treatment remains open. Here we compared the most frequently investigated human HCC model cell line, HepG2, with VX2 cells in vitro in terms of sensitivity towards the broad specificity kinase inhibitor sorafenib and responsiveness to the addition of platelet-derived growth factor AB (PDGF-AB), vascular endothelial growth factor (VEGF) and hepatic growth factor (HGF), as well as insulin and interleukin-1β (IL1β). Phosphorylation of protein kinase B (AKT) the mitogen-activated protein kinases (MAPKs) p38 and p42/44 (extracellular signal-regulated kinase, ERK1/2) and inhibitor of kappa light chain gene enhancer alpha (IĸBα) was determined by western blotting as these events are associated with early signaling cascades. Additionally, the inhibition of phosphorylation under sorafenib treatment was investigated. Sorafenib was equally toxic to both cell lines, but only in HepG2 was activation of caspase 3/7 activity, as a sign of apoptosis, observed. VX2 cells exhibited generally more intense phosphorylation signals in response to the growth factors and also serum. In contrast to VX2, HepG2 cells showed no response to PDGF-AB or VEGF as determined by kinase phosphorylation. In both cell lines, sorafenib inhibited growth factor-induced phosphorylation of ERK and p38-MAPK. AKT phosphorylation was only inhibited in VX2 cells and IĸBα phosphorylation was not influenced by this kinase inhibitor in either cell type. Taken together, the two cellular models for HCC share several features related to sorafenib application, but differed in their responsiveness towards growth factors. Therefore, results obtained with the VX2 model cannot be extended to human HCC without appropriate caution.
Lin ZY, Chuang WL
Contrary influence of clinically applied sorafenib concentrations among hepatocellular carcinoma patients.
Biomed Pharmacother. 2017; 86:27-31 [PubMed] Related Publications
Contrary influence of clinically applied sorafenib concentrations among hepatocellular carcinoma patients.
Biomed Pharmacother. 2017; 86:27-31 [PubMed] Related Publications
The treatment responses of sorafenib in hepatocellular carcinoma are modest which may be due to different characteristics of cancer cells or insufficient therapeutic concentrations. This study was to clarify this issue. The anti-proliferative effects and differential expressions of 8 genes related to sorafenib anti-cancer mechanisms (tyrosine kinase receptor genes: KDR, PDGFRB; RAF cascade: RAF1, BRAF, MAP2K1, MAP2K2, MAPK1, MAPK3) were investigated in primary cultured hepatocellular carcinoma cells collected from 8 patients using clinically applied sorafenib concentrations (5, 10μg/mL). The anti-proliferative effects of sorafenib at either 5 or 10μg/mL, which were related to down-regulations of KDR, PDGFRB and/or genes in the RAF cascade, were achieved only in one patient (HCC38/KMUH). However, either 5 or 10μg/mL sorafenib promoted proliferation in 4 patients (HCC29/KMUH, HCC62/KMUH, HCC87/KMUH, HCC98/KMUH). Among them, the RAF cascade, PDGFRB and/or KDR were up-regulated in 3 patients but no gene was differentially expressed in the remaining one patient (HCC87/KMUH). Increase the sorafenib concentration to 10μg/mL paradoxically up-regulated and/or obliterated the previously down-regulated genes in the RAF cascade and/or KDR in 4 patients (HCC29/KMUH, HCC76/KMUH, HCC87/KMUH, HCC98/KMUH). Significant down-regulations of the RAF cascade and PDGFRB by sorafenib but without anti-proliferative effects were detected in one patient (HCC54/KMUH). In conclusion, influence of sorafenib on proliferation is not simply through the RAF cascade. The responses of KDR, PDGFRB and the RAF cascade to sorafenib among patients are diverse or even contrary. Increase the sorafenib concentration has potential to up-regulate genes favored angiogenesis and proliferation.
Bruix J, Qin S, Merle P, et al.
Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial.
Lancet. 2017; 389(10064):56-66 [PubMed] Related Publications
Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial.
Lancet. 2017; 389(10064):56-66 [PubMed] Related Publications
BACKGROUND: There are no systemic treatments for patients with hepatocellular carcinoma (HCC) whose disease progresses during sorafenib treatment. We aimed to assess the efficacy and safety of regorafenib in patients with HCC who have progressed during sorafenib treatment.
METHODS: In this randomised, double-blind, parallel-group, phase 3 trial done at 152 sites in 21 countries, adults with HCC who tolerated sorafenib (≥400 mg/day for ≥20 of last 28 days of treatment), progressed on sorafenib, and had Child-Pugh A liver function were enrolled. Participants were randomly assigned (2:1) by a computer-generated randomisation list and interactive voice response system and stratified by geographical region, Eastern Cooperative Oncology Group performance status, macrovascular invasion, extrahepatic disease, and α-fetoprotein level to best supportive care plus oral regorafenib 160 mg or placebo once daily during weeks 1-3 of each 4-week cycle. Investigators, patients, and the funder were masked to treatment assignment. The primary endpoint was overall survival (defined as time from randomisation to death due to any cause) and analysed by intention to treat. This trial is registered with ClinicalTrials.gov, number NCT01774344.
FINDINGS: Between May 14, 2013, and Dec 31, 2015, 843 patients were screened, of whom 573 were enrolled and randomised (379 to regorafenib and 194 to placebo; population for efficacy analyses), and 567 initiated treatment (374 received regorafenib and 193 received placebo; population for safety analyses). Regorafenib improved overall survival with a hazard ratio of 0·63 (95% CI 0·50-0·79; one-sided p<0·0001); median survival was 10·6 months (95% CI 9·1-12·1) for regorafenib versus 7·8 months (6·3-8·8) for placebo. Adverse events were reported in all regorafenib recipients (374 [100%] of 374) and 179 (93%) of 193 placebo recipients. The most common clinically relevant grade 3 or 4 treatment-emergent events were hypertension (57 patients [15%] in the regorafenib group vs nine patients [5%] in the placebo group), hand-foot skin reaction (47 patients [13%] vs one [1%]), fatigue (34 patients [9%] vs nine patients [5%]), and diarrhoea (12 patients [3%] vs no patients). Of the 88 deaths (grade 5 adverse events) reported during the study (50 patients [13%] assigned to regorafenib and 38 [20%] assigned to placebo), seven (2%) were considered by the investigator to be related to study drug in the regorafenib group and two (1%) in the placebo group, including two patients (1%) with hepatic failure in the placebo group.
INTERPRETATION: Regorafenib is the only systemic treatment shown to provide survival benefit in HCC patients progressing on sorafenib treatment. Future trials should explore combinations of regorafenib with other systemic agents and third-line treatments for patients who fail or who do not tolerate the sequence of sorafenib and regorafenib.
FUNDING: Bayer.
METHODS: In this randomised, double-blind, parallel-group, phase 3 trial done at 152 sites in 21 countries, adults with HCC who tolerated sorafenib (≥400 mg/day for ≥20 of last 28 days of treatment), progressed on sorafenib, and had Child-Pugh A liver function were enrolled. Participants were randomly assigned (2:1) by a computer-generated randomisation list and interactive voice response system and stratified by geographical region, Eastern Cooperative Oncology Group performance status, macrovascular invasion, extrahepatic disease, and α-fetoprotein level to best supportive care plus oral regorafenib 160 mg or placebo once daily during weeks 1-3 of each 4-week cycle. Investigators, patients, and the funder were masked to treatment assignment. The primary endpoint was overall survival (defined as time from randomisation to death due to any cause) and analysed by intention to treat. This trial is registered with ClinicalTrials.gov, number NCT01774344.
FINDINGS: Between May 14, 2013, and Dec 31, 2015, 843 patients were screened, of whom 573 were enrolled and randomised (379 to regorafenib and 194 to placebo; population for efficacy analyses), and 567 initiated treatment (374 received regorafenib and 193 received placebo; population for safety analyses). Regorafenib improved overall survival with a hazard ratio of 0·63 (95% CI 0·50-0·79; one-sided p<0·0001); median survival was 10·6 months (95% CI 9·1-12·1) for regorafenib versus 7·8 months (6·3-8·8) for placebo. Adverse events were reported in all regorafenib recipients (374 [100%] of 374) and 179 (93%) of 193 placebo recipients. The most common clinically relevant grade 3 or 4 treatment-emergent events were hypertension (57 patients [15%] in the regorafenib group vs nine patients [5%] in the placebo group), hand-foot skin reaction (47 patients [13%] vs one [1%]), fatigue (34 patients [9%] vs nine patients [5%]), and diarrhoea (12 patients [3%] vs no patients). Of the 88 deaths (grade 5 adverse events) reported during the study (50 patients [13%] assigned to regorafenib and 38 [20%] assigned to placebo), seven (2%) were considered by the investigator to be related to study drug in the regorafenib group and two (1%) in the placebo group, including two patients (1%) with hepatic failure in the placebo group.
INTERPRETATION: Regorafenib is the only systemic treatment shown to provide survival benefit in HCC patients progressing on sorafenib treatment. Future trials should explore combinations of regorafenib with other systemic agents and third-line treatments for patients who fail or who do not tolerate the sequence of sorafenib and regorafenib.
FUNDING: Bayer.
