Found this page useful?
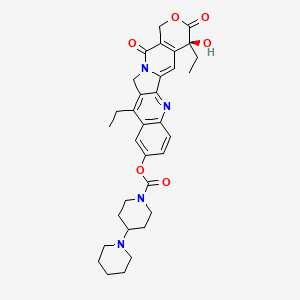
Irinotecan
 Web Resources: Irinotecan
Web Resources: Irinotecan Recent Research Publications
Recent Research PublicationsWeb Resources: Irinotecan (6 links)
Cancer Research UK
Macmillan Cancer Support
NHS Evidence
 Irinotecan - Substance Summary
Irinotecan - Substance Summary
PubChem
Irish Cancer Society
MedlinePlus
Recent Research Publications
Chang SM, Christian W, Wu MH, et al.
Novel indolizino[8,7-b]indole hybrids as anti-small cell lung cancer agents: Regioselective modulation of topoisomerase II inhibitory and DNA crosslinking activities.
Eur J Med Chem. 2017; 127:235-249 [PubMed] Related Publications
Novel indolizino[8,7-b]indole hybrids as anti-small cell lung cancer agents: Regioselective modulation of topoisomerase II inhibitory and DNA crosslinking activities.
Eur J Med Chem. 2017; 127:235-249 [PubMed] Related Publications
A novel series of bis(hydroxymethyl)indolizino[8,7-b]indole hybrids composed of β-carboline (topoisomerase I/II inhibition) and bis(hydroxymethyl)pyrrole (DNA cross-linking) are synthesized for antitumor evaluation. Of tumor cell lines tested, small cell lung cancer (SCLC) cell lines are the most sensitive to the newly synthesized compounds. These hybrids induce cell cycle arrest at the G2/M phase, trigger tumor cell apoptotic death, and display diverse mechanisms of action involving topoisomerase II (Topo II) inhibition and induction of DNA cross-linking. Intriguingly, the substituent at N(11) (H or Me) plays a critical role in modulating Topo II inhibition and DNA cross-linking activities. N(11)-Me derivatives predispose to induce DNA crosslinks, whereas N(11)-H derivatives potently inhibit Topo II. Computational analysis implicates that N(11)-Me restrict the torsion angles of the two adjacent OH on pyrrole resulting in a favorable of DNA cross-linking. Among these hybrids, compound 17a with N(11)-H is more effective than cisplatin and etoposide, but as potent as irinotecan, against the growth of SCLC H526 cells in xenograft model.
Chisaki Y, Nakamura N, Yano Y
Time-Series Modeling and Simulation for Comparative Cost-Effective Analysis in Cancer Chemotherapy: An Application to Platinum-Based Regimens for Advanced Non-small Cell Lung Cancer.
Biol Pharm Bull. 2017; 40(1):73-81 [PubMed] Related Publications
Time-Series Modeling and Simulation for Comparative Cost-Effective Analysis in Cancer Chemotherapy: An Application to Platinum-Based Regimens for Advanced Non-small Cell Lung Cancer.
Biol Pharm Bull. 2017; 40(1):73-81 [PubMed] Related Publications
The purpose of this study was to propose a time-series modeling and simulation (M&S) strategy for probabilistic cost-effective analysis in cancer chemotherapy using a Monte-Carlo method based on data available from the literature. The simulation included the cost for chemotherapy, for pharmaceutical care for adverse events (AEs) and other medical costs. As an application example, we describe the analysis for the comparison of four regimens, cisplatin plus irinotecan, carboplatin plus paclitaxel, cisplatin plus gemcitabine (GP), and cisplatin plus vinorelbine, for advanced non-small cell lung cancer. The factors, drug efficacy explained by overall survival or time to treatment failure, frequency and severity of AEs, utility value of AEs to determine QOL, the drugs' and other medical costs in Japan, were included in the model. The simulation was performed and quality adjusted life years (QALY) and incremental cost-effectiveness ratios (ICER) were calculated. An index, percentage of superiority (%SUP) which is the rate of the increased cost vs. QALY-gained plots within the area of positive QALY-gained and also below some threshold values of the ICER, was calculated as functions of threshold values of the ICER. An M&S process was developed, and for the simulation example, the GP regimen was the most cost-effective, in case of threshold values of the ICER=$70000/year, the %SUP for the GP are more than 50%. We developed an M&S process for probabilistic cost-effective analysis, this method would be useful for decision-making in choosing a cancer chemotherapy regimen in terms of pharmacoeconomic.
Vinzens S, Zindel J, Zweifel M, et al.
Granulocyte Colony-stimulating Factor Producing Anaplastic Carcinoma of the Pancreas: Case Report and Review of the Literature.
Anticancer Res. 2017; 37(1):223-228 [PubMed] Related Publications
Granulocyte Colony-stimulating Factor Producing Anaplastic Carcinoma of the Pancreas: Case Report and Review of the Literature.
Anticancer Res. 2017; 37(1):223-228 [PubMed] Related Publications
We report on the case of a 67-year-old man with granulocyte colony-stimulating factor (G-CSF) producing anaplastic carcinoma of the pancreas. Preoperative routine tests revealed an elevated white blood cell (WBC) count of 25.2 G/l, consisting almost exclusively of neutrophilic granulocytes (23.31 G/l) with a predominance of segmented neutrophils (78% of all neutrophilic granulocytes), and elevated levels of C-reactive protein at 87 mg/l. Upon surgery, local tumour infiltration was more extensive than expected from preoperative imaging. However, no peritoneal dissemination was found and curative resection was attempted. Only seven days after the operation, signs of relapse were seen upon computed tomograpy. Histology revealed an undifferentiated anaplastic carcinoma, on the basis of a poorly differentiated ductal adenocarcinoma. Immunohistochemistry demonstrated G-CSF and G-CSF-Receptor expression in some CD68-positive syncytial macrophages. Granulocyte colony-stimulating factor (G-CSF) in serum was elevated at 5.6 pg/ml, which further raised to 43 pg/ml one week after FOLFIRINOX chemotherapy (oxaliplatin, irinotecan, 5-fluorouracil), while WBC decreased from 103.3 G/l to 59.3 G/l. Granulocyte macrophage-colony stimulating factor (GM-CSF) in serum was normal (<0.5 pg/ml). The patient died on postoperative day 34.
Chen Q, Cheng M, Wang Z, Zhao S
The efficacy and safety of panitumumab plus irrinotecan-based chemotherapy in the treatment of metastatic colorectal cancer: A meta-analysis.
Medicine (Baltimore). 2016; 95(50):e5284 [PubMed] Free Access to Full Article Related Publications
The efficacy and safety of panitumumab plus irrinotecan-based chemotherapy in the treatment of metastatic colorectal cancer: A meta-analysis.
Medicine (Baltimore). 2016; 95(50):e5284 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Panitumumab, a fully human monoclonal antibody targeting epidermal growth factor receptor, is used in combination with chemotherapy for patients with metastatic colorectal cancer (mCRC). However, the effects of panitumumab in combination with irrinotecan-based chemotherapy remain uncertain. Therefore, we conducted this meta-analysis to assess the efficacy and safety of combination treatment of panitumumab plus chemotherapy in the treatment of mCRC.
METHODS: By searching electronic databases (PubMed, Embase, and Web of Science), all clinical trials which assessed the effects of panitumumab plus irrinotecan-based chemotherapy in mCRC would be included. Main outcome measures included progression-free survival (PFS), overall survival (OS), overall response rate (ORR), and adverse events. Pooled estimates were calculated by a fixed-effects model or random-effects model, according to the heterogeneity among the included studies.
RESULTS: Eleven trials with a total number of 1338 patients met the inclusion criteria and were included in this meta-analysis. The combination treatment of panitumumab and irrinotecan-based chemotherapy was associated with a median PFS of 5.83 months, OS of 11.15 months, and ORR of 33%. Subgroup analysis showed that, in the first-line and second-line treatment, the combination therapy for PFS was 9.27 and 5.01 months, for OS was 8.87 and 11.68 months, and for ORR was 61% and 26%, respectively. In the wild-type and mutant KRAS populations, the combination therapy for PFS was 5.76 and 5.27 months, for OS was 11.15 and 10.64 months, and for ORR was 37% and 18%, respectively. Moreover, combination therapy also induced an incidence of 56% treatment-related adverse events.
CONCLUSION: Panitumumab plus irrinotecan-based chemotherapy is effective and well-tolerated in the treatment of patients with mCRC, especially in those with wild-type KRAS tumors.
METHODS: By searching electronic databases (PubMed, Embase, and Web of Science), all clinical trials which assessed the effects of panitumumab plus irrinotecan-based chemotherapy in mCRC would be included. Main outcome measures included progression-free survival (PFS), overall survival (OS), overall response rate (ORR), and adverse events. Pooled estimates were calculated by a fixed-effects model or random-effects model, according to the heterogeneity among the included studies.
RESULTS: Eleven trials with a total number of 1338 patients met the inclusion criteria and were included in this meta-analysis. The combination treatment of panitumumab and irrinotecan-based chemotherapy was associated with a median PFS of 5.83 months, OS of 11.15 months, and ORR of 33%. Subgroup analysis showed that, in the first-line and second-line treatment, the combination therapy for PFS was 9.27 and 5.01 months, for OS was 8.87 and 11.68 months, and for ORR was 61% and 26%, respectively. In the wild-type and mutant KRAS populations, the combination therapy for PFS was 5.76 and 5.27 months, for OS was 11.15 and 10.64 months, and for ORR was 37% and 18%, respectively. Moreover, combination therapy also induced an incidence of 56% treatment-related adverse events.
