Found this page useful?
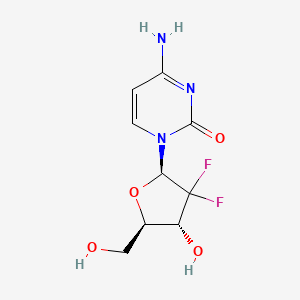
Gemcitabine
 Web Resources: Gemcitabine
Web Resources: Gemcitabine Recent Research Publications
Recent Research PublicationsWeb Resources: Gemcitabine (6 links)
Cancer Research UK
Macmillan Cancer Support
NHS Evidence
 Gemcitabine - Substance Summary
Gemcitabine - Substance Summary
PubChem
Irish Cancer Society
MedlinePlus
Recent Research Publications
Mukai Y, Matsuyama R, Koike I, et al.
Outcome of postoperative radiation therapy for cholangiocarcinoma and analysis of dose-volume histogram of remnant liver.
Medicine (Baltimore). 2019; 98(31):e16673 [PubMed] Related Publications
Outcome of postoperative radiation therapy for cholangiocarcinoma and analysis of dose-volume histogram of remnant liver.
Medicine (Baltimore). 2019; 98(31):e16673 [PubMed] Related Publications
The aim of this study was to analyze dose-volume histogram (DVH) of the remnant liver for postoperative cholangiocarcinoma (CCA) patients, to find toxicity rates, and to confirm efficacy of postoperative radiation therapy (RT).Thirty-two postoperative CCA patients received partial liver resection and postoperative RT with curative intent. The "liver reduction rate" was calculated by contouring liver volume at computed tomography (CT) just before the surgery and at CT for planning the RT. To evaluate late toxicity, the radiation-induced hepatic toxicity (RIHT) was determined by the common terminology criteria for adverse events toxicity grade of bilirubin, aspartate transaminase, alanine transaminase, alkaline phosphatase, and albumin, and was defined from 3 months after RT until liver metastasis was revealed. The radiation-induced liver disease (RILD) was also evaluated.Tumor stages were distributed as follows: I: 1, II: 8, IIIA: 1, IIIB: 6, IIIC: 14, IVA: 2. Median prescribed total dose was 50 Gy. Median follow-up time was 27 months. Two-year overall survival (OS): 72.4%, disease-free survival: 47.7%, local control: 65.3%, and the median survival time was 40 months. The median "liver reduction rate" was 21%. The OS had statistically significant difference in nodal status (P = .032) and "liver reduction rate" >30% (P = .016). In the association between the ≥grade 2 RIHT and DVH, there were significantly differences in V30 and V40 (P = .041, P = .034), respectively. The grade ≥2 RIHT rates differ also significantly by sex (P = .008). Two patients (6.2%) were suspected of RILD.We suggest that RT for remnant liver should be considered the liver V30, V40 to prevent radiation-induced liver dysfunction.
Merdin A, İskender D, Ulu BU, et al.
Pralatrexate induced durable response in a relapsed/refractory peripheral T-cell lymphoma patient with a history of autologous stem cell transplantation: Case report of a patient followed-up over 3 years under pralatrexate treatment.
Medicine (Baltimore). 2019; 98(30):e16482 [PubMed] Related Publications
Pralatrexate induced durable response in a relapsed/refractory peripheral T-cell lymphoma patient with a history of autologous stem cell transplantation: Case report of a patient followed-up over 3 years under pralatrexate treatment.
Medicine (Baltimore). 2019; 98(30):e16482 [PubMed] Related Publications
RATIONALE: Relapsed or refractory peripheral T-cell lymphomas are aggressive diseases. Pralatrexate is an antimetabolite. Hereby, we are reporting a pralatrexate induced durable response in a relapsed/refractory peripheral T-Cell lymphoma patient with a history of autologous stem cell transplantation.
PATIENT CONCERNS: A male patient born in February 1947 was diagnosed with lymphoma based on his cervical lymph node excisional biopsy.
DIAGNOSES: He was diagnosed with PTCL-NOS on February 19, 2013.
INTERVENTIONS: The patient received 6 cycles of CHOP (Cyclophosphamide, doxorubicine, vincristine, methylprednisolone) chemotherapy, which achieved a complete remission. The patient underwent autologous stem cell transplantation in December 2013. After relapse was detected in the third month of the transplantation, the patient was treated with 2 cycles of ViGePP (vinorelbine, gemcitabine, procarbazine, prednisone/ methylprednisolone) chemotherapy. The patient was considered refractory to treatment after the ViGePP chemotherapy, and he was given brentuximab vedotin. Once a full response to treatment was achieved after 2 cycles, the patient received 6 cycles of brentuximab vedotin treatment. After 6 cycles, a skin biopsy was performed and the patient was diagnosed with relapsed/refractory PTCL-NOS. Pralatrexate therapy was then started on February 1, 2016 at a dose of 30 mg/m once weekly for 6 weeks in 7-week cycles.
OUTCOMES: The patient responded to pralatrexate treatment. And he has been under pralatrexate treatment over 3 years.
LESSONS: Pralatrexate should also be kept in mind as a treatment alternative in relapsed or refractory peripheral T-cell lymphoma patients.
PATIENT CONCERNS: A male patient born in February 1947 was diagnosed with lymphoma based on his cervical lymph node excisional biopsy.
DIAGNOSES: He was diagnosed with PTCL-NOS on February 19, 2013.
INTERVENTIONS: The patient received 6 cycles of CHOP (Cyclophosphamide, doxorubicine, vincristine, methylprednisolone) chemotherapy, which achieved a complete remission. The patient underwent autologous stem cell transplantation in December 2013. After relapse was detected in the third month of the transplantation, the patient was treated with 2 cycles of ViGePP (vinorelbine, gemcitabine, procarbazine, prednisone/ methylprednisolone) chemotherapy. The patient was considered refractory to treatment after the ViGePP chemotherapy, and he was given brentuximab vedotin. Once a full response to treatment was achieved after 2 cycles, the patient received 6 cycles of brentuximab vedotin treatment. After 6 cycles, a skin biopsy was performed and the patient was diagnosed with relapsed/refractory PTCL-NOS. Pralatrexate therapy was then started on February 1, 2016 at a dose of 30 mg/m once weekly for 6 weeks in 7-week cycles.
OUTCOMES: The patient responded to pralatrexate treatment. And he has been under pralatrexate treatment over 3 years.
LESSONS: Pralatrexate should also be kept in mind as a treatment alternative in relapsed or refractory peripheral T-cell lymphoma patients.
Balsano R, Tommasi C, Garajova I
State of the Art for Metastatic Pancreatic Cancer Treatment: Where Are We Now?
Anticancer Res. 2019; 39(7):3405-3412 [PubMed] Related Publications
State of the Art for Metastatic Pancreatic Cancer Treatment: Where Are We Now?
Anticancer Res. 2019; 39(7):3405-3412 [PubMed] Related Publications
The prognosis of metastatic pancreatic cancer remains poor despite the recent progress on modern chemotherapeutic regimens, such as FOLFIRINOX, gemcitabine and nab-paclitaxel. A better understanding of the altered signalling pathways and the importance of stroma and the immune environment in pancreatic cancer have led to the development of new clinical trials with promising results. In the present review, a general outline of current first- and second-line therapies is provided. Further, new therapeutic possibilities are reviewed, in particular EGFR and VEGF inhibitors, immunotherapy and PARP inhibitors.
Peters GJ
From 'Targeted Therapy' to Targeted Therapy.
Anticancer Res. 2019; 39(7):3341-3345 [PubMed] Related Publications
From 'Targeted Therapy' to Targeted Therapy.
Anticancer Res. 2019; 39(7):3341-3345 [PubMed] Related Publications
In early 2000, the term 'targeted therapy' became popular and was used to indicate all types of tyrosine kinase inhibitors (TKI). However, the term targeted therapy had been used much earlier. Targeting tumor metabolism was already considered as targeted therapy, with methotrexate and 5-fluorouracil as the most successful examples. Hormone therapy is another successful type of targeted therapy. Imatinib was the first TKI for the fusion protein BCR-ABL and represented a breakthrough in the treatment of chronic myeloid leukemia. Many other TKIs have been introduced into the clinic, but most were less specific and had multiple targets, and therefore, by definition, not targeted. However, with the introduction of TKIs developed specifically against mutations in the active site of a TK, more truly targeted TKI have been approved, such as new anaplastic lymphoma kinase - echinoderm microtubule-associated protein-like 4 (ALK-EML4) inhibitors and the epidermal growth factor-T790M-targeted osimertinib. This article summarizes the content of the Burger-Kelland award lecture given by the Author in February 2019 during the 40th EORTC-PAMM Group meeting in Verona, Italy and reviews the development of various targeted agents.
Sugarman R, Patel R, Sharma S, et al.
Pharmacokinetics and pharmacodynamics of new drugs for pancreatic cancer.
Expert Opin Drug Metab Toxicol. 2019; 15(7):541-552 [PubMed] Related Publications
Pharmacokinetics and pharmacodynamics of new drugs for pancreatic cancer.
Expert Opin Drug Metab Toxicol. 2019; 15(7):541-552 [PubMed] Related Publications
Shima H, Tsurita G, Wada S, et al.
Randomized phase II trial of survivin 2B peptide vaccination for patients with HLA-A24-positive pancreatic adenocarcinoma.
Cancer Sci. 2019; 110(8):2378-2385 [PubMed] Free Access to Full Article Related Publications
Randomized phase II trial of survivin 2B peptide vaccination for patients with HLA-A24-positive pancreatic adenocarcinoma.