Mondal A, Bennett LL
Resveratrol enhances the efficacy of sorafenib mediated apoptosis in human breast cancer MCF7 cells through ROS, cell cycle inhibition, caspase 3 and PARP cleavage.
Biomed Pharmacother. 2016; 84:1906-1914 [PubMed] Related Publications
Resveratrol enhances the efficacy of sorafenib mediated apoptosis in human breast cancer MCF7 cells through ROS, cell cycle inhibition, caspase 3 and PARP cleavage.
Biomed Pharmacother. 2016; 84:1906-1914 [PubMed] Related Publications
Despite advances in diagnosis and treatment options, breast cancer is one of the main causes of cancer related death among women worldwide. Present study is aimed to preliminarily evaluate our hypothesis that the combination of resveratrol (RSV), a natural antioxidant, and lower dose of sorafenib (SF), a multi-kinase inhibitor and a component of ERK1/2 (extracellular signal-regulated kinase 1/2) pathway, would augment apoptosis in human breast cancer MCF7 cells. MCF7 cellexpressions s were treated with RSV, SF and their combination. MTT (3-[4,5-dimethylthiazol-2-yl] -2, 5-diphenyl-tetrazolium bromide) assay, DNA fragmentation assay, Hoechst33342, H2DCFDA (2', 7'-Dichlorodihydrofluorescein diacetate), Rhodamine123 staining, and Western Blot to detect different signaling protein expressions, were conducted to test the hypothesis. Combination of RSV and SF showed higher cytotoxicity on MCF7 cells than their individual treatment. Results from morphology change, Hoechst33342 staining, and DNA fragmentation suggested higher apoptosis data in the combinational treatment. Intracellular ROS (reactive oxygen species) levels, p53 and Bax/Bcl2 expressions, and decrease in mitochondrial membrane potential were also higher in the combinational treatment. Up-regulation of apaf-1, cl. caspase 9, cl. caspase 3 and cl. PARP (poly (ADP-Ribose) polymerase) were also noticed, while the expressions of cyclinD1 and cyclinB1 were decreased in the combinational group. The increase in apoptosis and signaling protein expressions with RSV and SF combinational treatment were increased over time. The combination of RSV and lower dose of SF at 6μM showed enhanced apoptotic activity than SF alone. Therefore, RSV can be considered as a neo-adjuvant to improve SF efficacy in breast cancer treatment.
Shiozawa K, Watanabe M, Ikehara T, et al.
Evaluation of sorafenib for advanced hepatocellular carcinoma with low α-fetoprotein in arrival time parametric imaging using contrast-enhanced ultrasonography.
J Med Ultrason (2001). 2017; 44(1):101-107 [PubMed] Free Access to Full Article Related Publications
Evaluation of sorafenib for advanced hepatocellular carcinoma with low α-fetoprotein in arrival time parametric imaging using contrast-enhanced ultrasonography.
J Med Ultrason (2001). 2017; 44(1):101-107 [PubMed] Free Access to Full Article Related Publications
PURPOSE: To determine the usefulness of arrival time parametric imaging (AtPI) using contrast-enhanced ultrasonography (CEUS) with Sonazoid in evaluating early response to sorafenib for hepatocellular carcinoma (HCC).
METHODS: Twenty-one advanced HCC patients with low α-fetoprotein (AFP) levels (≤35 ng/ml) who received sorafenib for at least 4 weeks were enrolled in this study. CEUS was performed before and 2 weeks after treatment, and the images of the target lesion in the arterial phase were analyzed by AtPI. In the color mapping images obtained by AtPI, the mean arrival time of the contrast agent in the target lesion from the reference point (mean time: MT) was calculated. In each patient, differences between MT before and MT 2 weeks after treatment were compared. MT (+) and MT (-) groups were defined as difference of 0 s or greater and less than 0 s, respectively. Overall survival was evaluated between the two groups.
RESULTS: In the MT (+) (11 patients) and MT (-) (10 patients) groups, the median survival time was 792 and 403 days, respectively, which was statistically significant.
CONCLUSIONS: The results suggested that AtPI was useful for evaluating early response to sorafenib for advanced HCC with low AFP level.
METHODS: Twenty-one advanced HCC patients with low α-fetoprotein (AFP) levels (≤35 ng/ml) who received sorafenib for at least 4 weeks were enrolled in this study. CEUS was performed before and 2 weeks after treatment, and the images of the target lesion in the arterial phase were analyzed by AtPI. In the color mapping images obtained by AtPI, the mean arrival time of the contrast agent in the target lesion from the reference point (mean time: MT) was calculated. In each patient, differences between MT before and MT 2 weeks after treatment were compared. MT (+) and MT (-) groups were defined as difference of 0 s or greater and less than 0 s, respectively. Overall survival was evaluated between the two groups.
RESULTS: In the MT (+) (11 patients) and MT (-) (10 patients) groups, the median survival time was 792 and 403 days, respectively, which was statistically significant.
CONCLUSIONS: The results suggested that AtPI was useful for evaluating early response to sorafenib for advanced HCC with low AFP level.
Giorgio A, Merola MG, Montesarchio L, et al.
Sorafenib Combined with Radio-frequency Ablation Compared with Sorafenib Alone in Treatment of Hepatocellular Carcinoma Invading Portal Vein: A Western Randomized Controlled Trial.
Anticancer Res. 2016; 36(11):6179-6183 [PubMed] Related Publications
Sorafenib Combined with Radio-frequency Ablation Compared with Sorafenib Alone in Treatment of Hepatocellular Carcinoma Invading Portal Vein: A Western Randomized Controlled Trial.
Anticancer Res. 2016; 36(11):6179-6183 [PubMed] Related Publications
AIM: To compare in a randomized controlled trial (RCT) 3-year survival of cirrhotic patients with hepatocellular carcinoma (HCC) accompanied by portal vein tumor thrombus (PVTT) treated with sorafenib plus percutaneous radiofrequency ablation (RFA) of both intraparenchymal HCC and PVTT (combination Group) or sorafenib alone (sorafenib-alone Group).
PATIENTS AND METHODS: Ninety-nine consecutive Child A cirrhotics were randomized to receive RFA of both HCC and main portal vein tumor thrombus (MPVTT) plus sorafenib (n=49) or sorafenib alone (n=50).
RESULTS: One-, 2- and 3-year survival rates were 60%, 35% and 26%, respectively, in the combination group and 37% and 0 % at 1- and 2-year, respectively, in the sorafenib alone group. At multivariate analysis, the combination of RFA of both HCC and MPVTT was the only factor predicting survival.
CONCLUSION: Use of RFA of both HCC and MPVTT plus sorafenib significantly increases 3-year survival compared to sorafenib alone.
PATIENTS AND METHODS: Ninety-nine consecutive Child A cirrhotics were randomized to receive RFA of both HCC and main portal vein tumor thrombus (MPVTT) plus sorafenib (n=49) or sorafenib alone (n=50).
RESULTS: One-, 2- and 3-year survival rates were 60%, 35% and 26%, respectively, in the combination group and 37% and 0 % at 1- and 2-year, respectively, in the sorafenib alone group. At multivariate analysis, the combination of RFA of both HCC and MPVTT was the only factor predicting survival.
CONCLUSION: Use of RFA of both HCC and MPVTT plus sorafenib significantly increases 3-year survival compared to sorafenib alone.
Garuti F, Camelli V, Spinardi L, et al.
Osteonecrosis of the jaw during sorafenib therapy for hepatocellular carcinoma.
Tumori. 2016; 102(Suppl. 2) [PubMed] Related Publications
Osteonecrosis of the jaw during sorafenib therapy for hepatocellular carcinoma.
Tumori. 2016; 102(Suppl. 2) [PubMed] Related Publications
INTRODUCTION: Sorafenib is an oral multiple tyrosine kinase inhibitor and is currently the only evidence-based treatment recommended for advanced hepatocellular carcinoma. We report a case of osteonecrosis of the jaw that occurred during sorafenib therapy in a patient with advanced hepatocellular carcinoma not treated with bisphosphonates or other antiangiogenic drugs.
METHODS: A systematic search in PubMed yielded some cases of osteonecrosis of the jaw in patients treated with antiangiogenic agents, alone or in combination with bisphosphonates, for metastatic renal cell carcinoma. The only case of osteonecrosis observed during sorafenib therapy not combined with other predisposing agents was described by Guillet et al.
RESULTS: A 74-year-old man diagnosed with hepatocellular carcinoma ensuing in hepatitis C virus infection, who was treated with sorafenib at a daily dose of 400 mg, developed osteonecrosis of the right mandibular body. The lesion was documented by a dental CT scan and surgical evaluation did not lead to an indication for curettage treatment. Sorafenib was discontinued because of the radiological and laboratory features of hepatocellular carcinoma progression and the high risk of jaw fracture.
CONCLUSIONS: To our knowledge, this is the first description of osteonecrosis of the jaw detected in a cirrhotic patient on sorafenib therapy not combined with bisphosphonates.
METHODS: A systematic search in PubMed yielded some cases of osteonecrosis of the jaw in patients treated with antiangiogenic agents, alone or in combination with bisphosphonates, for metastatic renal cell carcinoma. The only case of osteonecrosis observed during sorafenib therapy not combined with other predisposing agents was described by Guillet et al.
