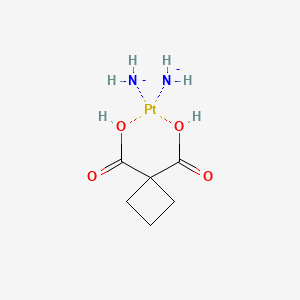
Carboplatin
"An organoplatinum compound that possesses antineoplastic activity." (MeSH 2013)
Found this page useful?
 Web Resources: Carboplatin
Web Resources: Carboplatin Latest Research Publications
Latest Research PublicationsWeb Resources: Carboplatin (6 links)
Cancer Research UK
Irish Cancer Society
Macmillan Cancer Support
NHS Evidence
 Carboplatin - Substance Summary
Carboplatin - Substance Summary
PubChem
MedlinePlus
Latest Research Publications
This list of publications is regularly updated (Source: PubMed).
Ruf CG, Borck S, Anheuser P, et al.
Adjuvant carboplatin therapy in patients with clinical stage 1 testicular seminoma: is long-term morbidity increased?
J Cancer Res Clin Oncol. 2019; 145(9):2335-2342 [PubMed] Related Publications
Adjuvant carboplatin therapy in patients with clinical stage 1 testicular seminoma: is long-term morbidity increased?
J Cancer Res Clin Oncol. 2019; 145(9):2335-2342 [PubMed] Related Publications
PURPOSE: Clinical stage (CS) 1 testicular seminoma is cured in almost 100% of cases following either retroperitoneal radiotherapy, carboplatin monotherapy, or surveillance strategies. Little is known about potential long-term effects of carboplatin. We, therefore, examined late sequelae of this drug in seminoma patients.
PATIENTS AND METHODS: We retrospectively identified 451 patients with CS1 testicular seminoma treated between 1994 and 2014, of whom 243 underwent carboplatin therapy [median follow-up (F/U) 96 months], 81 received radiotherapy (median F/U 142 months), and 127 underwent surveillance (median F/U 40 months). Satisfaction regarding management, as well as the following events during F/U, were analysed by questionnaire: subsequent malignant neoplasms (SMNs), cardiovascular events, arterial hypertension, peptic ulcer, tinnitus, peripheral neuropathy, hypogonadism, and infertility. The relative frequencies of the events were analysed using descriptive statistics. The frequency of observed SMNs was compared with the expected number.
RESULTS: Patients receiving carboplatin tolerated the treatment less well (71.2%) than those under surveillance (81.9%). After carboplatin, 12 SMNs (5.0%) were noted vis-a-vis 5.0 expected. There were three cases of prostatic cancer and 3 melanomas among the SMNs. Half of these SMNs occurred early after treatment. Among the other health events, only reported hypogonadism (13.2%) appeared to be marginally increased in frequency.
CONCLUSIONS: This study found a 2.4-fold higher than expected rate of SMN-and a slightly increased rate of hypogonadism-in the long-term period following carboplatin treatment. Although further studies are needed to confirm these preliminary findings, these results are probably informative for clinicians caring for seminoma patients.
PATIENTS AND METHODS: We retrospectively identified 451 patients with CS1 testicular seminoma treated between 1994 and 2014, of whom 243 underwent carboplatin therapy [median follow-up (F/U) 96 months], 81 received radiotherapy (median F/U 142 months), and 127 underwent surveillance (median F/U 40 months). Satisfaction regarding management, as well as the following events during F/U, were analysed by questionnaire: subsequent malignant neoplasms (SMNs), cardiovascular events, arterial hypertension, peptic ulcer, tinnitus, peripheral neuropathy, hypogonadism, and infertility. The relative frequencies of the events were analysed using descriptive statistics. The frequency of observed SMNs was compared with the expected number.
RESULTS: Patients receiving carboplatin tolerated the treatment less well (71.2%) than those under surveillance (81.9%). After carboplatin, 12 SMNs (5.0%) were noted vis-a-vis 5.0 expected. There were three cases of prostatic cancer and 3 melanomas among the SMNs. Half of these SMNs occurred early after treatment. Among the other health events, only reported hypogonadism (13.2%) appeared to be marginally increased in frequency.
CONCLUSIONS: This study found a 2.4-fold higher than expected rate of SMN-and a slightly increased rate of hypogonadism-in the long-term period following carboplatin treatment. Although further studies are needed to confirm these preliminary findings, these results are probably informative for clinicians caring for seminoma patients.
Mikkelsen MS, Christiansen T, Petersen LK, et al.
Morbidity after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy with carboplatin used for ovarian, tubal, and primary peritoneal cancer.
J Surg Oncol. 2019; 120(3):550-557 [PubMed] Related Publications
Morbidity after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy with carboplatin used for ovarian, tubal, and primary peritoneal cancer.
J Surg Oncol. 2019; 120(3):550-557 [PubMed] Related Publications
BACKGROUND AND OBJECTIVES: Hypertherm intraperitoneal chemotherapy (HIPEC) is increasingly used in the treatment of ovarian, tubal, and primary peritoneal cancer (OC). The aim was to evaluate short-term morbidity of cytoreductive surgery (CRS) and carboplatin HIPEC.
METHODS: Prospective feasibility study performed from January 2016 to December 2017. Twenty-five patients with primary OC (FIGO III-IV) received upfront or interval CRS combined with carboplatin HIPEC at dose 800 mg/m
RESULTS: No deaths (grade 5) or grade 4 adverse events were observed. Eleven patients (44.0%) experienced at least one grade 3 adverse event, the most common being an infection (28.0%) and neutropenia (12.0%). The reoperation rate was 8.0%. The median hospital stay was 14 days (range 9-25 days), and five patients (25.0%) were readmitted within 30 days after surgery. Median time from surgery to the administration of the first dose of systemic chemotherapy was 41 days (range 24-81 days).
CONCLUSION: Our small-scale prospective study supports that CRS and carboplatin HIPEC used for primary advanced-stage OC is feasible with acceptable morbidity.
METHODS: Prospective feasibility study performed from January 2016 to December 2017. Twenty-five patients with primary OC (FIGO III-IV) received upfront or interval CRS combined with carboplatin HIPEC at dose 800 mg/m
RESULTS: No deaths (grade 5) or grade 4 adverse events were observed. Eleven patients (44.0%) experienced at least one grade 3 adverse event, the most common being an infection (28.0%) and neutropenia (12.0%). The reoperation rate was 8.0%. The median hospital stay was 14 days (range 9-25 days), and five patients (25.0%) were readmitted within 30 days after surgery. Median time from surgery to the administration of the first dose of systemic chemotherapy was 41 days (range 24-81 days).
CONCLUSION: Our small-scale prospective study supports that CRS and carboplatin HIPEC used for primary advanced-stage OC is feasible with acceptable morbidity.
Vu MT, Bach LG, Nguyen DC, et al.
Modified Carboxyl-Terminated PAMAM Dendrimers as Great Cytocompatible Nano-Based Drug Delivery System.
Int J Mol Sci. 2019; 20(8) [PubMed] Free Access to Full Article Related Publications
Modified Carboxyl-Terminated PAMAM Dendrimers as Great Cytocompatible Nano-Based Drug Delivery System.
Int J Mol Sci. 2019; 20(8) [PubMed] Free Access to Full Article Related Publications
Polyamidoamine (PAMAM) dendrimers are extensively researched as potential drug delivery system thanks to their desirable features such as controlled and stable structures, and ease of functionalization onto their surface active groups. However, there have been concerns about the toxicity of full generation dendrimers and risks of premature clearance from circulation, along with other physical drawbacks presented in previous formulations, including large particle sizes and low drug loading efficiency. In our study, carboxyl-terminated PAMAM dendrimer G3.5 was grafted with poly (ethylene glycol) methyl ether (mPEG) to be employed as a nano-based drug delivery system with great cytocompatibility for the delivery of carboplatin (CPT), a widely prescribed anticancer drug with strong side effects so that the drug will be effectively entrapped and not exhibit uncontrolled outflow from the open structure of unmodified PAMAM G3.5. The particles formed were spherical in shape and had the optimal size range (around 36 nm) that accommodates high drug entrapment efficiency. Surface charge was also determined to be almost neutral and the system was cytocompatible. In vitro release patterns over 24 h showed a prolonged CPT release compared to free drug, which correlated to the cytotoxicity assay on malignant cell lines showing the lack of anticancer effect of CPT/mPEG-G3.5 compared with CPT.
Jeleniewicz W, Cybulski M, Nowakowski A, et al.
Anticancer Res. 2019; 39(4):1821-1827 [PubMed] Related Publications
Anticancer Res. 2019; 39(4):1821-1827 [PubMed] Related Publications
BACKGROUND/AIM: Ovarian cancer is the most frequent cause of death in women among gynecological cancers in Poland. MMP-2 and MMP-9 are frequently dysregulated in cancers and they are considered as potential biomarkers. Our goal was to assess the associations between MMP-2 and MMP-9 mRNA expression, clinicopathological parameters and patients' response to chemotherapy.
MATERIALS AND METHODS: We evaluated MMP-2 and MMP-9 mRNA expression in epithelial ovarian cancer (EOC) tissues from 44 untreated patients, four ovarian cancer cell lines, and human skin fibroblasts (HSF). The expression of both MMPs was estimated using qPCR.
RESULTS: MMP-2 expression was significantly higher (p=0.020) in EOCs sensitive to chemotherapy compared to resistant and refractory tumors. The highest MMP-2 expression was found in HSF and MMP-9 expression was the highest in EOCs (p<0.001). The expression of neither MMP was significantly associated with patients' overall survival (OS).
CONCLUSION: MMP-2 may be engaged in early stages of ovarian carcinogenesis. MMP-2 expression in EOCs may discriminate patients with a favorable response to first line chemotherapy.
MATERIALS AND METHODS: We evaluated MMP-2 and MMP-9 mRNA expression in epithelial ovarian cancer (EOC) tissues from 44 untreated patients, four ovarian cancer cell lines, and human skin fibroblasts (HSF). The expression of both MMPs was estimated using qPCR.
RESULTS: MMP-2 expression was significantly higher (p=0.020) in EOCs sensitive to chemotherapy compared to resistant and refractory tumors. The highest MMP-2 expression was found in HSF and MMP-9 expression was the highest in EOCs (p<0.001). The expression of neither MMP was significantly associated with patients' overall survival (OS).
CONCLUSION: MMP-2 may be engaged in early stages of ovarian carcinogenesis. MMP-2 expression in EOCs may discriminate patients with a favorable response to first line chemotherapy.
Han L, Wei ZX, Lv YF, Jiang AY
Efficacy of carboplatin plus S-1 for the treatment of non-small cell lung cancer: A protocol for a systematic review of randomized controlled trial.
