Found this page useful?
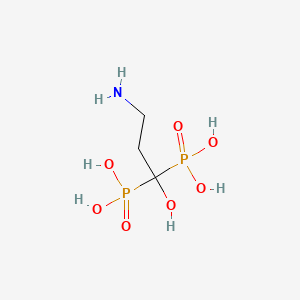
Pamidronate (Aredia)
 Web Resources: NBS
Web Resources: NBS Latest Research Publications
Latest Research PublicationsWeb Resources: NBS (7 links)
Macmillan Cancer Support![]() Content is developed by a team of information development nurses and content editors, and reviewed by health professionals. Further info.
Content is developed by a team of information development nurses and content editors, and reviewed by health professionals. Further info.
NHS Evidence
American Cancer Society
 pamidronate - Compound Summary
pamidronate - Compound Summary
Oncolink
National Cancer Institute
Short summary
MedlinePlus
Latest Research Publications
von Moos R, Costa L, Gonzalez-Suarez E, et al.
Management of bone health in solid tumours: From bisphosphonates to a monoclonal antibody.
Cancer Treat Rev. 2019; 76:57-67 [PubMed] Related Publications
Management of bone health in solid tumours: From bisphosphonates to a monoclonal antibody.
Cancer Treat Rev. 2019; 76:57-67 [PubMed] Related Publications
Patients with solid tumours are at risk of impaired bone health from metastases and cancer therapy-induced bone loss (CTIBL). We review medical management of bone health in patients with solid tumours over the past 30 years, from first-generation bisphosphonates to the receptor activator of nuclear factor κB ligand (RANKL)-targeted monoclonal antibody, denosumab. In the 1980s, first-generation bisphosphonates were shown to reduce the incidence of skeletal-related events (SREs) in patients with breast cancer. Subsequently, more potent second- and third-generation bisphosphonates were developed, particularly zoledronic acid (ZA). Head-to-head studies showed that ZA was significantly more effective than pamidronate for reducing SREs in patients with breast and castrate-resistant prostate cancer (CRPC), becoming the standard of care for more than a decade. The RANKL inhibitor denosumab was licensed in 2010, and head-to-head studies and integrated analyses confirmed its superiority to ZA for preventing SREs, particularly in breast cancer and CRPC. Bisphosphonates and denosumab have also been investigated for prevention of CTIBL in patients receiving hormonal therapy for breast and prostate cancer, and denosumab is licensed in this indication. Despite advances in management of bone health, several issues remain, notably the optimal time to initiate therapy, duration of therapy, and dosing frequency, and how to avoid toxicity, particularly with long-term treatment. In summary, introduction of ZA and denosumab has protected patients with bone metastasis from serious bone complications and improved their quality of life. Ongoing research will hopefully guide the optimal use of these agents to help maintain bone health in patients with solid tumours.
Tesfamariam Y, Jakob T, Wöckel A, et al.
Adjuvant bisphosphonates or RANK-ligand inhibitors for patients with breast cancer and bone metastases: A systematic review and network meta-analysis.
Crit Rev Oncol Hematol. 2019; 137:1-8 [PubMed] Related Publications
Adjuvant bisphosphonates or RANK-ligand inhibitors for patients with breast cancer and bone metastases: A systematic review and network meta-analysis.
Crit Rev Oncol Hematol. 2019; 137:1-8 [PubMed] Related Publications
Bone-modifying agents like bisphosphonates and receptor activator of nuclear factor kappaβ ligand (RANK-L) inhibitors are used as supportive treatments in breast cancer patients with bone metastases to prevent skeletal-related events (SREs). Due to missing head-to-head comparisons, a network meta-analysis was performed to provide a hierarchy of these therapeutic options. Through a systematic literature search, 21 randomized controlled trials (RCTs) that fulfilled the inclusion criteria were identified. To prevent SREs, the ranking through P-scores showed denosumab (RR: 0.62; 95%CI: 0.50-0.76), zoledronic acid (RR: 0.72; 95%CI: 0.61-0.84) and pamidronate (RR: 0.76; 95%CI: 0.67-0.85) to be significantly superior to placebo. Due to insufficient or heterogeneous data, overall survival, quality of life, pain response and adverse events were not able to be analyzed within the network. Although data were sparse on adverse events, the risk of significant adverse events appeared low. The results of this review can therefore be used to formulate clinical studies more precisely in order to standardise and focus on patient-relevant outcomes.