CONCLUSION: Panitumumab plus irrinotecan-based chemotherapy is effective and well-tolerated in the treatment of patients with mCRC, especially in those with wild-type KRAS tumors.
Coriat R, Faivre SJ, Mir O, et al.
Pharmacokinetics and safety of DTS-108, a human oligopeptide bound to SN-38 with an esterase-sensitive cross-linker in patients with advanced malignancies: a Phase I study.
Int J Nanomedicine. 2016; 11:6207-6216 [PubMed] Free Access to Full Article Related Publications
Pharmacokinetics and safety of DTS-108, a human oligopeptide bound to SN-38 with an esterase-sensitive cross-linker in patients with advanced malignancies: a Phase I study.
Int J Nanomedicine. 2016; 11:6207-6216 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: DTS-108 is a hydrosoluble prodrug, where the SN-38 moiety is covalently linked to a 20-amino acid vector peptide by a specific esterase-sensitive cross-linker, releasing 7-ethyl-10-hydroxycampthotecin (SN-38) by esterase bond cleavage.
METHODS: The pharmacokinetics of DTS-108, adverse events graded according to NCI-CTCv3.1, dose-limiting toxicities at cycle 1, the maximum tolerated dose (MTD), and the recommended Phase II dose (RP2D) of intravenous DTS-108 (1-2 hours) every 2 weeks were evaluated in a first-in-human Phase I study in patients with advanced/metastatic carcinomas, according to an accelerated dose escalation design. SN-38 and SN-38 glucuronide (SN-38G) levels were evaluated with fluorescence high-performance liquid chromatography (HPLC) test, then liquid chromatography-tandem mass spectrometry (LC/MS/MS) methods.
RESULTS: Forty-two patients received DTS-108 across 14 dosing cohorts (range 3-416 mg/m(2)). At 416 mg/m(2), three out of six patients had grade 4 neutropenia thereby defining the MTD and the RP2D at 313 mg/m(2). Fluorescence HPLC was inaccurate to quantify DTS-108 and its metabolites (SN-38 and SN-38G). New processes and analytical LC/MS/MS methods for testing SN-38 were implemented. At a dose of 313 mg/m(2), mean DTS-108, SN-38, and SN-38G area under the plasma concentration-time curve to infinity (coefficients of variation %) were 439,293 (24%), 1,992 (34%), and 4,538 (46%) h·ng/mL. Stable disease (according to Response Evaluation Criteria in Solid Tumors) was observed in nine patients.
CONCLUSION: Assessing SN-38 concentration using fluorescence HPLC is questionable since this method failed to monitor dose escalation of DTS-108, a new topoisomerase I inhibitor, due to ex vivo degradation. LC/MS/MS methods were consistent in evaluating SN-38 exposures allowing drug monitoring. The maximum tolerated dose of DTS-108 was 416 mg/m(2). The RP2D for intravenous DTS-108 was 313 mg/m(2) every 2 weeks in patients with advanced/metastatic solid tumors.
METHODS: The pharmacokinetics of DTS-108, adverse events graded according to NCI-CTCv3.1, dose-limiting toxicities at cycle 1, the maximum tolerated dose (MTD), and the recommended Phase II dose (RP2D) of intravenous DTS-108 (1-2 hours) every 2 weeks were evaluated in a first-in-human Phase I study in patients with advanced/metastatic carcinomas, according to an accelerated dose escalation design. SN-38 and SN-38 glucuronide (SN-38G) levels were evaluated with fluorescence high-performance liquid chromatography (HPLC) test, then liquid chromatography-tandem mass spectrometry (LC/MS/MS) methods.
RESULTS: Forty-two patients received DTS-108 across 14 dosing cohorts (range 3-416 mg/m(2)). At 416 mg/m(2), three out of six patients had grade 4 neutropenia thereby defining the MTD and the RP2D at 313 mg/m(2). Fluorescence HPLC was inaccurate to quantify DTS-108 and its metabolites (SN-38 and SN-38G). New processes and analytical LC/MS/MS methods for testing SN-38 were implemented. At a dose of 313 mg/m(2), mean DTS-108, SN-38, and SN-38G area under the plasma concentration-time curve to infinity (coefficients of variation %) were 439,293 (24%), 1,992 (34%), and 4,538 (46%) h·ng/mL. Stable disease (according to Response Evaluation Criteria in Solid Tumors) was observed in nine patients.
CONCLUSION: Assessing SN-38 concentration using fluorescence HPLC is questionable since this method failed to monitor dose escalation of DTS-108, a new topoisomerase I inhibitor, due to ex vivo degradation. LC/MS/MS methods were consistent in evaluating SN-38 exposures allowing drug monitoring. The maximum tolerated dose of DTS-108 was 416 mg/m(2). The RP2D for intravenous DTS-108 was 313 mg/m(2) every 2 weeks in patients with advanced/metastatic solid tumors.
Suzuki A, Kobayashi R, Fujii H, et al.
Control of Nausea and Vomiting in Patients with Colorectal Cancer Receiving Chemotherapy with Moderate Emetic Risk.
Anticancer Res. 2016; 36(12):6527-6533 [PubMed] Related Publications
Control of Nausea and Vomiting in Patients with Colorectal Cancer Receiving Chemotherapy with Moderate Emetic Risk.
Anticancer Res. 2016; 36(12):6527-6533 [PubMed] Related Publications
BACKGROUND: Chemotherapy with moderate emetic risk (MEC), including irinotecan-based and oxaliplatin-based chemotherapy regimens, are predominantly used for colorectal cancer chemotherapy. Chemotherapy-induced nausea and vomiting (CINV) remain unsatisfactorily controlled.
PATIENTS AND METHODS: The rates of prevalence of antiemetic medication and the control of CINV were investigated from medical records in patients with colorectal cancer who received the first cycle of irinotecan-based or oxaliplatin-based regimens. Risks for CINV were determined by multivariate logistic regression analysis.
RESULTS: A total of 179 patients received the first cycle of MEC regimens and the number of overall cycles was 2,176 during the study period from January 2013 to December 2015. Guideline-consistent antiemetic medication was performed in most cases. The rate of no-CINV was nearly 90% during the overall period. Female sex and age under 50 years were significant risks for CINV. Comparison considering only the group aged 50 years or more indicated that the control of CINV was significantly worse in irinotecan-based regimens than in the oxaliplatin-based regimens.
CONCLUSION: Female sex and age younger than 50 years were significant risks for CINV in patients receiving MEC for colorectal cancer. Moreover, the control of CINV was less sufficient for irinotecan-based than for oxaliplatin-based regimens.
PATIENTS AND METHODS: The rates of prevalence of antiemetic medication and the control of CINV were investigated from medical records in patients with colorectal cancer who received the first cycle of irinotecan-based or oxaliplatin-based regimens. Risks for CINV were determined by multivariate logistic regression analysis.
RESULTS: A total of 179 patients received the first cycle of MEC regimens and the number of overall cycles was 2,176 during the study period from January 2013 to December 2015. Guideline-consistent antiemetic medication was performed in most cases. The rate of no-CINV was nearly 90% during the overall period. Female sex and age under 50 years were significant risks for CINV. Comparison considering only the group aged 50 years or more indicated that the control of CINV was significantly worse in irinotecan-based regimens than in the oxaliplatin-based regimens.
CONCLUSION: Female sex and age younger than 50 years were significant risks for CINV in patients receiving MEC for colorectal cancer. Moreover, the control of CINV was less sufficient for irinotecan-based than for oxaliplatin-based regimens.
Li DZ, Zhang QZ, Wang CY, et al.
Synthesis and antitumor activity of novel substituted uracil-1'(N)-acetic acid ester derivatives of 20(S)-camptothecins.
Eur J Med Chem. 2017; 125:1235-1246 [PubMed] Related Publications
Synthesis and antitumor activity of novel substituted uracil-1'(N)-acetic acid ester derivatives of 20(S)-camptothecins.
Eur J Med Chem. 2017; 125:1235-1246 [PubMed] Related Publications
A series of novel substituted uracil-1'(N)-acetic acid esters (6-20) of camptothecins (CPTs) were synthesized by the acylation method. These new compounds were evaluated for in vitro antitumor activity against tumor cell lines, A549, Bel7402, BGC-823, HCT-8 and A2780. In vitro results showed that most of the derivatives exhibited comparable or superior cytotoxicity compare to CPT (1) and topotecan (TPT, 2), with 12 and 13 possessing the best efficacy. Four compounds, 9, 12, 13 and 16, were selected to be evaluated for in vivo antitumor activity against H22, BGC-823 and Bel-7402 in mice. In vivo testing results indicated that 12 and 13 had antitumor activity against mouse liver carcinoma H22 close to Paclitaxel and cyclophosphamide. 12 had similar antitumor activity against human gastric carcinoma BGC-823 in nude mice compared to irinotecan (3) and possessed better antitumor activity against human hepatocarcinoma Bel-7402 in nude mice than 2. It is also discovered that 12 showed a similar mechanism but better inhibitory activity on topoisomerase I (Topo I) compared to 2. These findings indicate that 20(S)-O-fluorouracil-1'(N)-acetic acid ester derivative of CPTs, 12, could be developed as an antitumor drug candidate for clinical trial.
Sartore-Bianchi A, Siena S, Tonini G, et al.
Overcoming dynamic molecular heterogeneity in metastatic colorectal cancer: Multikinase inhibition with regorafenib and the case of rechallenge with anti-EGFR.