Medicine (Baltimore). 2019; 98(14):e15099 [PubMed] Free Access to Full Article Related Publications
Efficacy of carboplatin plus S-1 for the treatment of non-small cell lung cancer: A protocol for a systematic review of randomized controlled trial.
Medicine (Baltimore). 2019; 98(14):e15099 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Non-small cell lung cancer (NSCLC) is the most common lung cancer. Numerous clinical studies have reported that the combination of carboplatin and S-1 (CS) can be used to treat NSCLC effectively. However, no systematic review has been conducted to assess its efficacy and safety for NSCLC. This systematic review aims to evaluate the efficacy and safety of CS for treatment of patients with NSCLC.
METHODS: This study will retrieve the following electronic databases from inception to the February 1, 2019: Cochrane Library, EMBASE, MEDILINE, CINAHL, AMED, and 4 Chinese databases without any language limitations. This systematic review will include randomized controlled trials (RCTs) and case-control studies for assessing the efficacy and safety of CS for the treatment of NSCLC. Cochrane risk of bias will be used as methodological quality assessment for each qualified study. The RevMan V.5.3 software will be utilized to synthesize the data and conduct the meta-analysis if it is allowed. The data will be pooled by using the random-effects model or fixed-effects model.
RESULTS: The primary outcome is overall response rate. The secondary outcomes are overall survival, progression-free survival, the disease control rate, and any adverse events.
CONCLUSION: It will provide latest evidence to determine the efficacy and safety of CS for treatment of patients with NSCLC.
ETHICS AND DISSEMINATION: No research ethic approval is needed in this study because this study will not analyze individual patient data. The results are expected to disseminate through peer-reviewed journals.
SYSTEMATIC REVIEW REGISTRATION: PROSPERO CRD42019124860.
METHODS: This study will retrieve the following electronic databases from inception to the February 1, 2019: Cochrane Library, EMBASE, MEDILINE, CINAHL, AMED, and 4 Chinese databases without any language limitations. This systematic review will include randomized controlled trials (RCTs) and case-control studies for assessing the efficacy and safety of CS for the treatment of NSCLC. Cochrane risk of bias will be used as methodological quality assessment for each qualified study. The RevMan V.5.3 software will be utilized to synthesize the data and conduct the meta-analysis if it is allowed. The data will be pooled by using the random-effects model or fixed-effects model.
RESULTS: The primary outcome is overall response rate. The secondary outcomes are overall survival, progression-free survival, the disease control rate, and any adverse events.
CONCLUSION: It will provide latest evidence to determine the efficacy and safety of CS for treatment of patients with NSCLC.
ETHICS AND DISSEMINATION: No research ethic approval is needed in this study because this study will not analyze individual patient data. The results are expected to disseminate through peer-reviewed journals.
SYSTEMATIC REVIEW REGISTRATION: PROSPERO CRD42019124860.
Viscarra T, Buchegger K, Jofre I, et al.
Functional and transcriptomic characterization of carboplatin-resistant A2780 ovarian cancer cell line.
Biol Res. 2019; 52(1):13 [PubMed] Free Access to Full Article Related Publications
Functional and transcriptomic characterization of carboplatin-resistant A2780 ovarian cancer cell line.
Biol Res. 2019; 52(1):13 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Ovarian cancer is a significant cancer-related cause of death in women worldwide. The most used chemotherapeutic regimen is based on carboplatin (CBDCA). However, CBDCA resistance is the main obstacle to a better prognosis. An in vitro drug-resistant cell model would help in the understanding of molecular mechanisms underlying this drug-resistance phenomenon. The aim of this study was to characterize cellular and molecular changes of induced CBDCA-resistant ovarian cancer cell line A2780.
METHODS: The cell selection strategy used in this study was a dose-per-pulse method using a concentration of 100 μM for 2 h. Once 20 cycles of exposure to the drug were completed, the cell cultures showed a resistant phenotype. Then, the ovarian cancer cell line A2780 was grown with 100 μM of CBDCA (CBDCA-resistant cells) or without CBDCA (parental cells). After, a drug sensitivity assay, morphological analyses, cell death assays and a RNA-seq analysis were performed in CBDCA-resistant A2780 cells.
RESULTS: Microscopy on both parental and CBDCA-resistant A2780 cells showed similar characteristics in morphology and F-actin distribution within cells. In cell-death assays, parental A2780 cells showed a significant increase in phosphatidylserine translocation and caspase-3/7 cleavage compared to CBDCA-resistant A2780 cells (P < 0.05 and P < 0.005, respectively). Cell viability in parental A2780 cells was significantly decreased compared to CBDCA-resistant A2780 cells (P < 0.0005). The RNA-seq analysis showed 156 differentially expressed genes (DEGs) associated mainly to molecular functions.
CONCLUSION: CBDCA-resistant A2780 ovarian cancer cells is a reliable model of CBDCA resistance that shows several DEGs involved in molecular functions such as transmembrane activity, protein binding to cell surface receptor and catalytic activity. Also, we found that the Wnt/β-catenin and integrin signaling pathway are the main metabolic pathway dysregulated in CBDCA-resistant A2780 cells.
METHODS: The cell selection strategy used in this study was a dose-per-pulse method using a concentration of 100 μM for 2 h. Once 20 cycles of exposure to the drug were completed, the cell cultures showed a resistant phenotype. Then, the ovarian cancer cell line A2780 was grown with 100 μM of CBDCA (CBDCA-resistant cells) or without CBDCA (parental cells). After, a drug sensitivity assay, morphological analyses, cell death assays and a RNA-seq analysis were performed in CBDCA-resistant A2780 cells.
RESULTS: Microscopy on both parental and CBDCA-resistant A2780 cells showed similar characteristics in morphology and F-actin distribution within cells. In cell-death assays, parental A2780 cells showed a significant increase in phosphatidylserine translocation and caspase-3/7 cleavage compared to CBDCA-resistant A2780 cells (P < 0.05 and P < 0.005, respectively). Cell viability in parental A2780 cells was significantly decreased compared to CBDCA-resistant A2780 cells (P < 0.0005). The RNA-seq analysis showed 156 differentially expressed genes (DEGs) associated mainly to molecular functions.
CONCLUSION: CBDCA-resistant A2780 ovarian cancer cells is a reliable model of CBDCA resistance that shows several DEGs involved in molecular functions such as transmembrane activity, protein binding to cell surface receptor and catalytic activity. Also, we found that the Wnt/β-catenin and integrin signaling pathway are the main metabolic pathway dysregulated in CBDCA-resistant A2780 cells.
Daniels AB, Froehler MT, Nunnally AH, et al.
Rabbit Model of Intra-Arterial Chemotherapy Toxicity Demonstrates Retinopathy and Vasculopathy Related to Drug and Dose, Not Procedure or Approach.
Invest Ophthalmol Vis Sci. 2019; 60(4):954-964 [PubMed] Free Access to Full Article Related Publications
Rabbit Model of Intra-Arterial Chemotherapy Toxicity Demonstrates Retinopathy and Vasculopathy Related to Drug and Dose, Not Procedure or Approach.
Invest Ophthalmol Vis Sci. 2019; 60(4):954-964 [PubMed] Free Access to Full Article Related Publications
Purpose: To use our intra-arterial chemotherapy (IAC) rabbit model to assess the impact of IAC procedure, drug, dose, and choice of technique on ocular structure and function, to study the nature and etiology of IAC toxicity, and to compare to observations in patients.
Methods: Rabbits received IAC melphalan (0.4-0.8 mg/kg), carboplatin (25-50 mg), or saline, either by direct ophthalmic artery cannulation, or with a technique emulating nonocclusion. Ocular structure/function were assessed with examination, electroretinography (ERG), fundus photography, fluorescein angiography, optical coherence tomography (OCT), and OCT angiography, prior to and 5 to 6 weeks after IAC. Blood counts were obtained weekly. We reviewed our last 50 IAC treatments in patients for evidence of ocular or systemic complications.
Results: No toxicity was seen in the saline control group. With standard (0.4 mg/kg) melphalan, no vascular/microvascular abnormalities were seen with either technique. However, severe microvascular pruning and arteriolar occlusions were seen occasionally at 0.8 mg/kg doses. ERG reductions were dose-dependent. Histology showed melphalan dose-dependent degeneration in all retinal layers, restricted geographically to areas of greatest vascular density. Carboplatin caused massive edema of ocular/periocular structures. IAC patients experienced occasional periocular swelling/rash, and only rarely experienced retinopathy or vascular events/hemorrhage in eyes treated multiple times with triple (melphalan/carboplatin/topotecan) therapy. Transient neutropenia occurred after 46% of IAC procedures, generally after triple therapy.
Conclusions: IAC toxicity appears to be related to the specific drug being used and is dose-dependent, rather than related to the IAC procedure itself or the specific technique selected. These rabbit findings are corroborated by our clinical findings in patients.
Methods: Rabbits received IAC melphalan (0.4-0.8 mg/kg), carboplatin (25-50 mg), or saline, either by direct ophthalmic artery cannulation, or with a technique emulating nonocclusion. Ocular structure/function were assessed with examination, electroretinography (ERG), fundus photography, fluorescein angiography, optical coherence tomography (OCT), and OCT angiography, prior to and 5 to 6 weeks after IAC. Blood counts were obtained weekly. We reviewed our last 50 IAC treatments in patients for evidence of ocular or systemic complications.
Results: No toxicity was seen in the saline control group. With standard (0.4 mg/kg) melphalan, no vascular/microvascular abnormalities were seen with either technique. However, severe microvascular pruning and arteriolar occlusions were seen occasionally at 0.8 mg/kg doses. ERG reductions were dose-dependent. Histology showed melphalan dose-dependent degeneration in all retinal layers, restricted geographically to areas of greatest vascular density. Carboplatin caused massive edema of ocular/periocular structures. IAC patients experienced occasional periocular swelling/rash, and only rarely experienced retinopathy or vascular events/hemorrhage in eyes treated multiple times with triple (melphalan/carboplatin/topotecan) therapy. Transient neutropenia occurred after 46% of IAC procedures, generally after triple therapy.
Conclusions: IAC toxicity appears to be related to the specific drug being used and is dose-dependent, rather than related to the IAC procedure itself or the specific technique selected. These rabbit findings are corroborated by our clinical findings in patients.
Nakashima K, Akamatsu H, Murakami H, et al.
Carboplatin Plus Nab-paclitaxel in Performance Status 2 Patients With Advanced Non-small-cell Lung Cancer.
Anticancer Res. 2019; 39(3):1463-1468 [PubMed] Related Publications
Carboplatin Plus Nab-paclitaxel in Performance Status 2 Patients With Advanced Non-small-cell Lung Cancer.
Anticancer Res. 2019; 39(3):1463-1468 [PubMed] Related Publications
BACKGROUND/AIM: This phase I/II study aimed at assessing the efficacy of combination therapy with carboplatin (CBDCA) on day 1 and nab-paclitaxel (Nab-PTX) on days 1 and 8 of a 21-day cycle in performance status (PS) 2 patients with non-small-cell lung cancer (NSCLC).