Mao TL, Miao CH, Liao YJ, et al.
Ex Vivo Expanded Human Vγ9Vδ2 T-Cells Can Suppress Epithelial Ovarian Cancer Cell Growth.
Int J Mol Sci. 2019; 20(5) [PubMed] Free Access to Full Article Related Publications
Ex Vivo Expanded Human Vγ9Vδ2 T-Cells Can Suppress Epithelial Ovarian Cancer Cell Growth.
Int J Mol Sci. 2019; 20(5) [PubMed] Free Access to Full Article Related Publications
γδ-T-cells have attracted attention because of their potent cytotoxicity towards tumors. Most γδ-T-cells become activated via a major histocompatibility complex (MHC)-independent pathway by the interaction of their receptor, Natural Killer Group 2 Member D (NKG2D) with the tumor-specific NKG2D ligands, including MHC class I-related chain A/B (MICA/B) and UL16-binding proteins (ULBPs), to kill tumor cells. However, despite their potent antitumor effects, the treatment protocols specifically targeting ovarian tumors require further improvements. Ovarian cancer is one of the most lethal and challenging female malignancies worldwide because of delayed diagnoses and resistance to traditional chemotherapy. In this study, we successfully enriched and expanded γδ-T-cells up to ~78% from peripheral blood mononuclear cells (PBMCs) with mostly the Vγ9Vδ2-T-cell subtype in the circulation. We showed that expanded γδ-T-cells alone exerted significant cytotoxic activities towards specific epithelial-type OVCAR3 and HTB75 cells, whereas the combination of γδ-T cells and pamidronate (PAM), a kind of aminobisphosphonates (NBPs), showed significantly enhanced cytotoxic activities towards all types of ovarian cancer cells in vitro. Furthermore, in tumor xenografts of immunodeficient NSG mice, γδ-T-cells not only suppressed tumor growth but also completely eradicated preexisting tumors with an initial size of ~5 mm. Thus, we concluded that γδ-T-cells alone possess dramatic cytotoxic activities towards epithelial ovarian cancers both in vitro and in vivo. These results strongly support the potential of clinical immunotherapeutic application of γδ-T-cells to treat this serious female malignancy.
Wen L, Yao J, Valderrama A
Evaluation of Treatment Patterns and Costs in Patients with Prostate Cancer and Bone Metastases.
J Manag Care Spec Pharm. 2019; 25(3-b Suppl):S1-S11 [PubMed] Related Publications
Evaluation of Treatment Patterns and Costs in Patients with Prostate Cancer and Bone Metastases.
J Manag Care Spec Pharm. 2019; 25(3-b Suppl):S1-S11 [PubMed] Related Publications
BACKGROUND: There are a lack of guideline recommendations for patients with metastatic castration-resistant prostate cancer (mCRPC) undergoing treatment progression and sequencing. Understanding treatment patterns and associated utilization and costs may help inform stakeholders and guide decision making.
OBJECTIVE: To describe treatment patterns and health care costs in prostate cancer (PC) patients with bone metastases treated with agents approved by the FDA for mCRPC.
METHODS: 2 large integrated claims databases (MarketScan and PharMetrics) were used to identify males aged ≥ 18 years who were diagnosed and treated for PC (ICD-9-CM code 185.xx or 233.4) with bone metastases (ICD-9-CM code 198.5) from June 2013 to September 2014. Patients were required to be continuously enrolled for ≥ 6 months before and after initiation of treatment with abiraterone, cabazitaxel, docetaxel, enzalutamide, mitoxantrone, radium-223, sipuleucel-T, or other chemotherapy. Study endpoints included lines of therapy, health care resource utilization per patient per month (PPPM), PPPM costs, and mortality rate. Descriptive analysis was completed for the study sample, and survival function was calculated via Kaplan-Meier estimates.