RESULTS: A 74-year-old man diagnosed with hepatocellular carcinoma ensuing in hepatitis C virus infection, who was treated with sorafenib at a daily dose of 400 mg, developed osteonecrosis of the right mandibular body. The lesion was documented by a dental CT scan and surgical evaluation did not lead to an indication for curettage treatment. Sorafenib was discontinued because of the radiological and laboratory features of hepatocellular carcinoma progression and the high risk of jaw fracture.
CONCLUSIONS: To our knowledge, this is the first description of osteonecrosis of the jaw detected in a cirrhotic patient on sorafenib therapy not combined with bisphosphonates.
Xu J, Lin H, Li G, et al.
The miR-367-3p Increases Sorafenib Chemotherapy Efficacy to Suppress Hepatocellular Carcinoma Metastasis through Altering the Androgen Receptor Signals.
EBioMedicine. 2016; 12:55-67 [PubMed] Free Access to Full Article Related Publications
The miR-367-3p Increases Sorafenib Chemotherapy Efficacy to Suppress Hepatocellular Carcinoma Metastasis through Altering the Androgen Receptor Signals.
EBioMedicine. 2016; 12:55-67 [PubMed] Free Access to Full Article Related Publications
The androgen receptor (AR) was found to suppress hepatocellular carcinoma (HCC) metastasis at late stages. Due to this discovery, we searched for some AR enhancers to increase the efficacy of Sorafenib chemotherapy, and identified the microRNA (miR)-367-3p, whose expression is positively correlated with AR expression in advanced HCC, as an HCC metastasis suppressor. Combining miR-367-3p with Sorafenib showed better efficacy to suppress HCC cell invasion in vitro and in vivo. Mechanism dissection revealed that miR-367-3p could increase AR expression via directly targeting the 3'UTR of MDM2 to decrease MDM2 protein expression. The resultant increase of AR expression might then promote the expression of FKBP5 and PHLPP, thus dephosphorylating and inactivating AKT and ERK, to suppress the HCC cell invasion. Interestingly, the suppression of pAKT by miR-367-3p could subsequently attenuate the phosphorylation of AR and MDM2, giving rise to additional enhancement of AR protein expression, effectively forming a positive feedback loop. Together, these results suggest that miR-367-3p may function as an AR enhancer to increase Sorafenib chemotherapy efficacy via altering the MDM2/AR/FKBP5/PHLPP/(pAKT and pERK) signals to better suppress HCC metastasis. Successful development of this newly combined chemotherapy in the future may help us to better suppress the HCC metastasis at late stages.
Kuzuya T, Ishigami M, Ishizu Y, et al.
Fever within 2 Weeks of Sorafenib Therapy Predicts Favorable Treatment Efficacy in Patients with Advanced Hepatocellular Carcinoma.
Oncology. 2016; 91(5):261-266 [PubMed] Related Publications
Fever within 2 Weeks of Sorafenib Therapy Predicts Favorable Treatment Efficacy in Patients with Advanced Hepatocellular Carcinoma.
Oncology. 2016; 91(5):261-266 [PubMed] Related Publications
OBJECTIVES: The aim of this study was to investigate the relationship between fever within 2 weeks after the start of sorafenib therapy and treatment efficacy in patients with advanced hepatocellular carcinoma (HCC).
METHODS: One hundred and two patients with advanced HCC were enrolled in this study. We retrospectively compared patients with fever (more than 38°C) within 2 weeks after the start of sorafenib therapy (fever group, n = 34) and patients without fever (non-fever group, n = 68) in terms of survival, best antitumor response, and change in intratumor blood on contrast-enhanced computed tomography (CE-CT) after 2 weeks of sorafenib therapy.
RESULTS: Fever was the only significant and independent predictor of better outcomes (hazard ratio, 0.517; 95% confidence interval, 0.319-0.838; p = 0.0071). In the fever group, the partial response rate, the disease control rate, and the rate of disappearance of arterial tumor enhancement on CE-CT after 2 weeks of sorafenib therapy were significantly higher than those in the non-fever group (38.2 vs. 5.9%, respectively, p = 0.0001; 85.3 vs. 60.3%, respectively, p = 0.0103; 76.5 vs. 35.3%, respectively, p < 0.0001).
CONCLUSIONS: Fever within 2 weeks after the start of sorafenib therapy may be a useful predictor of a favorable treatment response in patients with advanced HCC.
METHODS: One hundred and two patients with advanced HCC were enrolled in this study. We retrospectively compared patients with fever (more than 38°C) within 2 weeks after the start of sorafenib therapy (fever group, n = 34) and patients without fever (non-fever group, n = 68) in terms of survival, best antitumor response, and change in intratumor blood on contrast-enhanced computed tomography (CE-CT) after 2 weeks of sorafenib therapy.
RESULTS: Fever was the only significant and independent predictor of better outcomes (hazard ratio, 0.517; 95% confidence interval, 0.319-0.838; p = 0.0071). In the fever group, the partial response rate, the disease control rate, and the rate of disappearance of arterial tumor enhancement on CE-CT after 2 weeks of sorafenib therapy were significantly higher than those in the non-fever group (38.2 vs. 5.9%, respectively, p = 0.0001; 85.3 vs. 60.3%, respectively, p = 0.0103; 76.5 vs. 35.3%, respectively, p < 0.0001).
CONCLUSIONS: Fever within 2 weeks after the start of sorafenib therapy may be a useful predictor of a favorable treatment response in patients with advanced HCC.
Antoniou EA, Koutsounas I, Damaskos C, Koutsounas S
Remission of Psoriasis in a Patient with Hepatocellular Carcinoma Treated with Sorafenib.
In Vivo. 2016 09-10; 30(5):677-80 [PubMed] Related Publications
Remission of Psoriasis in a Patient with Hepatocellular Carcinoma Treated with Sorafenib.
In Vivo. 2016 09-10; 30(5):677-80 [PubMed] Related Publications
BACKGROUND: Psoriasis is a chronic, immune-mediated and angiogenesis-dependent disease. Activated keratinocytes in psoriatic lesions produce pro-angiogenic cytokines, including vascular endothelial growth factor (VEGF), which binds to vascular endothelial growth factor receptor (VEGFR) and promotes cell proliferation and angiogenesis. Sorafenib (BAY 43-9006) is a molecular multikinase inhibitor of RAF kinase, platelet-derived growth factor (PDGF), VEGFR-1, -2, -3, platelet-derived growth factor receptor (PDGFR)-β and c-Kit. This molecule inhibits tumor cell proliferation and angiogenesis and it is currently approved for the treatment of hepatocellular carcinoma (HCC).
CASE REPORT: We present the complete remission of resistant psoriasis in a hepatitis C virus (HCV)-infected cirrhotic patient who was treated with sorafenib, for recurrent HCC.
CONCLUSION: Several targeted therapies have demonstrated efficacy against psoriasis. More research and well-designed studies, both in novel drugs and those already marketed for other indications, are needed to determine their value as potential novel therapies for psoriasis.
CASE REPORT: We present the complete remission of resistant psoriasis in a hepatitis C virus (HCV)-infected cirrhotic patient who was treated with sorafenib, for recurrent HCC.
CONCLUSION: Several targeted therapies have demonstrated efficacy against psoriasis. More research and well-designed studies, both in novel drugs and those already marketed for other indications, are needed to determine their value as potential novel therapies for psoriasis.
Lamarca A, Abdel-Rahman O, Salu I, et al.
Identification of clinical biomarkers for patients with advanced hepatocellular carcinoma receiving sorafenib.
Clin Transl Oncol. 2017; 19(3):364-372 [PubMed] Related Publications
Identification of clinical biomarkers for patients with advanced hepatocellular carcinoma receiving sorafenib.
Clin Transl Oncol. 2017; 19(3):364-372 [PubMed] Related Publications
BACKGROUND: Identification of patients with advanced HCC-deriving preferential benefit from sorafenib is desirable, and treatment-related adverse events are potential clinical biomarkers.
METHODS: Survival and toxicity data for patients with HCC treated with sorafenib at the Christie NHS Foundation Trust from 11/09 to 02/15 were collected retrospectively.
RESULTS: Eighty-five eligible patients were identified. The most common grade 3 or 4 treatment-related toxicities were hypertension (HTN, 45 %), fatigue (8 %), and hand-foot syndrome (HFS, 8 %). Any-grade HFS and/or worsening HTN (HFS/HTN) were experienced by 58 % of patients. Estimated median progression-free and overall survival (OS) were 4.6 (95 % CI 2.8-5.2) and 6.5 (95 % CI 4.9-8.01) months, respectively. Child-Pugh score (p value <0.001) and the development of HFS/HTN were independent prognostic factors impacting on OS on multivariable analysis. Patients who developed HFS/HTN had median OS of 8.2 months (95 % CI 6.5-12.4) compared with 4.1 (95 % CI 2.7-5.4) for those without this toxicity (Hazard Ratio (HR) 0.4, 95 % CI 0.2-0.7, p value 0.003). The prognostic impact of HFS/HTN was confirmed by landmark analyses limited to patients who lived a minimum of 2 months (p value 0.019) or who developed HFS/HTN in the first 3 months of treatment (p value 0.006).