PATIENTS AND METHODS: PS 2 patients with NSCLC were enrolled into a phase I study using a 3 + 3 design. Once the recommended phase II dose (RP2D) was established, the patients were enrolled into phase II.
RESULTS: Based on the phase I findings, the RP2D was determined as CBDCA area under the curve 6 mg/ml/min and Nab-PTX 100 mg/m
CONCLUSION: CBDCA plus Nab-PTX therapy is a promising treatment strategy for PS 2 patients with NSCLC.
PATIENTS AND METHODS: PS 2 patients with NSCLC were enrolled into a phase I study using a 3 + 3 design. Once the recommended phase II dose (RP2D) was established, the patients were enrolled into phase II.
RESULTS: Based on the phase I findings, the RP2D was determined as CBDCA area under the curve 6 mg/ml/min and Nab-PTX 100 mg/m
CONCLUSION: CBDCA plus Nab-PTX therapy is a promising treatment strategy for PS 2 patients with NSCLC.
Torrisi R, Zuradelli M, Agostinetto E, et al.
Platinum salts in the treatment of BRCA-associated breast cancer: A true targeted chemotherapy?
Crit Rev Oncol Hematol. 2019; 135:66-75 [PubMed] Related Publications
Platinum salts in the treatment of BRCA-associated breast cancer: A true targeted chemotherapy?
Crit Rev Oncol Hematol. 2019; 135:66-75 [PubMed] Related Publications
Germline pathogenic mutations in breast cancer (BC) susceptibility genes (gBRCA1/2) are the most frequent inherited alterations in BC and are involved in the homologous recombination pathway, the principal mechanism of DNA double strand break repair. Platinum salts which act as DNA cross-linking agents are therefore more likely to be active in BRCA-deficient tumors. Women with gBRCA-associated tumors, particularly with triple negative BC, receiving neoadjuvant platinum containing regimens achieved higher pCR rates as compared to wild-type BC. However in two large randomized trials the addition of carboplatin significantly increased pCR rate only in wild-type tumors. On the contrary, the randomized TNT trial showed a significant benefit for carboplatin vs docetaxel in terms of response rate and PFS specifically in patients with advanced gBRCA -associated tumors. Biomarkers of sensitivity to DNA damaging agents beyond gBRCA mutations predicting activity of platinum salts have been proposed and should be validated prospectively.
Cruz-Galvez CC, Ortiz-Lazareno PC, Pedraza-Brindis EJ, et al.
Pentoxifylline Enhances the Apoptotic Effect of Carboplatin in Y79 Retinoblastoma Cells.
In Vivo. 2019 Mar-Apr; 33(2):401-412 [PubMed] Free Access to Full Article Related Publications
Pentoxifylline Enhances the Apoptotic Effect of Carboplatin in Y79 Retinoblastoma Cells.
In Vivo. 2019 Mar-Apr; 33(2):401-412 [PubMed] Free Access to Full Article Related Publications
BACKGROUND/AIM: Retinoblastoma (RB) is the most common primary intraocular malignancy. Carboplatin (CPt) is a DNA damage-inducing agent that is widely used for the treatment of RB. Unfortunately, this drug also activates the transcription factor nuclear factor-kappa B (NF-ĸB), leading to promotion of tumor survival. Pentoxifylline (PTX) is a drug that inhibits the phosphorylation of I kappa B-alpha (IĸBα) in serines 32 and 36, and this disrupts NF-ĸB activity that promotes tumor survival. The goal of this study was to evaluate the effect of the PTX on the antitumor activity of CPt.
MATERIALS AND METHODS: Y79 RB cells were treated with CPt, PTX, or both. Cell viability, apoptosis, loss of mitochondrial membrane potential, the activity of caspase-9, -8, and -3, cytochrome c release, cell-cycle progression, p53, and phosphorylation of IĸBα, and pro- and anti-apoptotic genes were evaluated.
RESULTS: Both drugs significantly affected the viability of the Y79 RB cells in a time- and dose-dependent manner. The PTX+CPt combination exhibited the highest rate of apoptosis, a decrease in cell viability and significant caspase activation, as well as loss of mitochondrial membrane potential, release of cytochrome c, and increased p53 protein levels. Cells treated with PTX alone displayed decreased I kappa B-alpha phosphorylation, compared to the CPt treated group. In addition, the PTX+CPt combination treatment induced up-regulation of the proapoptotic genes Bax, Bad, Bak, and caspases- 3, -8, and -9, compared to the CPt and PTX individual treated groups.
CONCLUSION: PTX induces apoptosis per se and increases the CPt-induced apoptosis, augmenting its antitumor effectiveness.
MATERIALS AND METHODS: Y79 RB cells were treated with CPt, PTX, or both. Cell viability, apoptosis, loss of mitochondrial membrane potential, the activity of caspase-9, -8, and -3, cytochrome c release, cell-cycle progression, p53, and phosphorylation of IĸBα, and pro- and anti-apoptotic genes were evaluated.
RESULTS: Both drugs significantly affected the viability of the Y79 RB cells in a time- and dose-dependent manner. The PTX+CPt combination exhibited the highest rate of apoptosis, a decrease in cell viability and significant caspase activation, as well as loss of mitochondrial membrane potential, release of cytochrome c, and increased p53 protein levels. Cells treated with PTX alone displayed decreased I kappa B-alpha phosphorylation, compared to the CPt treated group. In addition, the PTX+CPt combination treatment induced up-regulation of the proapoptotic genes Bax, Bad, Bak, and caspases- 3, -8, and -9, compared to the CPt and PTX individual treated groups.
CONCLUSION: PTX induces apoptosis per se and increases the CPt-induced apoptosis, augmenting its antitumor effectiveness.
Vrdoljak J, Boban T, Petrić Miše B, et al.
Efficacy and safety of TC dose-dense chemotherapy as first-line treatment of epithelial ovarian cancer: a single-institution retrospective cohort study.
Jpn J Clin Oncol. 2019; 49(4):347-353 [PubMed] Related Publications
Efficacy and safety of TC dose-dense chemotherapy as first-line treatment of epithelial ovarian cancer: a single-institution retrospective cohort study.
Jpn J Clin Oncol. 2019; 49(4):347-353 [PubMed] Related Publications
BACKGROUND: The optimal first-line therapy of advanced ovarian cancer still remains questionable: standard paclitaxel-carboplatin (TC), dose-dense TC, intraperitoneal chemotherapy or TC plus bevacizumab. In this study, we present the real-life results of dose-dense treatment of the single-institution on Caucasian population.
METHODS: A retrospective cohort study was used on consecutive samples of 74 patients treated with the conventional 3-weekly TC protocol (2008-11) and on 70 treated with TC dose-dense protocol (2012-16). The primary endpoint of this study was overall survival (OS). Secondary endpoints were progression free-survival (PFS) and toxicity. We made adjustments for age, pathohistological type, tumor grade, stage and postoperative residual disease by Cox regression.
RESULTS: After adjustment for pre-planned clinical and sociodemographic factors, patients treated with dose-dense protocol showed a significantly lower hazard for dying from any cause, than patients treated with conventional protocol (HR = 0.50; 95% CI 0.26-0.98; P = 0.042). Median OS, at 60 months follow-up had not been reached in the dose-dense group, while in the standard treatment group was 48 months (95% CI 33-62). Unadjusted PFS was significantly longer in the dose-dense group (HR = 0.58; 95% CI 0.38-0.88; P = 0.011), but not after the adjustment (P = 0.096). Generally, the level of toxicity was similar in both groups of patients. The need for blood transfusions and usage of filgrastim was significantly higher in the TC dd group. The incidence of neutropenia and thrombocytopenia Grade 3 or 4 were not significantly different in both regimens.
CONCLUSIONS: Our retrospective study has shown the superior efficacy and comparable toxicity of dose-dense chemotherapy regimen over the conventional regimen in treatment of ovarian cancer on Caucasian population at a single-institution.
METHODS: A retrospective cohort study was used on consecutive samples of 74 patients treated with the conventional 3-weekly TC protocol (2008-11) and on 70 treated with TC dose-dense protocol (2012-16). The primary endpoint of this study was overall survival (OS). Secondary endpoints were progression free-survival (PFS) and toxicity. We made adjustments for age, pathohistological type, tumor grade, stage and postoperative residual disease by Cox regression.
RESULTS: After adjustment for pre-planned clinical and sociodemographic factors, patients treated with dose-dense protocol showed a significantly lower hazard for dying from any cause, than patients treated with conventional protocol (HR = 0.50; 95% CI 0.26-0.98; P = 0.042). Median OS, at 60 months follow-up had not been reached in the dose-dense group, while in the standard treatment group was 48 months (95% CI 33-62). Unadjusted PFS was significantly longer in the dose-dense group (HR = 0.58; 95% CI 0.38-0.88; P = 0.011), but not after the adjustment (P = 0.096). Generally, the level of toxicity was similar in both groups of patients. The need for blood transfusions and usage of filgrastim was significantly higher in the TC dd group. The incidence of neutropenia and thrombocytopenia Grade 3 or 4 were not significantly different in both regimens.
CONCLUSIONS: Our retrospective study has shown the superior efficacy and comparable toxicity of dose-dense chemotherapy regimen over the conventional regimen in treatment of ovarian cancer on Caucasian population at a single-institution.
Bergamino M, Rullan AJ, Saigí M, et al.
Fasting plasma glucose is an independent predictor of survival in patients with locally advanced non-small cell lung cancer treated with concurrent chemoradiotherapy.
BMC Cancer. 2019; 19(1):165 [PubMed] Free Access to Full Article Related Publications
Fasting plasma glucose is an independent predictor of survival in patients with locally advanced non-small cell lung cancer treated with concurrent chemoradiotherapy.
BMC Cancer. 2019; 19(1):165 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Diabetes is related with increased cancer mortality across multiple cancer types. Its role in lung cancer mortality is still unclear. We aim to determine the prognostic value of fasting plasma glucose (FPG) and diabetes mellitus in patients with locally advanced non-small cell lung cancer (NSCLC) treated with concurrent chemoradiotherapy.
METHODS: One-hundred seventy patients with stage III NSCLC received definitive concurrent chemoradiotherapy from 2010 to 2014. Clinico-pathological data and clinical outcome was retrospectively registered. Fifty-six patients (33%), met criteria for type 2 diabetes mellitus (T2DM) at baseline. The prognostic value of FPG and other clinical variables was assessed. Overall survival (OS) and progression-free survival (PFS) were estimated using the Kaplan-Meier method and Cox proportional models and log-rank test were used.
