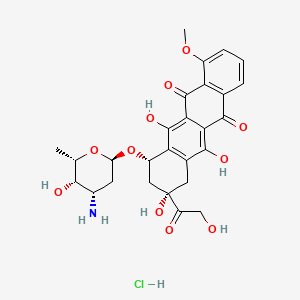
Doxorubicin
"Antineoplastic antibiotic obtained from Streptomyces peucetius. It is a hydroxy derivative of DAUNORUBICIN." (MeSH 2013)
Found this page useful?
 Web Resources: Doxorubicin
Web Resources: Doxorubicin Latest Research Publications
Latest Research Publications Liposomal Doxorubicin
Liposomal DoxorubicinWeb Resources: Doxorubicin (6 links)
Cancer Research UK
Irish Cancer Society
Macmillan Cancer Support
MedlinePlus
NHS Evidence
 Doxorubicin - Substance Summary
Doxorubicin - Substance Summary
PubChem
Latest Research Publications
Kim SH, Kang JG, Kim CS, et al.
Doxorubicin has a synergistic cytotoxicity with cucurbitacin B in anaplastic thyroid carcinoma cells.
Tumour Biol. 2017; 39(2):1010428317692252 [PubMed] Related Publications
Doxorubicin has a synergistic cytotoxicity with cucurbitacin B in anaplastic thyroid carcinoma cells.
Tumour Biol. 2017; 39(2):1010428317692252 [PubMed] Related Publications
In this study, the combined effect of doxorubicin with cucurbitacin B on survival of anaplastic thyroid carcinoma cells was evaluated. For experiments, 8505C and CAL62 human anaplastic thyroid carcinoma cells were used. Cell viability, the percentage of viable cells, and cytotoxic activity were measured using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay, multiplexed cytotoxicity assay, and cytotoxicity assay, respectively. Reactive oxygen species production was measured. In experiments, doxorubicin and cucurbitacin B reduced cell viability in a dose- and time-dependent manner. Cotreatment of doxorubicin and cucurbitacin B, compared with treatment of doxorubicin alone, decreased the percentage of viable cells and increased cytotoxic activity. All of the combination index values were lower than 1.0, suggesting the synergism between doxorubicin and cucurbitacin B in induction of cytotoxicity. In cells treated with both doxorubicin and cucurbitacin B, compared with doxorubicin alone, the protein levels of cleaved poly(adenosine diphosphate-ribose) polymerase and cyclooxygenase 2 and reactive oxygen species production were enhanced. In contrast, the protein levels of B-cell chronic lymphocytic leukemia/lymphoma 2 and survivin and B-cell chronic lymphocytic leukemia/lymphoma 2/B-cell chronic lymphocytic leukemia/lymphoma 2-associated x protein ratio were diminished. The protein levels of Janus kinase 2 and signal transducer and activator of transcription 3 were reduced, while phospho-extracellular signal-regulated kinase 1/2 protein levels were elevated without change in total extracellular signal-regulated kinase 1/2 protein levels. These results suggest that doxorubicin synergizes with cucurbitacin B in induction of cytotoxicity in anaplastic thyroid carcinoma cells. Moreover, synergistic cytotoxicity of doxorubicin with cucurbitacin B is mediated by B-cell chronic lymphocytic leukemia/lymphoma 2 family proteins, survivin, and reactive oxygen species and modulated by Janus kinase 2/signal transducer and activator of transcription 3 and extracellular signal-regulated kinase 1/2 in anaplastic thyroid carcinoma cells.
Luz JH, Luz PM, Martin HS, et al.
DEB TACE for Intermediate and advanced HCC - Initial Experience in a Brazilian Cancer Center.
Cancer Imaging. 2017; 17(1):5 [PubMed] Free Access to Full Article Related Publications
DEB TACE for Intermediate and advanced HCC - Initial Experience in a Brazilian Cancer Center.
Cancer Imaging. 2017; 17(1):5 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: According to Barcelona Clinic Liver Cancer classification transarterial chemoembolization is indicated in patients with Hepatocellular Carcinoma in the intermediate stage. Drug-eluting microspheres can absorb and release the chemotherapeutic agent slowly for 14 days after its intra-arterial administration. This type of transarterial chemoembolization approach appears to provide at least equivalent effectiveness with less toxicity.
METHODS: This is a prospective, single-center study, which evaluated 21 patients with intermediate and advanced hepatocellular carcinoma who underwent transarterial chemoembolization with drug-eluting microspheres. The follow up period was 2 years. Inclusion criteria was Child-Pugh A or B liver disease patients, intermediate or advanced hepatocellular carcinoma and performance status equal or below 2. Transarterial chemoembolization with drug-eluting microspheres was performed at 2-month intervals during the first two sessions. The third and subsequent sessions were performed according to the image findings on follow-up, on a "demand schedule". Tumor response and time to progression were evaluated along the two-year follow up period.
RESULTS: Of the 21 patients 90% presented with liver cirrhosis, 62% had Barcelona Clinic Liver Cancer stage B and 38% had Barcelona Clinic Liver Cancer stage C hepatocellular carcinoma. Average tumor size was 6.9 cm. The average number of Transarterial chemoembolization with drug-eluting microspheres procedures was 3 with a total of 64 sessions. The predominant toxicity was mild. Liver function was not significantly affected in most patients. Two deaths occurred within 90 days after Transarterial chemoembolization with drug-eluting microspheres (ischemic hepatitis and hydropic decompensation). Technical success was achieved in 63 of 64 procedures. The mean hospital stay was 1.5 days. The progression free and overall survival at 1 and 2 years were 73.0% and 37.1%, 73.7% and 41.6%, respectively.
CONCLUSION: Transarterial chemoembolization with drug-eluting microspheres is able to deliver significant tumor response and progression free survival rate with acceptable toxicity. Larger studies are needed to identify exactly which subset of advanced hepatocellular patients may benefit from this treatment.
TRIAL REGISTRATION: study ID ISRCTN16295622. Registered October 14th 2016. Retrospectively registered. Website registration: http://www.isrctn.com/ISRCTN16295622.
METHODS: This is a prospective, single-center study, which evaluated 21 patients with intermediate and advanced hepatocellular carcinoma who underwent transarterial chemoembolization with drug-eluting microspheres. The follow up period was 2 years. Inclusion criteria was Child-Pugh A or B liver disease patients, intermediate or advanced hepatocellular carcinoma and performance status equal or below 2. Transarterial chemoembolization with drug-eluting microspheres was performed at 2-month intervals during the first two sessions. The third and subsequent sessions were performed according to the image findings on follow-up, on a "demand schedule". Tumor response and time to progression were evaluated along the two-year follow up period.
RESULTS: Of the 21 patients 90% presented with liver cirrhosis, 62% had Barcelona Clinic Liver Cancer stage B and 38% had Barcelona Clinic Liver Cancer stage C hepatocellular carcinoma. Average tumor size was 6.9 cm. The average number of Transarterial chemoembolization with drug-eluting microspheres procedures was 3 with a total of 64 sessions. The predominant toxicity was mild. Liver function was not significantly affected in most patients. Two deaths occurred within 90 days after Transarterial chemoembolization with drug-eluting microspheres (ischemic hepatitis and hydropic decompensation). Technical success was achieved in 63 of 64 procedures. The mean hospital stay was 1.5 days. The progression free and overall survival at 1 and 2 years were 73.0% and 37.1%, 73.7% and 41.6%, respectively.
CONCLUSION: Transarterial chemoembolization with drug-eluting microspheres is able to deliver significant tumor response and progression free survival rate with acceptable toxicity. Larger studies are needed to identify exactly which subset of advanced hepatocellular patients may benefit from this treatment.
TRIAL REGISTRATION: study ID ISRCTN16295622. Registered October 14th 2016. Retrospectively registered. Website registration: http://www.isrctn.com/ISRCTN16295622.
Pradeepkumar P, Govindaraj D, Jeyaraj M, et al.
Assembling of multifunctional latex-based hybrid nanocarriers from Calotropis gigantea for sustained (doxorubicin) DOX releases.
Biomed Pharmacother. 2017; 87:461-470 [PubMed] Related Publications
Assembling of multifunctional latex-based hybrid nanocarriers from Calotropis gigantea for sustained (doxorubicin) DOX releases.
Biomed Pharmacother. 2017; 87:461-470 [PubMed] Related Publications
Natural rubber Latex (Lax) is a colloidal dispersion of polymer particles in liquid and shows good biodegradable, biocompatibility, and non-toxicity. Natural polymers are the most important materials used in food packaging, micro/nano-drug delivery, tissue engineering, agriculture, and coating. In the present study, natural compounds extracted from plant Lax were designed to function as drug carriers using various surfactants via emulation and solvent evaporation method. Calotropis gigantea belongs to the family Apocynaceae and has received considerable attention in modern medicine, ayurvedeic, siddha, and traditional medicine. Since, we were isolated biodegradable, non-toxic, and biocompatible materials as latex from Calotropis gigantea plant. The Lax was separated as per their solubility nature and it was designed as a carrier using surfactant namely; Sorbitanmonolaurate (Span-20), sodium lauryl sulfate (SLS), and cetyltrimethylammonium bromide (CTAB). The isolated compounds from Lax of Calotropis gigantea were analyzed using high-performance liquid chromatography. To confirm the encapsulation efficiency and in vitro drug release of the carriers, doxorubicin (DOX) was used as a model natural drug. The hybrid nanocarriers were successfully synthesized through simple solvent evaporation using three surfactants, and the morphology was characterized by SEM and TEM technique. The functionality and crystalline nature of the nanocarriers were confirmed using FTIR and XRD, respectively. Within 90min, the maximum amount of DOX was encapsulated in the carriers, and prolonged cumulative drug release by the nanocarriers was observed. The formulated natural carriers were found to have potentially effective cytotoxic effects on lung cancer cells.