CONCLUSION(S): The development of toxicities specific to sorafenib is associated with prolonged survival in a UK-based HCC patient series; prospective assessment of their significance is required.
METHODS: Survival and toxicity data for patients with HCC treated with sorafenib at the Christie NHS Foundation Trust from 11/09 to 02/15 were collected retrospectively.
RESULTS: Eighty-five eligible patients were identified. The most common grade 3 or 4 treatment-related toxicities were hypertension (HTN, 45 %), fatigue (8 %), and hand-foot syndrome (HFS, 8 %). Any-grade HFS and/or worsening HTN (HFS/HTN) were experienced by 58 % of patients. Estimated median progression-free and overall survival (OS) were 4.6 (95 % CI 2.8-5.2) and 6.5 (95 % CI 4.9-8.01) months, respectively. Child-Pugh score (p value <0.001) and the development of HFS/HTN were independent prognostic factors impacting on OS on multivariable analysis. Patients who developed HFS/HTN had median OS of 8.2 months (95 % CI 6.5-12.4) compared with 4.1 (95 % CI 2.7-5.4) for those without this toxicity (Hazard Ratio (HR) 0.4, 95 % CI 0.2-0.7, p value 0.003). The prognostic impact of HFS/HTN was confirmed by landmark analyses limited to patients who lived a minimum of 2 months (p value 0.019) or who developed HFS/HTN in the first 3 months of treatment (p value 0.006).
CONCLUSION(S): The development of toxicities specific to sorafenib is associated with prolonged survival in a UK-based HCC patient series; prospective assessment of their significance is required.
Basu S, Joshi A
68Ga DOTATATE PET/CT in Differentiated Thyroid Carcinoma With Fibular Metastasis and Mixed Response to Sorafenib.
Clin Nucl Med. 2016; 41(10):772-3 [PubMed] Related Publications
68Ga DOTATATE PET/CT in Differentiated Thyroid Carcinoma With Fibular Metastasis and Mixed Response to Sorafenib.
Clin Nucl Med. 2016; 41(10):772-3 [PubMed] Related Publications
We describe somatostatin receptor targeted imaging findings in a 56-year-old woman with elevated serum thyroglobulin and radioiodine negative DTC fibular metastasis. The fibular lesion was biopsy proven of poorly differentiated thyroid carcinoma and demonstrated high grade uptake on Tc-HYNIC-TOC scintigraphy. She opted for sorafenib therapy for progressively increasing fibular swelling and was started on 400 mg daily followed by dose escalation to 400 mg twice daily. At 17 months after sorafenib initiation, Ga DOTATATE PET/CT demonstrated necrosis of the fibular lesion; however, new lesions were documented in lower dorsal and lumbar vertebrae and skull, based upon which sorafenib withdrawal was contemplated.
Azumi J, Tsubota T, Sakabe T, Shiota G
miR-181a induces sorafenib resistance of hepatocellular carcinoma cells through downregulation of RASSF1 expression.
Cancer Sci. 2016; 107(9):1256-62 [PubMed] Free Access to Full Article Related Publications
miR-181a induces sorafenib resistance of hepatocellular carcinoma cells through downregulation of RASSF1 expression.
Cancer Sci. 2016; 107(9):1256-62 [PubMed] Free Access to Full Article Related Publications
Sorafenib, a multi-kinase inhibitor, is the only standard clinical drug for patients with advanced hepatocellular carcinoma (HCC); however, development of sorafenib resistance in HCC often prevents its long-term efficacy. Therefore, novel targets and strategies are urgently needed to improve the antitumor effect of sorafenib. In the present study, we examined the novel mechanisms of sorafenib resistance of HCC cells by investigating the difference in sorafenib sensitivity between two HCC cell lines. Sorafenib induced more apoptosis of HepG2 cells compared to Hep3B cells. Sorafenib exposure to HepG2 cells but not Hep3B cells increased the expression of proapoptotic factor PUMA, and activated PARP and caspase-3. Notably, microRNA-181a (miR-181a) expression levels were lower in HepG2 cells than in Hep3B cells. Exogenous miR-181a expression in HepG2 cells reduced apoptosis, whereas inhibition of miR-181a in Hpe3B cells increased apoptosis. In addition, we demonstrated that miR-181a directly targets RASSF1, a MAPK signaling factor, and knockdown of RASSF1 increased sorafenib resistance. Taken together, these results suggest that miR-181a provokes sorafenib resistance through suppression of RASSF1. Our data provide important insight into the novel therapeutic strategy against sorafenib resistance of HCC cells by targeting of miR-181a pathway.
Dinh VY, Bhatia S, Narayanan G, et al.
Pilot Study of Intrahepatic Artery Chemotherapy in Combination with Sorafenib in Hepatocellular Carcinoma.
Anticancer Res. 2016; 36(7):3555-63 [PubMed] Related Publications
Pilot Study of Intrahepatic Artery Chemotherapy in Combination with Sorafenib in Hepatocellular Carcinoma.
Anticancer Res. 2016; 36(7):3555-63 [PubMed] Related Publications
BACKGROUND/AIM: Sorafenib and chemoembolization of the liver (TACE) have both produced increased survival in hepatocellular carcinoma (HCC). Some patients cannot tolerate TACE due to portal vein thrombosis or risk of liver failure. In this pilot trial, we aimed to combine intrahepatic infusion (IA) of cisplatin or carboplatin with sorafenib for unresectable HCC.
PATIENTS AND METHODS: Patients with Child's A or early B received IA cisplatin or carboplatin every 6 weeks with oral sorafenib. MRI/CT scans were performed every 6 weeks.
RESULTS: Eleven patients were accrued. Of 10 evaluable patients, 6 had clinical benefit (4 partial responses for 2+, 3+, 8+ and 18 months, 2 minor responses). Two patients were down-staged enough for ablation therapy or liver transplant and remain free of disease for 32+ and 36+ months. Toxicity was generally tolerable.
CONCLUSION: Preliminary results are encouraging and this combination may down-stage some patients with unresectable disease.
PATIENTS AND METHODS: Patients with Child's A or early B received IA cisplatin or carboplatin every 6 weeks with oral sorafenib. MRI/CT scans were performed every 6 weeks.
RESULTS: Eleven patients were accrued. Of 10 evaluable patients, 6 had clinical benefit (4 partial responses for 2+, 3+, 8+ and 18 months, 2 minor responses). Two patients were down-staged enough for ablation therapy or liver transplant and remain free of disease for 32+ and 36+ months. Toxicity was generally tolerable.
CONCLUSION: Preliminary results are encouraging and this combination may down-stage some patients with unresectable disease.
Hatooka M, Kawaoka T, Aikata H, et al.
Comparison of Outcome of Hepatic Arterial Infusion Chemotherapy and Sorafenib in Patients with Hepatocellular Carcinoma Refractory to Transcatheter Arterial Chemoembolization.
Anticancer Res. 2016; 36(7):3523-9 [PubMed] Related Publications
Comparison of Outcome of Hepatic Arterial Infusion Chemotherapy and Sorafenib in Patients with Hepatocellular Carcinoma Refractory to Transcatheter Arterial Chemoembolization.
Anticancer Res. 2016; 36(7):3523-9 [PubMed] Related Publications
AIM: To compare the outcome of 5-fluorouracil (FU)-based hepatic arterial infusion chemotherapy (HAIC) with sorafenib monotherapy in patients with hepatocellular carcinoma (HCC) refractory to transcatheter arterial chemoembolization (TACE).
PATIENTS AND METHODS: In this retrospective cohort study, 123 patients with HCC refractory to TACE, with Child-Pugh A and free of extrahepatic metastasis, were divided into two groups: 65 received HAIC and 58 received sorafenib. Since the size of main tumor and portal vein invasion were significantly different between the HAIC and sorafenib groups, we selected 48 patients from the 65 patients of the HAIC group and 48 from the 58 patients of the sorafenib group. The model used one-to-one matching between the two groups using the case-control method matching method. The clinical characteristics of patients of the case-control HAIC (n=48) and sorafenib groups (n=48) were similar. Overall survival, time to progression and time to treatment failure (TTTF) were compared between the two groups.
RESULTS: The median survival time and TTTF were significantly longer in the sorafenib group than in the HAIC group (15 and 12.2 months versus 8 and 4.4 months, respectively; p=0.021 and p=0.002, respectively). Multivariate analysis identified male gender (p=0.008), relative tumor size <50% (p=0.012), α-fetoprotein <400 ng/ml (p=0.005), and treatment with sorafenib (p=0.001) as significant and independent determinants of better overall survival.
CONCLUSION: In patients with HCC refractory to TACE, overall survival was favorable in those treated with sorafenib rather than HAIC.
PATIENTS AND METHODS: In this retrospective cohort study, 123 patients with HCC refractory to TACE, with Child-Pugh A and free of extrahepatic metastasis, were divided into two groups: 65 received HAIC and 58 received sorafenib. Since the size of main tumor and portal vein invasion were significantly different between the HAIC and sorafenib groups, we selected 48 patients from the 65 patients of the HAIC group and 48 from the 58 patients of the sorafenib group. The model used one-to-one matching between the two groups using the case-control method matching method. The clinical characteristics of patients of the case-control HAIC (n=48) and sorafenib groups (n=48) were similar. Overall survival, time to progression and time to treatment failure (TTTF) were compared between the two groups.