Cancer Treat Rev. 2016; 51:54-62 [PubMed] Related Publications
Overcoming dynamic molecular heterogeneity in metastatic colorectal cancer: Multikinase inhibition with regorafenib and the case of rechallenge with anti-EGFR.
Cancer Treat Rev. 2016; 51:54-62 [PubMed] Related Publications
In metastatic colorectal cancer (mCRC), fluorouracil-based combination therapy with oxaliplatin or irinotecan is the mainstay of first-line treatment. Patient survival has been significantly improved with the introduction of monoclonal antibodies against VEGF (bevacizumab), VEGFR2 (ramucirumab) or EGFR (cetuximab or panitumumab) in first- and second-line therapies. However, all patients treated with chemotherapy and targeted therapies will eventually relapse, and recently the emergence of alterations in EGFR, RAS, BRAF, ERB-B2, MET and possibly in other genes has been shown to jeopardize response to EGFR blockade. In chemorefractory patients, multikinase inhibition with regorafenib has proved to be effective and rechallenge with chemotherapy or anti-EGFR agents is empirically pursued. This review will critically discuss how the evolving knowledge of mechanisms of resistance driven by intratumoural dynamic molecular heterogeneity can impact on rational choice of treatments in this setting.
Chen K, Gong Y, Zhang Q, et al.
Efficacy and safety of addition of bevacizumab to FOLFIRI or irinotecan/bolus 5-FU/LV (IFL) in patients with metastatic colorectal cancer: A meta-analysis.
Medicine (Baltimore). 2016; 95(46):e5221 [PubMed] Free Access to Full Article Related Publications
Efficacy and safety of addition of bevacizumab to FOLFIRI or irinotecan/bolus 5-FU/LV (IFL) in patients with metastatic colorectal cancer: A meta-analysis.
Medicine (Baltimore). 2016; 95(46):e5221 [PubMed] Free Access to Full Article Related Publications
Recent studies have paid much attention on the safety of bevacizumab as adjuvant chemotherapy for metastatic colorectal cancer. The aim of this meta-analysis was to study the efficacy and safety of bevacizumab in combination with irinotecan, bolus followed by infusional 5-fluorouracil, and leucovorin (FOLFIRI) and, irinotecan, bolus fluorouracil, leucovorin (IFL) for patients with metastatic colorectal cancer (mCRC).An electronic search of related trials was conducted from PubMed, EMBASE, Cochrane Library databases. Risk ratio (RRs) and its 95% confidence intervals (95% CIs) were calculated by using either DerSimonian-Laird method or Mantel-Haenszel method according to the heterogeneity of included articles. The risk of mortality, therapeutic efficacy, and adverse effect were meta-analyzed.In total, 6 RCTs including 2165 participants (1109 in the treatment group, 1056 in the control group) were included in this meta-analysis. Compared with FOLFIRI-panitumumab/cetuximab, the bevacizumab addition significantly reduced the complete response (CR) rate (RR [95%CI] = 0.31[0.11, 0.89], P = 0.03) and the risk of grade 3/4 adverse event (RR [95%CI] = 0.89[0.80, 0.98], P = 0.01). Compared with FOLFIRI and IFL alone, the addition of bevacizumb significantly increased the partial response (PR) and objective response (OR) rates. Compared with IFL alone, the addition of bevacizumb significantly reduced the mortality risk of PFS (RR [95%CI] = 0.53[0.42, 0.66], P < 0.00001) and OS (RR[95%CI] = 0.70[0.60, 0.82], P < 0.00001), but increased the risk of adverse events (RR[95%CI] = 1.14[1.06, 1.21], P = 0.0002).Combination chemotherapy of bevacizumab plus FOLFIRI or IFL had a relative high efficacy and acceptable safety for treatment of mCRC.
Iseki Y, Shibutani M, Maeda K, et al.
Prognostic Significance of MicroRNA-21 Expression in Patients with Unresectable Metastatic Colon Cancer.
Anticancer Res. 2016; 36(10):5145-5151 [PubMed] Related Publications
Prognostic Significance of MicroRNA-21 Expression in Patients with Unresectable Metastatic Colon Cancer.
Anticancer Res. 2016; 36(10):5145-5151 [PubMed] Related Publications
BACKGROUND/AIM: MicroRNA (miR)-21 is overexpressed in most solid tumors and a high expression of miR-21 in tumor tissue is associated with a poor clinical outcome. The aim of this study was to clarify the association between the miR-21 expression in the tumor and the chemotherapeutic outcomes and survival for unresectable metastatic colon cancer (CC).
MATERIALS AND METHODS: Formalin-fixed, paraffin-embedded (FFPE) samples of primary tumor were obtained from 32 patients who underwent primary tumor resection and received palliative chemotherapy for unresectable metastatic CC. MiR-21 was extracted from the FFPE and the expression of miR-21 was evaluated using quantitative real time-polymerase chain reaction (RT-PCR). The expression of miR-21 was calculated with 2-ΔΔCT.
RESULTS: A high miR-21 expression was associated with reduced progression-free survival (PFS) (p=0.0109) and tended to reduce overall survival (OS) (p=0.0675).
CONCLUSION: miR-21 expression might be a useful prognostic marker for chemotherapeutic outcome and survival in patients with unresectable metastatic CC.
MATERIALS AND METHODS: Formalin-fixed, paraffin-embedded (FFPE) samples of primary tumor were obtained from 32 patients who underwent primary tumor resection and received palliative chemotherapy for unresectable metastatic CC. MiR-21 was extracted from the FFPE and the expression of miR-21 was evaluated using quantitative real time-polymerase chain reaction (RT-PCR). The expression of miR-21 was calculated with 2-ΔΔCT.
RESULTS: A high miR-21 expression was associated with reduced progression-free survival (PFS) (p=0.0109) and tended to reduce overall survival (OS) (p=0.0675).
CONCLUSION: miR-21 expression might be a useful prognostic marker for chemotherapeutic outcome and survival in patients with unresectable metastatic CC.
Cercek A, Boucher TM, Gluskin JS, et al.
Response rates of hepatic arterial infusion pump therapy in patients with metastatic colorectal cancer liver metastases refractory to all standard chemotherapies.
J Surg Oncol. 2016; 114(6):655-663 [PubMed] Related Publications
Response rates of hepatic arterial infusion pump therapy in patients with metastatic colorectal cancer liver metastases refractory to all standard chemotherapies.
J Surg Oncol. 2016; 114(6):655-663 [PubMed] Related Publications
BACKGROUND AND OBJECTIVES: To evaluate the role of hepatic arterial infusion (HAI) in patients with metastatic colorectal cancer (mCRC) liver metastases (LM) refractory to oxaliplatin, irinotecan, and fluorouracil-based treatments.
METHODS: A search identified patients with mCRC treated after tumor progression on at least three standard systemic therapies.
RESULTS: One hundred and ten patients met criteria for inclusion (i.e., progression on at least three standard agents). Fifty seven patients had LM-only and 53 patients had LM and low volume extrahepatic metastases (LME). Patients with LM-only and LME had a response rate (RR) of 33% and 36%, median survival of 20 months and 11.4 months, respectively. Patients with LM-only had progression free survival of 6 months and hepatic progression free survival of 7.56 months. In a secondary analysis, 46 patients were RECIST-refractory to all standard therapies: LM-only (n = 24) and LME (n = 22). LM-only and LME had a RR of 29% and 36%, and median survival 17.2 months and 9.1 months, respectively.
CONCLUSIONS: Patients with refractory mCRC LM can achieve a response to HAI resulting in antitumor activity and improvement in survival. Responses are rarely seen in such heavily treated patients with systemic therapy alone, suggesting a regional directed approach is useful. J. Surg. Oncol. 2016;114:655-663. © 2016 Wiley Periodicals, Inc.
METHODS: A search identified patients with mCRC treated after tumor progression on at least three standard systemic therapies.
RESULTS: One hundred and ten patients met criteria for inclusion (i.e., progression on at least three standard agents). Fifty seven patients had LM-only and 53 patients had LM and low volume extrahepatic metastases (LME). Patients with LM-only and LME had a response rate (RR) of 33% and 36%, median survival of 20 months and 11.4 months, respectively. Patients with LM-only had progression free survival of 6 months and hepatic progression free survival of 7.56 months. In a secondary analysis, 46 patients were RECIST-refractory to all standard therapies: LM-only (n = 24) and LME (n = 22). LM-only and LME had a RR of 29% and 36%, and median survival 17.2 months and 9.1 months, respectively.
CONCLUSIONS: Patients with refractory mCRC LM can achieve a response to HAI resulting in antitumor activity and improvement in survival. Responses are rarely seen in such heavily treated patients with systemic therapy alone, suggesting a regional directed approach is useful. J. Surg. Oncol. 2016;114:655-663. © 2016 Wiley Periodicals, Inc.
Ponzetti A, Pinta F, Spadi R, et al.
Jaw osteonecrosis associated with aflibercept, irinotecan and fluorouracil: attention to oral district.
Tumori. 2016; 102(Suppl. 2) [PubMed] Related Publications
Jaw osteonecrosis associated with aflibercept, irinotecan and fluorouracil: attention to oral district.