Zhu B, Zhang H, Yu L
Novel transferrin modified and doxorubicin loaded Pluronic 85/lipid-polymeric nanoparticles for the treatment of leukemia: In vitro and in vivo therapeutic effect evaluation.
Biomed Pharmacother. 2017; 86:547-554 [PubMed] Related Publications
Novel transferrin modified and doxorubicin loaded Pluronic 85/lipid-polymeric nanoparticles for the treatment of leukemia: In vitro and in vivo therapeutic effect evaluation.
Biomed Pharmacother. 2017; 86:547-554 [PubMed] Related Publications
PURPOSE: Childhood leukemia is a common malignant disease in children. Doxorubicin (DOX) was widely used for the treatment of leukemia. However, severe toxic side effects and drug resistance are the major limitations of DOX. Nanocarriers offer the opportunity to overcome these drawbacks, there are many attempts to enhance the activity of DOX against drug resistance. This study aimed to develop a novel transferrin (Tf) modified and doxorubicin (DOX) loaded Pluronic 85/lipid-polymeric nanoparticles for the treatment of leukemia.
METHODS: In this study, a novel targeted ligand: transferrin-polyethylene glycol-oleic acid (Tf-PEG-OA) was synthesized. Tf modified and DOX loaded Pluronic 85/lipid-polymeric nanoparticles (Tf-DOX P85/LPNs) were prepared via the self-assembly of PLGA, P85, stearic acid and Tf-PEG-OA using the nanoprecipitation method. The physicochemical properties of LPNs were characterized. In vitro and in vivo anti-tumor efficacy of LPNs was evaluated in human promyelocytic leukemia cell line (HL-60 cells) and DOX resistance HL-60 cell line (HL-60/DOX cells) including the relevant animal models.
RESULTS: Tf-DOX P85/LPNs displayed strong anti-tumor ability on both HL-60 cells and HL-60/DOX cells than other formulations used as contrast. Also, in HL-60/DOX bearing animal models, Tf-DOX P85/LPNs exhibited the highest efficiency as well as the lowest systemic toxicity.
CONCLUSION: The results indicated that Tf P85/LPNs is a promising platform to enhance efficacy, reduce toxicity and overcome drug resistance of DOX for the treatment of leukemia.
METHODS: In this study, a novel targeted ligand: transferrin-polyethylene glycol-oleic acid (Tf-PEG-OA) was synthesized. Tf modified and DOX loaded Pluronic 85/lipid-polymeric nanoparticles (Tf-DOX P85/LPNs) were prepared via the self-assembly of PLGA, P85, stearic acid and Tf-PEG-OA using the nanoprecipitation method. The physicochemical properties of LPNs were characterized. In vitro and in vivo anti-tumor efficacy of LPNs was evaluated in human promyelocytic leukemia cell line (HL-60 cells) and DOX resistance HL-60 cell line (HL-60/DOX cells) including the relevant animal models.
RESULTS: Tf-DOX P85/LPNs displayed strong anti-tumor ability on both HL-60 cells and HL-60/DOX cells than other formulations used as contrast. Also, in HL-60/DOX bearing animal models, Tf-DOX P85/LPNs exhibited the highest efficiency as well as the lowest systemic toxicity.
CONCLUSION: The results indicated that Tf P85/LPNs is a promising platform to enhance efficacy, reduce toxicity and overcome drug resistance of DOX for the treatment of leukemia.
Qiao S, Zhao Y, Geng S, et al.
A novel double-targeted nondrug delivery system for targeting cancer stem cells.
Int J Nanomedicine. 2016; 11:6667-6678 [PubMed] Free Access to Full Article Related Publications
A novel double-targeted nondrug delivery system for targeting cancer stem cells.
Int J Nanomedicine. 2016; 11:6667-6678 [PubMed] Free Access to Full Article Related Publications
Instead of killing cancer stem cells (CSCs), the conventional chemotherapy used for cancer treatment promotes the enrichment of CSCs, which are responsible for tumor growth, metastasis, and recurrence. However, most therapeutic agents are only able to kill a small proportion of CSCs by targeting one or two cell surface markers or dysregulated CSC pathways, which are usually shared with normal stem cells (NSCs). In this study, we developed a novel nondrug delivery system for the dual targeting of CSCs by conjugating hyaluronic acid (HA) and grafting the doublecortin-like kinase 1 (DCLK1) monoclonal antibody to the surface of poly(ethylene glycol) (PEG)-poly(d,l-lactide-co-glycolide) (PLGA) nanoparticles (NPs), which can specifically target CD44 receptors and the DCLK1 surface marker - the latter was shown to possess the capacity to distinguish between CSCSs and NSCs. The size and morphology of these NPs were characterized by dynamic light scattering (DLS), transmission electron microscopy (TEM), and scanning electron microscopy (SEM). This was followed by studies of NP encapsulation efficiency and in vitro drug release properties. Then, the cytotoxicity of the NPs was tested via Cell Counting Kit-8 assay. Finally, the 4T1 CSCs were obtained from the alginate-based platform, which we developed as an in vitro tumor model. Tumor-bearing nude mice were used as in vivo models to systematically detect the ability of NPs to target CSCs. Our results showed that the DCLK1-HA-PEG-PLGA NPs exhibited a targeting effect toward CSCs both in vitro and in vivo. These findings have important implications for the rational design of drug delivery systems that target CSCs with high efficacy.
Wang Z, Tian Y, Zhang H, et al.
Using hyaluronic acid-functionalized pH stimuli-responsive mesoporous silica nanoparticles for targeted delivery to CD44-overexpressing cancer cells.
Int J Nanomedicine. 2016; 11:6485-6497 [PubMed] Free Access to Full Article Related Publications
Using hyaluronic acid-functionalized pH stimuli-responsive mesoporous silica nanoparticles for targeted delivery to CD44-overexpressing cancer cells.
Int J Nanomedicine. 2016; 11:6485-6497 [PubMed] Free Access to Full Article Related Publications
In this study, novel hyaluronic acid-pH stimuli-responsive lipid membrane mesoporous silica nanoparticles (HA-PL-MSNs) were designed and assembled, with the chemotherapeutic agent doxorubicin (DOX) as the model drug. HA-PL-MSNs exhibited a well-defined mesostructure covered by lipid bilayer and particle size of ~150 nm. The drug loading capacity was up to ~18.2%. DOX release could be effectively retained by the lipid bilayer in pH 7.4 buffer and exhibited a pH-triggered burst release in the acidic condition. Confocal laser scanning microscopy and fluorescence-activated cell sorting showed that HA-PL-MSNs exhibited higher cellular uptake efficiency via CD44 receptor-mediated endocytosis compared with PL-MSNs in HeLa cells. In vitro cytotoxicity studies demonstrated that HA-PL-MSNs could effectively enhance the targeted delivery of DOX and restrain the growth of HeLa cells. This might provide a promising alternative for the development of a targeted anticancer drug delivery system.
Fang Z, Sun Y, Xiao H, et al.
Targeted osteosarcoma chemotherapy using RGD peptide-installed doxorubicin-loaded biodegradable polymeric micelle.
Biomed Pharmacother. 2017; 85:160-168 [PubMed] Related Publications
Targeted osteosarcoma chemotherapy using RGD peptide-installed doxorubicin-loaded biodegradable polymeric micelle.
Biomed Pharmacother. 2017; 85:160-168 [PubMed] Related Publications
Osteosarcoma is the most common primary malignant bone tumor in the pediatric age group, and chemotherapy directed by targeted nanoparticulate drug delivery system represents a promising approach for osteosarcoma treatment recently. Here, we designed and developed a novel DOX-loaded targeted polymeric micelle self-assembled from RGD-terminated poly(ethylene glycol)-block-poly (trimethylene carbonate) (RGD-PEG-PTMC) amphiphilic biodegradable block copolymer, for high-efficiency targeted chemotherapy of osteosarcoma. Notably, the RGD-installed DOX-loaded biodegradable polymeric micelle (RGD-DOX-PM) with drug loading efficiency of 57%-73% displayed a narrow distribution (PDI=0.05-0.12) with average sizes ranging from 46 to 73nm depending on the DOX loading content. The release amount of DOX from RGD-DOX-PM achieved 63% within 60h under physiological condition. Interestingly, MTT assays in MG-63 and MNNG/HOS osteosarcoma cells exhibited that half-maximal inhibitory concentration (IC50) value of RGD-DOX-PM was much lower than its non-targeted counterpart (DOX-PM), implying RGD decorated nanoparticles had enhanced cell targeting ability and led to more effective anti-tumor effect. Furthermore, the targeting ability of RGD-DOX-PM was confirmed by in vitro flow cytometry and confocal laser scanning microscopy (CLSM) imaging assays, where the results showed more RGD-DOX-PM were taken up by MG-63 cells than that of DOX-PM. Therefore, this RGD decorated DOX-loaded polymeric micelle is promising for targeted chemotherapy of osteosarcoma.
Kusaba H, Kumagai H, Inadomi K, et al.
Efficacy analysis of the aprepitant-combined antiemetic prophylaxis for non-round cell soft-tissue sarcoma patients received adriamycin and ifosfamide therapy.
Medicine (Baltimore). 2016; 95(49):e5460 [PubMed] Free Access to Full Article Related Publications
Efficacy analysis of the aprepitant-combined antiemetic prophylaxis for non-round cell soft-tissue sarcoma patients received adriamycin and ifosfamide therapy.