RESULTS: The median survival time and TTTF were significantly longer in the sorafenib group than in the HAIC group (15 and 12.2 months versus 8 and 4.4 months, respectively; p=0.021 and p=0.002, respectively). Multivariate analysis identified male gender (p=0.008), relative tumor size <50% (p=0.012), α-fetoprotein <400 ng/ml (p=0.005), and treatment with sorafenib (p=0.001) as significant and independent determinants of better overall survival.
CONCLUSION: In patients with HCC refractory to TACE, overall survival was favorable in those treated with sorafenib rather than HAIC.
Maida M, Macaluso FS, Valenza F, Virdone R
Complete and Sustained Off-Therapy Response to Sorafenib in Advanced Hepatocellular Carcinoma.
J Gastrointestin Liver Dis. 2016; 25(2):253-5 [PubMed] Related Publications
Complete and Sustained Off-Therapy Response to Sorafenib in Advanced Hepatocellular Carcinoma.
J Gastrointestin Liver Dis. 2016; 25(2):253-5 [PubMed] Related Publications
UNLABELLED: A 75-year-old Caucasian woman with alcohol-related cirrhosis was admitted to our Unit in October 2012 for the diagnostic evaluation of a focal liver lesion detected by regular surveillance ultrasound. The subsequent dynamic CT and MR led to a diagnosis of infiltrative hepatocellular carcinoma (HCC) of 5 cm in the hepatic segment IV with neoplastic infiltration of the left branch of the portal vein, in absence of extrahepatic metastases. Therapy with sorafenib 400 mg bid was started and the subsequent dynamic CT performed at the 10th month of therapy showed a complete response according to RECIST criteria and mRECIST, while seriated dosages of α-fetoprotein levels showed a progressive reduction up to normalization. After 18 months of therapy, Sorafenib was discontinued due to a grade 3 adverse event. Nonetheless, all subsequent radiological controls, performed over the following two years confirmed a complete off-therapy response despite withdrawal of Sorafenib. After three years the patient is asymptomatic, with a preserved liver function and undetectable solid tumor lesions at dynamic CT. This case represents one of the few examples of complete response to anti-angiogenic drugs and, to our knowledge, the only case of sustained response, even after the discontinuation of Sorafenib, described so far in the literature.
KEY WORDS: hepatocellular carcinoma - HCC - BCLC - sorafenib - complete response.
ABBREVIATIONS: AFP: alpha-fetoprotein; AE: adverse event; BCLC: Barcelona Clinic Liver Cancer; CT: computed tomography; HCC: hepatocellular carcinoma; mRECIST: modified response evaluation criteria in solid tumors; PS: Performance status; RCTs: randomized controlled trials.
KEY WORDS: hepatocellular carcinoma - HCC - BCLC - sorafenib - complete response.
ABBREVIATIONS: AFP: alpha-fetoprotein; AE: adverse event; BCLC: Barcelona Clinic Liver Cancer; CT: computed tomography; HCC: hepatocellular carcinoma; mRECIST: modified response evaluation criteria in solid tumors; PS: Performance status; RCTs: randomized controlled trials.
Oya M, Tatsugami K, Kabu K, et al.
Little Impact on Renal Function in Advanced Renal Cell Carcinoma Patients Treated with Sorafenib--Analyses of Postmarketing Surveillance in Japan in over 3,200 Consecutive Cases.
Gan To Kagaku Ryoho. 2016; 43(5):559-69 [PubMed] Related Publications
Little Impact on Renal Function in Advanced Renal Cell Carcinoma Patients Treated with Sorafenib--Analyses of Postmarketing Surveillance in Japan in over 3,200 Consecutive Cases.
Gan To Kagaku Ryoho. 2016; 43(5):559-69 [PubMed] Related Publications
BACKGROUND: To assess the effect of sorafenib on renal function in patients with advanced renal cell carcinoma (RCC) included in a postmarketing surveillance.
METHODS: All patients in Japan with advanced RCC treated with sorafenib between February 2008 and September 2009 were followed for 12 months. Baseline characteristics, renal function, survival, safety, and dosage were stratified according to baseline estimated glomerular filtration rate (eGFR): G1 (eGFR≥90), G2 (eGFR≥60-<90), G3a (eGFR≥45-<60), G3b (eGFR≥30-<45), G4 (eGFR≥15-<30), and G5 (eGFR<15). A total of 3,255 and 3,171 patients were included in this analysis for safety and efficacy, respectively.
RESULTS: The mean eGFRs (mL/min/1.73 m2) were not substantially changed for each group at baseline and 12 months, respectively. Median daily doses of sorafenib were 726 mg (G1), 522 mg (G2), 524 mg (G3a), 517 mg (G3b), 483 mg (G4), and 400 mg (G5). Renal failure, reported as an adverse event, occurred more frequently in the G4 and G5 groups (9%and 3%, respectively) than in other groups. Objective response rates for each subgroup were as follows: G1, 23%; G2, 28%; G3a, 29%; G3b, 26%; G4, 24%; and G5, 18%. One-year survival was higher in the G3a and G3b groups (82% and 78%, respectively) and lower in the G1 group (50%).
CONCLUSIONS: This study demonstrated little impact of sorafenib on renal function in advanced RCC patients during the observational period. Patients showed sufficient clinical response and safety irrespective of baseline eGFR value.
METHODS: All patients in Japan with advanced RCC treated with sorafenib between February 2008 and September 2009 were followed for 12 months. Baseline characteristics, renal function, survival, safety, and dosage were stratified according to baseline estimated glomerular filtration rate (eGFR): G1 (eGFR≥90), G2 (eGFR≥60-<90), G3a (eGFR≥45-<60), G3b (eGFR≥30-<45), G4 (eGFR≥15-<30), and G5 (eGFR<15). A total of 3,255 and 3,171 patients were included in this analysis for safety and efficacy, respectively.
RESULTS: The mean eGFRs (mL/min/1.73 m2) were not substantially changed for each group at baseline and 12 months, respectively. Median daily doses of sorafenib were 726 mg (G1), 522 mg (G2), 524 mg (G3a), 517 mg (G3b), 483 mg (G4), and 400 mg (G5). Renal failure, reported as an adverse event, occurred more frequently in the G4 and G5 groups (9%and 3%, respectively) than in other groups. Objective response rates for each subgroup were as follows: G1, 23%; G2, 28%; G3a, 29%; G3b, 26%; G4, 24%; and G5, 18%. One-year survival was higher in the G3a and G3b groups (82% and 78%, respectively) and lower in the G1 group (50%).
CONCLUSIONS: This study demonstrated little impact of sorafenib on renal function in advanced RCC patients during the observational period. Patients showed sufficient clinical response and safety irrespective of baseline eGFR value.
Woo K, Stewart SG, Kong GS, et al.
Identification of a thalidomide derivative that selectively targets tumorigenic liver progenitor cells and comparing its effects with lenalidomide and sorafenib.
Eur J Med Chem. 2016; 120:275-83 [PubMed] Related Publications
Identification of a thalidomide derivative that selectively targets tumorigenic liver progenitor cells and comparing its effects with lenalidomide and sorafenib.
Eur J Med Chem. 2016; 120:275-83 [PubMed] Related Publications
BACKGROUND & AIMS: The availability of non-tumorigenic and tumorigenic liver progenitor cell (LPC) lines affords a method to screen putative anti-liver cancer agents to identify those that are selectively effective. To prove this principle we tested thalidomide and a range of its derivatives and compared them to lenalidomide and sorafenib, to assess their growth-inhibitory effects.
METHODS: Cell growth, the mitotic and apoptotic index of cell cultures were measured using the Cellavista instrument (SynenTec) using commercially available reagents.
RESULTS: Neither lenalidomide nor thalidomide (100 μM) affected tumorigenic LPCs but killed their non-tumorigenic counterparts. Sorafenib arrested growth in both cell types. All but two derivatives of thalidomide were ineffective; of the two effective derivatives, one (thalidomide C1) specifically affected the tumorigenic cell line (10 μM). Mitotic and apoptotic analyses revealed that thalidomide C1 induced apoptotic cell death and not mitotic arrest.
CONCLUSIONS: This study shows that screens incorporating non-tumorigenic and tumorigenic liver cell lines are a sound approach to identify agents that are effective and selective. A high throughput instrument such as the Cellavista affords robust and reproducible objective measurements with a large number of replicates that are reliable. These experiments show that neither lenalidomide nor thalidomide are potentially useful for anti-liver cancer therapy as they kill non-tumorigenic liver cells and not their tumorigenic counterparts. Sorafenib in contrast, is highly effective, but not selective. One tested thalidomide derivative has potential as an anti-tumor drug since it induced growth arrest; and importantly, it selectively induced apoptotic cell death only in tumorigenic liver progenitor cells.
METHODS: Cell growth, the mitotic and apoptotic index of cell cultures were measured using the Cellavista instrument (SynenTec) using commercially available reagents.