RESULTS: With a median follow-up of 36 months, median PFS was 8.0 months and median OS was 15.0 months in patients with FPG ≥7 mmol/L compared to 20 months (HR 1.13; 95% CI 1.07-1.19, p < 0.001) and 31 months (HR 1.09; 95% CI 1.04-1.15; p < 0.001) respectively, for patients with FPG < 7 mmol/L. In the multivariate analysis of the entire cohort adjusted by platinum compound and comorbidities, high levels of FPG as a continuous variable (HR 1.14; 95% CI 1.07-1.21; p < 0.001), the presence of comorbidity (HR 1.72; 95% CI 1.12-2.63; p = 0.012), and treatment with carboplatin (HR 1.95; 95% CI 1.26-2.99; p = 0.002) were independent predictors for shorter OS. In additional multivariate models considering non-diabetic patients as a reference group, diabetic patients with poor metabolic control (HbA1c > 8.5%) (HR 4.53; 95% CI 2.21-9.30; p < 0.001) and those receiving insulin (HR 3.22; 95% CI 1.90-5.46 p < 0.001) had significantly independent worse OS.
CONCLUSION: Baseline FPG level is an independent predictor of survival in our cohort of patients with locally advanced NSCLC treated with concurrent chemoradiotherapy. Studies in larger cohorts of patients are warranted to confirm this relevant association.
METHODS: One-hundred seventy patients with stage III NSCLC received definitive concurrent chemoradiotherapy from 2010 to 2014. Clinico-pathological data and clinical outcome was retrospectively registered. Fifty-six patients (33%), met criteria for type 2 diabetes mellitus (T2DM) at baseline. The prognostic value of FPG and other clinical variables was assessed. Overall survival (OS) and progression-free survival (PFS) were estimated using the Kaplan-Meier method and Cox proportional models and log-rank test were used.
RESULTS: With a median follow-up of 36 months, median PFS was 8.0 months and median OS was 15.0 months in patients with FPG ≥7 mmol/L compared to 20 months (HR 1.13; 95% CI 1.07-1.19, p < 0.001) and 31 months (HR 1.09; 95% CI 1.04-1.15; p < 0.001) respectively, for patients with FPG < 7 mmol/L. In the multivariate analysis of the entire cohort adjusted by platinum compound and comorbidities, high levels of FPG as a continuous variable (HR 1.14; 95% CI 1.07-1.21; p < 0.001), the presence of comorbidity (HR 1.72; 95% CI 1.12-2.63; p = 0.012), and treatment with carboplatin (HR 1.95; 95% CI 1.26-2.99; p = 0.002) were independent predictors for shorter OS. In additional multivariate models considering non-diabetic patients as a reference group, diabetic patients with poor metabolic control (HbA1c > 8.5%) (HR 4.53; 95% CI 2.21-9.30; p < 0.001) and those receiving insulin (HR 3.22; 95% CI 1.90-5.46 p < 0.001) had significantly independent worse OS.
CONCLUSION: Baseline FPG level is an independent predictor of survival in our cohort of patients with locally advanced NSCLC treated with concurrent chemoradiotherapy. Studies in larger cohorts of patients are warranted to confirm this relevant association.
Rojanaporn D, Chanthanaphak E, Boonyaopas R, et al.
Intra-Arterial Chemotherapy for Retinoblastoma: 8-Year Experience from a Tertiary Referral Institute in Thailand.
Asia Pac J Ophthalmol (Phila). 2019 May-Jun; 8(3):211-217 [PubMed] Related Publications
Intra-Arterial Chemotherapy for Retinoblastoma: 8-Year Experience from a Tertiary Referral Institute in Thailand.
Asia Pac J Ophthalmol (Phila). 2019 May-Jun; 8(3):211-217 [PubMed] Related Publications
PURPOSE: To study the safety and efficacy of intra-arterial chemotherapy (IAC) as a treatment for intraocular retinoblastoma in Thailand.
DESIGN: Retrospective, interventional case series.
METHODS: In this study, IAC was performed as primary or secondary treatment for patients with intraocular retinoblastoma using melphalan with or without additional topotecan or carboplatin. Survival rate, globe salvage rate, and treatment complications were recorded and analyzed.
RESULTS: Of 27 eyes of 26 patients with retinoblastoma, 7 (26%) had IAC as primary treatment and 20 (74%) had IAC as secondary treatment. The eyes were classified by International Classification of Retinoblastoma (ICRB) as group B (n = 3, 11%), group C (n = 1, 4%), group D (n = 12, 44%), and group E (n = 11, 41%). Catheterization was successful in 75 (94%) of 80 sessions. The median number of IAC sessions was 3 (range, 1-7). At a mean follow-up of 32 months (range, 3-95 months), the overall globe salvage rate was 52%, with 100% in groups B and C, 75% in group D, and 9% in group E. Complications of IAC included occlusive vasculopathy (n = 4, 15%), vitreous hemorrhage (n = 3, 11%), retinal artery precipitation (n = 2, 7%), strabismus (n = 2, 7%), and transient ischemic attack (n = 1, 4%). The overall survival rate was 96% (n = 25).
CONCLUSIONS: Our experience suggests that IAC is a safe and effective treatment for patients with ICRB group B, C, D, and some group E retinoblastoma. Careful patient selection and experienced surgeons are critical for achieving the best treatment outcome.
DESIGN: Retrospective, interventional case series.
METHODS: In this study, IAC was performed as primary or secondary treatment for patients with intraocular retinoblastoma using melphalan with or without additional topotecan or carboplatin. Survival rate, globe salvage rate, and treatment complications were recorded and analyzed.
RESULTS: Of 27 eyes of 26 patients with retinoblastoma, 7 (26%) had IAC as primary treatment and 20 (74%) had IAC as secondary treatment. The eyes were classified by International Classification of Retinoblastoma (ICRB) as group B (n = 3, 11%), group C (n = 1, 4%), group D (n = 12, 44%), and group E (n = 11, 41%). Catheterization was successful in 75 (94%) of 80 sessions. The median number of IAC sessions was 3 (range, 1-7). At a mean follow-up of 32 months (range, 3-95 months), the overall globe salvage rate was 52%, with 100% in groups B and C, 75% in group D, and 9% in group E. Complications of IAC included occlusive vasculopathy (n = 4, 15%), vitreous hemorrhage (n = 3, 11%), retinal artery precipitation (n = 2, 7%), strabismus (n = 2, 7%), and transient ischemic attack (n = 1, 4%). The overall survival rate was 96% (n = 25).
CONCLUSIONS: Our experience suggests that IAC is a safe and effective treatment for patients with ICRB group B, C, D, and some group E retinoblastoma. Careful patient selection and experienced surgeons are critical for achieving the best treatment outcome.
Yokoi T, Minami S, Shiroyama T, et al.
A Phase II Study of Tailored-dose S-1 Plus Carboplatin Followed by Maintenance S-1 for Advanced Squamous Cell Lung Cancer: OSAKA-LCSG 1102.
Intern Med. 2019; 58(10):1405-1410 [PubMed] Free Access to Full Article Related Publications
A Phase II Study of Tailored-dose S-1 Plus Carboplatin Followed by Maintenance S-1 for Advanced Squamous Cell Lung Cancer: OSAKA-LCSG 1102.
Intern Med. 2019; 58(10):1405-1410 [PubMed] Free Access to Full Article Related Publications
Objective A subset analysis of the LETS study suggested that S-1 plus carboplatin was more beneficial than paclitaxel plus carboplatin in terms of the overall survival (OS) in squamous cell lung cancer. However, the benefit of maintenance therapy for squamous cell non-small cell lung cancer (NSCLC) patients is still unknown. We herein report a phase II study to evaluate the efficacy and safety of a tailored dose of S-1 plus carboplatin followed by maintenance S-1 in chemotherapy-naive advanced squamous cell NSCLC. Methods Patients received carboplatin on day 1 plus S-1 on days 1 to 14 every 21 days. The dose of S-1 was determined by the body surface area and creatinine clearance. After four cycles of induction, non-progressive patients continued to receive S-1 until disease progression or unacceptable toxicity occurred. The primary endpoint was an objective response rate (RR) with a threshold value of 15%. The secondary endpoints were the progression-free survival (PFS) and OS from enrollment, the PFS in the maintenance phase, and safety. Results In the 33 patients analyzed, the rate of patients who met the primary endpoint was 30.3% (95% confidence interval: 15.6-48.7%), and the disease control rate was 75.8%. The median PFS and OS were 3.5 and 11.3 months, respectively. Ten patients received maintenance S-1, and the median PFS from the beginning of induction treatment was 5.3 months. Grade 3/4 toxicities with a frequency of more than 5% were all controllable. Conclusion Tailored-dose S-1 plus carboplatin followed by maintenance S-1 is an effective and feasible treatment for advanced squamous cell NSCLC.
Hamauchi S, Yokota T, Mizumachi T, et al.
Safety and efficacy of concurrent carboplatin or cetuximab plus radiotherapy for locally advanced head and neck cancer patients ineligible for treatment with cisplatin.
Int J Clin Oncol. 2019; 24(5):468-475 [PubMed] Related Publications
Safety and efficacy of concurrent carboplatin or cetuximab plus radiotherapy for locally advanced head and neck cancer patients ineligible for treatment with cisplatin.
Int J Clin Oncol. 2019; 24(5):468-475 [PubMed] Related Publications
BACKGROUND: Locally advanced squamous cell carcinoma of the head and neck (LASCCHN) is usually treated with cisplatin (CDDP)-based chemoradiotherapy, except when patients are elderly or have renal, cardiac, or neurogenic dysfunction. This study compared the safety and efficacy of concurrent carboplatin (CBDCA) to cetuximab (Cmab) plus radiotherapy (RT) in patients ineligible for CDDP treatment.
METHODS: We retrospectively analyzed LASCCHN patients who received CBDCA plus RT (n = 29) or Cmab plus RT (n = 18) due to ineligibility for CDDP treatment at two Japanese institutions between August 2006 and December 2015.
RESULTS: Patients characteristics for CBDCA plus RT and Cmab plus RT were: median age, 74 and 75 years; 0-1 performance status, 90% and 100%; main primary tumor site, hypopharynx 52% (n = 15) and oropharynx 39% (n = 7); and stage IV, 90% (n = 26) and 50% (n = 9), respectively. With a median follow-up time of 60.0 months for CBDCA plus RT and 53.6 months for Cmab plus RT, 3-year locoregional control rates were 56% versus 58%, and median progression-free survival was 42.7 versus 11.6 months. CBDCA plus RT was associated with more grade 3/4 hematologic toxicities, including neutropenia and thrombocytopenia, whereas Cmab plus RT was associated with more grade 3/4 oral mucositis and radiation dermatitis.
CONCLUSIONS: CBDCA or Cmab as a concurrent systemic therapy with RT is a possible treatment option for LASCCHN patients ineligible for CDDP treatment, although attention to hematological toxicity should be paid.