Cancer Sci. 2019; 110(8):2378-2385 [PubMed] Free Access to Full Article Related Publications
The prognosis of advanced pancreatic adenocarcinoma is still extremely poor. This study sought to determine the efficacy of, and immunological response to, peptide vaccination therapy in patients with this disease. In this multicenter randomized phase II study, patients with advanced pancreatic adenocarcinoma after gemcitabine and/or tegafur/gimeracil/oteracil were randomly assigned to 3 groups that each received a 2-step treatment course. In Step 1, the groups received treatments of: (i) survivin 2B peptide (SVN-2B) plus interferon-β (IFNβ); (ii) SVN-2B only; or (iii) placebo until the patients show progression. In Step 2, all patients who consented to participate received 4 treatments with SVN-2B plus IFNβ. The primary endpoint was progression-free survival (PFS) after initiation of Step 1 treatment. Secondary endpoints included immunological effects assessed by analysis of PBMCs after Step 1. Eighty-three patients were randomly assigned to receive SVN-2B plus IFNβ (n = 30), SVN-2B (n = 34), or placebo (n = 19). No significant improvement in PFS was observed. Survivin 2B-specific CTLs were found to be increased in the SVN-2B plus IFNβ group by tetramer assay. Among patients who participated in Step 2, those who had received SVN-2B plus IFNβ in Step 1 showed better overall survival compared with those who had received placebo in Step 1. Patients vaccinated with SVN-2B plus IFNβ did not have improved PFS, but showed significant immunological reaction after vaccination. Subgroup analysis suggested that a longer SVN-2B plus IFNβ vaccination protocol might confer survival benefit. (Clinical trial registration number: UMIN 000012146).
Panaro F, Kellil T, Vendrell J, et al.
Microvascular invasion is a major prognostic factor after pancreatico-duodenectomy for adenocarcinoma.
J Surg Oncol. 2019; 120(3):483-493 [PubMed] Related Publications
Microvascular invasion is a major prognostic factor after pancreatico-duodenectomy for adenocarcinoma.
J Surg Oncol. 2019; 120(3):483-493 [PubMed] Related Publications
BACKGROUND: Microvascular invasion (MVI) has been proved to be poor prognostic factor in many cancers. To date, only one study published highlights the relationship between this factor and the natural history of pancreatic cancer. The aim of this study was to assess the impact of MVI, on disease-free survival (DFS) and overall survival (OS), after pancreatico-duodenectomy (PD) for pancreatic head adenocarcinoma. Secondarily, we aim to demonstrate that MVI is the most important factor to predict OS after surgery compared with resection margin (RM) and lymph node (LN) status.
MATERIALS AND METHODS: Between January 2015 and December 2017, 158 PD were performed in two hepato-bilio-pancreatic (HBP) centers. Among these, only 79 patients fulfilled the inclusion criteria of the study. Clinical-pathological data and outcomes were retrospectively analyzed from a prospectively maintained database.
RESULTS: Of the 79 patients in the cohort, MVI was identified in 35 (44.3%). In univariate analysis, MVI (P = .012 and P < .0001), RM (P = .023 and P = .021), and LN status (P < .0001 and P = .0001) were significantly associated with DFS and OS. A less than 1 mm margin clearance did not influence relapse (P = .72) or long-term survival (P = .48). LN ratio > 0.226 had a negative impact on OS (P = .044). In multivariate analysis, MVI and RM persisted as independent prognostic factors of DFS (P = .0075 and P = .0098, respectively) and OS (P < .0001 and P = .0194, respectively). Using the likelihood ratio test, MVI was identified as the best fit to predict OS after PD for ductal adenocarcinomas compared with the margin status model (R0 vs R1) (P = .0014).
CONCLUSION: The MVI represents another major prognostic factor determining long-term outcomes.
MATERIALS AND METHODS: Between January 2015 and December 2017, 158 PD were performed in two hepato-bilio-pancreatic (HBP) centers. Among these, only 79 patients fulfilled the inclusion criteria of the study. Clinical-pathological data and outcomes were retrospectively analyzed from a prospectively maintained database.
RESULTS: Of the 79 patients in the cohort, MVI was identified in 35 (44.3%). In univariate analysis, MVI (P = .012 and P < .0001), RM (P = .023 and P = .021), and LN status (P < .0001 and P = .0001) were significantly associated with DFS and OS. A less than 1 mm margin clearance did not influence relapse (P = .72) or long-term survival (P = .48). LN ratio > 0.226 had a negative impact on OS (P = .044). In multivariate analysis, MVI and RM persisted as independent prognostic factors of DFS (P = .0075 and P = .0098, respectively) and OS (P < .0001 and P = .0194, respectively). Using the likelihood ratio test, MVI was identified as the best fit to predict OS after PD for ductal adenocarcinomas compared with the margin status model (R0 vs R1) (P = .0014).
CONCLUSION: The MVI represents another major prognostic factor determining long-term outcomes.
Bisello S, Buwenge M, Palloni A, et al.
Radiotherapy or Chemoradiation in Unresectable Biliary Cancer: A Retrospective Study.
Anticancer Res. 2019; 39(6):3095-3100 [PubMed] Related Publications
Radiotherapy or Chemoradiation in Unresectable Biliary Cancer: A Retrospective Study.
Anticancer Res. 2019; 39(6):3095-3100 [PubMed] Related Publications
BACKGROUND/AIM: To retrospectively evaluate the outcome of patients with unresectable biliary cholangiocarcinoma (CC) treated with radiotherapy (RT) plus/minus chemotherapy (CHT).
MATERIALS AND METHODS: Data of patients with intrahepatic CC (ICC), Klatskin's tumor (KT), distal extrahepatic CC (ECC), and gallbladder cancer (GBC) diagnosed from 1991 to 2017 were retrospectively analyzed. The treatment was mainly based on RT plus concurrent CHT +/- brachytherapy (BRT) boost. The Kaplan-Meier method was used to calculate survival curves that were compared using the log-rank test.
RESULTS: Seventy-six patients were included in this analysis (males: 59%; females: 41%; median age: 66.5 years). A minority of patients (7.9%) were treated for disease recurrence after surgery. According to TNM, 78.5% of patients had T stage >3 and 77.6% of patients were treated with concurrent CHT-RT while 22.3% received RT followed by sequential CHT. Median RT dose was 50 Gy (range: 16-75 Gy) delivered with conventional fractionation. CHT was based on Gemcitabine or 5-fluorouracil. BRT was prescribed to 51.3% of patient with a median dose of 14 Gy. Reported Grade ≥3 acute GI and hematological toxicity were 13.2% and 8.1%, respectively. No other severe acute toxicities were reported. One- and 2-year overall survival (OS) were 58.1% and 25.8%, respectively (median: 13.5 months), while 1- and 2-year progression-free survival (PFS) were 43.4% and 9.4%, respectively. None of the following variables had a significant impact on OS and PFS: BRT boost, tumor site, concurrent CHT, and the drugs used in concurrent CHT. In contrast, patients receiving RT with 2D technique showed a PFS significantly higher compared to patients treated with the 3D technique (median: 15.5 vs. 8.5 months; p=0.02).
CONCLUSION: Combined modality treatment (RT+CHT±BRT) in unresectable biliary cancer was associated with acceptable toxicity and OS comparable to the actual standard treatment (CHT). The significantly improved PFS in patients undergoing 2D-RT raises doubts regarding the adequacy of target delineation in these neoplasms.
MATERIALS AND METHODS: Data of patients with intrahepatic CC (ICC), Klatskin's tumor (KT), distal extrahepatic CC (ECC), and gallbladder cancer (GBC) diagnosed from 1991 to 2017 were retrospectively analyzed. The treatment was mainly based on RT plus concurrent CHT +/- brachytherapy (BRT) boost. The Kaplan-Meier method was used to calculate survival curves that were compared using the log-rank test.
RESULTS: Seventy-six patients were included in this analysis (males: 59%; females: 41%; median age: 66.5 years). A minority of patients (7.9%) were treated for disease recurrence after surgery. According to TNM, 78.5% of patients had T stage >3 and 77.6% of patients were treated with concurrent CHT-RT while 22.3% received RT followed by sequential CHT. Median RT dose was 50 Gy (range: 16-75 Gy) delivered with conventional fractionation. CHT was based on Gemcitabine or 5-fluorouracil. BRT was prescribed to 51.3% of patient with a median dose of 14 Gy. Reported Grade ≥3 acute GI and hematological toxicity were 13.2% and 8.1%, respectively. No other severe acute toxicities were reported. One- and 2-year overall survival (OS) were 58.1% and 25.8%, respectively (median: 13.5 months), while 1- and 2-year progression-free survival (PFS) were 43.4% and 9.4%, respectively. None of the following variables had a significant impact on OS and PFS: BRT boost, tumor site, concurrent CHT, and the drugs used in concurrent CHT. In contrast, patients receiving RT with 2D technique showed a PFS significantly higher compared to patients treated with the 3D technique (median: 15.5 vs. 8.5 months; p=0.02).
CONCLUSION: Combined modality treatment (RT+CHT±BRT) in unresectable biliary cancer was associated with acceptable toxicity and OS comparable to the actual standard treatment (CHT). The significantly improved PFS in patients undergoing 2D-RT raises doubts regarding the adequacy of target delineation in these neoplasms.
Seufferlein T, Hammel P, Delpero JR, et al.
Optimizing the management of locally advanced pancreatic cancer with a focus on induction chemotherapy: Expert opinion based on a review of current evidence.
Cancer Treat Rev. 2019; 77:1-10 [PubMed] Related Publications
Optimizing the management of locally advanced pancreatic cancer with a focus on induction chemotherapy: Expert opinion based on a review of current evidence.