Tumori. 2016; 102(Suppl. 2) [PubMed] Related Publications
INTRODUCTION: The antiangiogenic monoclonal antibody aflibercept in association with fluorouracil and irinotecan improves the survival of patients with metastatic colorectal cancer (mCRC) treated previously with oxaliplatin-based therapy. Multiple reports raised the hypothesis that the concomitant use of antiresorptive drugs and antiangiogenic drugs may increase the risk of osteonecrosis of the jaw (ONJ). Some reports have been published regarding cases of ONJ during treatment with bevacizumab for mCRC.
CASE DESCRIPTION: Here we describe the first reported case of ONJ occurring in a 64-year-old woman with untreated periodontitis and episodic previous pyorrhea occurring during treatment with aflibercept plus FOLFIRI during the expanded-access program.
CONCLUSIONS: This case report warrants further investigation into the potential association between the use of anti-VEGF agents and ONJ. Given the serious nature of ONJ, we recommend that particular attention be paid to the oral district prior to treating patients and during treatment with chemotherapy and targeted agents, especially anti-VEGF agents. Such measures could also be useful in reducing the incidence of stomatitis.
CASE DESCRIPTION: Here we describe the first reported case of ONJ occurring in a 64-year-old woman with untreated periodontitis and episodic previous pyorrhea occurring during treatment with aflibercept plus FOLFIRI during the expanded-access program.
CONCLUSIONS: This case report warrants further investigation into the potential association between the use of anti-VEGF agents and ONJ. Given the serious nature of ONJ, we recommend that particular attention be paid to the oral district prior to treating patients and during treatment with chemotherapy and targeted agents, especially anti-VEGF agents. Such measures could also be useful in reducing the incidence of stomatitis.
Koshkin S, Danilova A, Raskin G, et al.
Primary cultures of human colon cancer as a model to study cancer stem cells.
Tumour Biol. 2016; 37(9):12833-12842 [PubMed] Related Publications
Primary cultures of human colon cancer as a model to study cancer stem cells.
Tumour Biol. 2016; 37(9):12833-12842 [PubMed] Related Publications
The principal cause of death in cancer involves tumor progression and metastasis. Since only a small proportion of the primary tumor cells, cancer stem cells (CSCs), which are the most aggressive, have the capacity to metastasize and display properties of stem cells, it is imperative to characterize the gene expression of diagnostic markers and to evaluate the drug sensitivity in the CSCs themselves. Here, we have examined the key genes that are involved in the progression of colorectal cancer and are expressed in cancer stem cells. Primary cultures of colorectal cancer cells from a patient's tumors were studied using the flow cytometry and cytological methods. We have evaluated the clinical and stem cell marker expression in these cells, their resistance to 5-fluorouracil and irinotecan, and the ability of cells to form tumors in mice. The data shows the role of stem cell marker Oct4 in the resistance of primary colorectal cancer tumor cells to 5-fluorouracil.
Venturini M, Sallemi C, Agostini G, et al.
Chemoembolization with drug eluting beads preloaded with irinotecan (DEBIRI) vs doxorubicin (DEBDOX) as a second line treatment for liver metastases from cholangiocarcinoma: a preliminary study.
Br J Radiol. 2016; 89(1067):20160247 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
Chemoembolization with drug eluting beads preloaded with irinotecan (DEBIRI) vs doxorubicin (DEBDOX) as a second line treatment for liver metastases from cholangiocarcinoma: a preliminary study.
Br J Radiol. 2016; 89(1067):20160247 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
OBJECTIVE: The aim of our preliminary study was to compare the efficacy of drug-eluting beads preloaded with irinotecan (DEBIRI) vs drug-eluting beads preloaded with doxorubicin (DEBDOX) as second-line treatment of unresectable liver metastases from cholangiocarcinoma (CCA).
METHODS: In 2013, 10 patients affected by multiple liver metastases from CCA, resistant to the first-line chemotherapy regimen, were enrolled: 5 patients were submitted to lobar/segmental transarterial chemoembolization (TACE) with DEBIRI (100-mg irinotecan/1 vial) and 5 patients with DEBDOX (50-mg doxorubicin/1 vial), performed every 3 weeks. Patients treated with DEBIRI received antipain premedication consisting of 30-mg of morphine and 3-4 ml of intra-arterial lidocaine. Complications and efficacy were assessed (response evaluation criteria in solid tumour 1.1).
RESULTS: A total of 32 TACE were performed (mean: 3.2 TACE/patient), all well tolerated, with only 1 case of asymptomatic cholecystitis spontaneously recovered. Response rates of patients treated with DEBDOX and DEBIRI were: 4/5 progressive disease and 1/5 partial response vs 2/5 partial response, 2/5 stable disease and 1/5 progressive disease, respectively, with the appearance of variable necrosis percentage. Progression-free survival from the first procedure and progressive disease were 12.67 weeks for DEBIRI and 15.78 weeks for DEBDOX, respectively. Overall survival from time of primary diagnosis was 176 weeks for DEBIRI and 125 weeks for DEBDOX, respectively.
CONCLUSION: In our preliminary experience, DEBIRI was more effective than DEBDOX as a second-line treatment for hepatic metastases from CCA. Antipain drug administration and the use of the microcatheter led to a good treatment tolerability and a low complication rate. Advances in knowledge: In our preliminary experience, DEBIRI was more effective than DEBDOX as a second-line treatment of hepatic metastases from CCA; further studies involving a larger cohort of patients are needed.
METHODS: In 2013, 10 patients affected by multiple liver metastases from CCA, resistant to the first-line chemotherapy regimen, were enrolled: 5 patients were submitted to lobar/segmental transarterial chemoembolization (TACE) with DEBIRI (100-mg irinotecan/1 vial) and 5 patients with DEBDOX (50-mg doxorubicin/1 vial), performed every 3 weeks. Patients treated with DEBIRI received antipain premedication consisting of 30-mg of morphine and 3-4 ml of intra-arterial lidocaine. Complications and efficacy were assessed (response evaluation criteria in solid tumour 1.1).
RESULTS: A total of 32 TACE were performed (mean: 3.2 TACE/patient), all well tolerated, with only 1 case of asymptomatic cholecystitis spontaneously recovered. Response rates of patients treated with DEBDOX and DEBIRI were: 4/5 progressive disease and 1/5 partial response vs 2/5 partial response, 2/5 stable disease and 1/5 progressive disease, respectively, with the appearance of variable necrosis percentage. Progression-free survival from the first procedure and progressive disease were 12.67 weeks for DEBIRI and 15.78 weeks for DEBDOX, respectively. Overall survival from time of primary diagnosis was 176 weeks for DEBIRI and 125 weeks for DEBDOX, respectively.
CONCLUSION: In our preliminary experience, DEBIRI was more effective than DEBDOX as a second-line treatment for hepatic metastases from CCA. Antipain drug administration and the use of the microcatheter led to a good treatment tolerability and a low complication rate. Advances in knowledge: In our preliminary experience, DEBIRI was more effective than DEBDOX as a second-line treatment of hepatic metastases from CCA; further studies involving a larger cohort of patients are needed.
Shitara K, Yonesaka K, Denda T, et al.
Randomized study of FOLFIRI plus either panitumumab or bevacizumab for wild-type KRAS colorectal cancer-WJOG 6210G.
Cancer Sci. 2016; 107(12):1843-1850 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
Randomized study of FOLFIRI plus either panitumumab or bevacizumab for wild-type KRAS colorectal cancer-WJOG 6210G.
Cancer Sci. 2016; 107(12):1843-1850 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
This randomized phase II trial compared panitumumab plus fluorouracil, leucovorin, and irinotecan (FOLFIRI) with bevacizumab plus FOLFIRI as second-line chemotherapy for wild-type (WT) KRAS exon 2 metastatic colorectal cancer (mCRC) and to explore the values of oncogenes in circulating tumor DNA (ctDNA) and serum proteins as predictive biomarkers. Patients with WT KRAS exon 2 mCRC refractory to first-line chemotherapy containing oxaliplatin and bevacizumab were randomly assigned to panitumumab plus FOLFIRI or bevacizumab plus FOLFIRI. Of 121 randomly assigned patients, 117 were eligible. Median overall survival (OS) for panitumumab plus FOLFIRI and bevacizumab plus FOLFIRI were 16.2 and 13.4 months [hazard ratio (HR), 1.16; 95% CI, 0.76-1.77], respectively. Progression-free survival (PFS) was also similar (HR, 1.14; 95% CI, 0.78-1.66). KRAS, NRAS, and BRAF status using ctDNA was successfully examined in 109 patients, and mutations were identified in 19 patients (17.4%). Panitumumab plus FOLFIRI showed favorable survival compared with bevacizumab plus FOLFIRI in WT patients and unfavorable survival in those with mutations (P for interaction = 0.026 in OS and 0.054 in PFS). OS with bevacizumab plus FOLFIRI was better than panitumumab plus FOLFIRI in patients with high serum vascular endothelial growth factor-A (VEGF-A) levels and worse in those with low levels (P for interaction = 0.016). Second-line FOLFIRI plus panitumumab and FOLFIRI plus bevacizumab showed a similar efficacy in patients with WT KRAS exon 2 mCRC. RAS and BRAF mutation in ctDNA could be a negative predictive marker for panitumumab.
Pasquini G, Vasile E, Caparello C, et al.
Third-Line Chemotherapy with Irinotecan plus 5-Fluorouracil in Caucasian Metastatic Gastric Cancer Patients.
Oncology. 2016; 91(6):311-316 [PubMed] Related Publications
Third-Line Chemotherapy with Irinotecan plus 5-Fluorouracil in Caucasian Metastatic Gastric Cancer Patients.