METHODS: We retrospectively analyzed LASCCHN patients who received CBDCA plus RT (n = 29) or Cmab plus RT (n = 18) due to ineligibility for CDDP treatment at two Japanese institutions between August 2006 and December 2015.
RESULTS: Patients characteristics for CBDCA plus RT and Cmab plus RT were: median age, 74 and 75 years; 0-1 performance status, 90% and 100%; main primary tumor site, hypopharynx 52% (n = 15) and oropharynx 39% (n = 7); and stage IV, 90% (n = 26) and 50% (n = 9), respectively. With a median follow-up time of 60.0 months for CBDCA plus RT and 53.6 months for Cmab plus RT, 3-year locoregional control rates were 56% versus 58%, and median progression-free survival was 42.7 versus 11.6 months. CBDCA plus RT was associated with more grade 3/4 hematologic toxicities, including neutropenia and thrombocytopenia, whereas Cmab plus RT was associated with more grade 3/4 oral mucositis and radiation dermatitis.
CONCLUSIONS: CBDCA or Cmab as a concurrent systemic therapy with RT is a possible treatment option for LASCCHN patients ineligible for CDDP treatment, although attention to hematological toxicity should be paid.
Zhou H, Zhao H, Liu H, et al.
Influence of carboplatin on the proliferation and apoptosis of ovarian cancer cells through mTOR/p70s6k signaling pathway.
J BUON. 2018 Nov-Dec; 23(6):1732-1738 [PubMed] Related Publications
Influence of carboplatin on the proliferation and apoptosis of ovarian cancer cells through mTOR/p70s6k signaling pathway.
J BUON. 2018 Nov-Dec; 23(6):1732-1738 [PubMed] Related Publications
PURPOSE: To investigate the influence of carboplatin on the proliferation and apoptosis of ovarian cancer cells through mTOR/P70S6K signaling pathway.
METHODS: The mRNA and protein expressions were detected via Western blotting and RT-PCR to study whether the mTOR/p70S6K signaling pathway was activated in OVCAR-3 and Caov-3 ovarian cancer cell lines. After cells were treated with different concentrations of carboplatin, the mRNA and protein expressions of mTOR, p70S6K and 4E-BP1 were detected via RT-PCR and Western blotting. OVCAR-3 cells were treated with 20 and 50 μM carboplatin for 4 hrs, and then apoptosis was analyzed and assessed. OVCAR-3 cells were treated with different concentrations of carboplatin (20, 50, 100, 150 and 200 μM) for 24 and 48 hrs, respectively.
RESULTS: The mTOR signaling pathway was activated in OVCAR-3 and Caov-3 ovarian cancer cell lines. The mRNA level of mTOR in Caov-3 cells was higher, but that of p70S6K was lower. Carboplatin significantly reduced the mRNA expression of mTOR (p<0.01), whereas the mRNA expressions of p70S6K and 4E-BP1 in carboplatin-treated cells were increased in a dose-dependent manner (p<0.01). Carboplatin inhibited the mTOR protein expression in a dose-dependent manner (p<0.01). The proliferation of OVCAR-3 cells exposed to carboplatin was reduced compared with that of untreated cells (p<0.01), and the inhibitory effect of carboplatin on the proliferation of OVCAR-3 cells was time- and dose-dependent.
CONCLUSION: The mTOR/p70S6K pathway was activated in ovarian cancer. Carboplatin could rapidly inhibit the expression of mTOR, and the phosphorylation of its major downstream effectors p70S6K and 4E-binding protein 1 (4E-BP1) arrested cells in G0/G1 phase and induced ovarian cancer cell apoptosis.
METHODS: The mRNA and protein expressions were detected via Western blotting and RT-PCR to study whether the mTOR/p70S6K signaling pathway was activated in OVCAR-3 and Caov-3 ovarian cancer cell lines. After cells were treated with different concentrations of carboplatin, the mRNA and protein expressions of mTOR, p70S6K and 4E-BP1 were detected via RT-PCR and Western blotting. OVCAR-3 cells were treated with 20 and 50 μM carboplatin for 4 hrs, and then apoptosis was analyzed and assessed. OVCAR-3 cells were treated with different concentrations of carboplatin (20, 50, 100, 150 and 200 μM) for 24 and 48 hrs, respectively.
RESULTS: The mTOR signaling pathway was activated in OVCAR-3 and Caov-3 ovarian cancer cell lines. The mRNA level of mTOR in Caov-3 cells was higher, but that of p70S6K was lower. Carboplatin significantly reduced the mRNA expression of mTOR (p<0.01), whereas the mRNA expressions of p70S6K and 4E-BP1 in carboplatin-treated cells were increased in a dose-dependent manner (p<0.01). Carboplatin inhibited the mTOR protein expression in a dose-dependent manner (p<0.01). The proliferation of OVCAR-3 cells exposed to carboplatin was reduced compared with that of untreated cells (p<0.01), and the inhibitory effect of carboplatin on the proliferation of OVCAR-3 cells was time- and dose-dependent.
CONCLUSION: The mTOR/p70S6K pathway was activated in ovarian cancer. Carboplatin could rapidly inhibit the expression of mTOR, and the phosphorylation of its major downstream effectors p70S6K and 4E-binding protein 1 (4E-BP1) arrested cells in G0/G1 phase and induced ovarian cancer cell apoptosis.
Song Y, Liu Y, Lin M, et al.
Efficacy of neoadjuvant platinum-based chemotherapy during the second and third trimester of pregnancy in women with cervical cancer: an updated systematic review and meta-analysis.
Drug Des Devel Ther. 2019; 13:79-102 [PubMed] Free Access to Full Article Related Publications
Efficacy of neoadjuvant platinum-based chemotherapy during the second and third trimester of pregnancy in women with cervical cancer: an updated systematic review and meta-analysis.
Drug Des Devel Ther. 2019; 13:79-102 [PubMed] Free Access to Full Article Related Publications
Purpose: To evaluate the efficacy and safety of neoadjuvant platinum-based chemotherapy during pregnancy in women with cervical cancer.
Methods: The PubMed, Embase, and Cochrane Library databases were fully searched to find eligible studies regarding platinum use during pregnancy in women with cervical cancer from January 1980 to September 2018. Data were extracted from the selected studies independently by two authors. Descriptive statistics were calculated for categorical data (frequency and percentage) and numeration data (mean and SD for normally distributed data and median and range for abnormally distributed data). Survival analyses were performed using Kaplan-Meier survival curves and log-rank tests to estimate overall survival and progression-free survival for all patients.
Results: A total of 39 studies including 88 cervical cancer patients with platinum administration during pregnancy were selected in this meta-analysis, and 64 women provided International Federation of Gynecology and Obstetrics stage information. Among the latter, 56 of 64 (87.5%) were diagnosed with early stages (I and IIA) and the remaining 8 of 64 (12.5%) had advanced stages (IIB, III, and IV). In relation to cisplatin, 86 pregnant women were identified, whereas only 2 pregnant women with carboplatin application were retrieved. Overall, 88 newborns were delivered from 84 pregnancies, including two sets of twins and one set of triplets, among which 71 neonates (71 of 88, 80.7%) were completely healthy at birth. All children were healthy at the end of follow-up (median 17 months, range 0-149.5 months), except one who was diagnosed with retroperitoneal embryonal rhabdomyosarcoma at 5 years old and one who had acute myeloid leukemia at 22 months of age. At the end of follow-up (range 4.75-156 months), 16 of 81 (19.8%) patients were diagnosed with recurrence of cervical cancer, and 11 (90%) of those died because of cancer relapse. Neither median overall survival nor median progression-free survival were reached.
Conclusion: Our results demonstrated that neoadjuvant platinum-based chemotherapy could be a favorable choice for the management of patients with cervical cancer during the second and third trimesters. To reduce the side effects of chemotherapy, cisplatin might be good to use as monotherapy in these patients.
Methods: The PubMed, Embase, and Cochrane Library databases were fully searched to find eligible studies regarding platinum use during pregnancy in women with cervical cancer from January 1980 to September 2018. Data were extracted from the selected studies independently by two authors. Descriptive statistics were calculated for categorical data (frequency and percentage) and numeration data (mean and SD for normally distributed data and median and range for abnormally distributed data). Survival analyses were performed using Kaplan-Meier survival curves and log-rank tests to estimate overall survival and progression-free survival for all patients.
Results: A total of 39 studies including 88 cervical cancer patients with platinum administration during pregnancy were selected in this meta-analysis, and 64 women provided International Federation of Gynecology and Obstetrics stage information. Among the latter, 56 of 64 (87.5%) were diagnosed with early stages (I and IIA) and the remaining 8 of 64 (12.5%) had advanced stages (IIB, III, and IV). In relation to cisplatin, 86 pregnant women were identified, whereas only 2 pregnant women with carboplatin application were retrieved. Overall, 88 newborns were delivered from 84 pregnancies, including two sets of twins and one set of triplets, among which 71 neonates (71 of 88, 80.7%) were completely healthy at birth. All children were healthy at the end of follow-up (median 17 months, range 0-149.5 months), except one who was diagnosed with retroperitoneal embryonal rhabdomyosarcoma at 5 years old and one who had acute myeloid leukemia at 22 months of age. At the end of follow-up (range 4.75-156 months), 16 of 81 (19.8%) patients were diagnosed with recurrence of cervical cancer, and 11 (90%) of those died because of cancer relapse. Neither median overall survival nor median progression-free survival were reached.
Conclusion: Our results demonstrated that neoadjuvant platinum-based chemotherapy could be a favorable choice for the management of patients with cervical cancer during the second and third trimesters. To reduce the side effects of chemotherapy, cisplatin might be good to use as monotherapy in these patients.
Milic M, Hall M, Hawkins A, et al.
A Qualitative Analysis of the Impact of Carboplatin AUC 10 on Physical, Work Functioning and Bone Marrow Toxicity Among Seminoma Patients - A Single-centre Experience.
In Vivo. 2019 Jan-Feb; 33(1):233-237 [PubMed] Free Access to Full Article Related Publications
A Qualitative Analysis of the Impact of Carboplatin AUC 10 on Physical, Work Functioning and Bone Marrow Toxicity Among Seminoma Patients - A Single-centre Experience.
In Vivo. 2019 Jan-Feb; 33(1):233-237 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Single-agent carboplatin at area under the curve 10 (AUC10) is an effective treatment for metastatic seminoma. As far as we are aware of, there have been no studies reporting its effects on short-term quality of life. The objective was to study the efficacy, safety and tolerability, using health-related quality of life, of carboplatin AUC10 chemotherapy in patients with metastatic seminoma.