RESULTS: Neither lenalidomide nor thalidomide (100 μM) affected tumorigenic LPCs but killed their non-tumorigenic counterparts. Sorafenib arrested growth in both cell types. All but two derivatives of thalidomide were ineffective; of the two effective derivatives, one (thalidomide C1) specifically affected the tumorigenic cell line (10 μM). Mitotic and apoptotic analyses revealed that thalidomide C1 induced apoptotic cell death and not mitotic arrest.
CONCLUSIONS: This study shows that screens incorporating non-tumorigenic and tumorigenic liver cell lines are a sound approach to identify agents that are effective and selective. A high throughput instrument such as the Cellavista affords robust and reproducible objective measurements with a large number of replicates that are reliable. These experiments show that neither lenalidomide nor thalidomide are potentially useful for anti-liver cancer therapy as they kill non-tumorigenic liver cells and not their tumorigenic counterparts. Sorafenib in contrast, is highly effective, but not selective. One tested thalidomide derivative has potential as an anti-tumor drug since it induced growth arrest; and importantly, it selectively induced apoptotic cell death only in tumorigenic liver progenitor cells.
Leung HW, Liu CF, Chan AL
Cost-effectiveness of sorafenib versus SBRT for unresectable advanced hepatocellular carcinoma.
Radiat Oncol. 2016; 11:69 [PubMed] Free Access to Full Article Related Publications
Cost-effectiveness of sorafenib versus SBRT for unresectable advanced hepatocellular carcinoma.
Radiat Oncol. 2016; 11:69 [PubMed] Free Access to Full Article Related Publications
OBJECTIVE: Stereotactic body radiotherapy (SBRT) has been shown to improve overall survival in patients with advanced hepatocellular carcinoma. This study aimed to assess the cost-effectiveness of SBRT compared to sorafenib which is the only drug for advanced hepatocellular carcinoma.
METHODS: A Markov decision-analytic model was performed to compare the cost-effectiveness of SBRT and sorafenib for unresectable advanced hepatocellular carcinoma. Patients transitioned between three health states: stable disease, progression disease and death. We calculated the data on cost from the perspective of our National Health Insurance Bureau. Sensitivity analyses were conducted to determine the impact of several variables.
RESULTS: The incremental cost effectiveness ratio (ICER) for sorafenib compared to SBRT was NT$3,788,238 per quality-adjusted life year gained (cost/QALY), which was higher than the willingness to pay threshold of Taiwan according to WHO's guideline. One-way sensitivity analysis revealed that the utility of progression disease for the sorafenib treatment, utility of progression free survival for SBRT, utility of progression free survival for sorafenib, utility of PFS to progression disease for SBRT and transition probability of progression disease to dead for SBRT were the most sensitive parameters in all cost scenarios. The Monte-Carlo simulation demonstrated that the probability of cost-effectiveness at a willingness to pay threshold of NT$ 2,213,145 per QALY was 100 % and 0 % chance for SBRT and sorafenib.
CONCLUSION: This study indicated that SBRT for advanced hepatocellular carcinoma is cost-effective at a willingness to pay threshold as defined by WHO guideline in Taiwan.
METHODS: A Markov decision-analytic model was performed to compare the cost-effectiveness of SBRT and sorafenib for unresectable advanced hepatocellular carcinoma. Patients transitioned between three health states: stable disease, progression disease and death. We calculated the data on cost from the perspective of our National Health Insurance Bureau. Sensitivity analyses were conducted to determine the impact of several variables.
RESULTS: The incremental cost effectiveness ratio (ICER) for sorafenib compared to SBRT was NT$3,788,238 per quality-adjusted life year gained (cost/QALY), which was higher than the willingness to pay threshold of Taiwan according to WHO's guideline. One-way sensitivity analysis revealed that the utility of progression disease for the sorafenib treatment, utility of progression free survival for SBRT, utility of progression free survival for sorafenib, utility of PFS to progression disease for SBRT and transition probability of progression disease to dead for SBRT were the most sensitive parameters in all cost scenarios. The Monte-Carlo simulation demonstrated that the probability of cost-effectiveness at a willingness to pay threshold of NT$ 2,213,145 per QALY was 100 % and 0 % chance for SBRT and sorafenib.
CONCLUSION: This study indicated that SBRT for advanced hepatocellular carcinoma is cost-effective at a willingness to pay threshold as defined by WHO guideline in Taiwan.
Gu W, Wang B, Gan H, et al.
Prognostic value of pathological features of primary lesion in metastatic renal cell carcinoma treated with sorafenib.
Future Oncol. 2016; 12(15):1783-93 [PubMed] Related Publications
Prognostic value of pathological features of primary lesion in metastatic renal cell carcinoma treated with sorafenib.
Future Oncol. 2016; 12(15):1783-93 [PubMed] Related Publications
AIM: This study aimed to investigate whether the pathological features of primary lesions show additional prognostic value in patients with metastatic renal cell carcinoma who are treated with sorafenib.
PATIENTS & METHODS: A consecutive cohort of 284 patients was included from Fudan University Shanghai Cancer Center between 2007 and 2013. The association between survival and pathological features of primary tumors was assessed using the Cox proportional hazards model. The incremental value of prognostication was evaluated.
RESULTS: We found that the pathological features of primary lesions provided added prognostic value over the Memorial Sloan-Kettering Cancer Center model in patients with metastatic renal cell carcinoma who were treated with sorafenib.
CONCLUSION: Addition of a pathological score in the clinical setting could better identify patients at risk of poor survival.
PATIENTS & METHODS: A consecutive cohort of 284 patients was included from Fudan University Shanghai Cancer Center between 2007 and 2013. The association between survival and pathological features of primary tumors was assessed using the Cox proportional hazards model. The incremental value of prognostication was evaluated.
RESULTS: We found that the pathological features of primary lesions provided added prognostic value over the Memorial Sloan-Kettering Cancer Center model in patients with metastatic renal cell carcinoma who were treated with sorafenib.
CONCLUSION: Addition of a pathological score in the clinical setting could better identify patients at risk of poor survival.
Hsiao WD, Peng CY, Chuang PH, et al.
Evaluation of dose-efficacy of sorafenib and effect of transarterial chemoembolization in hepatocellular carcinoma patients: a retrospective study.
BMC Gastroenterol. 2016; 16:50 [PubMed] Free Access to Full Article Related Publications
Evaluation of dose-efficacy of sorafenib and effect of transarterial chemoembolization in hepatocellular carcinoma patients: a retrospective study.
BMC Gastroenterol. 2016; 16:50 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Transarterial chemoembolization (TACE) and sorafenib are the therapeutic standard for intermediate and advanced stage hepatocellular carcinoma (HCC) patients respectively. High costs with adverse events (AE) of sorafenib might limit sorafenib dosage, further affecting therapeutic response. To attain greatest benefit, we evaluated the efficacy of different doses and effect of TACE during and after sorafenib discontinuation in patients representing Child-Pugh Classification Class A with venous or extra-hepatic invasion.
METHODS: A total 156 patients met the criteria and were divided into Groups I (n = 52) accepting 800 mg/day; II (n = 58) accepting 800 mg/day and reduced to 400 mg/day owing to AE; and III (n = 46) accepting 400 mg/day. TACE was performed during and after sorafenib discontinuation and therapeutic response bimonthly to four-monthly was rated thereafter.
RESULTS: Median duration of sorafenib treatment and patients' survival were 4.00 ± 0.45 and 7.50 ± 1.44 months in all cases; 2.50 ± 0.90 and 5.00 ± 1.10 months in Group I; 5.50 ± 1.27 and 16.50 ± 1.86 months in Group II; 4.00 ± 0.94 and 6.50 ± 2.49 months in Group III. Group II presented the best response and survival benefit (p = 0.010 and p = 0.011 respectively). Child-Pugh Classification score 5 (Hazard Ratio = 0.492, p = 0.049), absent AE (3.423, p = 0.015), tumor numbers ≤ 3 (0.313, p = 0.009), sorafenib duration ≤ 1 cycle (3.694, p = 0.004), and absent TACE (3.197, p = 0.008) significantly correlated with patient survival. TACE benefit appeared in separate and total cases during (p = 0.002, p = 0.595, p = 0.074, p = 0.002 respectively) and after discontinuation of sorafenib administration (p = 0.001, p = 0.034, p = 0.647, p = 0.001 respectively).
CONCLUSIONS: Low-dosage sorafenib not only appeared tolerable and lowered economic pressure but also provided satisfactory results. TACE benefited patient's survival during and after sorafenib discontinuation.
METHODS: A total 156 patients met the criteria and were divided into Groups I (n = 52) accepting 800 mg/day; II (n = 58) accepting 800 mg/day and reduced to 400 mg/day owing to AE; and III (n = 46) accepting 400 mg/day. TACE was performed during and after sorafenib discontinuation and therapeutic response bimonthly to four-monthly was rated thereafter.