Medicine (Baltimore). 2016; 95(49):e5460 [PubMed] Free Access to Full Article Related Publications
Appropriate antiemetic prophylaxis for moderately emetogenic chemotherapy in patients with non-round cell soft-tissue sarcomas (NRC-STS) remains unclear. We retrospectively investigated efficacy and safety of aprepitant-combined antiemetic prophylaxis in patients with NRC-STS receiving adriamycin plus ifosfamide (AI) therapy. Forty NRC-STS patients were enrolled, their median age was 50 years (range 18-74), and 13 (32.5%) were female. Median cycle number of AI therapy was 4. Twenty patients received the doublet antiemetic prophylaxis (5-hydroxytryptamine-3 receptor antagonist and dexamethasone), and 20 received triplet (5-hydroxytryptamine-3 receptor antagonist, dexamethasone, and aprepitant). In the overall period, complete response rate for nausea and emesis in the triplet group was significantly higher than that in the doublet group (70% vs 35%; P = 0.027). Patients with no-emesis in the overall period were more frequently observed in the triplet group than in the doublet group (90% vs 65%; P = 0.058). All toxicities other than emesis were almost equivalent in both the groups. These results suggest that a triplet antiemetic prophylaxis may be optimal in the treatment with AI therapy for NRC-STS.
Oh Y, Moorthy MS, Manivasagan P, et al.
Magnetic hyperthermia and pH-responsive effective drug delivery to the sub-cellular level of human breast cancer cells by modified CoFe2O4 nanoparticles.
Biochimie. 2017; 133:7-19 [PubMed] Related Publications
Magnetic hyperthermia and pH-responsive effective drug delivery to the sub-cellular level of human breast cancer cells by modified CoFe2O4 nanoparticles.
Biochimie. 2017; 133:7-19 [PubMed] Related Publications
Magnetic iron oxide nanoparticles (MNPs) have been extensively utilized in a wide range of biomedical applications including magnetic hyperthermia agent. To improve the efficiency of the MNPs in therapeutic applications, in this study, we have synthesized CoFe2O4 nanoparticles and its surface was further functionalized with meso-2,3-dimercaptosuccinic acid (DMSA). The anticancer agent, Doxorubucin (DOX) was conjugated with CoFe2O4@DMSA nanoparticle to evaluate the combined effects of thermotherapy and chemotherapy. The drug delivery efficiency of the DOX loaded CoFe2O4@DMSA nanoparticles were examined based on magnetically triggered delivery of DOX into the subcellular level of cancer cells by using MDA-MB-231 cell line. The amine part of the DOX molecules were effectively attached through an electrostatic interactions and/or hydrogen bonding interactions with the carboxylic acid groups of the DMSA functionalities present onto the surface of the CoFe2O4 nanoparticles. The DOX loaded CoFe2O4@DMSA nanoparticles can effectively uptake with cancer cells via typical endocytosis process. After endocytosis, DOX release from CoFe2O4 nanoparticles was triggered by intracellular endosomal/lysosomal acidic environments and the localized heat can be generated under an alternating magnetic field (AMF). In the presence of AMF, the released DOX molecules were accumulated with high concentrations into the subcellular level at a desired sites and exhibited a synergistic effect of an enhanced cell cytotoxicity by the combined effects of thermal-chemotherapy. Importantly, pH- and thermal-responsive Dox-loaded CoFe2O4 nanoparticles induced significant cellular apoptosis more efficiently mediated by active mitochondrial membrane and ROS generation than the free Dox. Thus, the Dox-loaded CoFe2O4@DMSA nanoparticles can be used as a potential therapeutic agent in cancer therapy by combining the thermo-chemotherapy techniques.
Zhao X, Yang Y, Yao F, et al.
Unfolded Protein Response Promotes Doxorubicin-Induced Nonsmall Cell Lung Cancer Cells Apoptosis via the mTOR Pathway Inhibition.
Cancer Biother Radiopharm. 2016; 31(10):347-351 [PubMed] Related Publications
Unfolded Protein Response Promotes Doxorubicin-Induced Nonsmall Cell Lung Cancer Cells Apoptosis via the mTOR Pathway Inhibition.
Cancer Biother Radiopharm. 2016; 31(10):347-351 [PubMed] Related Publications
Drug resistance is extremely common in nonsmall cell lung cancer (NSCLC) and is one of the major problems in NSCLC chemotherapy. However, the detailed mechanisms remain largely unknown. Unfolded protein response (UPR) is involved in the tumorigenesis of NSCLC. Here, the authors demonstrated that the UPR promotes poly (ADP-ribose) polymerase activation (PARP) cleavage in NSCLC cells on doxorubicin treatment, which is a hallmark of apoptosis and caspase activation. In NSCLC cells, doxorubicin treatment triggers the UPR activation, which subsequently promotes doxorubicin-mediated apoptosis. Importantly, mild endoplasmic reticulum stress precondition enhances the sensitivity of NSCLC cells to doxorubicin-initiated apoptosis. Furthermore, the eukaryotic translation initiation factor 2α (eIF2α) branch of the UPR is involved in the synergistic role of the UPR in NSCLC cell apoptosis on doxorubicin treatment. They also demonstrated that the mTOR pathway plays an essential role in synergistic induction of apoptosis by the UPR and doxorubicin in NSCLC cells. Taken together, these results provide a potential mechanism that the UPR promotes doxorubicin-induced apoptosis in NSCLC cells, at least in part, by eIF2α-mediated mTOR signal inactivation.
Juang V, Lee HP, Lin AM, Lo YL
Cationic PEGylated liposomes incorporating an antimicrobial peptide tilapia hepcidin 2-3: an adjuvant of epirubicin to overcome multidrug resistance in cervical cancer cells.
Int J Nanomedicine. 2016; 11:6047-6064 [PubMed] Free Access to Full Article Related Publications
Cationic PEGylated liposomes incorporating an antimicrobial peptide tilapia hepcidin 2-3: an adjuvant of epirubicin to overcome multidrug resistance in cervical cancer cells.
Int J Nanomedicine. 2016; 11:6047-6064 [PubMed] Free Access to Full Article Related Publications
Antimicrobial peptides (AMPs) have been recently evaluated as a new generation of adjuvants in cancer chemotherapy. In this study, we designed PEGylated liposomes encapsulating epirubicin as an antineoplastic agent and tilapia hepcidin 2-3, an AMP, as a multidrug resistance (MDR) transporter suppressor and an apoptosis/autophagy modulator in human cervical cancer HeLa cells. Cotreatment of HeLa cells with PEGylated liposomal formulation of epirubicin and hepcidin 2-3 significantly increased the cytotoxicity of epirubicin. The liposomal formulations of epirubicin and/or hepcidin 2-3 were found to noticeably escalate the intracellular H2O2 and O2(-) levels of cancer cells. Furthermore, these treatments considerably reduced the mRNA expressions of MDR protein 1, MDR-associated protein (MRP) 1, and MRP2. The addition of hepcidin 2-3 in liposomes was shown to markedly enhance the intracellular epirubicin uptake and mainly localized into the nucleus. Moreover, this formulation was also found to trigger apoptosis and autophagy in HeLa cells, as validated by significant increases in the expressions of cleaved poly ADP ribose polymerase, caspase-3, caspase-9, and light chain 3 (LC3)-II, as well as a decrease in mitochondrial membrane potential. The apoptosis induction was also confirmed by the rise in sub-G1 phase of cell cycle assay and apoptosis percentage of annexin V/propidium iodide assay. We found that liposomal epirubicin and hepcidin 2-3 augmented the accumulation of GFP-LC3 puncta as amplified by chloroquine, implying the involvement of autophagy. Interestingly, the partial inhibition of necroptosis and the epithelial-mesenchymal transition by this combination was also verified. Altogether, our results provide evidence that coincubation with PEGylated liposomes of hepcidin 2-3 and epirubicin caused programmed cell death in cervical cancer cells through modulation of multiple signaling pathways, including MDR transporters, apoptosis, autophagy, and/or necroptosis. Thus, this formulation may provide a new platform for the combined treatment of traditional chemotherapy and hepcidin 2-3 as a new adjuvant for effective MDR reversal.
Sun F, Shi J, Geng C
Dexrazoxane improves cardiac autonomic function in epirubicin-treated breast cancer patients with type 2 diabetes.
Medicine (Baltimore). 2016; 95(44):e5228 [PubMed] Related Publications
Dexrazoxane improves cardiac autonomic function in epirubicin-treated breast cancer patients with type 2 diabetes.
Medicine (Baltimore). 2016; 95(44):e5228 [PubMed] Related Publications
OBJECTIVE: The study objective was to investigate the protective effects of dexrazoxane (DRZ) on the cardiac autonomic nervous system (ANS) activity in anthracycline-treated breast cancer patients with diabetes.
METHODS: A total of 110 early stage breast cancer patients with type 2 diabetes were divided randomly into 2 even groups: chemotherapy alone (Chemo) and chemotherapy + DRZ (Chemo + DRZ). All patients underwent adjuvant chemotherapy (80 mg/m epirubicin and 500 mg/m cyclophosphamide) for a total of 6 cycles with 21 days/cycle. The Chemo + DRZ group patients were treated intravenously with 800 mg/m DRZ 30 minutes prior to the administration of epirubicin, while the Chemo group patients were given saline. The cardiac ANS function was evaluated for each patient before and after 6 cycles of chemotherapy by resting heart rate (RHR) and heart rate variability (HRV), which was evaluated by both time and frequency domains.