Cancer Treat Rev. 2019; 77:1-10 [PubMed] Related Publications
Surgical resection of pancreatic cancer offers a chance of cure, but currently only 15-20% of patients are diagnosed with resectable disease, while 30-40% are diagnosed with non-metastatic, unresectable locally advanced pancreatic cancer (LAPC). Treatment for LAPC usually involves systemic chemotherapy, with the aim of controlling disease progression, reducing symptoms and maintaining quality of life. In a small proportion of patients with LAPC, primary chemotherapy may successfully convert unresectable tumours to resectable tumours. In this setting, primary chemotherapy is termed 'induction therapy' rather than 'neoadjuvant'. There is currently a lack of data from randomized studies to thoroughly evaluate the benefits of induction chemotherapy in LAPC, but Phase II and retrospective data have shown improved survival and high R0 resection rates. New chemotherapy regimens such as nab-paclitaxel + gemcitabine and FOLFIRINOX have demonstrated improvement in overall survival for metastatic disease and shown promise as neoadjuvant treatment in patients with resectable and borderline resectable disease. Prospective trials are underway to evaluate these regimens further as induction therapy in LAPC and preliminary data indicate a beneficial effect of FOLFIRINOX in this setting. Further research into optimal induction schedules is needed, as well as guidance on the patients who are most suitable for induction therapy. In this expert opinion article, a panel of surgeons, medical oncologists and gastrointestinal oncologists review the available evidence on management strategies for LAPC and provide their recommendations for patient care, with a particular focus on the use of induction chemotherapy.
Jin HB, Lu L, Xie L, et al.
Concentration changes in gemcitabine and its metabolites after hyperthermia in pancreatic cancer cells assessed using RP-HPLC.
Cell Mol Biol Lett. 2019; 24:30 [PubMed] Free Access to Full Article Related Publications
Concentration changes in gemcitabine and its metabolites after hyperthermia in pancreatic cancer cells assessed using RP-HPLC.
Cell Mol Biol Lett. 2019; 24:30 [PubMed] Free Access to Full Article Related Publications
Background: Gemcitabine (2',2'-difluoro-2'-deoxycytidine;dFdC) is a first-line chemotherapy drug for pancreatic cancer. Recently, a synergistic anti-tumor treatment of dFdC and hyperthermia has achieved good clinical results, but there are few reports on the molecular mechanism influenced by hyperthermia. This study is an initial exploration of the effects of hyperthermia on changes in the concentration of dFdC and its metabolites in pancreatic cancer cells. The aim is to provide a theoretical basis for clinical detection and pharmacokinetic research.
Methods: PANC-1 cells at logarithmic growth phase were used as the experimental object. The MTT assay was performed to determine the half maximal inhibitory concentration (IC
Results: We found that 41 °C and 43 °Chyperthermia gave rise to a decrease in dFdC and dFdU content. At 41 °C, the levels respectively fell to 9.28 and 30.93% of the baseline, and at 43 °C, to 24.76 and 57.80%, respectively. The dFdCTP content increased by 21.82% at 41 °C and 42.42% at 43 °C.
Conclusion: The two heat treatments could alter the mechanism of dFdC metabolism in PANC-1 cells. The effect of 43 °C hyperthermia is more significant. Our observations may be instrumental to explaining the higher anti-tumor efficacy of this combination therapy.
Methods: PANC-1 cells at logarithmic growth phase were used as the experimental object. The MTT assay was performed to determine the half maximal inhibitory concentration (IC
Results: We found that 41 °C and 43 °Chyperthermia gave rise to a decrease in dFdC and dFdU content. At 41 °C, the levels respectively fell to 9.28 and 30.93% of the baseline, and at 43 °C, to 24.76 and 57.80%, respectively. The dFdCTP content increased by 21.82% at 41 °C and 42.42% at 43 °C.
Conclusion: The two heat treatments could alter the mechanism of dFdC metabolism in PANC-1 cells. The effect of 43 °C hyperthermia is more significant. Our observations may be instrumental to explaining the higher anti-tumor efficacy of this combination therapy.
Ma Y, Mou Q, Zhu L, et al.
Polygemcitabine nanogels with accelerated drug activation for cancer therapy.
Chem Commun (Camb). 2019; 55(46):6603-6606 [PubMed] Related Publications
Polygemcitabine nanogels with accelerated drug activation for cancer therapy.
Chem Commun (Camb). 2019; 55(46):6603-6606 [PubMed] Related Publications
To overcome the slow activation of gemcitabine, we synthesized a DNA-like polygemcitabine (Ge10) strand through solid-phase synthesis, which not only undergoes rapid intracellular degradation to generate active gemcitabine derivatives, but can also self-assemble into nanogels through molecular recognition, rendering them as promising self-delivered nanodrugs for cancer therapy.
Soumarová R, Gürlich R, Hajer J, et al.
The current role of radiotherapy and systemic therapy in the multidisciplinary treatment of cholangiocarcinoma.
Cas Lek Cesk. 2019; 158(2):78-82 [PubMed] Related Publications
The current role of radiotherapy and systemic therapy in the multidisciplinary treatment of cholangiocarcinoma.
Cas Lek Cesk. 2019; 158(2):78-82 [PubMed] Related Publications
Cholangiocarcinoma is a cancer with very poor prognosis. The only potentially curative approach is surgical resection of tumor. However, the rate of local and distant recurrence after radical surgery is still high. Benefit of adjuvant therapy is not clearly defined, nevertheless patients at high risk of recurrence are indicated to chemotherapy or chemoradiotherapy. Locally advanced, unresectable disease can also be treated with chemotherapy alone, or with her combination with radiotherapy. Required radiation doses are relatively high, therefore it is necessary to use highly conformal radiation therapy. Treatment of metastatic disease is currently based on systemic therapy, combination of gemcitabine and cisplatin as standard of care. Benefit of targeted molecular therapy is not clear at present, but ongoing research in genetic profiling of tumor may help to improve current clinical practice. Patients with cholangiocarcinoma have to be discussed during multidisciplinary team meetings.
El Hassouni B, Li Petri G, Liu DSK, et al.
Pharmacogenetics of treatments for pancreatic cancer.
Expert Opin Drug Metab Toxicol. 2019; 15(6):437-447 [PubMed] Related Publications
Pharmacogenetics of treatments for pancreatic cancer.
Expert Opin Drug Metab Toxicol. 2019; 15(6):437-447 [PubMed] Related Publications
Drenberg CD, Shelat A, Dang J, et al.
A high-throughput screen indicates gemcitabine and JAK inhibitors may be useful for treating pediatric AML.
Nat Commun. 2019; 10(1):2189 [PubMed] Free Access to Full Article Related Publications
A high-throughput screen indicates gemcitabine and JAK inhibitors may be useful for treating pediatric AML.
Nat Commun. 2019; 10(1):2189 [PubMed] Free Access to Full Article Related Publications
Improvement in survival has been achieved for children and adolescents with AML but is largely attributed to enhanced supportive care as opposed to the development of better treatment regimens. High risk subtypes continue to have poor outcomes with event free survival rates <40% despite the use of high intensity chemotherapy in combination with hematopoietic stem cell transplant. Here we combine high-throughput screening, intracellular accumulation assays, and in vivo efficacy studies to identify therapeutic strategies for pediatric AML. We report therapeutics not currently used to treat AML, gemcitabine and cabazitaxel, have broad anti-leukemic activity across subtypes and are more effective relative to the AML standard of care, cytarabine, both in vitro and in vivo. JAK inhibitors are selective for acute megakaryoblastic leukemia and significantly prolong survival in multiple preclinical models. Our approach provides advances in the development of treatment strategies for pediatric AML.
Morita Y, Sakaguchi T, Kitajima R, et al.
Body weight loss after surgery affects the continuity of adjuvant chemotherapy for pancreatic cancer.
BMC Cancer. 2019; 19(1):416 [PubMed] Free Access to Full Article Related Publications
Body weight loss after surgery affects the continuity of adjuvant chemotherapy for pancreatic cancer.
BMC Cancer. 2019; 19(1):416 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Postoperative chemotherapy is beneficial for many pancreatic cancer patients. However, some patients require dose reduction or the discontinuation of adjuvant chemotherapy because of adverse treatment-related effects. In this study, we aimed to evaluate two main outcomes. First, we evaluated the clinicopathological factors affecting patient disease-free survival (DFS) and overall survival (OS) following upfront surgery. Second, we evaluated the factors that influence the continuity of adjuvant chemotherapy.
METHODS: Fifty-four patients with resected pancreatic cancer were enrolled. First, we evaluated the clinicopathological factors affecting postoperative survival using the Kaplan-Meier method and Cox regression method. Next, factors affecting the continuity of adjuvant chemotherapy were analyzed using multiple logistic regression analysis.
RESULTS: Univariate and multivariate analyses revealed that positive LN metastasis (HR (95% CI) 6.329 (2.381-16.95); p < 0.001) and relative dose intensity (RDI) < 80% for adjuvant chemotherapy (HR (95% CI) 5.154 (1.761-15.15); p = 0.003) were independent predictive factors for DFS. Regarding OS, extended dissection of the nerve plexus around the superior mesenteric artery (SMA) (HR (95% CI) 4.504 (1.721-11.76); p = 0.002), positive microscopic surgical margin (HR (95% CI) 5.565 (1.724-17.96); p = 0.004), and adjuvant chemotherapy of RDI < 80% (HR (95% CI) 3.534 (1.135-2.667); p = 0.029) were also independent predictive factors. Moreover, the level of RDI significantly correlated with DFS and OS. Multiple logistic regression analysis revealed that low RDI was significantly associated with postoperative body weight loss (BWL) ≥ 10%.
CONCLUSIONS: The following factors were significantly associated with poor survival: extended dissection of the nerve plexus around the SMA, lymph node metastasis, residual tumor, and RDI of the adjuvant chemotherapy. Patient's prognosis with adjuvant chemotherapy of RDI < 80% was worse. BWL ≥10% was the most important factor affecting the continuity of adjuvant chemotherapy. Perioperative nutritional intervention is necessary for patients who receive adjuvant chemotherapy for advanced pancreatic cancer.