PATIENTS AND METHODS: Forty-four patients with metastatic seminoma treated at Mount Vernon Cancer Centre with carboplatin AUC10 were included in this study. Response to treatment was determined by radiological imaging (Response Evaluation Criteria in Solid Tumors v 1.1) and serum tumour markers. Toxicities were evaluated using the Common Terminology Criteria for Adverse Events Version 4.0. Quality of life treatment-related toxicities were assessed during treatment at pre-chemotherapy assessments. After treatment, toxicity was assessed using a defined telephone questionnaire consisting of four questions relating to hair loss, hearing impairment, days absent from work, and neuropathy.
RESULTS: At a median follow-up of 27.5 (range=4-84) months, no patient had experienced relapse. Grade 3/4 neutropenia was seen in 15 (35%) patients, nine (21%) required prophylactic granulocyte colony-stimulating factor, 13 (30%) patients had grade 3/4 thrombocytopenia. Commonest non-haematological toxicities were fatigue in 28 (65%) and nausea 14 (33%) patients. They were grade 1 in 82% and 92% of cases, respectively. Six out of 44 (14%) had residual tinnitus. One patient had residual grade 1 peripheral neuropathy. Ten patients continued to work throughout treatment and two patients were retired. Of the remaining patients, 16 (37%), took fewer than 5 days off work.
CONCLUSION: Carboplatin AUC10 is a safe and effective treatment for stage II/III seminoma with better health-related quality of life than experienced with combination cisplatin-based chemotherapy.
PATIENTS AND METHODS: Forty-four patients with metastatic seminoma treated at Mount Vernon Cancer Centre with carboplatin AUC10 were included in this study. Response to treatment was determined by radiological imaging (Response Evaluation Criteria in Solid Tumors v 1.1) and serum tumour markers. Toxicities were evaluated using the Common Terminology Criteria for Adverse Events Version 4.0. Quality of life treatment-related toxicities were assessed during treatment at pre-chemotherapy assessments. After treatment, toxicity was assessed using a defined telephone questionnaire consisting of four questions relating to hair loss, hearing impairment, days absent from work, and neuropathy.
RESULTS: At a median follow-up of 27.5 (range=4-84) months, no patient had experienced relapse. Grade 3/4 neutropenia was seen in 15 (35%) patients, nine (21%) required prophylactic granulocyte colony-stimulating factor, 13 (30%) patients had grade 3/4 thrombocytopenia. Commonest non-haematological toxicities were fatigue in 28 (65%) and nausea 14 (33%) patients. They were grade 1 in 82% and 92% of cases, respectively. Six out of 44 (14%) had residual tinnitus. One patient had residual grade 1 peripheral neuropathy. Ten patients continued to work throughout treatment and two patients were retired. Of the remaining patients, 16 (37%), took fewer than 5 days off work.
CONCLUSION: Carboplatin AUC10 is a safe and effective treatment for stage II/III seminoma with better health-related quality of life than experienced with combination cisplatin-based chemotherapy.
Damiani E, Solorio JA, Doyle AP, Wallace HM
How reliable are in vitro IC
Toxicol Lett. 2019; 302:28-34 [PubMed] Related Publications
How reliable are in vitro IC
Toxicol Lett. 2019; 302:28-34 [PubMed] Related Publications
Increasing evidence shows that discrepancies exist among in vitro cytotoxicity methods resulting in unreliable drug toxicity profiles. This is particularly criticial for cell lines such as gliomas which are histologically and genetically heterogeneous. The high level of variation in these cells makes comparative analysis difficult and is a severe limitation for the usefulness of high-throughput screening methods. Here we examine variations between four conventional in vitro cytotoxicity assays (MTT, Alamar Blue, Acid Phosphatase and Trypan Blue) for assessing the viable cell number following treatment of two human glioblastoma cell lines (U87MG and U373MG) with different chemical agents (carboplatin, etoposide, paraquat). The variations in IC
Mouri A, Yamaguchi O, Miyauchi S, et al.
Combination therapy with carboplatin and paclitaxel for small cell lung cancer.
Respir Investig. 2019; 57(1):34-39 [PubMed] Related Publications
Combination therapy with carboplatin and paclitaxel for small cell lung cancer.
Respir Investig. 2019; 57(1):34-39 [PubMed] Related Publications
BACKGROUND: Although small cell lung cancer (SCLC) is an aggressive cancer, few useful treatment options exist after relapse. Information concerning the efficacy and safety of carboplatin plus paclitaxel in patients with SCLC is limited.
METHODS: From April 2007 to October 2016, 318 patients with SCLC received chemotherapy at our institution. The medical records of patients treated with carboplatin and paclitaxel after first-line chemotherapy with platinum plus etoposide or irinotecan were retrospectively analyzed. The objectives were to investigate the frequency at which a carboplatin and paclitaxel regimen was administered to patients with SCLC in clinical practice, and to determine the response rate, progression-free survival (PFS), and tolerability of such agents.
RESULTS: A total of 24 (7.5%) patients (male, n = 21; female, n = 3; median age, 67 years; performance status, 0-1/≥2, 15/8 patients; limited/extensive disease, 6/15 patients; sensitive/refractory relapse, 3/21 patients) were treated with carboplatin plus paclitaxel. This regimen was chosen due to interstitial lung disease (ILD) (n = 17), radiation pneumonitis (n = 3), combination with palliative radiation therapy (n = 2), and the presence of other cancers (n = 2). The response rate was 33.3%, and the disease control rate was 62.5%. The median PFS and overall survival were 4.1 and 8.7 months, respectively. Grade 3/4 hematologic toxicities observed included neutropenia (54.2%), anemia (4.2%), and thrombocytopenia (8.3%). With the exception of grade 3 neuropathies (n = 2), non-hematologic toxicities were mild. No patients experienced an acute exacerbation of ILD.
CONCLUSION: A combination of carboplatin plus paclitaxel as second-line chemotherapy is effective and feasible in patients with SCLC, especially in those with ILD.
METHODS: From April 2007 to October 2016, 318 patients with SCLC received chemotherapy at our institution. The medical records of patients treated with carboplatin and paclitaxel after first-line chemotherapy with platinum plus etoposide or irinotecan were retrospectively analyzed. The objectives were to investigate the frequency at which a carboplatin and paclitaxel regimen was administered to patients with SCLC in clinical practice, and to determine the response rate, progression-free survival (PFS), and tolerability of such agents.
RESULTS: A total of 24 (7.5%) patients (male, n = 21; female, n = 3; median age, 67 years; performance status, 0-1/≥2, 15/8 patients; limited/extensive disease, 6/15 patients; sensitive/refractory relapse, 3/21 patients) were treated with carboplatin plus paclitaxel. This regimen was chosen due to interstitial lung disease (ILD) (n = 17), radiation pneumonitis (n = 3), combination with palliative radiation therapy (n = 2), and the presence of other cancers (n = 2). The response rate was 33.3%, and the disease control rate was 62.5%. The median PFS and overall survival were 4.1 and 8.7 months, respectively. Grade 3/4 hematologic toxicities observed included neutropenia (54.2%), anemia (4.2%), and thrombocytopenia (8.3%). With the exception of grade 3 neuropathies (n = 2), non-hematologic toxicities were mild. No patients experienced an acute exacerbation of ILD.
CONCLUSION: A combination of carboplatin plus paclitaxel as second-line chemotherapy is effective and feasible in patients with SCLC, especially in those with ILD.
Yamamoto M, Suzuki S, Togashi K, et al.
AS602801, an Anticancer Stem Cell Candidate Drug, Reduces Survivin Expression and Sensitizes A2780 Ovarian Cancer Stem Cells to Carboplatin and Paclitaxel.
Anticancer Res. 2018; 38(12):6699-6706 [PubMed] Related Publications
AS602801, an Anticancer Stem Cell Candidate Drug, Reduces Survivin Expression and Sensitizes A2780 Ovarian Cancer Stem Cells to Carboplatin and Paclitaxel.
Anticancer Res. 2018; 38(12):6699-6706 [PubMed] Related Publications
BACKGROUND: AS602801, a novel inhibitor of c-Jun N-terminal kinase (JNK), suppresses tumor initiation capacity and metastatic potential of cancer stem cells (CSCs). However, it remains unknown whether this inhibitor can chemosensitize CSCs.
MATERIALS AND METHODS: Using A2780 CSLC, a CSC line derived from ovarian cancer, this study examined the combinational effects of AS602801 and carboplatin or paclitaxel and explored the mechanism of those effects.
RESULTS: AS602801 chemosensitized A2780 CSLC cells to carboplatin and paclitaxel. With respect to the mechanism of chemosensitization, the expression of survivin, an anti-apoptotic protein, was reduced by AS602801. Pharmacological and genetic inhibition of survivin chemosensitized the cells to carboplatin and paclitaxel. Suppression of survivin by AS602801 was also observed in other types of CSCs and non-CSCs.
CONCLUSION: AS602801, which reduces survivin expression, can chemosensitize ovarian CSCs and is a candidate drug that targets the chemoresistance, tumor-initiating capacity and metastasis of CSCs.
MATERIALS AND METHODS: Using A2780 CSLC, a CSC line derived from ovarian cancer, this study examined the combinational effects of AS602801 and carboplatin or paclitaxel and explored the mechanism of those effects.
RESULTS: AS602801 chemosensitized A2780 CSLC cells to carboplatin and paclitaxel. With respect to the mechanism of chemosensitization, the expression of survivin, an anti-apoptotic protein, was reduced by AS602801. Pharmacological and genetic inhibition of survivin chemosensitized the cells to carboplatin and paclitaxel. Suppression of survivin by AS602801 was also observed in other types of CSCs and non-CSCs.
CONCLUSION: AS602801, which reduces survivin expression, can chemosensitize ovarian CSCs and is a candidate drug that targets the chemoresistance, tumor-initiating capacity and metastasis of CSCs.
Vetter MH, Khan A, Backes FJ, et al.
Outpatient desensitization of patients with moderate (high-risk) to severe platinum hypersensitivity reactions.
Gynecol Oncol. 2019; 152(2):316-321 [PubMed] Related Publications
Outpatient desensitization of patients with moderate (high-risk) to severe platinum hypersensitivity reactions.
Gynecol Oncol. 2019; 152(2):316-321 [PubMed] Related Publications
OBJECTIVES: Platinum hypersensitivity reactions (HSR) affect approximately 5% of the general oncologic population. Here we report the efficacy and safety of outpatient platinum desensitization protocol (PD) in gynecologic oncology patients with moderate (high-risk) to severe platinum HSR.
METHODS: This is a retrospective report of patients with gynecologic malignancies undergoing an outpatient PD for moderate (high-risk) to severe platinum HSR from 2011 to 2017. Patient demographics, chemotherapy histories, and PD outcomes were collected. Descriptive statistics were performed given the exploratory nature of the study.