RESULTS: There were 953 patients meeting all inclusion criteria in the MarketScan database and 565 patients in the PharMetrics database. The median follow-up time was 18 months (interquartile range [IQR] = 14-23) for MarketScan and 14 months (IQR = 11-18) for PharMetrics. Mean age (SD) was 71 (± 10.7) and 66 (± 9.3) years, respectively. Before mCRPC treatment initiation, patients received palliative radiation therapy and bone antiresorptive therapy. For MarketScan and PharMetrics, respectively, 14.0% and 18.2% of patients received radiation therapy, 36.1% and 40.0% received denosumab; 16.5% and 16.8% received zoledronic acid; and 0.2% and 0.8% received pamidronate. Across both databases, abiraterone was the most commonly received bone metastasis treatment agent across all lines of therapy, except fourth line. Radium-223, cabazitaxel, and mitoxantrone were the least utilized therapies. The median cost PPPM during the post-index period was $10,916 (IQR=$5,334-$13,457) in MarketScan and $10,292 (IQR = $7,245-$14,699) in PharMetrics. The cost PPPM during the 6-month pre-index period was $2,643 (IQR = $850-$4,357) in MarketScan and $2,742 (IQR = $1,484-$4,730) in PharMetrics.
CONCLUSIONS: Patients were treated mainly with abiraterone across most lines of care, with radium-223, cabazitaxel, and mitoxantrone as the least utilized therapies. Median costs PPPM increased by approximately $8,900 after initiation of FDA-approved agents for mCRPC, with the largest increase in cost stemming from oral medications.
DISCLOSURES: Funding for this study was provided by Bayer HealthCare Pharmaceuticals. All authors were employees at Bayer HealthCare Pharmaceuticals at the time this study was conducted. This study was presented as a poster at the 2017 American Society of Clinical Oncology (ASCO) Genitourinary Cancers Symposium; February 16-18, 2017; Orlando, FL.
OBJECTIVE: To describe treatment patterns and health care costs in prostate cancer (PC) patients with bone metastases treated with agents approved by the FDA for mCRPC.
METHODS: 2 large integrated claims databases (MarketScan and PharMetrics) were used to identify males aged ≥ 18 years who were diagnosed and treated for PC (ICD-9-CM code 185.xx or 233.4) with bone metastases (ICD-9-CM code 198.5) from June 2013 to September 2014. Patients were required to be continuously enrolled for ≥ 6 months before and after initiation of treatment with abiraterone, cabazitaxel, docetaxel, enzalutamide, mitoxantrone, radium-223, sipuleucel-T, or other chemotherapy. Study endpoints included lines of therapy, health care resource utilization per patient per month (PPPM), PPPM costs, and mortality rate. Descriptive analysis was completed for the study sample, and survival function was calculated via Kaplan-Meier estimates.
RESULTS: There were 953 patients meeting all inclusion criteria in the MarketScan database and 565 patients in the PharMetrics database. The median follow-up time was 18 months (interquartile range [IQR] = 14-23) for MarketScan and 14 months (IQR = 11-18) for PharMetrics. Mean age (SD) was 71 (± 10.7) and 66 (± 9.3) years, respectively. Before mCRPC treatment initiation, patients received palliative radiation therapy and bone antiresorptive therapy. For MarketScan and PharMetrics, respectively, 14.0% and 18.2% of patients received radiation therapy, 36.1% and 40.0% received denosumab; 16.5% and 16.8% received zoledronic acid; and 0.2% and 0.8% received pamidronate. Across both databases, abiraterone was the most commonly received bone metastasis treatment agent across all lines of therapy, except fourth line. Radium-223, cabazitaxel, and mitoxantrone were the least utilized therapies. The median cost PPPM during the post-index period was $10,916 (IQR=$5,334-$13,457) in MarketScan and $10,292 (IQR = $7,245-$14,699) in PharMetrics. The cost PPPM during the 6-month pre-index period was $2,643 (IQR = $850-$4,357) in MarketScan and $2,742 (IQR = $1,484-$4,730) in PharMetrics.
CONCLUSIONS: Patients were treated mainly with abiraterone across most lines of care, with radium-223, cabazitaxel, and mitoxantrone as the least utilized therapies. Median costs PPPM increased by approximately $8,900 after initiation of FDA-approved agents for mCRPC, with the largest increase in cost stemming from oral medications.