METHODS: Fifty-four patients with resected pancreatic cancer were enrolled. First, we evaluated the clinicopathological factors affecting postoperative survival using the Kaplan-Meier method and Cox regression method. Next, factors affecting the continuity of adjuvant chemotherapy were analyzed using multiple logistic regression analysis.
RESULTS: Univariate and multivariate analyses revealed that positive LN metastasis (HR (95% CI) 6.329 (2.381-16.95); p < 0.001) and relative dose intensity (RDI) < 80% for adjuvant chemotherapy (HR (95% CI) 5.154 (1.761-15.15); p = 0.003) were independent predictive factors for DFS. Regarding OS, extended dissection of the nerve plexus around the superior mesenteric artery (SMA) (HR (95% CI) 4.504 (1.721-11.76); p = 0.002), positive microscopic surgical margin (HR (95% CI) 5.565 (1.724-17.96); p = 0.004), and adjuvant chemotherapy of RDI < 80% (HR (95% CI) 3.534 (1.135-2.667); p = 0.029) were also independent predictive factors. Moreover, the level of RDI significantly correlated with DFS and OS. Multiple logistic regression analysis revealed that low RDI was significantly associated with postoperative body weight loss (BWL) ≥ 10%.
CONCLUSIONS: The following factors were significantly associated with poor survival: extended dissection of the nerve plexus around the SMA, lymph node metastasis, residual tumor, and RDI of the adjuvant chemotherapy. Patient's prognosis with adjuvant chemotherapy of RDI < 80% was worse. BWL ≥10% was the most important factor affecting the continuity of adjuvant chemotherapy. Perioperative nutritional intervention is necessary for patients who receive adjuvant chemotherapy for advanced pancreatic cancer.
Liang W, Guo M, Pan Z, et al.
Association between certain non-small cell lung cancer driver mutations and predictive markers for chemotherapy or programmed death-ligand 1 inhibition.
Cancer Sci. 2019; 110(6):2014-2021 [PubMed] Free Access to Full Article Related Publications
Association between certain non-small cell lung cancer driver mutations and predictive markers for chemotherapy or programmed death-ligand 1 inhibition.
Cancer Sci. 2019; 110(6):2014-2021 [PubMed] Free Access to Full Article Related Publications
This study aimed to analyze the association between driver mutations and predictive markers for some anti-tumor agents in non-small cell lung cancer (NSCLC). A cohort of 785 Chinese patients with NSCLC who underwent resection from March 2016 to November 2017 in the First Affiliated Hospital of Guangzhou Medical University was investigated. The specimens were subjected to hybridization capture and sequence of 8 important NSCLC-related driver genes. In addition, the slides were tested for PD-L1, excision repair cross-complementation group 1 (ERCC1), ribonucleotide reductase subunit M1 (RRM1), thymidylate synthase (TS) and β-tubulin III by immunohistochemical staining. A total of 498 (63.4%) patients had at least 1 driver gene alteration. Wild-type, EGFR rare mutation (mut), ALK fusion (fus), RAS mut, RET fus and MET mut had relatively higher proportions of lower ERCC1 expression. EGFR 19del, EGFR L858R, EGFR rare mut, ALK fus, HER2 mut, ROS1 fus and MET mut were more likely to have TS low expression. Wild-type, EGFR L858R, EGFR rare mut and BRAF mut were associated with lower β-tubulin III expression. In addition, wild-type, RAS mut, ROS1 fus, BRAF and MET mut had higher proportion of PD-L1 high expression. As a pilot validation, 21 wild-type patients with advanced NSCLC showed better depth of response and response rate to taxanes compared with pemetrexed/gemcitabine (31.2%/60.0% vs 26.6%/45.5%). Our study may aid in selecting the optimal salvage regimen after targeted therapy failure, or the chemo-regimen where targeted therapy has not been a routine option. Further validation is warranted.
Wang W, Hu Z, Huang Y, et al.
Pretreatment with Gemcitabine/5-Fluorouracil Enhances the Cytotoxicity of Trastuzumab to HER2-Negative Human Gallbladder Cancer Cells In Vitro and In Vivo.
Biomed Res Int. 2019; 2019:9205851 [PubMed] Free Access to Full Article Related Publications
Pretreatment with Gemcitabine/5-Fluorouracil Enhances the Cytotoxicity of Trastuzumab to HER2-Negative Human Gallbladder Cancer Cells In Vitro and In Vivo.
Biomed Res Int. 2019; 2019:9205851 [PubMed] Free Access to Full Article Related Publications
The effects of standard clinical therapies including surgery and chemotherapy are poor in advanced gallbladder cancer (GBC). There are a few reported cases of human epidermal growth factor receptor 2 (HER2)-positive GBC that responded well to trastuzumab. But trastuzumab has not yet been used to treat HER2-negative GBC. In this study, we investigated the cytotoxic effects of different combined therapies with trastuzumab and gemcitabine and/or 5-fluorouracil on HER2-negative GBC cell lines in vitro and in vivo. Trastuzumab alone showed almost no cytotoxicity to GBC cells with originally low HER2 gene amplification. Sequential therapy with chemotherapy followed by trastuzumab showed superiority over reverse sequential chemotherapy (
Song W, Jeong JY, Jeon HG, et al.
Impact of adjuvant chemotherapy on oncologic outcomes following radical nephroureterectomy for patients with pT3NanyM0 upper tract urothelial carcinoma: A retrospective cohort study.
Int J Surg. 2019; 66:12-17 [PubMed] Related Publications
Impact of adjuvant chemotherapy on oncologic outcomes following radical nephroureterectomy for patients with pT3NanyM0 upper tract urothelial carcinoma: A retrospective cohort study.
Int J Surg. 2019; 66:12-17 [PubMed] Related Publications
OBJECTIVE: We investigated the impact of cisplatin-based adjuvant chemotherapy (AC) on oncologic outcomes including recurrence-free survival (RFS), cancer-specific survival (CSS) and overall survival (OS) after radical nephroureterectomy (RNU) for patients with pT3NanyM0 upper tract urothelial carcinoma (UTUC).
METHODS: We retrospectively reviewed 293 patients who underwent RNU for UTUC between 1995 and 2017. Clinicopathologic characteristics of patients were examined and compared according to the use of AC. Kaplan-Meier survival analysis was used to illustrate RFS, CSS and OS. Cox proportional hazard models were applied to identify factors predicting oncologic outcomes.
RESULTS: Among the 293 total patients, 127 (43.3%) patients received AC. During a mean follow-up of 59.7 months, recurrence and/or distant metastasis were identified in 124 (42.3%) patients, and 106 (36.2%) patients died overall, of which 93 (31.7%) died from UTUC. The 5-year RFS, CSS and OS rates of overall patients were 51.3%, 68.0% and 64.7%, respectively. In multivariate analysis, AC was inversely associated with tumor recurrence (HR = 0.74, P = 0.028) but not significantly associated with death from UTUC (P = 0.237) and death from all-cause (P = 0.433). The 5-year RFS of patients who had received AC was 58.0%, while 44.0% for patients who had only been observed after RNU.
CONCLUSION: AC improved RFS, but did not have a significant effect on CSS and OS in patients with pT3NanyM0 UTUCs following RNU. Further efforts are needed to identify reliable criteria in the clinic for patients that would benefit from AC.
METHODS: We retrospectively reviewed 293 patients who underwent RNU for UTUC between 1995 and 2017. Clinicopathologic characteristics of patients were examined and compared according to the use of AC. Kaplan-Meier survival analysis was used to illustrate RFS, CSS and OS. Cox proportional hazard models were applied to identify factors predicting oncologic outcomes.
RESULTS: Among the 293 total patients, 127 (43.3%) patients received AC. During a mean follow-up of 59.7 months, recurrence and/or distant metastasis were identified in 124 (42.3%) patients, and 106 (36.2%) patients died overall, of which 93 (31.7%) died from UTUC. The 5-year RFS, CSS and OS rates of overall patients were 51.3%, 68.0% and 64.7%, respectively. In multivariate analysis, AC was inversely associated with tumor recurrence (HR = 0.74, P = 0.028) but not significantly associated with death from UTUC (P = 0.237) and death from all-cause (P = 0.433). The 5-year RFS of patients who had received AC was 58.0%, while 44.0% for patients who had only been observed after RNU.
CONCLUSION: AC improved RFS, but did not have a significant effect on CSS and OS in patients with pT3NanyM0 UTUCs following RNU. Further efforts are needed to identify reliable criteria in the clinic for patients that would benefit from AC.
Fan X, Wang W, Li C, et al.
An osteoclast-like giant cell tumor embedded in the mural nodule of a pancreatic mucinous cystic neoplasm: A case report and literature review.
Medicine (Baltimore). 2019; 98(16):e15246 [PubMed] Free Access to Full Article Related Publications
An osteoclast-like giant cell tumor embedded in the mural nodule of a pancreatic mucinous cystic neoplasm: A case report and literature review.
Medicine (Baltimore). 2019; 98(16):e15246 [PubMed] Free Access to Full Article Related Publications
RATIONALE: Mucinous cystic neoplasms (MCNs) are relatively rare lesions, accounting for 2%-5% of all exocrine pancreatic neoplasms. MCNs mainly occur in women (female:male ratio = 20:1), with a peak incidence in the 5th decade of life. Osteoclast-like giant cell tumors (OGCTs) are rare and relatively aggressive neoplasms, comprising <1% of all pancreatic carcinomas. Herein, we present a rare "combination tumor" case and discuss the impact of mural nodules in pancreatic MCNs considering malignant transformation.