RESULTS: Forty-eight patients meeting inclusion criteria were identified. Most patients were being treated for ovarian cancer (56.3%) and were receiving carboplatin during their initial platinum HSR (75.0%). Patients received a mean of 10.3 platinum doses prior to their initial HSR. Transient hypertension was the most common sign of moderate (high-risk) HSR while persistent tachycardia was the most common sign of severe HSR. A total of 295 PD cycles were attempted with a successful completion rate of 96.6%. The mean number of PD cycles received by patients was 5.1. Almost 65% of patients experienced breakthrough reactions but over 58% of these breakthrough reactions were isolated to the first PD cycle. Only 8.3% of patients had severe breakthrough reactions, all of whom initially underwent shortened desensitization. Of these 4 patients, 2 successfully underwent desensitization with a prolonged protocol.
CONCLUSION: Outpatient PD is safe and effective in patients with gynecologic malignancies. This may present a feasible option for institutions with multi-disciplinary teams experienced with the management of platinum HSR.
METHODS: This is a retrospective report of patients with gynecologic malignancies undergoing an outpatient PD for moderate (high-risk) to severe platinum HSR from 2011 to 2017. Patient demographics, chemotherapy histories, and PD outcomes were collected. Descriptive statistics were performed given the exploratory nature of the study.
RESULTS: Forty-eight patients meeting inclusion criteria were identified. Most patients were being treated for ovarian cancer (56.3%) and were receiving carboplatin during their initial platinum HSR (75.0%). Patients received a mean of 10.3 platinum doses prior to their initial HSR. Transient hypertension was the most common sign of moderate (high-risk) HSR while persistent tachycardia was the most common sign of severe HSR. A total of 295 PD cycles were attempted with a successful completion rate of 96.6%. The mean number of PD cycles received by patients was 5.1. Almost 65% of patients experienced breakthrough reactions but over 58% of these breakthrough reactions were isolated to the first PD cycle. Only 8.3% of patients had severe breakthrough reactions, all of whom initially underwent shortened desensitization. Of these 4 patients, 2 successfully underwent desensitization with a prolonged protocol.
CONCLUSION: Outpatient PD is safe and effective in patients with gynecologic malignancies. This may present a feasible option for institutions with multi-disciplinary teams experienced with the management of platinum HSR.
Walsh EM, Shalaby A, O'Loughlin M, et al.
Outcome for triple negative breast cancer in a retrospective cohort with an emphasis on response to platinum-based neoadjuvant therapy.
Breast Cancer Res Treat. 2019; 174(1):1-13 [PubMed] Free Access to Full Article Related Publications
Outcome for triple negative breast cancer in a retrospective cohort with an emphasis on response to platinum-based neoadjuvant therapy.
Breast Cancer Res Treat. 2019; 174(1):1-13 [PubMed] Free Access to Full Article Related Publications
PURPOSE: The rate of pathological complete response (pCR) for patients with triple negative breast cancer (TNBC) is increased when carboplatin is added to neo-adjuvant chemotherapy (NACT). However, while phase III trial data showing a survival benefit are awaited, carboplatin is not yet standard-of-care for TNBC. The aim of this study was to examine the rate of pCR and the outcome for those treated with carboplatin and to examine the predictors of response to therapy.
METHODS: The retrospective series comprised 333 consecutive patients with TNBC (median follow-up time, 43 months). Adjuvant chemotherapy was given to 51% (n = 168) of patients and 29% (n = 97) received anthracycline-taxane NACT with carboplatin given to 9% (n = 31) of patients.
RESULTS: Overall, 25% (n = 78) of patients experienced a breast cancer recurrence and 22% (n = 68) died from disease. A pCR breast and pCR breast/axilla was more common in those who received carboplatin (n = 18, 58% and n = 17, 55%, respectively) compared those who did not (n = 23, 36% and n = 18, 28%, respectively) (p = 0.041 and p = 0.011, respectively). By multivariable analysis, carboplatin and high tumor grade were independent predictors of pCR breast/axilla (OR
CONCLUSION: Carboplatin therapy and high tumor grade are associated with a significant increase in the rate of pCR, which is an independent predictor of outcome. These data support the use of carboplatin in NACT for TNBC, while results from phase III studies are awaited.
METHODS: The retrospective series comprised 333 consecutive patients with TNBC (median follow-up time, 43 months). Adjuvant chemotherapy was given to 51% (n = 168) of patients and 29% (n = 97) received anthracycline-taxane NACT with carboplatin given to 9% (n = 31) of patients.
RESULTS: Overall, 25% (n = 78) of patients experienced a breast cancer recurrence and 22% (n = 68) died from disease. A pCR breast and pCR breast/axilla was more common in those who received carboplatin (n = 18, 58% and n = 17, 55%, respectively) compared those who did not (n = 23, 36% and n = 18, 28%, respectively) (p = 0.041 and p = 0.011, respectively). By multivariable analysis, carboplatin and high tumor grade were independent predictors of pCR breast/axilla (OR
CONCLUSION: Carboplatin therapy and high tumor grade are associated with a significant increase in the rate of pCR, which is an independent predictor of outcome. These data support the use of carboplatin in NACT for TNBC, while results from phase III studies are awaited.
Hu XL, Feng JH, Pham TA, et al.
Identification of amentoflavone as a potent highly selective PARP-1 inhibitor and its potentiation on carboplatin in human non-small cell lung cancer.
Phytomedicine. 2018; 50:88-98 [PubMed] Related Publications
Identification of amentoflavone as a potent highly selective PARP-1 inhibitor and its potentiation on carboplatin in human non-small cell lung cancer.
Phytomedicine. 2018; 50:88-98 [PubMed] Related Publications
BACKGROUND: Nuclear protein poly (ADP-ribose) polymerase-1 (PARP-1) is a key enzyme in the repair of DNA and is a promising target in the development of chemosensitizers. This study first investigated the inhibitory effects of amentoflavone (AMF) and its derivatives on PARP-1 and the potentiation of AMF on carboplatin (CBP) in non-small cell lung cancer (NSCLC).
PURPOSE: This study aims to evaluate the inhibitory effect of AMF against PARP-1 and its potentiation on CBP in lung cancer both in vitro and in vivo.
STUDY DESIGN: The inhibitory effect of AMF on PARP-1 was investigated using molecular docking and cell-free model of PARP-1 assay. Its potentiation on CBP in lung cancer was also evaluated.
METHODS: Fluorescence resonance energy transfer assay was used to detect the inhibitory effects of AMF and its analogues on PARP-1. Molecular docking was employed to predict the binding mode of AMF and PARP-1. MTT assay, isobologram analysis, Hoechst staining, and Annexin V-PI double staining were used to confirm the potentiation of AMF on CBP in vitro. siRNA (PARP-1)-A549 cells were used to reveal the action target of AMF. Western blot analysis, immunohistochemistry, and Tunnel assay were employed to evaluate the potentiation of AMF on CBP in A549 xenograft mice.
RESULTS: AMF and its analogues exerted excellent inhibitory effects on PARP-1 with IC
CONCLUSION: All results suggest that AMF can be a potential PARP-1 inhibitor and a candidate adjuvant agent to boost the anticancer effect of CBP in NSCLC.
PURPOSE: This study aims to evaluate the inhibitory effect of AMF against PARP-1 and its potentiation on CBP in lung cancer both in vitro and in vivo.
STUDY DESIGN: The inhibitory effect of AMF on PARP-1 was investigated using molecular docking and cell-free model of PARP-1 assay. Its potentiation on CBP in lung cancer was also evaluated.
METHODS: Fluorescence resonance energy transfer assay was used to detect the inhibitory effects of AMF and its analogues on PARP-1. Molecular docking was employed to predict the binding mode of AMF and PARP-1. MTT assay, isobologram analysis, Hoechst staining, and Annexin V-PI double staining were used to confirm the potentiation of AMF on CBP in vitro. siRNA (PARP-1)-A549 cells were used to reveal the action target of AMF. Western blot analysis, immunohistochemistry, and Tunnel assay were employed to evaluate the potentiation of AMF on CBP in A549 xenograft mice.
RESULTS: AMF and its analogues exerted excellent inhibitory effects on PARP-1 with IC
CONCLUSION: All results suggest that AMF can be a potential PARP-1 inhibitor and a candidate adjuvant agent to boost the anticancer effect of CBP in NSCLC.
Rinnerthaler G, Gampenrieder SP, Petzer A, et al.
Ixazomib in combination with carboplatin in pretreated women with advanced triple-negative breast cancer, a phase I/II trial of the AGMT (AGMT MBC-10 trial).
BMC Cancer. 2018; 18(1):1074 [PubMed] Free Access to Full Article Related Publications
Ixazomib in combination with carboplatin in pretreated women with advanced triple-negative breast cancer, a phase I/II trial of the AGMT (AGMT MBC-10 trial).
BMC Cancer. 2018; 18(1):1074 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Triple-negative breast cancer (TNBC) comprises a heterogeneous group of diseases which are generally associated with poor prognosis. Up to now, no targeted treatment beyond anti-VEGF therapy has been approved for TNBC and cytotoxic agents remain the mainstay of treatment. Ixazomib is a selective and reversible inhibitor of the proteasome, which has been mainly investigated in the treatment of multiple myeloma. In a preclinical study TNBC cells were treated with the first-generation proteasome inhibitor bortezomib in combination with cisplatin and synergistic efficacy was demonstrated. Clinical data are available for carboplatin plus bortezomib in metastatic ovarian and lung cancers showing remarkable antitumor activity and good tolerability (Mol Cancer 11:26 2012, J Thorac Oncol 4:87-92 2009, J Thorac Oncol 7:1032-1040, 2012). Based on this evidence, the phase I/II MBC-10 trial will evaluate the toxicity profile and efficacy of the second-generation proteasome inhibitor ixazomib in combination with carboplatin in patients with advanced TNBC.
METHODS: Patients with metastatic TNBC pretreated with at least one prior line of chemotherapy for advanced disease with a confirmed disease progression and measurable disease according to RECIST criteria 1.1 are eligible for this study. Patients will receive ixazomib in combination with carboplatin on days 1, 8, and 15 in a 28-day cycle. The phase I part of this study utilizes an alternate dose escalation accelerated titration design. After establishing the maximum tolerated dose (MTD), the efficacy and safety of the combination will be further evaluated (phase II, including 41 evaluable patients). All patients will continue on study drugs until disease progression, unacceptable toxicity or discontinuation for any other reason. Primary endpoint of the phase II is overall response rate, secondary endpoints include progression-free survival, safety, and quality of life. This trial is open for patient enrollment since November 2016 in six Austrian cancer centers. Accrual is planned to be completed within 2 years.
DISCUSSION: Based on preclinical and clinical findings an ixazomib and carboplatin combination is thought to be effective in metastatic TNBC patients. The MBC-10 trial is accompanied by a broad biomarker program investigating predictive biomarkers for treatment response and potential resistance mechanisms to the investigational drug combination.