RESULTS: Before and after chemotherapy, patients in both groups showed significant decreases in HRV indices and increases in RHR and the low-frequency/high-frequency ratio. There were no significant differences between Chemo and Chemo + DRZ groups in terms of RHR and HRV indices before chemotherapy; however, after chemotherapy, patients in the Chemo group had a higher average RHR and lower HRV indices compared with patients in the Chemo + DRZ group.
CONCLUSION: DRZ protects the cardiac ANS in epirubicin-treated early stage breast cancer patients with diabetes.
METHODS: A total of 110 early stage breast cancer patients with type 2 diabetes were divided randomly into 2 even groups: chemotherapy alone (Chemo) and chemotherapy + DRZ (Chemo + DRZ). All patients underwent adjuvant chemotherapy (80 mg/m epirubicin and 500 mg/m cyclophosphamide) for a total of 6 cycles with 21 days/cycle. The Chemo + DRZ group patients were treated intravenously with 800 mg/m DRZ 30 minutes prior to the administration of epirubicin, while the Chemo group patients were given saline. The cardiac ANS function was evaluated for each patient before and after 6 cycles of chemotherapy by resting heart rate (RHR) and heart rate variability (HRV), which was evaluated by both time and frequency domains.
RESULTS: Before and after chemotherapy, patients in both groups showed significant decreases in HRV indices and increases in RHR and the low-frequency/high-frequency ratio. There were no significant differences between Chemo and Chemo + DRZ groups in terms of RHR and HRV indices before chemotherapy; however, after chemotherapy, patients in the Chemo group had a higher average RHR and lower HRV indices compared with patients in the Chemo + DRZ group.
CONCLUSION: DRZ protects the cardiac ANS in epirubicin-treated early stage breast cancer patients with diabetes.
Sandoval TA, Urueña CP, Llano M, et al.
Standardized Extract from Caesalpinia spinosa is Cytotoxic Over Cancer Stem Cells and Enhance Anticancer Activity of Doxorubicin.
Am J Chin Med. 2016; 44(8):1693-1717 [PubMed] Related Publications
Standardized Extract from Caesalpinia spinosa is Cytotoxic Over Cancer Stem Cells and Enhance Anticancer Activity of Doxorubicin.
Am J Chin Med. 2016; 44(8):1693-1717 [PubMed] Related Publications
Cancer stem cells (CSC) are the primary cell type responsible for metastasis and relapse. ABC-transporters are integral membrane proteins involved in the translocation of substrates across membranes protecting CSC from chemotherapeutic agents. A plant extract derived from C. spinosa (P2Et) previously investigated for its antitumor activity has been shown to reduce lung and spleen metastasis in mice that have been transplanted with breast cancer cells, suggesting that P2Et has a significant activity against cancer stem cells (CSC). P2Et extract was thoroughly characterized by HPLC/MS. The cytotoxicity of P2Et extract was evaluated using a MTT assay in human and murine cell lines with different profiles of resistance, by Pgp overexpression or by enrichment in cancer stem cells. The synergistic effect of P2Et with doxorubicin was evaluated in vitro in several cell lines and in vivo in mice transplanted with TS/A cells, a highly resistant cell line and enriched in CD44[Formula: see text]CD24[Formula: see text]CSC. The chromatographic fingerprint of P2Et extract revealed 13 gallotannins. We also found that P2Et extract was cytotoxic to cells regardless of their resistant phenotype. Similarly, complementary activities were observed as drug efflux reversion and antioxidant activity. Short-treatment with P2Et extract, revealed a synergistic effect with doxorubicin in resistant cell lines. In vivo the P2Et increases mice survival in a TS/A breast cancer model associated with augmentation of calreticulin expression. Our results suggest that P2Et treatment could be used as adjuvant along with conventional chemotherapy to treat tumors with a MDR phenotype or with high frequency of CSC.
Kumar A, Lale SV, Aji Alex MR, et al.
Folic acid and trastuzumab conjugated redox responsive random multiblock copolymeric nanocarriers for breast cancer therapy: In-vitro and in-vivo studies.
Colloids Surf B Biointerfaces. 2017; 149:369-378 [PubMed] Related Publications
Folic acid and trastuzumab conjugated redox responsive random multiblock copolymeric nanocarriers for breast cancer therapy: In-vitro and in-vivo studies.
Colloids Surf B Biointerfaces. 2017; 149:369-378 [PubMed] Related Publications
The study represents synthesis, characterization and biological evaluation of redox responsive polymeric nanoparticles based on random multiblock copolymer for doxorubicin delivery in breast cancer. The random multiblock copolymer was synthesized via ring opening polymerization of lactide with polyethylene glycol to form triblock copolymer followed by isomerization polymerization of the triblock copolymer and 2-hydroxyethyl disulfide with the help of hexamethylene diisocynate in presence of dibutyltin dilaurate as a catalyst. Folic acid was conjugated to hydroxyl group from the multiblock polymer through DCC-NHS coupling. High drug loading content of ∼22% was achieved in the polymeric nanoparticles with size range of ∼110nm and polyethylene glycol fraction of ∼18% in the multiblock copolymer. Drug release profile confirmed the redox responsive behavior of polymeric nanoparticles with ∼72% drug release at pH 5.5 in presence of 10mM GSH as compared to ∼18% drug release at pH 7.4. In vitro cellular uptake studies showed ∼22% cellular uptake with dual (folic acid and trastuzumab) conjugated polymeric nanoparticles as compared to non-targeted polymeric nanoparticles. Fluorescence activated cell sorting (FACS) studies demonstrated higher apoptosis (∼80%) as compared to non-conjugated polymeric nanoparticles (20%) in MCF-7 cell line. In vivo studies showed 91% tumor regression in Ehrlich ascites tumor (EAT) as compared to free doxorubicin treated mice without showing any significant toxicity. Thus, it is envisaged that these redox responsive polymeric nanocarriers act as Trojan horses in cancer therapeutics.
Gu Y, Li J, Li Y, et al.
Nanomicelles loaded with doxorubicin and curcumin for alleviating multidrug resistance in lung cancer.
Int J Nanomedicine. 2016; 11:5757-5770 [PubMed] Free Access to Full Article Related Publications
Nanomicelles loaded with doxorubicin and curcumin for alleviating multidrug resistance in lung cancer.
Int J Nanomedicine. 2016; 11:5757-5770 [PubMed] Free Access to Full Article Related Publications
PURPOSE: A new type of polymeric micelle (PM) was assembled using a polyethylene glycol (PEG)-linked (PEGylated) amphiphilic copolymer and d-tocopheryl PEG1000 succinate (TPGS1000). The micelles were used to deliver doxorubicin (DOX) and curcumin (CUR) for alleviating multidrug resistance (MDR) in lung cancer cells while enhancing the therapeutic efficacy of DOX.
METHODS: Micelles loaded with DOX and CUR were assembled using a film-forming technique. Micelles were used to treat A549/Adr cells to find out whether micelles had the ability to reverse the MDR of A549/Adr cells. Some investigations were conducted using tumor-bearing mice to assess whether these micelles had enhanced antitumor efficacy as compared to DOX alone or the combination of DOX and CUR.
RESULTS: Some micelles (DOX + CUR)-PMs had a small average size of about 17 nm and showed definite ability to deliver both DOX and CUR into DOX-resistant A549/Adr cells. The PMs had high cytotoxicity toward A549/Adr cells when the applied equivalent DOX dose was 1 µg/mL or higher. The cellular uptake of (DOX + CUR)-PMs into A549/Adr cells was found to be associated with an energy-dependent, caveolae-mediated, and clathrin-independent mechanism. (DOX + CUR)-PMs helped to prolong the circulation of DOX or CUR as compared to the individual administration of DOX or CUR, and they exhibited high inhibiting efficiency against the growth of tumors and were able to reduce the side effects of DOX.
CONCLUSION: TPGS1000 and CUR could synergistically reverse DOX-resistance of A549/Adr cells. In vivo examinations confirmed that the micelles had the capability to increase the plasma concentration of DOX or CUR, as well as to prolong their respective blood circulation. These micelles were able to significantly inhibit tumor growth in Lewis lung carcinoma tumor-bearing mice while reducing the side effects of DOX. The micelles showed potential in the treatment of lung cancer.
METHODS: Micelles loaded with DOX and CUR were assembled using a film-forming technique. Micelles were used to treat A549/Adr cells to find out whether micelles had the ability to reverse the MDR of A549/Adr cells. Some investigations were conducted using tumor-bearing mice to assess whether these micelles had enhanced antitumor efficacy as compared to DOX alone or the combination of DOX and CUR.
RESULTS: Some micelles (DOX + CUR)-PMs had a small average size of about 17 nm and showed definite ability to deliver both DOX and CUR into DOX-resistant A549/Adr cells. The PMs had high cytotoxicity toward A549/Adr cells when the applied equivalent DOX dose was 1 µg/mL or higher. The cellular uptake of (DOX + CUR)-PMs into A549/Adr cells was found to be associated with an energy-dependent, caveolae-mediated, and clathrin-independent mechanism. (DOX + CUR)-PMs helped to prolong the circulation of DOX or CUR as compared to the individual administration of DOX or CUR, and they exhibited high inhibiting efficiency against the growth of tumors and were able to reduce the side effects of DOX.
CONCLUSION: TPGS1000 and CUR could synergistically reverse DOX-resistance of A549/Adr cells. In vivo examinations confirmed that the micelles had the capability to increase the plasma concentration of DOX or CUR, as well as to prolong their respective blood circulation. These micelles were able to significantly inhibit tumor growth in Lewis lung carcinoma tumor-bearing mice while reducing the side effects of DOX. The micelles showed potential in the treatment of lung cancer.