PATIENT CONCERNS: A 54-year-old Mongolian man, without vomiting, nausea or jaundice, presented with abdominal distention since 3 months. He had a 7-year history of diabetes. Physical examinations indicated slight middle abdominal tenderness without rebound tenderness or rigidity. Laboratory results revealed that the level of carcinoembryonic antigen (CEA) was 1.16 ng/ml (normal: <5 ng/ml); CA-199: 30.02 U/ml (normal: <27 U/ml); hemoglobin: 143 g/L; fasting glucose: 7.71 mmol/L; and albumin: 43 g/L. Abdominal enhanced computed tomography revealed a 7 × 6 cm solid neoplasm in the pancreatic body with partial enhancement and heterogeneity. Endoscopic ultrasound revealed a solid-cystic space-occupying lesion in the pancreatic body.
DIAGNOSIS: The preoperative preliminary diagnosis was pancreatic solid-cystic tumor, possibly a solid pseudopapillary tumor. Postoperative pathological findings revealed a pancreatic borderline MCN with an OGCT embedded in a mural nodule of the capsule. Immunohistochemical results indicated a simultaneous dual origin from the epithelium and stroma.
INTERVENTIONS: The patient underwent open distal pancreatectomy and splenectomy. Postoperative blood glucose levels were closely monitored and regulated. We intravenously administered single-agent gemcitabine (1400 mg on day 1) as the first-time chemotherapy, 1 month after surgery. After the first chemotherapy, the patient refused to receive further treatment owing to personal reasons.
OUTCOMES: The patient showed uneventful recovery and was discharged 13 days after the initial surgery. Follow-up was performed 1, 3 and 6 months after surgery. At 6 months, abdominal computed tomography scan showed no signs of recurrence, regional lymphadenopathy, or other abnormalities. And laboratory tests showed a platelet count of 301 × 10/L, postprandial blood glucose of 12.9 mmol/L and CA-199 level of 20 U/ml. The patient had no obvious discomfort.
LESSONS: Although pancreatic MCNs are widely accepted as borderline tumors, malignant transformations may occur due to various risk factors (cyst size, mural nodules, septations, and tumor location). The combination tumor in this case was more likely to increase the possibility of malignant biological behavior, thereby worsening overall prognosis. Therefore, long-term follow-up must be maintained with strict monitoring.
PATIENT CONCERNS: A 54-year-old Mongolian man, without vomiting, nausea or jaundice, presented with abdominal distention since 3 months. He had a 7-year history of diabetes. Physical examinations indicated slight middle abdominal tenderness without rebound tenderness or rigidity. Laboratory results revealed that the level of carcinoembryonic antigen (CEA) was 1.16 ng/ml (normal: <5 ng/ml); CA-199: 30.02 U/ml (normal: <27 U/ml); hemoglobin: 143 g/L; fasting glucose: 7.71 mmol/L; and albumin: 43 g/L. Abdominal enhanced computed tomography revealed a 7 × 6 cm solid neoplasm in the pancreatic body with partial enhancement and heterogeneity. Endoscopic ultrasound revealed a solid-cystic space-occupying lesion in the pancreatic body.
DIAGNOSIS: The preoperative preliminary diagnosis was pancreatic solid-cystic tumor, possibly a solid pseudopapillary tumor. Postoperative pathological findings revealed a pancreatic borderline MCN with an OGCT embedded in a mural nodule of the capsule. Immunohistochemical results indicated a simultaneous dual origin from the epithelium and stroma.
INTERVENTIONS: The patient underwent open distal pancreatectomy and splenectomy. Postoperative blood glucose levels were closely monitored and regulated. We intravenously administered single-agent gemcitabine (1400 mg on day 1) as the first-time chemotherapy, 1 month after surgery. After the first chemotherapy, the patient refused to receive further treatment owing to personal reasons.
OUTCOMES: The patient showed uneventful recovery and was discharged 13 days after the initial surgery. Follow-up was performed 1, 3 and 6 months after surgery. At 6 months, abdominal computed tomography scan showed no signs of recurrence, regional lymphadenopathy, or other abnormalities. And laboratory tests showed a platelet count of 301 × 10/L, postprandial blood glucose of 12.9 mmol/L and CA-199 level of 20 U/ml. The patient had no obvious discomfort.
LESSONS: Although pancreatic MCNs are widely accepted as borderline tumors, malignant transformations may occur due to various risk factors (cyst size, mural nodules, septations, and tumor location). The combination tumor in this case was more likely to increase the possibility of malignant biological behavior, thereby worsening overall prognosis. Therefore, long-term follow-up must be maintained with strict monitoring.
Imafuji H, Matsuo Y, Ueda G, et al.
Acquisition of gemcitabine resistance enhances angiogenesis via upregulation of IL‑8 production in pancreatic cancer.
Oncol Rep. 2019; 41(6):3508-3516 [PubMed] Related Publications
Acquisition of gemcitabine resistance enhances angiogenesis via upregulation of IL‑8 production in pancreatic cancer.
Oncol Rep. 2019; 41(6):3508-3516 [PubMed] Related Publications
Gemcitabine (Gem) is widely used as chemotherapy for pancreatic cancer (PaCa), but its effect is not fully satisfactory. One of the reasons for this is the acquisition of Gem resistance (Gem‑R). To elucidate the mechanism of Gem‑R, two Gem‑R PaCa cell lines were established from AsPC‑1 and MIA PaCa‑2 cells. It was demonstrated that expression of interleukin‑8 (IL‑8) mRNA was significantly upregulated in Gem‑R PaCa cells by cDNA microarray and RT‑qPCR analyses. Increased IL‑8 secretion by Gem‑R cells was confirmed by cytokine array and enzyme‑linked immunosorbent assay. Moreover, we found that co‑culture with Gem‑R PaCa cells significantly enhanced tube formation of human umbilical vein endothelial cells, and treatment with an anti‑CXCR2 (main receptor for IL‑8) antibody significantly prevented this effect. We previously reported that a chemokine network centered on the IL‑8/CXCR2 axis plays an important role in PaCa angiogenesis, and suppression of this axis has an antitumor effect. Since acquisition of Gem‑R increased IL‑8 production and consequently increased tumor angiogenesis, the IL‑8/CXCR2 axis may be a potential novel therapeutic target for PaCa after acquiring Gem‑R.
Yang Y, Yang CL, Zhao ZJ, et al.
Microwave hyperthermia enhances the sensitivity of lung cancer cells to gemcitabine through reactive oxygen species‑induced autophagic death.
Oncol Rep. 2019; 41(5):3100-3110 [PubMed] Related Publications
Microwave hyperthermia enhances the sensitivity of lung cancer cells to gemcitabine through reactive oxygen species‑induced autophagic death.
Oncol Rep. 2019; 41(5):3100-3110 [PubMed] Related Publications
The pleiotropic effects of hyperthermia on cancer cells have been well documented, and microwave hyperthermia (MWHT) has been widely applied for multifarious cancer treatment. However, the mechanisms underlying the anticancer effect of MWHT combined with gemcitabine (GEM) remain poorly understood. The aim of the present study was to investigate the role of autophagy in the thermo‑chemotherapy of human squamous cell lung carcinoma cells. It was observed that MWHT combined with GEM potently suppressed the viability of NCI‑H2170 and NCI‑H1703 cells, and induced G0/G1 cell cycle arrest. Notably, MWHT with GEM induced autophagy, as indicated by the formation of autophagic vacuoles, downregulation of p62 and upregulation of light chain 3‑II. It was further demonstrated that the autophagy was due to the production of reactive oxygen species (ROS), whereas N‑acetyl cysteine, an ROS scavenger, attenuated the level of autophagy. However, when the autophagy inhibitor 3‑methyladenine was used, there was no significant change in the production of ROS. Furthermore, it was observed that MWHT combined with GEM downregulated the protein expression levels of phosphoinositide 3‑kinase (PI3K), phosphorylated (p)‑PI3K, protein kinase B (AKT), p‑AKT, mammalian target of rapamycin (mTOR), p‑mTOR, phosphorylated S6 (pS6) and p70 S6 kinase, which are associated with autophagy. In addition, the results demonstrated that ROS served as an upstream mediator of PI3K/AKT/mTOR signaling. In light of these findings, the present study provides original insights into the molecular mechanisms underlying the cell death induced by MWHT combined with GEM, and this may be a promising approach for the treatment of human squamous cell lung carcinoma.
Das A, Dean A, Clay T
Gemcitabine-induced haemolytic uraemic syndrome in pancreatic adenocarcinoma.
BMJ Case Rep. 2019; 12(4) [PubMed] Related Publications
Gemcitabine-induced haemolytic uraemic syndrome in pancreatic adenocarcinoma.
BMJ Case Rep. 2019; 12(4) [PubMed] Related Publications
A woman in her mid-70s with metastatic pancreatic adenocarcinoma presented with fatigue, nausea and bilateral leg swelling, 4 days after an intravenous gemcitabine infusion. Additional examination and laboratory tests showed mild hypertension, low haemoglobin, high lactate dehydrogenase, low platelet count and high serum creatinine. The patient was subsequently diagnosed with haemolytic uraemic syndrome (HUS), and gemcitabine administration was immediately ceased. The patient received a 5-day course of methylprednisolone, with a full recovery being made 10 days after diagnosis. Clinicians should be aware of the rare but serious complication of gemcitabine-induced HUS (GiHUS), as early diagnosis and management, which includes prompt discontinuation of gemcitabine, are crucial in promptly resolving this condition. This case report describes one treatment that can be used for the treatment of GiHUS, while briefly covering some other novel treatments that have been described in other studies.
Yang WH, Xie J, Lai ZY, et al.
Radiofrequency deep hyperthermia combined with chemotherapy in the treatment of advanced non-small cell lung cancer.
Chin Med J (Engl). 2019; 132(8):922-927 [PubMed] Free Access to Full Article Related Publications
Radiofrequency deep hyperthermia combined with chemotherapy in the treatment of advanced non-small cell lung cancer.