Oncology. 2016; 91(6):311-316 [PubMed] Related Publications
PURPOSE: The aim of this study was to evaluate the activity of the combination of 5-fluorouracil/folinic acid and irinotecan (FOLFIRI) as third-line chemotherapy (CT) in metastatic gastric cancer (mGC) patients pretreated with platinum derivatives, fluoropyrimidines, and taxanes.
METHODS: We prospectively collected data of mGC patients treated with third-line FOLFIRI at our institution from 2009 to 2014. Eligible patients should be treated with a fluoropyrimidine-platinum first-line CT and a subsequent taxane-based second-line CT. FOLFIRI consisted of irinotecan 180 mg/m2 and leucovorin 200 mg/m2, followed by 5-fluorouracil 2,800 mg/m2 (administered as 48-hour i.v. continuous infusion from day 1 to 3), with cycles repeated every 2 weeks. Response rate (RR) was evaluated according to RECIST version 1.0, while progression-free (PFS) and overall survival (OS) were estimated using the Kaplan-Meier method.
RESULTS: A total of 33 patients were included. The majority (97%) had good performance status (0-1 according to ECOG), while median PFS after first-line and second-line CT was 5.2 and 4.4 months, respectively. Two patients experienced an objective response (RR: 6%), while 14 patients achieved disease stabilization (disease control rate: 42%). Median PFS and OS from the start of third-line CT were 3.3 and 7.5 months, respectively. Hematological and nonhematological grade 3-4 toxicities were uncommon and included neutropenia (6.1%), diarrhea (9.1%), vomiting (3%), and asthenia (3%). Febrile neutropenia was not reported.
CONCLUSIONS: Third-line CT with FOLFIRI may be an option in heavily pretreated mGC patients with preserved performance status and organ function. This regimen has a favorable safety profile, and signs of activity have been observed after standard first- and second-line CT.
METHODS: We prospectively collected data of mGC patients treated with third-line FOLFIRI at our institution from 2009 to 2014. Eligible patients should be treated with a fluoropyrimidine-platinum first-line CT and a subsequent taxane-based second-line CT. FOLFIRI consisted of irinotecan 180 mg/m2 and leucovorin 200 mg/m2, followed by 5-fluorouracil 2,800 mg/m2 (administered as 48-hour i.v. continuous infusion from day 1 to 3), with cycles repeated every 2 weeks. Response rate (RR) was evaluated according to RECIST version 1.0, while progression-free (PFS) and overall survival (OS) were estimated using the Kaplan-Meier method.
RESULTS: A total of 33 patients were included. The majority (97%) had good performance status (0-1 according to ECOG), while median PFS after first-line and second-line CT was 5.2 and 4.4 months, respectively. Two patients experienced an objective response (RR: 6%), while 14 patients achieved disease stabilization (disease control rate: 42%). Median PFS and OS from the start of third-line CT were 3.3 and 7.5 months, respectively. Hematological and nonhematological grade 3-4 toxicities were uncommon and included neutropenia (6.1%), diarrhea (9.1%), vomiting (3%), and asthenia (3%). Febrile neutropenia was not reported.
CONCLUSIONS: Third-line CT with FOLFIRI may be an option in heavily pretreated mGC patients with preserved performance status and organ function. This regimen has a favorable safety profile, and signs of activity have been observed after standard first- and second-line CT.
Vogel A, Ciardiello F, Hubner RA, et al.
Post-gemcitabine therapy for patients with advanced pancreatic cancer - A comparative review of randomized trials evaluating oxaliplatin- and/or irinotecan-containing regimens.
Cancer Treat Rev. 2016; 50:142-147 [PubMed] Related Publications
Post-gemcitabine therapy for patients with advanced pancreatic cancer - A comparative review of randomized trials evaluating oxaliplatin- and/or irinotecan-containing regimens.
Cancer Treat Rev. 2016; 50:142-147 [PubMed] Related Publications
A systematic review and critical evaluation of randomized trial evidence for oxaliplatin- or irinotecan-containing regimens in patients with advanced pancreatic cancer previously treated with gemcitabine has not yet been published. We conducted a comparative systematic review of randomized trials evaluating oxaliplatin- or irinotecan-based therapies in patients with advanced pancreatic cancer previously treated with gemcitabine to assess trial similarity and the feasibility of performing an indirect treatment comparison (ITC). Studies were identified through PubMed and key oncology conference abstracts. The following trials met our criteria: NAPOLI-1 (nanoliposomal irinotecan [nal-IRI] or nal-IRI+5-fluorouracil [5-FU]/leucovorin [LV] vs 5-FU/LV), CONKO-003 (oxaliplatin+5-FU/LV [OFF] vs 5-FU/LV), PANCREOX (oxaliplatin+5-FU/LV [mFOLFOX6] vs 5-FU/LV), and Yoo et al. (2009) (irinotecan+5-FU/LV [mFOLFIRI3] vs mFOLFOX). Fundamental differences were identified in study design (i.e., number of study sites, number of countries), patient (i.e., locally advanced vs metastatic disease, stratification variables, prior and subsequent treatments) and treatment (i.e., regimens, dose intensity) characteristics, and primary and secondary outcomes (i.e., primary vs secondary outcomes, overall survival [OS], progression-free survival [PFS]) among the 4 included trials. Our comparative review demonstrated significant dissimilarity across trials, which precluded conducting an ITC. In the absence of head-to-head nal-IRI- and/or oxaliplatin-based therapy trials, clinicians are advised to interpret these studies separately within the context of their individual patient population.
Huang CW, Yeh YS, Ma CJ, et al.
Patients with Metastatic Colorectal Cancer and Hyperbilirubinemia Treated with FOLFIRI plus Bevacizumab as First-Line Treatment.
Chemotherapy. 2017; 62(1):80-84 [PubMed] Related Publications
Patients with Metastatic Colorectal Cancer and Hyperbilirubinemia Treated with FOLFIRI plus Bevacizumab as First-Line Treatment.
Chemotherapy. 2017; 62(1):80-84 [PubMed] Related Publications
Metastatic colorectal cancer (mCRC) combined with hyperbilirubinemia is typically considered a contraindication to irinotecan-based therapy, a proven first-line treatment of mCRC. Herein, we present 6 consecutive patients with mCRC combined with hyperbilirubinemia who underwent UGT1A1 genotyping before receiving FOLFIRI plus bevacizumab. Dose escalation of irinotecan was performed according to the results of UGT1A1 genotyping in all patients. Improvement in the serum total bilirubin level to a normal range was noted in all 6 patients. Disease control was 100%. The median progression-free survival was 7.5 months and the median overall survival was 8.5 months. FOLFIRI plus bevacizumab as a first-line chemotherapy may achieve effective disease control and be safe in patients with mCRC and hyperbilirubinemia based on UGT1A1 genotyping. More prospective clinical studies are necessary to evaluate the clinical benefits and safety of this treatment approach.
Kiss I, Mlcochova J, Bortlicek Z, et al.
Efficacy and Toxicity of Panitumumab After Progression on Cetuximab and Predictive Value of MiR-31-5p in Metastatic Wild-type KRAS Colorectal Cancer Patients.
Anticancer Res. 2016; 36(9):4955-9 [PubMed] Related Publications
Efficacy and Toxicity of Panitumumab After Progression on Cetuximab and Predictive Value of MiR-31-5p in Metastatic Wild-type KRAS Colorectal Cancer Patients.
Anticancer Res. 2016; 36(9):4955-9 [PubMed] Related Publications
BACKGROUND: In metastatic colorectal cancer (mCRC), panitumumab is generally considered to be ineffective after the progression on cetuximab therapy. However, few studies have demonstrated that a small subset of mCRC patients may benefit from panitumumab in this setting.
PATIENTS AND METHODS: In our study, wild-type KRAS mCRC patients, enrolled into the nationwide Czech registry CORECT between January 2007 and December 2012, were screened for panitumumab therapy after progression on cetuximab.
RESULTS: We identified 26 mCRC in the registry with well documented progression on cetuximab in combination with irinotecan-based chemotherapy (FOLFIRI or irinotecan alone) who received panitumumab monotherapy. Partial response (PR) was achieved in 3 (11.5%) patients and stable disease (SD) in 7 (26.9%) patients after 8 weeks of therapy. Thirteen (50.0%) patients had evidence of progressive disease (PD) and in 3 (11.5%) cases response was not available. Furthermore, we confirmed that higher expression levels of newly described biomarker, miR-31-5p, in tumor are significantly associated with shorter progression-free survival (PFS) in patients treated with cetuximab (p=0.038); however, we did not observe association between miR-31-5p and response to panitumumab in mCRC patients after progression on cetuximab.
CONCLUSION: It remains possible that a subset of mCRC patients may benefit from panitumumab after progression on cetuximab.
PATIENTS AND METHODS: In our study, wild-type KRAS mCRC patients, enrolled into the nationwide Czech registry CORECT between January 2007 and December 2012, were screened for panitumumab therapy after progression on cetuximab.
RESULTS: We identified 26 mCRC in the registry with well documented progression on cetuximab in combination with irinotecan-based chemotherapy (FOLFIRI or irinotecan alone) who received panitumumab monotherapy. Partial response (PR) was achieved in 3 (11.5%) patients and stable disease (SD) in 7 (26.9%) patients after 8 weeks of therapy. Thirteen (50.0%) patients had evidence of progressive disease (PD) and in 3 (11.5%) cases response was not available. Furthermore, we confirmed that higher expression levels of newly described biomarker, miR-31-5p, in tumor are significantly associated with shorter progression-free survival (PFS) in patients treated with cetuximab (p=0.038); however, we did not observe association between miR-31-5p and response to panitumumab in mCRC patients after progression on cetuximab.