Jiang S, Wang X, Zhang Z, et al.
CD20 monoclonal antibody targeted nanoscale drug delivery system for doxorubicin chemotherapy: an in vitro study of cell lysis of CD20-positive Raji cells.
Int J Nanomedicine. 2016; 11:5505-5518 [PubMed] Free Access to Full Article Related Publications
CD20 monoclonal antibody targeted nanoscale drug delivery system for doxorubicin chemotherapy: an in vitro study of cell lysis of CD20-positive Raji cells.
Int J Nanomedicine. 2016; 11:5505-5518 [PubMed] Free Access to Full Article Related Publications
A monoclonal antibody targeted nanoscale drug delivery system (NDDS) for chemotherapy was evaluated in CD20-positive Raji cells in vitro. Nanoparticles were formed by the assembly of an amphiphilic polymer consisting of 1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-methoxypolyethyleneglycol-2000 (DSPE-PEG2000). Active carbon nanoparticles (ACNP) were conjugated to the chemotherapeutic agent, doxorubicin (DOX), and the nanoliposome carrier, DSPE-PEG2000 and DSPE-PEG2000-NH2 conjugated to the human anti-CD20 monoclonal antibody that targets B-lymphocytes. This monoclonal antibody targeted nanoparticle delivery system for chemotherapy formed the active NDDS complex, ACNP-DOX-DSPE-PEG2000-anti-CD20. This active NDDS was spherical in morphology and had good dispersion in the culture medium. When compared with the effects on CD20-negative YTS cells derived from natural killer/T-cell lymphoma, the active NDDS, ACNP-DOX-DSPE-PEG2000-anti-CD20, demonstrated DOX delivery to CD20-positive Raji cells derived from Burkitt's lymphoma (B cell lymphoma), resulting in increased cell killing in vitro. The intracellular targeting efficiency of the ACNP-DOX-DSPE-PEG2000-anti-CD20 complex was assessed by confocal laser microscopy and flow cytometry. The findings of this in vitro study have shown that the DSPE-PEG2000 polymeric liposome is an effective nanocarrier of both a monoclonal antibody and a chemotherapy agent and can be used to target chemotherapy to specific cells, in this case to CD20-positive B-cells. Future developments in this form of targeted therapy will depend on the development of monoclonal antibodies that are specific for malignant cells, including antibodies that can distinguish between lymphoma cells and normal lymphocyte subsets.
Cho SH, Hong JH, Noh YW, et al.
Raspberry-like poly(γ-glutamic acid) hydrogel particles for pH-dependent cell membrane passage and controlled cytosolic delivery of antitumor drugs.
Int J Nanomedicine. 2016; 11:5621-5632 [PubMed] Free Access to Full Article Related Publications
Raspberry-like poly(γ-glutamic acid) hydrogel particles for pH-dependent cell membrane passage and controlled cytosolic delivery of antitumor drugs.
Int J Nanomedicine. 2016; 11:5621-5632 [PubMed] Free Access to Full Article Related Publications
In this research, we synthesized bioderived poly(amino acid) hydrogel particles that showed pH-dependent membrane-disrupting properties and controlled cytosolic delivery of antitumor drugs. Poly(γ-glutamic acid) (γ-PGA) that has been produced extensively using bacteria, especially those of Bacillus subtilis species, was modified with cholesterol (γ-PGA/Chol), and the γ-PGA/Chol conjugates were used to form polymeric nanoparticles the size of 21.0±1.1 nm in aqueous solution. When the polymeric nanoparticles were mixed with doxorubicin (Dox), raspberry-like hydrogel particles (RBHPs) were formed by the electrostatic interaction between the cationically charged Dox and the anionically charged nanoparticles. The average size and surface charge of the RBHPs in aqueous solution were 444.9±122.5 nm and -56.44 mV, respectively. The loaded amount of Dox was approximately 63.9 μg/mg of RBHPs. The RBHPs showed controlled drug release behavior in both in vitro and ex vivo cell-based experiments. Through fluorescence microscopy and fluorescence-activated cell sorting, the cellular uptake of RBHPs into human cervical cancer cells (HeLa) was analyzed. The cytotoxic effect, evaluated by the methyl tetrazolium salt assay, was dependent on both the concentration of RBHPs and the treatment time. The pH-dependent membrane-disrupting properties of the RBHPs and the subsequent cytosolic delivery of Dox were evaluated using a standard hemolysis assay. Upon an increase in hydrophobicity at the lysosomal acidic pH, RBHPs could easily interact, penetrate cell membranes, and destabilize them. Taken together, the data suggested that RBHPs could be used as drug delivery carriers after loading with other therapeutic drugs, such as proteins or small interfering RNA for cancer therapy.
Cheng L, Ke Y, Yu S, Jing J
Co-delivery of doxorubicin and recombinant plasmid pHSP70-Plk1-shRNA by bacterial magnetosomes for osteosarcoma therapy.
Int J Nanomedicine. 2016; 11:5277-5286 [PubMed] Free Access to Full Article Related Publications
Co-delivery of doxorubicin and recombinant plasmid pHSP70-Plk1-shRNA by bacterial magnetosomes for osteosarcoma therapy.
Int J Nanomedicine. 2016; 11:5277-5286 [PubMed] Free Access to Full Article Related Publications
To explore a novel combination of chemotherapy, gene therapy, and thermotherapy for osteosarcoma, a targeted heat-sensitive co-delivery system based on bacterial magnetosomes (BMs) was developed. The optimal culture conditions of magnetotactic bacteria (MTB) AMB-1 and characterization of BMs were achieved. A recombinant eukaryotic plasmid heat shock protein 70-polo-like kinase 1-short hairpin RNA (pHSP70-Plk1-shRNA) under transcriptional control of a thermosensitive promoter (human HSP70 promoter) was constructed for gene therapy. Doxorubicin (DOX) and pHSP70-Plk1-shRNA were included in the targeted thermosensitive co-delivery system, and in vitro DOX release activity, targeted gene silencing efficiency and in vitro antitumor efficacy were investigated. The results showed that the optimal culture conditions of MTB AMB-1 are an oxygen concentration of 4.0%, a pH value of 7.0, 20 μmol/L of ferrous sulfate, 800 mg/L of sodium nitrate, and 200 mg/L of succinic acid. The temperature of BMs reached 43°C within 3 minutes and could be maintained for 30 minutes by adjusting the magnitude of the alternating magnetic field (AMF). The diameters of BMs, BM-DOX, BM-recombinant eukaryotic plasmid pHSP70-Plk1-shRNA (shPlk1), and BM-DOX-shPlk1 were 43.7±4.6, 79.2±5.4, 88.9±7.8, and 133.5±11.4 nm, respectively. The zeta potentials of BMs, BM-DOX, BM-shPlk1, and BM-DOX-shPlk1 were -29.4±6.9, -9.5±5.6, -16.7±4.8, and -10.3±3.1 mV, respectively. Besides, the system exhibited good release behavior. DOX release rate from BM-DOX-shPlk1 was 54% after incubation with phosphate-buffered saline at 43°C and 37% after incubation with 50% fetal bovine serum, which was significantly higher than that at 37°C (P<0.05). In addition, the expressions of Plk1 mRNA and protein were significantly suppressed in cells treated with BM-DOX-shPlk1 following hyperthermia treatment under the influence of an AMF compared to other groups (P<0.05). Furthermore, evaluation of the effect of in vitro antitumor revealed that BM-DOX-shPlk1 following hyperthermia treatment under the influence of an AMF was significantly more effective than others in tumor inhibition. In conclusion, the new heat-sensitive co-delivery system represents a promising approach for the treatment of cancer.
Shah SA, Aslam Khan MU, Arshad M, et al.
Doxorubicin-loaded photosensitive magnetic liposomes for multi-modal cancer therapy.
Colloids Surf B Biointerfaces. 2016; 148:157-164 [PubMed] Related Publications
Doxorubicin-loaded photosensitive magnetic liposomes for multi-modal cancer therapy.
Colloids Surf B Biointerfaces. 2016; 148:157-164 [PubMed] Related Publications
Multifunctional magnetic nanosystems have attracted an enormous attention of researchers for their potential applications in cancer diagnostics and therapy. The localized nanotherapies triggered by the external stimuli, like magnetic fields and visible light, are significant in clinical applications. We report a liposomal system that aims to treat cancer by magnetic hyperthermia, photodynamic therapy and chemotherapy simultaneously. The liposomes enclose clinically used photosensitizer m-THPC (Foscan) and anti-cancer drug doxorubicin, in its hydrophobic lipid bilayers, and contains magnetite nanoparticles in hydrophilic core. Three different sizes of magnetic nanoparticles (10, 22 and 30nm) and liposomes (40, 70 and 110nm) were used in this study. Magnetite single domain nanoparticles forming the magnetic core were superparamagnetic but liposomes expressed slight coercivity and hysteresis due to the clustering of nanoparticles in the core. This enhanced the heating efficiency (specific power loss) of the liposomes under an AC field (375kHz, 170Oe). Cell viability and toxicity were studied on HeLa cells using MTT assay and proteomic analysis. Confocal and fluorescence microscopy were used to study the photosensitizer's profile and cells response to combined therapy. It revealed that combined therapy almost completely eliminated the cancer cells as opposed to the separate treatments. Magnetic hyperthermia and photodynamic therapies were almost equally effective whereas chemotherapy showed the least effect.
Denel-Bobrowska M, Lukawska M, Oszczapowicz I, Marczak A
Histological Subtype of Ovarian Cancer as a Determinant of Sensitivity to Formamidine Derivatives of Doxorubicin - in Vitro Comparative Studies with SKOV-3 and ES-2 Cancer Cell Lines.