Chin Med J (Engl). 2019; 132(8):922-927 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: In the era of precision medicine, chemotherapy is still considered the cornerstone of treatment for lung cancer patients without gene mutations. How to reduce the toxicity and increase the efficiency of chemotherapy is worth exploring. This study aimed to investigate the curative effects and safety of hyperthermia combined with chemotherapy (HCT) for advanced patients with non-small cell lung cancer (NSCLC), especially those with malignant pleural effusion.
METHODS: We retrospectively evaluated medical records of 93 patients with advanced NSCLC (stage IIIB-IV) from March 2011 to January 2014. The patients were divided into HCT and chemotherapy (CT) groups. The HCT group was treated with gemcitabine and cisplatin (GP) regimen combined with regional radiofrequency deep hyperthermia, while the CT group was treated with GP regimen only. Those with malignant pleural effusion extra underwent thoracentesis and intrapleural injection chemotherapy combined with hyperthermic or not. Clinical treatment results and adverse reactions were compared and analyzed after treatment. SPSS 19.0 software (SPSS Inc., USA) was used for statistical data processing. P values less than 0.05 were accepted to be statistically significant.
RESULTS: Among the 93 patients, HCT group included 48 patients (16 patients with malignant pleural effusion), CT group included 45 patients (10 patients with malignant pleural effusion). There was no significant difference between the two groups in patient characteristics. The overall response rate (ORR) of pleural effusions was much better in HCT group than that in CT group (81.2% vs. 40.0%, P = 0.046). The patients in HCT group had lower incidence rate of weakness (12.5% vs. 46.7%, χ = 13.16, P < 0.001) and gastrointestinal (25.0% vs. 77.8%, χ = 25.88, P < 0.001) adverse reactions than that in CT group. The objective tumor response and survival showed no significant differences.
CONCLUSIONS: Hyperthermia combined with chemotherapy might lead to the development of better therapeutic strategy for advanced NSCLC with malignant pleural effusion patients. Also, it could greatly reduce the chemotherapy toxic effects in the incidence of weakness and gastrointestinal adverse reactions in advanced NSCLC patients.
METHODS: We retrospectively evaluated medical records of 93 patients with advanced NSCLC (stage IIIB-IV) from March 2011 to January 2014. The patients were divided into HCT and chemotherapy (CT) groups. The HCT group was treated with gemcitabine and cisplatin (GP) regimen combined with regional radiofrequency deep hyperthermia, while the CT group was treated with GP regimen only. Those with malignant pleural effusion extra underwent thoracentesis and intrapleural injection chemotherapy combined with hyperthermic or not. Clinical treatment results and adverse reactions were compared and analyzed after treatment. SPSS 19.0 software (SPSS Inc., USA) was used for statistical data processing. P values less than 0.05 were accepted to be statistically significant.
RESULTS: Among the 93 patients, HCT group included 48 patients (16 patients with malignant pleural effusion), CT group included 45 patients (10 patients with malignant pleural effusion). There was no significant difference between the two groups in patient characteristics. The overall response rate (ORR) of pleural effusions was much better in HCT group than that in CT group (81.2% vs. 40.0%, P = 0.046). The patients in HCT group had lower incidence rate of weakness (12.5% vs. 46.7%, χ = 13.16, P < 0.001) and gastrointestinal (25.0% vs. 77.8%, χ = 25.88, P < 0.001) adverse reactions than that in CT group. The objective tumor response and survival showed no significant differences.
CONCLUSIONS: Hyperthermia combined with chemotherapy might lead to the development of better therapeutic strategy for advanced NSCLC with malignant pleural effusion patients. Also, it could greatly reduce the chemotherapy toxic effects in the incidence of weakness and gastrointestinal adverse reactions in advanced NSCLC patients.
Morino K, Seo S, Yoh T, et al.
The Efficacy and Limitations of Postoperative Adjuvant Chemotherapy in Patients With Extrahepatic Cholangiocarcinoma.
Anticancer Res. 2019; 39(4):2155-2161 [PubMed] Related Publications
The Efficacy and Limitations of Postoperative Adjuvant Chemotherapy in Patients With Extrahepatic Cholangiocarcinoma.
Anticancer Res. 2019; 39(4):2155-2161 [PubMed] Related Publications
BACKGROUND/AIM: The impact of adjuvant chemotherapy (AC) for extrahepatic cholangiocarcinoma (ECC) remains unclear. This study evaluated the efficacy and limitations of AC.
PATIENTS AND METHODS: Between 2006 and 2016, 106 patients with stage II-IV ECC who underwent curative resection with biliary tract reconstruction were retrospectively analyzed. Patients were divided into two groups: Those who received AC (n=57) and those who did not (n=49).
RESULTS: Fewer grade 3-4 complications were observed in the AC group compared to the non-AC group (38.6 vs. 61.2%, p=0.03). In the non-AC group, complications were the most frequent reason for omitting AC (n=21, including 13 with biliary fistula). In the AC group, the therapy completion rate was 56.1% and the main reason for discontinuation was adverse events (n=12, including six with cholangitis). AC was not associated with survival benefits (median survival: 50.4 vs. 37.3 months, p=0.916).
CONCLUSION: AC for ECC might be inadequate as a standard strategy due to the low implementation and completion rates because complications often hamper administration.
PATIENTS AND METHODS: Between 2006 and 2016, 106 patients with stage II-IV ECC who underwent curative resection with biliary tract reconstruction were retrospectively analyzed. Patients were divided into two groups: Those who received AC (n=57) and those who did not (n=49).
RESULTS: Fewer grade 3-4 complications were observed in the AC group compared to the non-AC group (38.6 vs. 61.2%, p=0.03). In the non-AC group, complications were the most frequent reason for omitting AC (n=21, including 13 with biliary fistula). In the AC group, the therapy completion rate was 56.1% and the main reason for discontinuation was adverse events (n=12, including six with cholangitis). AC was not associated with survival benefits (median survival: 50.4 vs. 37.3 months, p=0.916).
CONCLUSION: AC for ECC might be inadequate as a standard strategy due to the low implementation and completion rates because complications often hamper administration.
Mu XY, Wang RJ, Yao ZX, et al.
RS 504393 inhibits M-MDSCs recruiting in immune microenvironment of bladder cancer after gemcitabine treatment.
Mol Immunol. 2019; 109:140-148 [PubMed] Related Publications
RS 504393 inhibits M-MDSCs recruiting in immune microenvironment of bladder cancer after gemcitabine treatment.
Mol Immunol. 2019; 109:140-148 [PubMed] Related Publications
Bladder cancer (BC) is a malignant tumor of urinary epithelium. Gemcitabine is an introduced treatment for BC and also has immunomodulatory function, but the immunoregulation mechanism is not clear. In this study, we found that gemcitabine-treated BC cell recruited more monocyte-myeloid-derived suppressed cells (M-MDSCs), which played a significant role in immune suppression and contributed to cancer progression. We found that this phenomenon was induced by Chemokine (C-C motif) ligand 2 (CCL2), an M-MDSCs recruitment related monomeric polypeptide. Gemcitabine treatment promotes the generation of CCL2 and CCL2 could attach to C-C chemokine receptor type 2 (CCR2) to recruit M-MDSCs. We used RS 504393, a selective CCR2 antagonist, to inhibit the recruitment of M-MDSCs. RS 504393 improved the prognosis by blocking chemotaxis of M-MDSCs, and this finding sheds lights on how to prevent and alleviate the side effects occurred on the gemcitabine-treated BC patients.
Werthmann PG, Kempenich R, Lang-Avérous G, Kienle GS
Long-term survival of a patient with advanced pancreatic cancer under adjunct treatment with
World J Gastroenterol. 2019; 25(12):1524-1530 [PubMed] Free Access to Full Article Related Publications
Long-term survival of a patient with advanced pancreatic cancer under adjunct treatment with
World J Gastroenterol. 2019; 25(12):1524-1530 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Advanced pancreatic cancer (aPC) has a poor prognosis with limited survival benefit from current standard treatment.
CASE SUMMARY: A 59-year-old architect developed epigastric pain. A cystic lesion of the pancreas of 45-mm diameter was detected. In a follow-up magnetic resonance imaging, about one year later, multiple lesions were seen in the corpus and the tail of the pancreas; CA-19-9 was elevated to 58.5 U/mL. A distal pancreatectomy with splenectomy was performed, and a tumor of 7 cm × 5 cm × 3.5 cm was excised. Histologic investigation showed an intraductal papillary mucinous neoplasm-associated invasive adenocarcinoma with invasion of the lymph vessels, perineural invasion, and positive nodes (2/27); surgical margins showed tumor cells, and the tumor was classified as pT3 N1 M0 R1. The patient was treated with radiation of the tumor bed and capecitabine/oxaliplatin followed by gemcitabine and FOLFIRINOX. Seven months after surgery, a liver metastasis was detected and treatment with FOLFIRINOX was started. Four months after detection of the metastasis, the patient opted for additional treatment with VAE. Another month later, the metastasis was treated with radiofrequency ablation (RFA). Eight months later, the hepatic lesion recurred and was again treated with RFA. The continuous VAE treatment was increased in dose, and the patient stayed recurrence-free for the next 39 mo in good health and working full-time (as of the time this case report was written).
CONCLUSION: We present the case of a patient with aPC with R1-resection with development of liver metastasis during the course of treatment who showed an overall survival of 63 mo and a relapse-free survival of 39 mo under increasing VAE therapy. The possible synergistic effect on tumor control of RFA treatment and immune-stimulatory effects of VAE should be further investigated.