CONCLUSION: It remains possible that a subset of mCRC patients may benefit from panitumumab after progression on cetuximab.
Forgacz K, Agrawal AK, Sawicki T, Marek GW
Second-Line Chemotherapy of Advanced Colorectal Cancer: Predictive and Prognostic Factors.
Adv Clin Exp Med. 2016 Jul-Aug; 25(4):725-32 [PubMed] Related Publications
Second-Line Chemotherapy of Advanced Colorectal Cancer: Predictive and Prognostic Factors.
Adv Clin Exp Med. 2016 Jul-Aug; 25(4):725-32 [PubMed] Related Publications
BACKGROUND: Colorectal cancer progression presents a significant clinical problem. After its dissemination, the foundation of its treatment comprises of palliative chemotherapy.
OBJECTIVES: The aim of this study was to assess the predictive and prognostic value of clinical response to second line treatment (with capecitabine or with a two-drug regimen including irinotecan) and to analyze its relation to selected clinical and pathological variables with respect to time to disease progression.
MATERIAL AND METHODS: The retrospective analysis of 164 patients with advanced colorectal cancer treated in 2001- -2008 included chosen clinical, pathological and follow-up data.
RESULTS: Response to second-line chemotherapy was observed in 34 out of 164 patients: In 18/82 in the irinotecan group (22%) and in 16/82 in the capecitabine group (19.5%). The mean survival time to progression following the second line of treatment amounted to 5.85 and 6.2 months respectively. Statistically, a higher number of patients in good condition of 0 to 1 was documented in the group responding to treatment. Significant correlation was documented between primary stage of the disease and time to progression in patients treated with capecitabine (p = 0.0258). The recurrence of the disease was observed in 44/45 patients following operation with radical intention but with an insufficient number of excised lymph nodes. A significantly longer time to progression was observed in women treated with capecitabine. In logistic regression, lack of treatment response was found to be an independent factor affecting the time to disease progression. Patients who did not respond to the second line of treatment demonstrated a significantly shorter time to disease progression than patients who responded to it and they showed a significantly higher number of patients with leucopenia during treatment.
CONCLUSIONS: Clinical response to treatment in both treated groups is of significant importance for the probability of local recurrence of the disease, preservation of a good patient's condition and the higher level of leukocytes during treatment.
OBJECTIVES: The aim of this study was to assess the predictive and prognostic value of clinical response to second line treatment (with capecitabine or with a two-drug regimen including irinotecan) and to analyze its relation to selected clinical and pathological variables with respect to time to disease progression.
MATERIAL AND METHODS: The retrospective analysis of 164 patients with advanced colorectal cancer treated in 2001- -2008 included chosen clinical, pathological and follow-up data.
RESULTS: Response to second-line chemotherapy was observed in 34 out of 164 patients: In 18/82 in the irinotecan group (22%) and in 16/82 in the capecitabine group (19.5%). The mean survival time to progression following the second line of treatment amounted to 5.85 and 6.2 months respectively. Statistically, a higher number of patients in good condition of 0 to 1 was documented in the group responding to treatment. Significant correlation was documented between primary stage of the disease and time to progression in patients treated with capecitabine (p = 0.0258). The recurrence of the disease was observed in 44/45 patients following operation with radical intention but with an insufficient number of excised lymph nodes. A significantly longer time to progression was observed in women treated with capecitabine. In logistic regression, lack of treatment response was found to be an independent factor affecting the time to disease progression. Patients who did not respond to the second line of treatment demonstrated a significantly shorter time to disease progression than patients who responded to it and they showed a significantly higher number of patients with leucopenia during treatment.
CONCLUSIONS: Clinical response to treatment in both treated groups is of significant importance for the probability of local recurrence of the disease, preservation of a good patient's condition and the higher level of leukocytes during treatment.
Paolicchi E, Vivaldi C, De Gregorio V, et al.
Topoisomerase 1 Promoter Variants and Benefit from Irinotecan in Metastatic Colorectal Cancer Patients.
Oncology. 2016; 91(5):283-288 [PubMed] Related Publications
Topoisomerase 1 Promoter Variants and Benefit from Irinotecan in Metastatic Colorectal Cancer Patients.
Oncology. 2016; 91(5):283-288 [PubMed] Related Publications
OBJECTIVE: Topoisomerase 1 (topo-1) is an important target for the treatment of metastatic colorectal cancer (CRC). The aim of the present study was to evaluate the correlation between topo-1 single-nucleotide polymorphisms (SNPs) and clinical outcome in metastatic CRC (mCRC) patients.
METHODS: With the use of specific software (PROMO 3.0), we performed an in silico analysis of topo-1 promoter SNPs; the rs6072249 and rs34282819 SNPs were included in the study. DNA was extracted from 105 mCRC patients treated with FOLFIRI ± bevacizumab in the first line. SNP genotyping was performed by real-time PCR. Genotypes were correlated with clinical parameters (objective response rate, progression-free survival, and overall survival).
RESULTS: No single genotype was significantly associated with clinical variables. The G allelic variant of rs6072249 topo-1 SNP is responsible for GC factor and X-box-binding protein transcription factor binding. The same allelic variant showed a nonsignificant trend toward a shorter progression-free survival (GG, 7.5 months; other genotypes, 9.3 months; HR 1.823, 95% CI 0.8904-3.734; p = 0.1).
CONCLUSION: Further analyses are needed to confirm that the topo-1 SNP rs6072249 and transcription factor interaction could be a part of tools to predict clinical outcome in mCRC patients treated with irinotecan-based regimens.
METHODS: With the use of specific software (PROMO 3.0), we performed an in silico analysis of topo-1 promoter SNPs; the rs6072249 and rs34282819 SNPs were included in the study. DNA was extracted from 105 mCRC patients treated with FOLFIRI ± bevacizumab in the first line. SNP genotyping was performed by real-time PCR. Genotypes were correlated with clinical parameters (objective response rate, progression-free survival, and overall survival).
RESULTS: No single genotype was significantly associated with clinical variables. The G allelic variant of rs6072249 topo-1 SNP is responsible for GC factor and X-box-binding protein transcription factor binding. The same allelic variant showed a nonsignificant trend toward a shorter progression-free survival (GG, 7.5 months; other genotypes, 9.3 months; HR 1.823, 95% CI 0.8904-3.734; p = 0.1).
CONCLUSION: Further analyses are needed to confirm that the topo-1 SNP rs6072249 and transcription factor interaction could be a part of tools to predict clinical outcome in mCRC patients treated with irinotecan-based regimens.
Horii N, Morioka D, Yamaguchi K, et al.
Bowel strangulation caused by massive intraperitoneal adhesion due to effective chemotherapy for multiple peritoneal metastases originating from descending colon cancer.
Clin J Gastroenterol. 2016; 9(5):306-11 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
Bowel strangulation caused by massive intraperitoneal adhesion due to effective chemotherapy for multiple peritoneal metastases originating from descending colon cancer.
Clin J Gastroenterol. 2016; 9(5):306-11 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
We describe a case of bowel strangulation caused by massive peritoneal adhesion as a result of effective chemotherapy. A 71-year-old man, who had obstructive descending colon cancer with massive peritoneal metastases and, therefore, received palliative surgery consisting of diverting colostomy and sampling of peritoneal nodules, developed bowel strangulation on day 4 of the 2nd course of chemotherapy, including irinotecan, l-leucovorin, and 5-fluorouracil. Emergent celiotomy showed a massive intraperitoneal adhesion formed around several intestinal loops, which were not observed at the prior surgery. One loop was strangled, but recovered by adhesiotomy alone. Intestinal loops were formed around aggregates of peritoneal nodules as the centers, several of which were then sampled. We closed the abdomen after all intestinal loops were eradicated by total enterolysis. Fortunately, the patient has been doing well and received chemotherapy without recurrent bowel obstruction 10 months after the present episode. Histological findings of the aggregates causing intestinal loops demonstrated extensive necrosis of cancerous tissue surrounded by fibrosis with abundant lymphocyte infiltration. These findings were not observed in the specimen sampled before chemotherapy, suggesting that intestinal loops were caused by inflammatory adhesion occurring around the peritoneal metastases as a result of effectiveness of chemotherapy.
Rodrigues D, Longatto-Filho A, Martins SF
Predictive Biomarkers in Colorectal Cancer: From the Single Therapeutic Target to a Plethora of Options.
Biomed Res Int. 2016; 2016:6896024 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
Predictive Biomarkers in Colorectal Cancer: From the Single Therapeutic Target to a Plethora of Options.
Biomed Res Int. 2016; 2016:6896024 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
Colorectal cancer (CRC) is one of the most frequent cancers and is a leading cause of cancer death worldwide. Treatments used for CRC may include some combination of surgery, radiation therapy, chemotherapy, and targeted therapy. The current standard drugs used in chemotherapy are 5-fluorouracil and leucovorin in combination with irinotecan and/or oxaliplatin. Most recently, biologic agents have been proven to have therapeutic benefits in metastatic CRC alone or in association with standard chemotherapy. However, patients present different treatment responses, in terms of efficacy and toxicity; therefore, it is important to identify biological markers that can predict the response to therapy and help select patients that would benefit from specific regimens. In this paper, authors review CRC genetic markers that could be useful in predicting the sensitivity/resistance to chemotherapy.