Asian Pac J Cancer Prev. 2016; 17(9):4223-4231 [PubMed] Related Publications
Histological Subtype of Ovarian Cancer as a Determinant of Sensitivity to Formamidine Derivatives of Doxorubicin - in Vitro Comparative Studies with SKOV-3 and ES-2 Cancer Cell Lines.
Asian Pac J Cancer Prev. 2016; 17(9):4223-4231 [PubMed] Related Publications
BACKGROUND: Development of new apoptosis-inducing drugs is a promising trend in anticancer therapy. For this purpose several formamidinoderivatives of doxorubicin were synthesized. The aim of our study was to investigate effects of the five formamidinodoxorubicins in the ES-2 human ovarian clear cell carcinoma line, for comparison with data obtained previously for SKOV-3 human ovarian adenocarcinoma cells, to answer the question of whether and to what extent the histological cell type is a possible determinant of sensitivity to tested anthracyclines.
MATERIALS AND METHODS: In our experimental work the following methods were used: spectrophotometric assays with MTT; fluorimetric assays - double staining with Hoechst 33258 and propidium iodide (PI), measurement of caspase-3, -8, -9 activity, intracellular accumulation of DOX and analogues, estimation of drug uptake, mitochondrial transmembrane potential; flow cytometry - phosphatidylserine (PS) externalization with annexin V-FITC and PI fluorochromes.
RESULTS: Effects of the derivatives of doxorubicin were partially linked with the specific type of cancer cell although intracellular accumulation and cellular uptake of DOX and derivatives were similar in both. All of the investigated derivatives were considerably more cytotoxic than DOX. Formamidinodoxorubicins were able to induce caspase-dependent apoptotic cell death in both cell types.
CONCLUSIONS: All new formamidine derivatives of DOX were able to induce caspase - dependent apoptosis in human ovarian cancer cell lines SKOV-3 and ES-2. Obtained results suggested that formamidine derivatives of DOX may be promising candidates for the prospective chemotherapeutic agents for the two different histological subtypes of ovarian cancer.
MATERIALS AND METHODS: In our experimental work the following methods were used: spectrophotometric assays with MTT; fluorimetric assays - double staining with Hoechst 33258 and propidium iodide (PI), measurement of caspase-3, -8, -9 activity, intracellular accumulation of DOX and analogues, estimation of drug uptake, mitochondrial transmembrane potential; flow cytometry - phosphatidylserine (PS) externalization with annexin V-FITC and PI fluorochromes.
RESULTS: Effects of the derivatives of doxorubicin were partially linked with the specific type of cancer cell although intracellular accumulation and cellular uptake of DOX and derivatives were similar in both. All of the investigated derivatives were considerably more cytotoxic than DOX. Formamidinodoxorubicins were able to induce caspase-dependent apoptotic cell death in both cell types.
CONCLUSIONS: All new formamidine derivatives of DOX were able to induce caspase - dependent apoptosis in human ovarian cancer cell lines SKOV-3 and ES-2. Obtained results suggested that formamidine derivatives of DOX may be promising candidates for the prospective chemotherapeutic agents for the two different histological subtypes of ovarian cancer.
Wollina U, Langner D, Hansel G, Haroske G
Pegylated liposomal-encapsulated doxorubicin in cutaneous composite lymphoma: A case report.
Medicine (Baltimore). 2016; 95(43):e4796 [PubMed] Free Access to Full Article Related Publications
Pegylated liposomal-encapsulated doxorubicin in cutaneous composite lymphoma: A case report.
Medicine (Baltimore). 2016; 95(43):e4796 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Cutaneous composite lymphomas are very rare. Their treatment depends upon the different contributing lymphoma entities. Peripheral T-cell lymphoma, not otherwise specified, (PTCL-NOS) represents an aggressive lymphoma subtype. Follicular cutaneous B-cell lymphoma (FCBCL) runs an indolent course. Treatment with pegylated liposomal encapsulated doxorubicin (PLE-DOXO) has yet not been reported in this entity.
CASE PRESENTATION: A 73-year-old male patient presented with 3 rapidly growing, painful nodules on his left leg. He was diagnosed as composite cutaneous lymphoma consisting of PTCL-NOS and FCBCL. All lesions had been surgically removed. Staging was unremarkable. After 4 months a relapse occurred with involvement of inguinal lymph nodes and systemic treatment with PEL-DOXO 20 mg/ m every 3 weeks was initiated. After 6 cycles PLE-DOXO, which were well tolerated without grade 3 or 4 toxicities, a mixed response was obtained with complete remission of cutaneous lesions.Lymph nodes were treated by radiotherapy. A second relapse occurred after 8 months and various polychemotherapy regimens were applied without remission. The overall survival was 28 months.
CONCLUSION: PEL-DOXO is a possible initial systemic treatment in case of PCTL-NOS. Whether polychemotherapy offers an advantage for survival remains questionable but further investigations are needed.
CASE PRESENTATION: A 73-year-old male patient presented with 3 rapidly growing, painful nodules on his left leg. He was diagnosed as composite cutaneous lymphoma consisting of PTCL-NOS and FCBCL. All lesions had been surgically removed. Staging was unremarkable. After 4 months a relapse occurred with involvement of inguinal lymph nodes and systemic treatment with PEL-DOXO 20 mg/ m every 3 weeks was initiated. After 6 cycles PLE-DOXO, which were well tolerated without grade 3 or 4 toxicities, a mixed response was obtained with complete remission of cutaneous lesions.Lymph nodes were treated by radiotherapy. A second relapse occurred after 8 months and various polychemotherapy regimens were applied without remission. The overall survival was 28 months.
CONCLUSION: PEL-DOXO is a possible initial systemic treatment in case of PCTL-NOS. Whether polychemotherapy offers an advantage for survival remains questionable but further investigations are needed.
Zhang L, Lu J, Qiu L
Synergistic effects of A-B-C-type amphiphilic copolymer on reversal of drug resistance in MCF-7/ADR breast carcinoma.
Int J Nanomedicine. 2016; 11:5205-5220 [PubMed] Free Access to Full Article Related Publications
Synergistic effects of A-B-C-type amphiphilic copolymer on reversal of drug resistance in MCF-7/ADR breast carcinoma.
Int J Nanomedicine. 2016; 11:5205-5220 [PubMed] Free Access to Full Article Related Publications
P-glycoprotein (P-gp) overexpression has become the most common cause of occurrence of multidrug resistance in clinical settings. We aimed to construct a micellar polymer carrier to sensitize drug-resistant tumors to doxorubicin (DOX). This A-B-C-type amphiphilic copolymer was prepared by the sequential linkage of β-cyclodextrin, hydrophobic poly(d,l-lactide), and hydrophilic poly(ethylene glycol). Upon incubation of the DOX-loaded micelles with DOX-resistant human breast carcinoma MCF-7/ADR cells, significantly enhanced cytotoxicity and apoptosis were achieved. A series of studies on the action mechanism showed that the polymer components such as β-cyclodextrin, hydrophobic poly(d,l-lactide) segment, and poly(ethylene glycol) coordinatively contributed to the improved intracellular ATP depletion and ATPase activity, increased intracellular uptake of P-gp substrates via competitive binding to P-gp, and decreased P-gp expression in MCF-7/ADR cells. More interestingly, a similar phenomenon was observed in the zebrafish xenograft model, resulting in ~64% inhibition of MCF-7/ADR tumor growth. These results implied that the polymeric micelles displayed great potentials as P-gp modulators to reverse DOX resistance in MCF-7/ADR breast carcinoma.
Hu D, Mezghrani O, Zhang L, et al.
GE11 peptide modified and reduction-responsive hyaluronic acid-based nanoparticles induced higher efficacy of doxorubicin for breast carcinoma therapy.
Int J Nanomedicine. 2016; 11:5125-5147 [PubMed] Free Access to Full Article Related Publications
GE11 peptide modified and reduction-responsive hyaluronic acid-based nanoparticles induced higher efficacy of doxorubicin for breast carcinoma therapy.
Int J Nanomedicine. 2016; 11:5125-5147 [PubMed] Free Access to Full Article Related Publications
Novel breast carcinoma dual-targeted redox-responsive nanoparticles (NPs) based on cholesteryl-hyaluronic acid conjugates were designed for intracellular delivery of the antitumor drug doxorubicin (DOX). A series of reduction-responsive hyaluronic acid derivatives grafted with hydrophobic cholesteryl moiety (HA-ss-Chol) and GE11 peptide conjugated HA-ss-Chol (GE11-HA-ss-Chol) were synthesized. The obtained conjugates showed attractive self-assembly characteristics and high drug loading capacity. GE11-HA-ss-Chol NPs were highly stable under conditions mimicking normal physiological conditions, while showing a fast degradation of the vehicle's structure and accelerating the drug release dramatically in the presence of intracellular reductive environment. Furthermore, the cellular uptake assay confirmed GE11-HA-ss-Chol NPs were taken up by MDA-MB-231 cells through CD44- and epidermal growth factor receptor-mediated endocytosis. The internalization pathways of GE11-HA-ss-Chol NPs might involve clathrin-mediated endocytosis and macropinocytosis. The intracellular distribution of DOX in GE11-HA-ss-Chol NPs showed a faster release and more efficient nuclear delivery than the insensitive control. Enhanced in vitro cytotoxicity of GE11-HA-ss-Chol DOX-NPs further confirmed the superiority of their dual-targeting and redox-responsive capacity. Moreover, in vivo imaging investigation in MDA-MB-231 tumor-bearing mice confirmed that GE11-HA-ss-Chol NPs labeled with 1,1'-dioctadecyl-3,3,3',3'-tetramethylindotricarbocyanine iodide, a near-infrared fluorescence dye, possessed a preferable tumor accumulation ability as compared to the single-targeting counterpart (HA-ss-Chol NPs). The antitumor efficacy showed an improved therapy efficacy and lower systemic side effect. These results suggest GE11-HA-ss-Chol NPs provide a good potential platform for antitumor drugs.