DISCLOSURES: Funding for this study was provided by Bayer HealthCare Pharmaceuticals. All authors were employees at Bayer HealthCare Pharmaceuticals at the time this study was conducted. This study was presented as a poster at the 2017 American Society of Clinical Oncology (ASCO) Genitourinary Cancers Symposium; February 16-18, 2017; Orlando, FL.
Haykal T, Sundus S, Bachuwa G, Danish R
Primary isolated hepatosplenic sarcoidosis mimicking malignancy and causing symptomatic hypercalcaemia.
BMJ Case Rep. 2019; 12(1) [PubMed] Related Publications
Primary isolated hepatosplenic sarcoidosis mimicking malignancy and causing symptomatic hypercalcaemia.
BMJ Case Rep. 2019; 12(1) [PubMed] Related Publications
This is a case of a 67-year-old woman, known to have multiple medical problems, mainly papillary thyroid cancer status post-total thyroidectomy and cervical neck dissection in addition to radioactive iodine currently in remission for 1 year, who presented to the hospital with severe weakness and fatigue. The initial workup showed significant hypercalcaemia and suppressed Parathyroid hormone (PTH). The patient was treated with hydration and pamidronate and her hypercalcaemia and symptoms improved. The differential was wide, however, a CT scan of the chest, abdomen and pelvis did show multiple liver and splenic nodular lesions; therefore, malignancy was the highest possible diagnosis. Biopsy of the splenic lesion confirmed the diagnosis of sarcoidosis. Therefore, the patient was diagnosed with primary isolated nodular hepatosplenic sarcoidosis mimicking malignancy and causing significant symptomatic hypercalcaemia.
Yan Y, Gao X, Zhang S, et al.
A Carboxyl-Terminated Dendrimer Enables Osteolytic Lesion Targeting and Photothermal Ablation of Malignant Bone Tumors.
ACS Appl Mater Interfaces. 2019; 11(1):160-168 [PubMed] Related Publications
A Carboxyl-Terminated Dendrimer Enables Osteolytic Lesion Targeting and Photothermal Ablation of Malignant Bone Tumors.
ACS Appl Mater Interfaces. 2019; 11(1):160-168 [PubMed] Related Publications
Malignant bone tumor accompanied by tumor-associated osteolysis remains a challenging task in clinical practice. Nanomedicines engineered with bone-targeting ligands, such as alendronate and pamidronate, are developed for targeted delivery of therapeutic agents to bone tumors. However, these targeting strategies usually show relatively poor selectivity toward the healthy skeletons and the osteolytic lesions because of the high binding affinity of bisphosphonates with all the bone tissues. Here, we reported a carboxyl-terminated dendrimer as the candidate to preferentially deliver therapeutic nanoparticles to the osteolytic lesions in a malignant bone tumor model. The high density of carboxyl groups on dendrimer surface endow the polymer with natural bone-binding capability. The dendrimer encapsulated with platinum nanoparticle predominantly accumulates at the osteolytic lesions around bone tumors rather than at healthy bone tissues in vivo. The therapeutic experiments reveal that the dendrimer-mediated photothermal therapy efficiently suppresses bone tumors and osteolysis, and the anionic polymer exhibits minimal cytotoxicity and hematologic toxicity. The results suggest that the carboxyl-terminated dendrimer is a promising candidate for selective delivery of therapeutics to the osteolytic lesions and photothermal treatment of malignant bone tumors.
Kanellias N, Gavriatopoulou M, Terpos E, Dimopoulos MA
Management of multiple myeloma bone disease: impact of treatment on renal function.
Expert Rev Hematol. 2018; 11(11):881-888 [PubMed] Related Publications
Management of multiple myeloma bone disease: impact of treatment on renal function.
Expert Rev Hematol. 2018; 11(11):881-888 [PubMed] Related Publications
INTRODUCTION: Bone disease (BD) is one of the most common features of multiple myeloma. Seventy to eighty percent of patients at diagnosis present with lytic lesions which may lead to skeletal-related events. Areas covered: The aim of this review is to present the possible adverse profile of bisphosphonates (BPs) on renal function, the underlying mechanisms by which BPs may affect renal function and the novel therapeutic approaches on myeloma bone disease management. Expert commentary: BPs remain the cornerstone in the management of myeloma-related BD. Zoledronic acid and Pamidronate are currently the gold standard, however cannot be used in patients with severe renal dysfunction. Renal impairment is another hallmark of myeloma with approximately 60% of the patients presenting with or developing renal dysfunction during the disease course. Although BPs rarely cause renal impairment, they should be administered with caution in patients with impaired renal function. The exact mechanism by which BPs cause renal impairment is yet to be elucidated. Another promising agent is denosumab, a RANKL inhibitor, which can be administrated regardless of renal function and does not need the relevant dose-adjustments.