CASE SUMMARY: A 59-year-old architect developed epigastric pain. A cystic lesion of the pancreas of 45-mm diameter was detected. In a follow-up magnetic resonance imaging, about one year later, multiple lesions were seen in the corpus and the tail of the pancreas; CA-19-9 was elevated to 58.5 U/mL. A distal pancreatectomy with splenectomy was performed, and a tumor of 7 cm × 5 cm × 3.5 cm was excised. Histologic investigation showed an intraductal papillary mucinous neoplasm-associated invasive adenocarcinoma with invasion of the lymph vessels, perineural invasion, and positive nodes (2/27); surgical margins showed tumor cells, and the tumor was classified as pT3 N1 M0 R1. The patient was treated with radiation of the tumor bed and capecitabine/oxaliplatin followed by gemcitabine and FOLFIRINOX. Seven months after surgery, a liver metastasis was detected and treatment with FOLFIRINOX was started. Four months after detection of the metastasis, the patient opted for additional treatment with VAE. Another month later, the metastasis was treated with radiofrequency ablation (RFA). Eight months later, the hepatic lesion recurred and was again treated with RFA. The continuous VAE treatment was increased in dose, and the patient stayed recurrence-free for the next 39 mo in good health and working full-time (as of the time this case report was written).
CONCLUSION: We present the case of a patient with aPC with R1-resection with development of liver metastasis during the course of treatment who showed an overall survival of 63 mo and a relapse-free survival of 39 mo under increasing VAE therapy. The possible synergistic effect on tumor control of RFA treatment and immune-stimulatory effects of VAE should be further investigated.
Cheng SH, Cheng YJ, Jin ZY, Xue HD
Unresectable pancreatic ductal adenocarcinoma: Role of CT quantitative imaging biomarkers for predicting outcomes of patients treated with chemotherapy.
Eur J Radiol. 2019; 113:188-197 [PubMed] Related Publications
Unresectable pancreatic ductal adenocarcinoma: Role of CT quantitative imaging biomarkers for predicting outcomes of patients treated with chemotherapy.
Eur J Radiol. 2019; 113:188-197 [PubMed] Related Publications
OBJECTIVES: The primary aim of this study was to determine if computed tomographic (CT) texture analysis measurements of the tumor are independently associated with progression-free survival (PFS) and overall survival (OS) in patients with unresectable pancreatic ductal adenocarcinoma (PDAC), including both unresectable locally advanced and metastatic PDAC, who were treated with chemotherapy.
METHODS: After an institutional review board waiver was obtained, contrast material-enhanced CT studies in 41 patients with unresectable PDAC who underwent contrast-enhanced CT before chemotherapy between 2014 and 2017 were analyzed in terms of tumor texture, with quantification of mean gray-level intensity (Mean), entropy, mean of positive pixels (MPP), kurtosis, standard deviation (SD), and skewness for fine to coarse textures (spatial scaling factor (SSF) 0-6, respectively). The association between pretreatment and posttreatment texture parameters, as well as Δ value (difference between posttreatment and pretreatment texture parameters), and survival time was assessed by using Cox proportional hazards models and Kaplan-Meier analysis.
RESULTS: Findings from the multivariate Cox model indicated that tumor size, tumor SD (HR, 0.942; 95% CI: 0.898, 0.988) and skewness (HR, 0.407; 95% CI: 0.172, 0.962) measurements with SSF = 3, and tumor SD (HR, 0.958; 95% CI: 0.92, 0.997) measurements with SSF = 4 were significantly and independently associated with PFS, while tumor size and tumor SD (HR, 0.928; 95% CI: 0.882, 0.976) measurements with SSF = 3 were significantly and independently associated with OS. None of the post-therapy texture parameters or Δ value had a significant association with OS or PFS in multivariate Cox regression models. Medium SD (SSF = 3) of more than 38.38 and coarse SD (SSF = 4) of more than 40.67 were associated with longer PFS after chemotherapy (for SSF = 3, median PFS was 10.0 vs 6.0 months [P = 0.024], and for SSF = 4, median PFS was 12.0 vs 6.0 months [P = 0.003]). SD of 38.38 or greater (SSF = 3) as a dichotomized variable was a significant positive prognostic factor for OS (median OS, 20.0 vs 9.0 months [P = 0.04]). Survival models that included a combination of pretreatment SD (SSF = 3) with tumor size, had the potential to perform better than SD alone, while having no statistical significance in this study (area under the ROC curve, 0.756 vs 0.715 [P = 0.066]).
CONCLUSIONS: Pretreatment CT quantitative imaging biomarkers from texture analysis are associated with PFS and OS in patients with unresectable PDAC who were treated with chemotherapy, and the combination of pretreatment texture parameters and tumor size have the potential to perform better in survival models than imaging biomarker alone.
METHODS: After an institutional review board waiver was obtained, contrast material-enhanced CT studies in 41 patients with unresectable PDAC who underwent contrast-enhanced CT before chemotherapy between 2014 and 2017 were analyzed in terms of tumor texture, with quantification of mean gray-level intensity (Mean), entropy, mean of positive pixels (MPP), kurtosis, standard deviation (SD), and skewness for fine to coarse textures (spatial scaling factor (SSF) 0-6, respectively). The association between pretreatment and posttreatment texture parameters, as well as Δ value (difference between posttreatment and pretreatment texture parameters), and survival time was assessed by using Cox proportional hazards models and Kaplan-Meier analysis.
RESULTS: Findings from the multivariate Cox model indicated that tumor size, tumor SD (HR, 0.942; 95% CI: 0.898, 0.988) and skewness (HR, 0.407; 95% CI: 0.172, 0.962) measurements with SSF = 3, and tumor SD (HR, 0.958; 95% CI: 0.92, 0.997) measurements with SSF = 4 were significantly and independently associated with PFS, while tumor size and tumor SD (HR, 0.928; 95% CI: 0.882, 0.976) measurements with SSF = 3 were significantly and independently associated with OS. None of the post-therapy texture parameters or Δ value had a significant association with OS or PFS in multivariate Cox regression models. Medium SD (SSF = 3) of more than 38.38 and coarse SD (SSF = 4) of more than 40.67 were associated with longer PFS after chemotherapy (for SSF = 3, median PFS was 10.0 vs 6.0 months [P = 0.024], and for SSF = 4, median PFS was 12.0 vs 6.0 months [P = 0.003]). SD of 38.38 or greater (SSF = 3) as a dichotomized variable was a significant positive prognostic factor for OS (median OS, 20.0 vs 9.0 months [P = 0.04]). Survival models that included a combination of pretreatment SD (SSF = 3) with tumor size, had the potential to perform better than SD alone, while having no statistical significance in this study (area under the ROC curve, 0.756 vs 0.715 [P = 0.066]).
CONCLUSIONS: Pretreatment CT quantitative imaging biomarkers from texture analysis are associated with PFS and OS in patients with unresectable PDAC who were treated with chemotherapy, and the combination of pretreatment texture parameters and tumor size have the potential to perform better in survival models than imaging biomarker alone.
Liu T, He Z, Dang J, Li G
Comparative efficacy and safety for different chemotherapy regimens used concurrently with thoracic radiation for locally advanced non-small cell lung cancer: a systematic review and network meta-analysis.
Radiat Oncol. 2019; 14(1):55 [PubMed] Free Access to Full Article Related Publications
Comparative efficacy and safety for different chemotherapy regimens used concurrently with thoracic radiation for locally advanced non-small cell lung cancer: a systematic review and network meta-analysis.
Radiat Oncol. 2019; 14(1):55 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: It remains unknown which is the most preferable regimen used concurrently with thoracic radiation for locally advanced non-small cell lung cancer (NSCLC). We performed a network meta-analysis to address this important issue.
METHODS: PubMed, Embase, Cochrane Library, Web of Science and major international scientific meetings were searched for relevant randomized controlled trials (RCTs). Overall survival (OS) data was the primary outcome of interest, and progression-free survival (PFS), and serious adverse events (SAEs) were the secondary outcomes of interests, reported as hazard ratio (HR) or odds ratio (OR) and 95% confidence intervals (CIs).
RESULTS: 14 RCTs with a total of 2975 patients randomized to receive twelve categories of treatments were included in the meta-analysis. Direct comparison meta-analysis showed that etoposide-cisplatin (EP) was more effective than paclitaxel-cisplatin/carboplatin (PC) in terms of OS (HR = 0.85, 95% CI: 0.77-0.94) and PFS (HR = 0.66, 95% CI: 0.47-0.95). In network meta-analysis, all regimen comparisons did not produce statistically significant differences in survival. Based on treatment ranking of OS and the benefit-risk ratio, S-1-cisplatin (SP) was likely to be the most preferable regimen for its best efficacy and low risk of causing SAEs. Uracil/tegafur-cisplatin (UP) and pemetrexed-cisplatin/carboplatin (PP) were ranked the second and third respectively. Gemcitabine-cisplatin (GP) and PC + Cetuximab (PC-Cet) appeared to be the worst and second-worst regimens for their poor efficacy and poor tolerability.
CONCLUSIONS: Based on efficacy and tolerability, SP is likely to be the most preferable regimen used concurrently with thoracic radiation for locally advanced NSCLC, followed by UP and PP. Further direct head-to-head studies are needed to confirm these findings.
METHODS: PubMed, Embase, Cochrane Library, Web of Science and major international scientific meetings were searched for relevant randomized controlled trials (RCTs). Overall survival (OS) data was the primary outcome of interest, and progression-free survival (PFS), and serious adverse events (SAEs) were the secondary outcomes of interests, reported as hazard ratio (HR) or odds ratio (OR) and 95% confidence intervals (CIs).
RESULTS: 14 RCTs with a total of 2975 patients randomized to receive twelve categories of treatments were included in the meta-analysis. Direct comparison meta-analysis showed that etoposide-cisplatin (EP) was more effective than paclitaxel-cisplatin/carboplatin (PC) in terms of OS (HR = 0.85, 95% CI: 0.77-0.94) and PFS (HR = 0.66, 95% CI: 0.47-0.95). In network meta-analysis, all regimen comparisons did not produce statistically significant differences in survival. Based on treatment ranking of OS and the benefit-risk ratio, S-1-cisplatin (SP) was likely to be the most preferable regimen for its best efficacy and low risk of causing SAEs. Uracil/tegafur-cisplatin (UP) and pemetrexed-cisplatin/carboplatin (PP) were ranked the second and third respectively. Gemcitabine-cisplatin (GP) and PC + Cetuximab (PC-Cet) appeared to be the worst and second-worst regimens for their poor efficacy and poor tolerability.