Dean A, Byrne A, Marinova M, Hayden I
Clinical Outcomes of Patients with Rare and Heavily Pretreated Solid Tumors Treated according to the Results of Tumor Molecular Profiling.
Biomed Res Int. 2016; 2016:4627214 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
Clinical Outcomes of Patients with Rare and Heavily Pretreated Solid Tumors Treated according to the Results of Tumor Molecular Profiling.
Biomed Res Int. 2016; 2016:4627214 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
Patients with heavily pretreated advanced cancer or with rare tumors are difficult to treat. Molecular profiling (MP) of tumors to identify biomarkers that predict potential outcomes with individual therapies is an emerging strategy to guide treatment decisions. Patients with rare tumors for which standard-of-care therapy was unavailable or more common tumors for which standard-of-care options had been exhausted underwent MP at a single Australian center. Data regarding treating physicians' choice of therapy, MP results and recommendations, and patient outcomes were collected. Seven patients had received prior standard first-line therapy (PST), 16 had rare tumors, and 31 had been heavily pretreated (HPT; ≥2 prior lines). Most treatments suggested by MP (541/594; 91.1%) were common chemotherapy drugs available in generic formulations. MP-guided therapy recommendations differed from physician's recommendations in 48 patients (88.9%). MP-guided therapy produced clinical benefit (improved QOL and/or performance status, symptoms, bodyweight, or RECIST) in 19/31 (61.3%), 11/16 (68.8%), and 3/7 (42.9%) patients with HPTs, rare tumors, and PSTs, respectively, and had a PFS ratio ≥1.3 in 22/37 evaluable patients (59.5%; 95% confidence interval 44-76%). The null hypothesis that ≤15% of these patients would have a PFS ratio ≥1.3 was rejected (one-sided p < 0.0001). In conclusion, using MP to guide therapy selection is feasible in clinical practice and may improve patient outcomes.
Kentepozidis N, Economopoulou P, Christofyllakis C, et al.
Salvage treatment with irinotecan/cisplatin versus pemetrexed/cisplatin in patients with non-small cell lung cancer pre-treated with a non-platinum-based regimen in the first-line setting: a randomized phase II study of the Hellenic Oncology Research Group (HORG).
Clin Transl Oncol. 2017; 19(3):317-325 [PubMed] Related Publications
Salvage treatment with irinotecan/cisplatin versus pemetrexed/cisplatin in patients with non-small cell lung cancer pre-treated with a non-platinum-based regimen in the first-line setting: a randomized phase II study of the Hellenic Oncology Research Group (HORG).
Clin Transl Oncol. 2017; 19(3):317-325 [PubMed] Related Publications
BACKGROUND: Platinum-based chemotherapy is the standard front-line treatment for patients with advanced non-small cell lung cancer (NSCLC). However, non-platinum combinations of third-generation chemotherapeutic agents are considered an alternative therapeutic option for patients who cannot tolerate the toxic effects of platinum compounds. In this study, the efficacy and toxicity of the combination of irinotecan plus cisplatin (IC) was compared to pemetrexed plus cisplatin (PC) regimen, in platinum-naïve patients with advanced NSCLC, who had been previously treated with the combination of a taxane plus gemcitabine.
PATIENTS AND METHODS: A total of 124 patients with locally advanced or metastatic NSCLC were randomly assigned to either irinotecan 110 mg/m(2) on day 1 and 100 mg/m(2) on day 8 plus cisplatin 80 mg/m(2) on day 8 every 3 weeks (IC arm) or pemetrexed 500 mg/m(2) plus cisplatin 80 mg/m(2) on day 1 every 3 weeks (PC arm). The primary endpoint of the study was the overall response rate (ORR).
RESULTS: The ORR and median progression-free survival (PFS) in the IC arm were 18 % and 3.3 months, respectively, while in the PC arm were 19 % and 4.2 months (p = ns). Median overall survival (OS) was significantly higher in patients with PC (6.9 vs. 10.9; p = 0.013). PC regimen had a better toxicity profile compared to IC, with a statistically significant lower incidence of grade 3/4 neutropenia (3 vs. 31 %; p = 0.0001) and diarrhea (1.6 vs. 14.7 %, p = 0.018).
CONCLUSIONS: In patients with advanced NSCLC pretreated with docetaxel/gemcitabine, the combination of pemetrexed/cisplatin is associated with increased OS and is better tolerated than the combination of irinotecan/cisplatin and should be considered as a valid therapeutic option for platinum-naive, previously treated patients. CLINICALTRIALS.
GOV IDENTIFIER: NCT00614965.
PATIENTS AND METHODS: A total of 124 patients with locally advanced or metastatic NSCLC were randomly assigned to either irinotecan 110 mg/m(2) on day 1 and 100 mg/m(2) on day 8 plus cisplatin 80 mg/m(2) on day 8 every 3 weeks (IC arm) or pemetrexed 500 mg/m(2) plus cisplatin 80 mg/m(2) on day 1 every 3 weeks (PC arm). The primary endpoint of the study was the overall response rate (ORR).
RESULTS: The ORR and median progression-free survival (PFS) in the IC arm were 18 % and 3.3 months, respectively, while in the PC arm were 19 % and 4.2 months (p = ns). Median overall survival (OS) was significantly higher in patients with PC (6.9 vs. 10.9; p = 0.013). PC regimen had a better toxicity profile compared to IC, with a statistically significant lower incidence of grade 3/4 neutropenia (3 vs. 31 %; p = 0.0001) and diarrhea (1.6 vs. 14.7 %, p = 0.018).
CONCLUSIONS: In patients with advanced NSCLC pretreated with docetaxel/gemcitabine, the combination of pemetrexed/cisplatin is associated with increased OS and is better tolerated than the combination of irinotecan/cisplatin and should be considered as a valid therapeutic option for platinum-naive, previously treated patients. CLINICALTRIALS.
GOV IDENTIFIER: NCT00614965.
Ploquin A, Zerimech F, Escande F, et al.
Lack of Relationship Between Clinical Features and KRAS Mutations in Patients with Metastatic Colorectal Cancer.
Anticancer Res. 2016; 36(8):4233-6 [PubMed] Related Publications
Lack of Relationship Between Clinical Features and KRAS Mutations in Patients with Metastatic Colorectal Cancer.
Anticancer Res. 2016; 36(8):4233-6 [PubMed] Related Publications
BACKGROUND/AIM: We previously identified three clinical predictive factors of efficacy of cetuximab-irinotecan. Here, we analyzed the clinical characteristics of patients with metastatic colorectal cancer (CRC) in order to detect potent correlations with KRAS mutations.
PATIENTS AND METHODS: We conducted a retrospective, multicenter study between 2008 and 2012. We included patients with metastatic colorectal adenocarcinomas, previously treated by irinotecan, and with an available KRAS mutation test.
RESULTS: We included 299 patients. The median age was 60 years; the median number of metastatic sites was 2. One hundred and eight patients (36.1%) had a previous objective response to irinotecan. The median interval between diagnosis and irinotecan discontinuation was 1.94 years. A KRAS mutation was detected in 133 patients (44.5%). In univariate and multivariate analyses, none of the assessed factors was associated with the presence of a KRAS mutation.
CONCLUSION: No easily clinically assessable parameter was significantly associated with KRAS mutations in patients with colorectal cancer.
PATIENTS AND METHODS: We conducted a retrospective, multicenter study between 2008 and 2012. We included patients with metastatic colorectal adenocarcinomas, previously treated by irinotecan, and with an available KRAS mutation test.
RESULTS: We included 299 patients. The median age was 60 years; the median number of metastatic sites was 2. One hundred and eight patients (36.1%) had a previous objective response to irinotecan. The median interval between diagnosis and irinotecan discontinuation was 1.94 years. A KRAS mutation was detected in 133 patients (44.5%). In univariate and multivariate analyses, none of the assessed factors was associated with the presence of a KRAS mutation.
CONCLUSION: No easily clinically assessable parameter was significantly associated with KRAS mutations in patients with colorectal cancer.
Zhang X, Shimodaira H, Soeda H, et al.
CpG island methylator phenotype is associated with the efficacy of sequential oxaliplatin- and irinotecan-based chemotherapy and EGFR-related gene mutation in Japanese patients with metastatic colorectal cancer.
Int J Clin Oncol. 2016; 21(6):1091-1101 [PubMed] Related Publications
CpG island methylator phenotype is associated with the efficacy of sequential oxaliplatin- and irinotecan-based chemotherapy and EGFR-related gene mutation in Japanese patients with metastatic colorectal cancer.
Int J Clin Oncol. 2016; 21(6):1091-1101 [PubMed] Related Publications
BACKGROUND: The CpG island methylator phenotype (CIMP) with multiple promoter methylated loci has been observed in a subset of human colorectal cancer (CRC) cases. CIMP status, which is closely associated with specific clinicopathological and molecular characteristics, is considered a potential predictive biomarker for efficacy of cancer treatment. However, the relationship between the effect of standard chemotherapy, including cytotoxic drugs and anti-epidermal growth factor receptor (EGFR) antibodies, and CIMP status has not been elucidated.
METHODS: In 125 metastatic colorectal cancer (mCRC) patients, we investigated how clinical outcome of chemotherapy was related to CIMP status as detected by methylation-specific PCR (MSP) and to genetic status in five EGFR-related genes (KRAS, BRAF, PIK3CA, NRAS, and AKT1) as detected by direct sequencing.