Wu J, Xue X, Zhang B, et al.
Enhanced antitumor activity and attenuated cardiotoxicity of Epirubicin combined with Paeonol against breast cancer.
Tumour Biol. 2016; 37(9):12301-12313 [PubMed] Related Publications
Enhanced antitumor activity and attenuated cardiotoxicity of Epirubicin combined with Paeonol against breast cancer.
Tumour Biol. 2016; 37(9):12301-12313 [PubMed] Related Publications
Epirubicin is widely used for the therapy of various breast cancers. However, it has serious adverse side effects, particularly cardiotoxicity, which can cause irreversible damage in patients. Paeonol, an active component from Moutan Cortex, enhances antitumor activity of antineoplastics and reduces toxicities induced by chemotherapeutics. In this study, we investigated the anticancer activity of Paeonol in combination with Epirubicin against breast cancer and the alleviated effect of Paeonol on cardiotoxicity induced by Epirubicin. The apoptosis results and the coefficient of drug interaction values suggested significantly synergistic in combination of Paeonol and Epirubicin to 4T1 and MCF-7 cells. We further examined antitumor activities of Paeonol or/and Epirubicin in vivo in BALB/c mice and found that co-treatment of Paeonol and Epirubicin had a synergistic inhibitory effect on tumor growth and enhanced apoptosis in tumors in vivo compared with Epirubicin alone. Increased apoptosis was associated with the activation of apoptosis-related proteins including PARP, Bax, caspase 3, and inhibition of p38/JNK/ERK MAPKs. Moreover, Paeonol exhibited a mitigative effect on Epirubicin-induced cardiotoxicity through suppressing NF-kB pathway. In conclusion, Paeonol (a) enhanced the antitumor activity of Epirubicin in a synergistic manner against breast cancer cells via inhibiting p38/JNK/ERK MAPKs and (b) alleviated Epirubicin-induced cardiotoxicity by suppressing NF-kB pathway. These findings suggest that combination of Paeonol and Epirubicin is potentially applicable for breast cancer treatment.
Drozd E, Krzysztoń-Russjan J, Marczewska J, et al.
Up-regulation of glutathione-related genes, enzyme activities and transport proteins in human cervical cancer cells treated with doxorubicin.
Biomed Pharmacother. 2016; 83:397-406 [PubMed] Related Publications
Up-regulation of glutathione-related genes, enzyme activities and transport proteins in human cervical cancer cells treated with doxorubicin.
Biomed Pharmacother. 2016; 83:397-406 [PubMed] Related Publications
Doxorubicin (DOX), one of the most effective anticancer drugs, acts in a variety of ways including DNA damage, enzyme inhibition and generation of reactive oxygen species. Glutathione (GSH) and glutathione-related enzymes including: glutathione peroxidase (GPX), glutathione reductase (GSR) and glutathione S-transferases (GST) may play a role in adaptive detoxification processes in response to the oxidative stress, thus contributing to drug resistance phenotype. In this study, we investigated effects of DOX treatment on expression and activity of GSH-related enzymes and multidrug resistance-associated proteins in cultured human cervical cancer cells displaying different resistance against this drug (HeLa and KB-V1). Determination of expression level of genes encoding GST isoforms and MRP proteins (GCS, GPX, GSR, GSTA1-3, GSTM1, GSTP1, ABCC1-3, MGST1-3) was performed using StellARray™ Technology. Enzymatic activities of GPX and GSR were measured using biochemical methods. Expression of MRP1 was examined by immunofluorescence microscopy. This study showed that native expression levels of GSTM1 and GSTA3 were markedly higher in KB-V1 cells (2000-fold and 200-fold) compared to HeLa cells. Resistant cells have also shown significantly elevated expression of GSTA1 and GSTA2 genes (200-fold and 50-fold) as a result of DOX treatment. In HeLa cells, exposure to DOX increased expression of all genes: GSTM1 (7-fold) and GSTA1-3 (550-fold, 150-fold and 300-fold). Exposure to DOX led to the slight increase of GCS expression as well as GPX activity in KB-V1 cells, while in HeLa cells it did not. Expression of ABCC1 (MRP1) was not increased in any of the tested cell lines. Our results indicate that expression of GSTM1 and GSTA1-3 genes is up-regulated by DOX treatment and suggest that activity of these genes may be associated with drug resistance of the tested cells. At the same time, involvement of MRP1 in DOX resistance in the given experimental conditions is unlikely.
Alinejad V, Hossein Somi M, Baradaran B, et al.
Co-delivery of IL17RB siRNA and doxorubicin by chitosan-based nanoparticles for enhanced anticancer efficacy in breast cancer cells.
Biomed Pharmacother. 2016; 83:229-240 [PubMed] Related Publications
Co-delivery of IL17RB siRNA and doxorubicin by chitosan-based nanoparticles for enhanced anticancer efficacy in breast cancer cells.
Biomed Pharmacother. 2016; 83:229-240 [PubMed] Related Publications
Overexpression of IL17RB is associated with poor prognosis and short survival of the breast cancer patients.IL17RB/IL17B signaling triggers a substantial increase in the cell growth, proliferation and migration through the activation of NF-κB as well as the up-regulation of the Bcl-2. In this study we designed carboxymethyl dextran (CMD) Chitosan nanoparticles (ChNPs) to encapsulated IL17RB siRNA and doxorubicin (DOX) as an anticancer drug. Then we investigated the efficiency of the simultaneous delivery of drug/siRNA on viability and gene expression of MDA-MB361 cell lines. Furthermore the efficacy of dual agent nanoparticles to induce apoptosis and inhibit migration of breast cancer cells was assessed by Annexin-V and wound healing assays respectively. Our results showed that DOX-siRNA-CMD-ChNPs had about 114nm size; with polydispersity index and zeta potential about 0.3 and 10.1mV respectively. Fourier transform infrared spectroscopy (FTIR) confirmed the formation of DOX-siRNA-CMD-ChNPs complex. In addition IL17RB siRNA had significant effect on DOX-induced cytotoxicity in MDA-MB361 cells. Furthermore treatment with dual agent nanoparticles resulted in a significant silencing of NF-κB and Bcl-2 relative gene expression, apoptosis induction and migration inhibition in MDA-MB361 cells. In conclusion, co-delivery of IL17RB siRNA and DOX can be considered as an effective system for the treatment of breast cancer.
Venturini M, Sallemi C, Agostini G, et al.
Chemoembolization with drug eluting beads preloaded with irinotecan (DEBIRI) vs doxorubicin (DEBDOX) as a second line treatment for liver metastases from cholangiocarcinoma: a preliminary study.
Br J Radiol. 2016; 89(1067):20160247 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
Chemoembolization with drug eluting beads preloaded with irinotecan (DEBIRI) vs doxorubicin (DEBDOX) as a second line treatment for liver metastases from cholangiocarcinoma: a preliminary study.
Br J Radiol. 2016; 89(1067):20160247 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
OBJECTIVE: The aim of our preliminary study was to compare the efficacy of drug-eluting beads preloaded with irinotecan (DEBIRI) vs drug-eluting beads preloaded with doxorubicin (DEBDOX) as second-line treatment of unresectable liver metastases from cholangiocarcinoma (CCA).
METHODS: In 2013, 10 patients affected by multiple liver metastases from CCA, resistant to the first-line chemotherapy regimen, were enrolled: 5 patients were submitted to lobar/segmental transarterial chemoembolization (TACE) with DEBIRI (100-mg irinotecan/1 vial) and 5 patients with DEBDOX (50-mg doxorubicin/1 vial), performed every 3 weeks. Patients treated with DEBIRI received antipain premedication consisting of 30-mg of morphine and 3-4 ml of intra-arterial lidocaine. Complications and efficacy were assessed (response evaluation criteria in solid tumour 1.1).
RESULTS: A total of 32 TACE were performed (mean: 3.2 TACE/patient), all well tolerated, with only 1 case of asymptomatic cholecystitis spontaneously recovered. Response rates of patients treated with DEBDOX and DEBIRI were: 4/5 progressive disease and 1/5 partial response vs 2/5 partial response, 2/5 stable disease and 1/5 progressive disease, respectively, with the appearance of variable necrosis percentage. Progression-free survival from the first procedure and progressive disease were 12.67 weeks for DEBIRI and 15.78 weeks for DEBDOX, respectively. Overall survival from time of primary diagnosis was 176 weeks for DEBIRI and 125 weeks for DEBDOX, respectively.
CONCLUSION: In our preliminary experience, DEBIRI was more effective than DEBDOX as a second-line treatment for hepatic metastases from CCA. Antipain drug administration and the use of the microcatheter led to a good treatment tolerability and a low complication rate. Advances in knowledge: In our preliminary experience, DEBIRI was more effective than DEBDOX as a second-line treatment of hepatic metastases from CCA; further studies involving a larger cohort of patients are needed.