TRIAL REGISTRATION: EudraCT Number: 2016-001421-13 received on March 31, 2016, ClinicalTrials.gov Identifier: NCT02993094 first posted on December 15, 2016. This trial was registered prospectively.
METHODS: Patients with metastatic TNBC pretreated with at least one prior line of chemotherapy for advanced disease with a confirmed disease progression and measurable disease according to RECIST criteria 1.1 are eligible for this study. Patients will receive ixazomib in combination with carboplatin on days 1, 8, and 15 in a 28-day cycle. The phase I part of this study utilizes an alternate dose escalation accelerated titration design. After establishing the maximum tolerated dose (MTD), the efficacy and safety of the combination will be further evaluated (phase II, including 41 evaluable patients). All patients will continue on study drugs until disease progression, unacceptable toxicity or discontinuation for any other reason. Primary endpoint of the phase II is overall response rate, secondary endpoints include progression-free survival, safety, and quality of life. This trial is open for patient enrollment since November 2016 in six Austrian cancer centers. Accrual is planned to be completed within 2 years.
DISCUSSION: Based on preclinical and clinical findings an ixazomib and carboplatin combination is thought to be effective in metastatic TNBC patients. The MBC-10 trial is accompanied by a broad biomarker program investigating predictive biomarkers for treatment response and potential resistance mechanisms to the investigational drug combination.
TRIAL REGISTRATION: EudraCT Number: 2016-001421-13 received on March 31, 2016, ClinicalTrials.gov Identifier: NCT02993094 first posted on December 15, 2016. This trial was registered prospectively.
Elliott DA, Rana SR, Nabavizadeh N, et al.
Underutilization of the CROSS Regimen Among US Radiation Oncologists: A National Survey of Practice Patterns.
Anticancer Res. 2018; 38(11):6375-6379 [PubMed] Related Publications
Underutilization of the CROSS Regimen Among US Radiation Oncologists: A National Survey of Practice Patterns.
Anticancer Res. 2018; 38(11):6375-6379 [PubMed] Related Publications
AIM: To examine patterns of clinical practice in locally advanced esophageal cancer among US radiation oncologists after publication of the CROSS trial.
MATERIALS AND METHODS: US radiation oncologists were surveyed on 13 questions pertaining to the management of esophageal cancer. Respondents' demographics and their clinical rationale were analyzed for statistical association with their treatment recommendations.
RESULTS: Few respondents (15%) offered the CROSS regimen to patients considered suitable surgical candidates, while a near-equivalent number (16%) prescribed between 41.4 and 50.4 Gy contingent upon radiation planning parameters. Among respondents who prescribed 50.4 Gy, 50% and 17% reported concurrent administration of carboplatin/paclitaxel and cisplatin/5-FU, respectively. Higher radiation doses, over 50.4 Gy, were utilized by 15% and 38% of respondents for borderline surgical candidates and candidates unfit for surgery, respectively. The majority of respondents believed that higher complete pathological response and R0 resection would be achieved, as well as higher toxicity conferred using 50.4 Gy instead of 41.4 Gy. A clinical trial comparing 41.4 Gy to 50.4 Gy with concurrent carboplatin/paclitaxel was supported by 76% of respondents.
CONCLUSION: Despite results from the CROSS trial, the majority of responding US radiation oncologists do not offer 41.4 Gy with concurrent chemotherapy for surgically-fit patients with locally advanced esophageal cancer, believing that a higher dose will translate to improved response.
MATERIALS AND METHODS: US radiation oncologists were surveyed on 13 questions pertaining to the management of esophageal cancer. Respondents' demographics and their clinical rationale were analyzed for statistical association with their treatment recommendations.
RESULTS: Few respondents (15%) offered the CROSS regimen to patients considered suitable surgical candidates, while a near-equivalent number (16%) prescribed between 41.4 and 50.4 Gy contingent upon radiation planning parameters. Among respondents who prescribed 50.4 Gy, 50% and 17% reported concurrent administration of carboplatin/paclitaxel and cisplatin/5-FU, respectively. Higher radiation doses, over 50.4 Gy, were utilized by 15% and 38% of respondents for borderline surgical candidates and candidates unfit for surgery, respectively. The majority of respondents believed that higher complete pathological response and R0 resection would be achieved, as well as higher toxicity conferred using 50.4 Gy instead of 41.4 Gy. A clinical trial comparing 41.4 Gy to 50.4 Gy with concurrent carboplatin/paclitaxel was supported by 76% of respondents.
CONCLUSION: Despite results from the CROSS trial, the majority of responding US radiation oncologists do not offer 41.4 Gy with concurrent chemotherapy for surgically-fit patients with locally advanced esophageal cancer, believing that a higher dose will translate to improved response.
Loizzi V, Del Vecchio V, Crupano FM, et al.
A phase II study: dose-dense carboplatin and paclitaxel as neoadjuvant chemotherapy in locally advanced cervical cancer.
J Chemother. 2018; 30(4):247-252 [PubMed] Related Publications
A phase II study: dose-dense carboplatin and paclitaxel as neoadjuvant chemotherapy in locally advanced cervical cancer.
J Chemother. 2018; 30(4):247-252 [PubMed] Related Publications
This study evaluates the efficacy and toxicity of dose-dense weekly paclitaxel and carboplatin as neoadjuvant chemotherapy in locally advanced cervical cancer (LACC). We collected 23 cases of LACC treated with weekly paclitaxel and carboplatin for nine cycles: 20 patients had complete or partial response to chemotherapy and were submitted to surgery, 3 with poor response received chemoradiation therapy. Pathologic examination showed complete response in four patients, myometrial invasion <50% in nine and >50% in seven patients, parametrial involvement in two, vaginal metastasis in one and lymphovascular space invasion, with positive margins, in another case. Despite seven patients had radiological evidence of lymph nodes involvement at diagnosis, only one had nodal metastases. Five patients showed grade 3-4 of hematologic toxicity.
Khosravi A, Salimi B, Esfahani-Monfared Z, et al.
A Phase IV Efficacy Study of Formeta Plus Carboplatin as First-Line Treatment of Advanced Non-Squamous, Non-Small Cell Lung Cancer in Iran: An Affordable Price with Clinical Benefit
Asian Pac J Cancer Prev. 2018; 19(10):2973-2978 [PubMed] Free Access to Full Article Related Publications
A Phase IV Efficacy Study of Formeta Plus Carboplatin as First-Line Treatment of Advanced Non-Squamous, Non-Small Cell Lung Cancer in Iran: An Affordable Price with Clinical Benefit
Asian Pac J Cancer Prev. 2018; 19(10):2973-2978 [PubMed] Free Access to Full Article Related Publications
Background: This study performed to assess the efficacy and safety of Formeta (generic form of Pemetrexed) plus
Carboplatin as first-line chemotherapy in advanced stage, non- squamous, non small cell lung cancer ( NSCLC) in Iran.
Methods: This was a post marketing single-arm phase IV efficacy study of Formeta (manufactured by Oncomed.,Czech
Republic ) and Carboplatin in chemo-naive advanced non-squamous NSCLC Iranian patients. Patients received up to six
cycles of Formeta (500 mg/m2) combined with Carboplatin (area under the curve: AUC 5) every 3 weeks. The primary
endpoint was the progression free survival (PFS) and secondary endpoints were safety and overall survival (OS).
Results: Fifty-two patients were enrolled between June 2014 to January 2016, and 44 patients were evaluable for both
safety and efficacy. Partial and complete responses were achieved in 19 (36.5 %) and 2 (3.8%) patients, respectively
as well as stable disease in 8 patients (15.3 %). Median of PFS and OS were 7.9 ± 1.1 months and 12.43±0.6 months,
respectively. Anemia was the most prevalent adverse events of this regimen. Grades 3 or 4 of adverse events were not
observed in any patients. Non-hematologic and other grades of hematologic toxicities were generally mild, and there
were no treatment-related deaths. Conclusion: The combination of Formeta and Carboplatin was effective in advanced
non-squamous NSCLC and can be a suitable candidate as first-line treatment in these patient’s population.
Zafeiriou Z, Bianchini D, Chandler R, et al.
Genomic Analysis of Three Metastatic Prostate Cancer Patients with Exceptional Responses to Carboplatin Indicating Different Types of DNA Repair Deficiency.
Eur Urol. 2019; 75(1):184-192 [PubMed] Free Access to Full Article Related Publications
Genomic Analysis of Three Metastatic Prostate Cancer Patients with Exceptional Responses to Carboplatin Indicating Different Types of DNA Repair Deficiency.
Eur Urol. 2019; 75(1):184-192 [PubMed] Free Access to Full Article Related Publications
Platinum-based regimens have not been proved to increase survival from advanced prostate cancer (PCa). Incontrovertible evidence that a proportion of prostate cancers have homologous recombination DNA (HRD) repair defects, and that such genomic aberrations are synthetically lethal with both poly(ADP)-ribose polymerase inhibition and platinum, has increased interest in the utilisation of these drugs against a subset of these diseases. Here in we report three patients with advanced castration-resistant PCa with HRD defects having exceptional responses to carboplatin.
Ishikawa M, Nakamura K, Shibata T, et al.
A randomized phase II/III trial of conventional paclitaxel and carboplatin with or without bevacizumab vs dose-dense paclitaxel and carboplatin with or without bevacizumab, in stage IVB, recurrent or persistent cervical carcinoma: Japan Clinical Oncology Group Study (JCOG1311).
Jpn J Clin Oncol. 2018; 48(12):1096-1100 [PubMed] Related Publications
A randomized phase II/III trial of conventional paclitaxel and carboplatin with or without bevacizumab vs dose-dense paclitaxel and carboplatin with or without bevacizumab, in stage IVB, recurrent or persistent cervical carcinoma: Japan Clinical Oncology Group Study (JCOG1311).
Jpn J Clin Oncol. 2018; 48(12):1096-1100 [PubMed] Related Publications
A randomized controlled trial has been initiated to compare chemotherapy containing dose-dense paclitaxel plus carboplatin with or without bevacizumab to a conventional regimen containing tri-weekly paclitaxel plus carboplatin with or without bevacizumab. Eligible patients are those with stage IVB, recurrent or persistent cervical carcinoma not amenable to curative treatment with local therapy. Patients are randomly assigned to either the conventional or dose-dense regimen. However, patients who are at increased risk of adverse events following bevacizumab administration will not receive this drug. The primary endpoint of phase II part is response rate. If the response rate of the dose-dense regimen is better than that of conventional regimen, this study will proceed to phase III, where the primary endpoint is overall survival. Secondary endpoints in phase III part are progression-free survival, response rates, adverse events, serious adverse events and the proportion of non-hospitalization periods compared with planned treatment periods.


 Testicular Cancer
Testicular Cancer