RESULTS: CIMP-positive status was significantly associated with proximal tumor location and peritoneum metastasis (all P values <0.05). The progression-free survival of patients with CIMP-positive tumors receiving sequential therapy with FOLFOX as the first-line treatment followed by irinotecan-based therapy as the second-line treatment (median = 6.6 months) was inferior to that of such patients receiving the reverse sequence (median = 15.2 months; P = 0.043). Furthermore, CIMP-positive tumors showed higher mutation frequencies for the five EGFR-related genes (74.1 %) than the CIMP-negative tumors did (50.0 %). Among the KRAS wild-type tumors, CIMP-positive tumors were associated with a worse clinical outcome than CIMP-negative tumors following anti-EGFR antibody therapy.
CONCLUSION: Sequential FOLFOX followed by an irinotecan-based regimen is unfavorable in patients with CIMP-positive tumors. High frequencies of mutation in EGFR-related genes in CIMP-positive tumors may cause the lower response to anti-EGFR antibody therapy seen in patients with wild-type KRAS and CIMP-positive tumors.
METHODS: In 125 metastatic colorectal cancer (mCRC) patients, we investigated how clinical outcome of chemotherapy was related to CIMP status as detected by methylation-specific PCR (MSP) and to genetic status in five EGFR-related genes (KRAS, BRAF, PIK3CA, NRAS, and AKT1) as detected by direct sequencing.
RESULTS: CIMP-positive status was significantly associated with proximal tumor location and peritoneum metastasis (all P values <0.05). The progression-free survival of patients with CIMP-positive tumors receiving sequential therapy with FOLFOX as the first-line treatment followed by irinotecan-based therapy as the second-line treatment (median = 6.6 months) was inferior to that of such patients receiving the reverse sequence (median = 15.2 months; P = 0.043). Furthermore, CIMP-positive tumors showed higher mutation frequencies for the five EGFR-related genes (74.1 %) than the CIMP-negative tumors did (50.0 %). Among the KRAS wild-type tumors, CIMP-positive tumors were associated with a worse clinical outcome than CIMP-negative tumors following anti-EGFR antibody therapy.
CONCLUSION: Sequential FOLFOX followed by an irinotecan-based regimen is unfavorable in patients with CIMP-positive tumors. High frequencies of mutation in EGFR-related genes in CIMP-positive tumors may cause the lower response to anti-EGFR antibody therapy seen in patients with wild-type KRAS and CIMP-positive tumors.
Hu W, Fang J, Nie J, et al.
Efficacy and safety of extended use of platinum-based doublet chemotherapy plus endostatin in patients with advanced nonsmall cell lung cancer.
Medicine (Baltimore). 2016; 95(28):e4183 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
Efficacy and safety of extended use of platinum-based doublet chemotherapy plus endostatin in patients with advanced nonsmall cell lung cancer.
Medicine (Baltimore). 2016; 95(28):e4183 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
The aim of this study was to investigate the efficacy and safety of the extended use of platinum-based doublet chemotherapy (PT-DC) plus endostatin in patients with advanced nonsmall cell lung cancer (NSCLC).We performed a retrospective analysis of 200 newly diagnosed advanced NSCLC patients who had received at least 1 cycle of endostatin plus PT-DC between September 2009 and November 2014. Of these patients, 155 received 4 or more cycles of therapy (the extended therapy group), while 45 received less than 4 cycles of therapy (the control group). Clinical tumor responses, progression-free survival (PFS), overall survival (OS), and toxicity profiles were recorded and retrospectively analyzed.In the extended therapy group, 67 patients (43.2%) achieved a best overall response rate of partial response (PR), while in the control group, 13 patients (28.9%) had a best overall response rate of PR. After a median follow-up of 15.9 months, the median PFS and OS were 8.0 and 23.1 months in the extended arm and 5.8 and 14.0 months in the control arm, respectively. There were statistically significant differences in median PFS and OS between these 2 arms. Hematologic and gastrointestinal toxicities occurred more frequently in the extended therapy group, but no statistically significant difference was detected in grade 3 to 4 toxicities overall between these 2 groups.In conclusion, extended treatment using endostatin combined with PT-DC can provide additional survival benefits and satisfactory toxicity profiles in previously untreated patients with NSCLC, which merits further evaluation in a larger prospective study.
Ter Veer E, Haj Mohammad N, van Valkenhoef G, et al.
Second- and third-line systemic therapy in patients with advanced esophagogastric cancer: a systematic review of the literature.
Cancer Metastasis Rev. 2016; 35(3):439-56 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
Second- and third-line systemic therapy in patients with advanced esophagogastric cancer: a systematic review of the literature.
Cancer Metastasis Rev. 2016; 35(3):439-56 [PubMed] Article available free on PMC after 01/11/2017 Related Publications
The optimal second- and third-line chemotherapy and targeted therapy for patients with advanced esophagogastric cancer is still a matter of debate. Therefore, a literature search was carried out in Medline, EMBASE, CENTRAL, and oncology conferences until January 2016 for randomized controlled trials that compared second- or third-line therapy. We included 28 studies with 4810 patients. Second-line, single-agent taxane/irinotecan showed increased survival compared to best supportive care (BSC) (hazard ratio 0.65, 95 % confidence interval 0.53-0.79). Median survival gain ranged from 1.4 to 2.7 months among individual studies. Taxane- and irinotecan-based regimens showed equal survival benefit. Doublet chemotherapy taxane/irinotecan plus platinum and fluoropyrimidine was not different in survival, but showed increased toxicity vs. taxane/irinotecan monotherapy. Compared to BSC, second-line ramucirumab and second- or third-line everolimus and regorafenib showed limited median survival gain ranging from 1.1 to 1.4 months, and progression-free survival gain, ranging from 0.3 to 1.6 months. Third- or later-line apatinib showed increased survival benefit over BSC (HR 0.50, 0.32-0.79). Median survival gain ranged from 1.8 to 2.3 months. Compared to taxane-alone, survival was superior for second-line ramucirumab plus taxane (HR 0.81, 0.68-0.96), and olaparib plus taxane (HR 0.56, 0.35-0.87), with median survival gains of 2.2 and 4.8 months respectively. Targeted agents, either in monotherapy or combined with chemotherapy showed increased toxicity compared to BSC and chemotherapy-alone. This review indicates that, given the survival benefit in a phase III study setting, ramucirumab plus taxane is the preferred second-line treatment. Taxane or irinotecan monotherapy are alternatives, although the absolute survival benefit was limited. In third-line setting, apatinib monotherapy is preferred.
Turkmen E, Erdogan B, Kodaz H, et al.
Post progression survival analysis of metastatic gastric and gastroesophageal junction cancer patients after second-line treatment.
Acta Gastroenterol Belg. 2016 Apr-Jun; 79(2):211-5 [PubMed] Related Publications
Post progression survival analysis of metastatic gastric and gastroesophageal junction cancer patients after second-line treatment.
Acta Gastroenterol Belg. 2016 Apr-Jun; 79(2):211-5 [PubMed] Related Publications
PURPOSE: The aim of this study was to define the factors that -affect response and post-progression survival of metastatic gastric cancer (MGC) and gastroesophageal junction cancer (GEJ) -patients treated with second-line chemotherapy.
METHODS: We retrospectively reviewed the data of 59 patients with MGC or GEJ adenocarcinoma who received second-line treatment.
RESULTS: The median age was 54 years old (26-77). Response to second-line treatment was strongly associated with disease control with first-line treatment (p < 0.01). Median progression-free survival (PFS), overall survival (OS) and post-progression survival (PPS) were 3.2 (95% CI : 2.63-3.80), 6.5 (95% CI : 3.78-9.35) and 2.7 months (95% CI : 1.89-3.68), respectively. PFS (r = 0.55, p < 0.01) and PPS (r = 0.89, p < 0.01) were correlated with OS. Response to second-line treatment was independently related to PFS (HR : 0.12 95%CI : 0.53-0.26, p < 0.001). Having an ECOG 0 performance status (HR : 0.42 ; 95%CI : 0.21-0.86, p = 0.02) and response to second-line therapy (HR : 0.47 ; 95%CI : 0.25-0.85, p = 0.01) were independently associated with OS.
CONCLUSION: PPS and PFS were correlated with OS after second-line treatment of MGC. Response to second-line treatment prolonged OS by increasing PFS, and having an ECOG 0 PS prolonged OS by increasing PPS.
METHODS: We retrospectively reviewed the data of 59 patients with MGC or GEJ adenocarcinoma who received second-line treatment.
RESULTS: The median age was 54 years old (26-77). Response to second-line treatment was strongly associated with disease control with first-line treatment (p < 0.01). Median progression-free survival (PFS), overall survival (OS) and post-progression survival (PPS) were 3.2 (95% CI : 2.63-3.80), 6.5 (95% CI : 3.78-9.35) and 2.7 months (95% CI : 1.89-3.68), respectively. PFS (r = 0.55, p < 0.01) and PPS (r = 0.89, p < 0.01) were correlated with OS. Response to second-line treatment was independently related to PFS (HR : 0.12 95%CI : 0.53-0.26, p < 0.001). Having an ECOG 0 performance status (HR : 0.42 ; 95%CI : 0.21-0.86, p = 0.02) and response to second-line therapy (HR : 0.47 ; 95%CI : 0.25-0.85, p = 0.01) were independently associated with OS.
CONCLUSION: PPS and PFS were correlated with OS after second-line treatment of MGC. Response to second-line treatment prolonged OS by increasing PFS, and having an ECOG 0 PS prolonged OS by increasing PPS.


 Apoptosis
Apoptosis