RESULTS: Median duration of sorafenib treatment and patients' survival were 4.00 ± 0.45 and 7.50 ± 1.44 months in all cases; 2.50 ± 0.90 and 5.00 ± 1.10 months in Group I; 5.50 ± 1.27 and 16.50 ± 1.86 months in Group II; 4.00 ± 0.94 and 6.50 ± 2.49 months in Group III. Group II presented the best response and survival benefit (p = 0.010 and p = 0.011 respectively). Child-Pugh Classification score 5 (Hazard Ratio = 0.492, p = 0.049), absent AE (3.423, p = 0.015), tumor numbers ≤ 3 (0.313, p = 0.009), sorafenib duration ≤ 1 cycle (3.694, p = 0.004), and absent TACE (3.197, p = 0.008) significantly correlated with patient survival. TACE benefit appeared in separate and total cases during (p = 0.002, p = 0.595, p = 0.074, p = 0.002 respectively) and after discontinuation of sorafenib administration (p = 0.001, p = 0.034, p = 0.647, p = 0.001 respectively).
CONCLUSIONS: Low-dosage sorafenib not only appeared tolerable and lowered economic pressure but also provided satisfactory results. TACE benefited patient's survival during and after sorafenib discontinuation.
Li J, Hou Y, Cai XB, Liu B
Sorafenib after resection improves the outcome of BCLC stage C hepatocellular carcinoma.
World J Gastroenterol. 2016; 22(15):4034-40 [PubMed] Free Access to Full Article Related Publications
Sorafenib after resection improves the outcome of BCLC stage C hepatocellular carcinoma.
World J Gastroenterol. 2016; 22(15):4034-40 [PubMed] Free Access to Full Article Related Publications
AIM: To evaluate whether sorafenib use after resection impacts tumor relapse and survival in Barcelona Clinic Liver Cancer (BCLC) stage C hepatocellular carcinoma (HCC).
METHODS: This retrospective study enrolled 36 male BCLC stage C HCC patients with portal vein thrombus and Child-Pugh class A liver function. Twenty-four patients received only surgical resection (SR), and 12 patients received oral sorafenib within 30 d after surgery. The primary outcomes were time to progression (TTP) (the time from surgical resection until HCC recurrence or extrahepatic metastases) and overall survival (OS). The secondary outcome was the rate of postoperative recurrence or metastasis. TTP and OS were analyzed using Kaplan Meier curves.
RESULTS: There were no significant differences between the two groups in the serum levels of alpha-fetoprotein, copies of hepatitis B virus-DNA, preoperative laboratory results, degree of hepatic fibrosis, types of portal vein tumor thrombus, number of satellite lesions, tumor diameter, pathological results, volume of blood loss, volume of blood transfusion, or surgery time (all P > 0.05). Patients in the SR + sorafenib group had a significantly longer TTP (29 mo vs 22 mo, P = 0.041) and a significantly longer median OS (37 mo vs 30 mo, P = 0.01) compared to patients in the SR group. The SR group had 18 cases (75%) of recurrence/metastasis while the SR + sorafenib group had six cases (50%) of recurrence/metastasis. A total of 19 patients died after surgery (five in the SR + sorafenib group and 14 in the SR group). The most common sorafenib-related adverse events were skin reactions, diarrhea, and hypertension, all of which were resolved with treatment.
CONCLUSION: Sorafenib after SR was well-tolerated. Patients who received sorafenib after SR had better outcomes compared to patients who received only SR.
METHODS: This retrospective study enrolled 36 male BCLC stage C HCC patients with portal vein thrombus and Child-Pugh class A liver function. Twenty-four patients received only surgical resection (SR), and 12 patients received oral sorafenib within 30 d after surgery. The primary outcomes were time to progression (TTP) (the time from surgical resection until HCC recurrence or extrahepatic metastases) and overall survival (OS). The secondary outcome was the rate of postoperative recurrence or metastasis. TTP and OS were analyzed using Kaplan Meier curves.
RESULTS: There were no significant differences between the two groups in the serum levels of alpha-fetoprotein, copies of hepatitis B virus-DNA, preoperative laboratory results, degree of hepatic fibrosis, types of portal vein tumor thrombus, number of satellite lesions, tumor diameter, pathological results, volume of blood loss, volume of blood transfusion, or surgery time (all P > 0.05). Patients in the SR + sorafenib group had a significantly longer TTP (29 mo vs 22 mo, P = 0.041) and a significantly longer median OS (37 mo vs 30 mo, P = 0.01) compared to patients in the SR group. The SR group had 18 cases (75%) of recurrence/metastasis while the SR + sorafenib group had six cases (50%) of recurrence/metastasis. A total of 19 patients died after surgery (five in the SR + sorafenib group and 14 in the SR group). The most common sorafenib-related adverse events were skin reactions, diarrhea, and hypertension, all of which were resolved with treatment.
CONCLUSION: Sorafenib after SR was well-tolerated. Patients who received sorafenib after SR had better outcomes compared to patients who received only SR.
Wang Z, Hu P, Tang F, Xie C
HDAC6-mediated EGFR stabilization and activation restrict cell response to sorafenib in non-small cell lung cancer cells.
Med Oncol. 2016; 33(5):50 [PubMed] Related Publications
HDAC6-mediated EGFR stabilization and activation restrict cell response to sorafenib in non-small cell lung cancer cells.
Med Oncol. 2016; 33(5):50 [PubMed] Related Publications
Sorafenib is a multi-targeted kinase inhibitor and has been the subject of extensive clinical research in advanced non-small cell lung cancer (NSCLC). However, sorafenib fails to improve overall survival of patients with advanced NSCLC. The molecular mechanisms that account for this phenomenon are unclear. Here we show that sorafenib treatment stabilizes epidermal growth factor receptor (EGFR) and activates EGFR pathway. Moreover, this is partly mediated by stabilization of histone deacetylase 6 (HDAC6), which has been shown to regulate EGFR endocytic trafficking and degradation. Overexpression of HDAC6 confers resistance to sorafenib in NSCLC cells. Inhibition of HDAC6 with selective inhibitors synergizes with sorafenib to kill NSCLC cells via inhibition of sorafenib-mediated EGFR pathway activation. Taken together, our findings might partly explain the failure of Phase III trial of sorafenib in improving overall survival of advanced NSCLC patients and bear possible implications for the improvement on the efficacy of sorafenib in treatment of NSCLC.
Lee JM, Jang BK, Lee YJ, et al.
Survival outcomes of hepatic resection compared with transarterial chemoembolization or sorafenib for hepatocellular carcinoma with portal vein tumor thrombosis.
Clin Mol Hepatol. 2016; 22(1):160-7 [PubMed] Free Access to Full Article Related Publications
Survival outcomes of hepatic resection compared with transarterial chemoembolization or sorafenib for hepatocellular carcinoma with portal vein tumor thrombosis.
Clin Mol Hepatol. 2016; 22(1):160-7 [PubMed] Free Access to Full Article Related Publications
BACKGROUND/AIMS: Treating hepatocellular carcinoma (HCC) with portal vein tumor thrombosis (PVTT) remains controversial. We compared the outcomes of hepatic resection (HR), transarterial chemoembolization (TACE), and sorafenib therapy as treatments for HCC with PVTT.
METHODS: Patients diagnosed as HCC with PVTT between January 2000 and December 2011 who received treatment with sorafenib, HR, or TACE were included. Patients with main PVTT, superior mesenteric vein tumor thrombosis, or Child-Turcotte-Pugh (CTP) class C were excluded. The records of 172 patients were analyzed retrospectively. HR, TACE, and sorafenib treatment were performed is 40, 80, and 52 patients respectively. PVTT was classified as either involving the segmental branch (type I) or extending to involve the right or left portal vein (type II).
RESULTS: The median survival time was significantly longer in the HR group (19.9 months) than in the TACE and sorafenib groups (6.6 and 6.2 months, respectively; both p<0.001), and did not differ significantly between the latter two groups (p=0.698). Among patients with CTP class A, type I PVTT or unilobar-involved HCC, the median survival time was longer in the HR group than in the TACE and sorafenib groups (p=0.006). In univariate analyses, the initial treatment method, tumor size, PVTT type, involved lobe, CTP class, and presence of cirrhosis or ascites were correlated with overall survival. The significant prognostic factors for overall survival in Cox proportional-hazards regression analysis were initial treatment method (HR vs. TACE: hazard ratio=1.750, p=0.036; HR vs. sorafenib: hazard ratio=2.262, p=0.006), involved lobe (hazard ratio=1.705, p=0.008), PVTT type (hazard ratio=1.617, p=0.013), and CTP class (hazard ratio=1.712, p=0.012).
CONCLUSIONS: Compared with TACE or sorafenib, HR may prolong the survival of patients with HCC in cases of CTP class A, type I PVTT or unilobar-involved HCC.
METHODS: Patients diagnosed as HCC with PVTT between January 2000 and December 2011 who received treatment with sorafenib, HR, or TACE were included. Patients with main PVTT, superior mesenteric vein tumor thrombosis, or Child-Turcotte-Pugh (CTP) class C were excluded. The records of 172 patients were analyzed retrospectively. HR, TACE, and sorafenib treatment were performed is 40, 80, and 52 patients respectively. PVTT was classified as either involving the segmental branch (type I) or extending to involve the right or left portal vein (type II).