CONCLUSIONS: Based on efficacy and tolerability, SP is likely to be the most preferable regimen used concurrently with thoracic radiation for locally advanced NSCLC, followed by UP and PP. Further direct head-to-head studies are needed to confirm these findings.
Liu D, Qiao X, Ge Z, et al.
IMB0901 inhibits muscle atrophy induced by cancer cachexia through MSTN signaling pathway.
Skelet Muscle. 2019; 9(1):8 [PubMed] Free Access to Full Article Related Publications
IMB0901 inhibits muscle atrophy induced by cancer cachexia through MSTN signaling pathway.
Skelet Muscle. 2019; 9(1):8 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Cancer cachexia as a metabolic syndrome can lead to at least 25% of cancer deaths. The inhibition of muscle atrophy is a main strategy to treat cancer cachexia. In this process, myostatin (MSTN) can exert a dual effect on protein metabolism, including inhibition of protein biosynthesis and enhancement of protein degradation. In this study, we will test the effect on muscle atrophy induced by cancer cachexia of IMB0901, a MSTN inhibitor.
METHODS: Two high-throughput screening models against MSTN were developed. By screening, IMB0901, 2-((1-(3,4-dichlorophenyl)-1H-pyrazolo [3,4-d] pyrimidin-4-yl) amino) butan-1-ol, was picked out from the compound library. The in vitro cell model and the C26 animal model of muscle atrophy induced by cancer cachexia were used to determine the pharmacological activity of IMB0901. Whether IMB0901 could inhibit the aggravating effect of doxorubicin on muscle wasting was examined in vitro and in vivo.
RESULTS: IMB0901 inhibited the MSTN promoter activity, the MSTN signaling pathway, and the MSTN positive feedback regulation. In atrophied C2C12 myotubes, IMB0901 had a potent efficiency of decreasing MSTN expression and modulating MSTN signaling pathway which was activated by C26-conditioned medium (CM). In C2C12 myotubes, the expressions of three common myotube markers, myosin heavy chain (MyHC), myogenic differentiation 1 (MyoD), and myogenin (MyoG), were downregulated by CM, which could be efficiently reversed by IMB0901 via reduction of ubiquitin-mediated proteolysis and enhancement of AKT/mTOR-mediated protein synthesis. In the C26 animal model, IMB0901 mitigated the weight loss of body, quadricep and liver, and protected the quadriceps cell morphology. Furthermore, IMB0901 decreased the expression of two E3 ligases Atrogin-1 and MuRF-1 in the quadriceps in vivo. At the cellular level, IMB0901 had no influence on anti-tumor effect of three chemotherapeutic agents (cisplatin, doxorubicin, and gemcitabine) and lowered doxorubicin-induced upregulation of MSTN in C2C12 myotubes. IMB0901 did not affect the inhibitory effect of doxorubicin on C26 tumor and delayed the weight loss of muscle and adipose tissue caused by C26 tumor and doxorubicin.
CONCLUSIONS: IMB0901 inhibits muscle atrophy induced by cancer cachexia by suppressing ubiquitin-mediated proteolysis and promoting protein synthesis. These findings collectively suggest that IMB0901 is a promising leading compound for the management of muscle atrophy induced by cancer cachexia.
METHODS: Two high-throughput screening models against MSTN were developed. By screening, IMB0901, 2-((1-(3,4-dichlorophenyl)-1H-pyrazolo [3,4-d] pyrimidin-4-yl) amino) butan-1-ol, was picked out from the compound library. The in vitro cell model and the C26 animal model of muscle atrophy induced by cancer cachexia were used to determine the pharmacological activity of IMB0901. Whether IMB0901 could inhibit the aggravating effect of doxorubicin on muscle wasting was examined in vitro and in vivo.
RESULTS: IMB0901 inhibited the MSTN promoter activity, the MSTN signaling pathway, and the MSTN positive feedback regulation. In atrophied C2C12 myotubes, IMB0901 had a potent efficiency of decreasing MSTN expression and modulating MSTN signaling pathway which was activated by C26-conditioned medium (CM). In C2C12 myotubes, the expressions of three common myotube markers, myosin heavy chain (MyHC), myogenic differentiation 1 (MyoD), and myogenin (MyoG), were downregulated by CM, which could be efficiently reversed by IMB0901 via reduction of ubiquitin-mediated proteolysis and enhancement of AKT/mTOR-mediated protein synthesis. In the C26 animal model, IMB0901 mitigated the weight loss of body, quadricep and liver, and protected the quadriceps cell morphology. Furthermore, IMB0901 decreased the expression of two E3 ligases Atrogin-1 and MuRF-1 in the quadriceps in vivo. At the cellular level, IMB0901 had no influence on anti-tumor effect of three chemotherapeutic agents (cisplatin, doxorubicin, and gemcitabine) and lowered doxorubicin-induced upregulation of MSTN in C2C12 myotubes. IMB0901 did not affect the inhibitory effect of doxorubicin on C26 tumor and delayed the weight loss of muscle and adipose tissue caused by C26 tumor and doxorubicin.
CONCLUSIONS: IMB0901 inhibits muscle atrophy induced by cancer cachexia by suppressing ubiquitin-mediated proteolysis and promoting protein synthesis. These findings collectively suggest that IMB0901 is a promising leading compound for the management of muscle atrophy induced by cancer cachexia.
Gao S, Zhu X, Shi X, et al.
Comparisons of different neoadjuvant chemotherapy regimens with or without stereotactic body radiation therapy for borderline resectable pancreatic cancer: study protocol of a prospective, randomized phase II trial (BRPCNCC-1).
Radiat Oncol. 2019; 14(1):52 [PubMed] Free Access to Full Article Related Publications
Comparisons of different neoadjuvant chemotherapy regimens with or without stereotactic body radiation therapy for borderline resectable pancreatic cancer: study protocol of a prospective, randomized phase II trial (BRPCNCC-1).
Radiat Oncol. 2019; 14(1):52 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Few patients with pancreatic cancer may be candidates for immediate surgical resection at the initial diagnosis. Even if patients with borderline resectable pancreatic cancer (BRPC), micrometastases may occur before surgery. Therefore, neoadjuvant therapy is vital for improved survival, which has been confirmed in previous studies that neoadjuvant chemotherapy with or without radiotherapy provides superior overall compared with upfront surgery. However, question of whether the addition of radiotherapy to neoadjuvant chemotherapy can improve prognosis compared with chemotherapy alone is a challenging matter. Moreover, most of previous studies only adopted conventional radiotherapy as the neoadjuvant modality though stereotactic body radiation therapy (SBRT) has been proven effective and commonly employed in pancreatic cancer. Also, no studies have evaluated the efficacy of S-1 as the neoadjuvant chemotherapy regimen for BRPC albeit similar prognosis has been found between S-1 and gemcitabine in advanced pancreatic cancer. Hence, the aim of this study is to investigate whether neoadjuvant chemotherapy plus SBRT results in better outcomes compared with neoadjuvant chemotherapy alone and also compare the efficacy of gemcitabine plus nab-paclitaxel with SBRT and S-1 plus nab-paclitaxel with SBRT.
METHODS: Patients with biopsy and radiographically confirmed BRPC, no prior treatment and severe morbidities are enrolled. They will be randomly allocated into three groups: neoadjuvant gemcitabine plus nab-paclitaxel, neoadjuvant gemcitabine plus nab-paclitaxel with SBRT and neoadjuvant S-1 plus nab-paclitaxel with SBRT. Standard doses of gemcitabine and nab-paclitaxel are used. The radiation dose of SBRT is 7.5-8Gy/f for 5 fractions. Surgical resection will be performed 3 weeks after SBRT. Artery first approach pancreaticoduodenectomy or radical antegrade modular pancreatosplenectomy will be used for the tumor in the head or body and tail of the pancreas, respectively. The primary endpoint is overall survival. The secondary outcomes are disease free survival, pathological complete response rate, R0 resection rate and incidence of adverse effects.
DISCUSSION: If results show the survival benefits of neoadjuvant chemotherapy plus SBRT and similar outcomes between S-1 and gemcitabine, it may provide evidence of clinical practice of this modality for BRPC.
TRIAL REGISTRATION: The study has been registered in ClinicalTrial.gov ( NCT03777462 ).
METHODS: Patients with biopsy and radiographically confirmed BRPC, no prior treatment and severe morbidities are enrolled. They will be randomly allocated into three groups: neoadjuvant gemcitabine plus nab-paclitaxel, neoadjuvant gemcitabine plus nab-paclitaxel with SBRT and neoadjuvant S-1 plus nab-paclitaxel with SBRT. Standard doses of gemcitabine and nab-paclitaxel are used. The radiation dose of SBRT is 7.5-8Gy/f for 5 fractions. Surgical resection will be performed 3 weeks after SBRT. Artery first approach pancreaticoduodenectomy or radical antegrade modular pancreatosplenectomy will be used for the tumor in the head or body and tail of the pancreas, respectively. The primary endpoint is overall survival. The secondary outcomes are disease free survival, pathological complete response rate, R0 resection rate and incidence of adverse effects.
DISCUSSION: If results show the survival benefits of neoadjuvant chemotherapy plus SBRT and similar outcomes between S-1 and gemcitabine, it may provide evidence of clinical practice of this modality for BRPC.
TRIAL REGISTRATION: The study has been registered in ClinicalTrial.gov ( NCT03777462 ).


 Cisplatin
Cisplatin