METHODS: In 2013, 10 patients affected by multiple liver metastases from CCA, resistant to the first-line chemotherapy regimen, were enrolled: 5 patients were submitted to lobar/segmental transarterial chemoembolization (TACE) with DEBIRI (100-mg irinotecan/1 vial) and 5 patients with DEBDOX (50-mg doxorubicin/1 vial), performed every 3 weeks. Patients treated with DEBIRI received antipain premedication consisting of 30-mg of morphine and 3-4 ml of intra-arterial lidocaine. Complications and efficacy were assessed (response evaluation criteria in solid tumour 1.1).
RESULTS: A total of 32 TACE were performed (mean: 3.2 TACE/patient), all well tolerated, with only 1 case of asymptomatic cholecystitis spontaneously recovered. Response rates of patients treated with DEBDOX and DEBIRI were: 4/5 progressive disease and 1/5 partial response vs 2/5 partial response, 2/5 stable disease and 1/5 progressive disease, respectively, with the appearance of variable necrosis percentage. Progression-free survival from the first procedure and progressive disease were 12.67 weeks for DEBIRI and 15.78 weeks for DEBDOX, respectively. Overall survival from time of primary diagnosis was 176 weeks for DEBIRI and 125 weeks for DEBDOX, respectively.
CONCLUSION: In our preliminary experience, DEBIRI was more effective than DEBDOX as a second-line treatment for hepatic metastases from CCA. Antipain drug administration and the use of the microcatheter led to a good treatment tolerability and a low complication rate. Advances in knowledge: In our preliminary experience, DEBIRI was more effective than DEBDOX as a second-line treatment of hepatic metastases from CCA; further studies involving a larger cohort of patients are needed.
Seifi-Najmi M, Hajivalili M, Safaralizadeh R, et al.
SiRNA/DOX lodeded chitosan based nanoparticles: Development, Characterization and in vitro evaluation on A549 lung cancer cell line.
Cell Mol Biol (Noisy-le-grand). 2016; 62(11):87-94 [PubMed] Related Publications
SiRNA/DOX lodeded chitosan based nanoparticles: Development, Characterization and in vitro evaluation on A549 lung cancer cell line.
Cell Mol Biol (Noisy-le-grand). 2016; 62(11):87-94 [PubMed] Related Publications
High-mobility group AT-hook2 (HMGA2), involved in epithelial mesenchymal transition (EMT) process, has a pivotal role in lung cancer metastasis. Lung cancer therapy with HMGA2 suppressing small interfering RNA (siRNA) has been introduced recently while doxorubicin (DOX) has been used as a frequent cancer chemotherapy agent. Both reagents have been faced with obstacles in clinic which make them ineffective. NanoParticles (NPs) provided a platform for efficient co delivery of the anticancer drugs. The aim of this study was production and in vitro characterization of different pharmacological groups (siRNA, DOX or siRNA-DOX) of carboxymethyl dextran thrimethyl chitosan nanoparticles (CMDTMChiNPs) on cytotoxicity, gene expression, apoptosis and migration of metastatic lung cancer cell line (A-549). CMDTMChiNPs were synthesized and encapsulated with siRNA, DOX or siRNA-DOX. Then the effects of HMGA2 siRNA and DOX co delivery was assessed in A549 viability and target genes (HMGA2, Ecadherin, vimentin and MMP9) by MTT and real time PCR, respectively. In addition capability of apoptosis induction and anti-migratory features of formulated NPs were analyzed by flowcytometry and wound healing assays. SiRNA-DOX-CMDTM ChiNPs approximate size were 207±5 with poly dispersity index (PDI) and zeta potential of 0.4 and 16.3±0.3, respectively. NPs loaded with DOX and siRNA were the most efficient drug formulations in A549 cell cytotoxicity, altering of EMT markers, apoptosis induction and migration inhibition. Generally our results showed that co delivery of HMGA2 siRNA and DOX by novel designed CMDTMChiNPs is a new therapeutic approach with great potential efficiency for lung cancer treatment.
Xie GL, Guo DP, Li ZG, et al.
Application of radiofrequency thermocoagulation combined with adriamycin injection in dorsal root ganglia for controlling refractory pain induced by rib metastasis of lung cancer (a STROBE-compliant article).
Medicine (Baltimore). 2016; 95(40):e4785 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
Application of radiofrequency thermocoagulation combined with adriamycin injection in dorsal root ganglia for controlling refractory pain induced by rib metastasis of lung cancer (a STROBE-compliant article).
Medicine (Baltimore). 2016; 95(40):e4785 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
This study aimed to observe the therapeutic effects and adverse reactions of radiofrequency thermocoagulation combined with adriamycin injection in dorsal root ganglia on lung cancer rib metastasis-related refractory pain which has no response to conventional therapy.This study contained 27 patients with lung cancer rib metastasis-related moderate or severe pain which had no response to conventional therapy. Under computed tomography (CT)-guidance, radiofrequency puncture need reached the corresponding intervertebral foramens to ensure needle point near dorsal root ganglia (DRG) by sensory and motor stimulation tests, and then radiofrequency thermocoagulation was performed on each corresponding DRG followed by injection of 0.5 to 1 mL of adriamycin (0.5%). The conditions of pain and complications were observed before management and 3 days, 1 month, and 3 months after management, respectively.Numerical rating scale (NRS) scores and dosage of morphine were all significantly decreased after management as compared with those before management (all P < 0.01). Although the number of patients with chest wall numbness was significantly increased after management as compared with that before management (all P < 0.01), the degree of chest wall numbness was tolerable. There were no statistical differences between before and after management in nausea and vomiting, and constipation.CT-guided radiofrequency thermocoagulation combined with adriamycin injection in DRG can effectively control lung cancer rib metastasis-related pain which has no response to conventional therapy. This combinatory treatment regimen is featured by better therapeutic effects and a few complications, so it is worthy of being recommended in clinical application.
Shen H, Wang D, Li L, et al.
MiR-222 promotes drug-resistance of breast cancer cells to adriamycin via modulation of PTEN/Akt/FOXO1 pathway.
Gene. 2017; 596:110-118 [PubMed] Related Publications
MiR-222 promotes drug-resistance of breast cancer cells to adriamycin via modulation of PTEN/Akt/FOXO1 pathway.
Gene. 2017; 596:110-118 [PubMed] Related Publications
BACKGROUND AND PURPOSE: Acquisition of resistance to adriamycin (ADR) is one of the most important clinical obstacles in the treatment of breast cancer, but the molecular mechanisms underlying sensitivity to ADR remain elusive. In our previous study, through miRNA microarray and experiments, we have emphasized that miR-222 could promote the ADR-resistance in breast cancer cells. The aim of this study was to explore the possible mechanism by which miR-222 affects sensitivity to ADR.
METHODS: Through pathway enrichment analyses for miR-222, we found that PTEN/Akt/FOXO1 signaling pathway may be of importance. RT-qPCR analyses and western blot assays confirmed the relationship between miR-222 expression and target genes. Immunofluorescence further visually displayed the location of FOXO1. When blocking PTEN/Akt/FOXO1 signaling pathway, we demonstrated the effects of miR-222-mediated ADR resistance by MTT and apoptosis assays.
RESULTS: RT-qPCR and Western blot results showed that miR-222 expression was negatively correlated with FOXO1 expression. In addition, the subcellular translocation of FOXO1 due to the altered expression of miR-222 was observed from immunofluorescence. Moreover, upregulation of miR-222 expression in MCF-7/S cells is associated with decreased PTEN expression levels and increased phospho-Akt (p-Akt) expression. Conversely in MCF-7/ADR cells, inhibition of miR-222 resulted in increased PTEN expression and decreased p-Akt expression. For further validation, results of the present study also demonstrated that PTEN/Akt/FOXO1 signaling was responsible for the ADR-resistance of breast cancer cells since LY294002, an inhibitor of Akt signaling, partially increased the sensitivity of MCF-7/S cells to ADR. More importantly, we postulated that high expression of miR-222 is closely related to poor overall survival by TCGA database validation.
CONCLUSIONS: Taken together, these data elucidated that miR-222 mediated ADR-resistance of breast cancer cells partly through regulation of PTEN/Akt/FOXO1 signaling pathway and inhibition of miR-222 may improve the prognosis of breast cancer patients.
METHODS: Through pathway enrichment analyses for miR-222, we found that PTEN/Akt/FOXO1 signaling pathway may be of importance. RT-qPCR analyses and western blot assays confirmed the relationship between miR-222 expression and target genes. Immunofluorescence further visually displayed the location of FOXO1. When blocking PTEN/Akt/FOXO1 signaling pathway, we demonstrated the effects of miR-222-mediated ADR resistance by MTT and apoptosis assays.
RESULTS: RT-qPCR and Western blot results showed that miR-222 expression was negatively correlated with FOXO1 expression. In addition, the subcellular translocation of FOXO1 due to the altered expression of miR-222 was observed from immunofluorescence. Moreover, upregulation of miR-222 expression in MCF-7/S cells is associated with decreased PTEN expression levels and increased phospho-Akt (p-Akt) expression. Conversely in MCF-7/ADR cells, inhibition of miR-222 resulted in increased PTEN expression and decreased p-Akt expression. For further validation, results of the present study also demonstrated that PTEN/Akt/FOXO1 signaling was responsible for the ADR-resistance of breast cancer cells since LY294002, an inhibitor of Akt signaling, partially increased the sensitivity of MCF-7/S cells to ADR. More importantly, we postulated that high expression of miR-222 is closely related to poor overall survival by TCGA database validation.
CONCLUSIONS: Taken together, these data elucidated that miR-222 mediated ADR-resistance of breast cancer cells partly through regulation of PTEN/Akt/FOXO1 signaling pathway and inhibition of miR-222 may improve the prognosis of breast cancer patients.


 Thyroid Cancer
Thyroid Cancer