RESULTS: The median survival time was significantly longer in the HR group (19.9 months) than in the TACE and sorafenib groups (6.6 and 6.2 months, respectively; both p<0.001), and did not differ significantly between the latter two groups (p=0.698). Among patients with CTP class A, type I PVTT or unilobar-involved HCC, the median survival time was longer in the HR group than in the TACE and sorafenib groups (p=0.006). In univariate analyses, the initial treatment method, tumor size, PVTT type, involved lobe, CTP class, and presence of cirrhosis or ascites were correlated with overall survival. The significant prognostic factors for overall survival in Cox proportional-hazards regression analysis were initial treatment method (HR vs. TACE: hazard ratio=1.750, p=0.036; HR vs. sorafenib: hazard ratio=2.262, p=0.006), involved lobe (hazard ratio=1.705, p=0.008), PVTT type (hazard ratio=1.617, p=0.013), and CTP class (hazard ratio=1.712, p=0.012).
CONCLUSIONS: Compared with TACE or sorafenib, HR may prolong the survival of patients with HCC in cases of CTP class A, type I PVTT or unilobar-involved HCC.
Sorafenib (NEXAVAR) and differentiated thyroid cancer. Toxic, and no proof of improved survival.
Prescrire Int. 2016; 25(168):37 [PubMed] Related Publications
Radiological progression was delayed by 5 months in one trial, but its design does not allow reliable analysis of survival. Numerous, sometimes serious, adverse effects occurred.
Pitoia F, Jerkovich F
Selective use of sorafenib in the treatment of thyroid cancer.
Drug Des Devel Ther. 2016; 10:1119-31 [PubMed] Free Access to Full Article Related Publications
Selective use of sorafenib in the treatment of thyroid cancer.
Drug Des Devel Ther. 2016; 10:1119-31 [PubMed] Free Access to Full Article Related Publications
Sorafenib is a multiple kinase inhibitor (MKI) approved for the treatment of primary advanced renal cell carcinoma and advanced primary liver cancer. It was recently approved by several health agencies around the world as the first available MKI treatment for radioactive iodine-refractory advanced and progressive differentiated thyroid cancer. Sorafenib targets C-RAF, B-RAF, VEGF receptor-1, -2, -3, PDGF receptor-β, RET, c-kit, and Flt-3. As a multifunctional inhibitor, sorafenib has the potential of inhibiting tumor growth, progression, metastasis, and angiogenesis and downregulating mechanisms that protect tumors from apoptosis and has shown to increase the progression-free survival in several Phase II trials. This led to the Phase III trial (DECISION) which showed that there was an improvement in progression-free survival of 5 months for patients on sorafenib when compared to those on placebo. Adverse events with this drug are common but usually manageable. The development of resistance after 1 or 2 years is almost a rule in most patients who showed partial response or stabilization of the disease while on sorafenib, which makes it necessary to think of a plan for subsequent therapies. These may include the use of another MKI, such as lenvatinib, the second approved MKI for advanced differentiated thyroid cancer, or include patients in clinical trials or the off-label use of other MKIs. Given sorafenib's earlier approval, most centers now have access to its prescription. The goal of this review was to improve the care of these patients by describing key aspects that all prescribers will need to master in order to optimize outcomes.
Thomas VA, Balthasar JP
Sorafenib Decreases Tumor Exposure to an Anti-carcinoembryonic Antigen Monoclonal Antibody in a Mouse Model of Colorectal Cancer.
AAPS J. 2016; 18(4):923-32 [PubMed] Related Publications
Sorafenib Decreases Tumor Exposure to an Anti-carcinoembryonic Antigen Monoclonal Antibody in a Mouse Model of Colorectal Cancer.
AAPS J. 2016; 18(4):923-32 [PubMed] Related Publications
In this investigation, we test the hypothesis that treatment with sorafenib, an anti-angiogenic agent, decreases tumor vascularization and, consequently, hinders the delivery of monoclonal antibodies (mAb) to xenograft tumors. Severe combined immunodeficiency mice bearing carcinoembryonic antigen (CEA) expressing tumor xenografts were divided into control and sorafenib-treated groups. Sorafenib was administered to the latter group at 50 mg/kg IP every 48 h, starting 4 days post-tumor implantation. When tumors attained a size of 200-300 mm(3), mice were evaluated for (a) tumor microvessel density (using immunohistochemical analysis), (b) tumor macromolecular extravasation (using Evans Blue Dye (EBD)), (c) pharmacokinetics of an anti-CEA mAb, T84.66, following an intravenous dose of 10 mg/kg, and (d) intra-tumoral spatial distribution of T84.66 (using autoradiography). Sorafenib treatment resulted in a substantial reduction in tumor growth rate, a visible reduction in tumor microvessel density, and in a 46.4% decrease in EBD extravasation in tumor tissue (p < 0.0455). For control and treated mice, no significant difference was found for the area under the mAb plasma concentration-time curve (AUC(0-7d): 1.67 × 10(3) ± 1.28 × 10(2) vs. 1.76 × 10(3) ± 1.75 × 10(2) nM × day, p = 0.51). However, tumor AUC(0-7d) was reduced by 40.8% in sorafenib-treated mice relative to that observed in control mice (5.61 × 10(2) ± 4.27 × 10(1) vs. 9.48 × 10(2) ± 5.61 × 10(1) nM × day, p < 0.001). Sorafenib therapy was also found to markedly alter mAb tumor spatial distribution. The results collectively suggest that sorafenib treatment causes a significant reduction in mAb delivery to, and distribution within, solid tumors.
Yao X, Yan D, Zeng H, et al.
Concurrent sorafenib therapy extends the interval to subsequent TACE for patients with unresectable hepatocellular carcinoma.
J Surg Oncol. 2016; 113(6):672-7 [PubMed] Related Publications
Concurrent sorafenib therapy extends the interval to subsequent TACE for patients with unresectable hepatocellular carcinoma.
J Surg Oncol. 2016; 113(6):672-7 [PubMed] Related Publications
BACKGROUND AND OBJECTIVES: To compare the impact of concurrent TACE + sorafenib versus TACE alone on overall survival (OS) and time to progression (TTP) in patients with unresectable hepatocellular carcinoma (uHCC). A secondary goal was to determine if sorafenib use increases the interval between courses of TACE.
METHODS: This study enrolled 150 patients with uHCC from June 2011 to June 2014, including 50 treated with TACE + sorafenib and 100 treated with TACE alone. Factors associated with OS and TTP were identified by univariate and multivariate Cox-regression model analyses. Average TACE interval was defined as TTP/TACE frequency.
RESULTS: The median OS (21.7 vs. 11.5 months) and TTP (10.2 vs. 6.7 months) were longer in the TACE + sorafenib group compared to the TACE group. Patients receiving combination therapy had higher survival rate (P < 0.032) and longer average interval to TACE (P < 0.001), but lower progression rate (P < 0.001). TACE + sorafenib therapy was associated with improved OS (P ≤ 0.009) and TTP (P ≤ 0.021). The majority of AEs identified in patients receiving the combination therapy were classified as Grades 1 and 2, and skin-related reactions and fatigue were the most common.
CONCLUSION: Concurrent sorafenib with TACE provides survival benefits over TACE monotherapy, which may be related to a prolonged interval between subsequent TACE courses. J. Surg. Oncol. 2016;113:672-677. © 2016 Wiley Periodicals, Inc.
METHODS: This study enrolled 150 patients with uHCC from June 2011 to June 2014, including 50 treated with TACE + sorafenib and 100 treated with TACE alone. Factors associated with OS and TTP were identified by univariate and multivariate Cox-regression model analyses. Average TACE interval was defined as TTP/TACE frequency.
RESULTS: The median OS (21.7 vs. 11.5 months) and TTP (10.2 vs. 6.7 months) were longer in the TACE + sorafenib group compared to the TACE group. Patients receiving combination therapy had higher survival rate (P < 0.032) and longer average interval to TACE (P < 0.001), but lower progression rate (P < 0.001). TACE + sorafenib therapy was associated with improved OS (P ≤ 0.009) and TTP (P ≤ 0.021). The majority of AEs identified in patients receiving the combination therapy were classified as Grades 1 and 2, and skin-related reactions and fatigue were the most common.
CONCLUSION: Concurrent sorafenib with TACE provides survival benefits over TACE monotherapy, which may be related to a prolonged interval between subsequent TACE courses. J. Surg. Oncol. 2016;113:672-677. © 2016 Wiley Periodicals, Inc.
Lorenzin D, Pravisani R, Leo CA, et al.
Complete Remission of Unresectable Hepatocellular Carcinoma After Combined Sorafenib and Adjuvant Yttrium-90 Radioembolization.
Cancer Biother Radiopharm. 2016; 31(2):65-9 [PubMed] Related Publications
Complete Remission of Unresectable Hepatocellular Carcinoma After Combined Sorafenib and Adjuvant Yttrium-90 Radioembolization.
Cancer Biother Radiopharm. 2016; 31(2):65-9 [PubMed] Related Publications
Sorafenib has improved the median overall survival of unresectable or otherwise untreatable hepatocellular carcinoma (HCC) of ∼3 months, compared to supportive cares. Complete response, although rare, has been reported. The authors reported herein a case of complete biochemical and radiological remission of advanced unresectable HCC with lymph node metastasis and tumoral portal vein thrombosis treated by 5 months therapy with sorafenib followed by adjuvant Yttrium-90 radioembolization. At 12 months follow-up, there is no evidence of HCC recurrence.



 Liver Cancer
Liver Cancer