Mahmoud S, Mitwally H, El Zeer HS, et al.
Use of Pamidronate to Treat Hypercalcemia in an Oncology Dialysis Patient: A Case Report.
Am J Case Rep. 2018; 19:1087-1089 [PubMed] Free Access to Full Article Related Publications
Use of Pamidronate to Treat Hypercalcemia in an Oncology Dialysis Patient: A Case Report.
Am J Case Rep. 2018; 19:1087-1089 [PubMed] Free Access to Full Article Related Publications
BACKGROUND Hypercalcemia is a common complication in the intensive care unit (ICU). It can be a result of diverse etiologies, such as malignancy. In this case, bisphosphonates can serve as an effective therapeutic option. However, bisphosphonates are not safe to use in patients with end stage renal disease. CASE REPORT We report a case of severe hypercalcemia possibly secondary to bone metastasis. The patient is known to have end-stage renal disease (ESRD) and undergoing dialysis 3 times a week. She had severe persistent hypercalcemia which did not resolve with regular measures or calcitonin. The literature was searched for the possibility of administering bisphosphonate as a treatment option. It was found that pamidronate pharmacokinetics can be safe and effective in end-stage renal disease patients. Therefore, Pamidronate was administered, showing effective results with regards to the level of calcium and no observed adverse effects. Re-dosing was required at an 8-week interval, with no adverse effects. CONCLUSIONS Pamidronate is a safe option to use in treating hypercalcemia in end-stage renal disease patients on dialysis. This can be especially beneficial in patients with sustained hypercalcemia secondary to malignancy.
Wazzan T, Kashtwari D, Almaden WF, et al.
Radiographic bone loss and the risk of medication-related osteonecrosis of the jaw (MRONJ) in multiple myeloma patients-A retrospective case control study.
Spec Care Dentist. 2018; 38(6):356-361 [PubMed] Related Publications
Radiographic bone loss and the risk of medication-related osteonecrosis of the jaw (MRONJ) in multiple myeloma patients-A retrospective case control study.
Spec Care Dentist. 2018; 38(6):356-361 [PubMed] Related Publications
Risk factors for medication-related osteonecrosis of the jaws (MRONJ) include type and duration of antiresorptive drugs, dental trauma, local anatomy, systemic underlying conditions and therapy, smoking, and the presence of periodontal disease. However, there is a lack of studies elucidating the role of periodontal disease as risk predictor. In the present study, the dental charts of 100 multiple myeloma (MM) patients and 16 MM patients who developed MRONJ were studied. Information about age, gender, smoking history, diabetes, steroid drug intake, type and duration of bisphosphonate (BP) treatments, MRONJ status, missing teeth, periapical lesions, widening of the periodontal ligament, and periodontal status was collected. The periodontal status was determined as a percentage of missing bone at the mesial and distal surfaces of each tooth. Multivariable logistic regression was performed to identify risk factors associated with MRONJ. In the selected model, using the COX analysis, categorical bone loss percentage is significantly associated with MRONJ (P = 0.009), with hazard ratio 0.042 (high vs low) and 95% CI 0.004 to 0.453. Gender, steroid, Aredia BP type, and periapical are also significant in selected model. In conclusion, advanced alveolar bone loss and missing teeth were strongly related to the occurrence of MRONJ in MM patients.
Zain MA, Raza A, Hanif MO, et al.
Double Trouble - Severe Hypernatremia Secondary to Central Diabetes Insipidus Complicated by Hypercalcemic Nephrogenic Diabetes Insipidus: A Case Report.
Am J Case Rep. 2018; 19:973-977 [PubMed] Free Access to Full Article Related Publications
Double Trouble - Severe Hypernatremia Secondary to Central Diabetes Insipidus Complicated by Hypercalcemic Nephrogenic Diabetes Insipidus: A Case Report.
Am J Case Rep. 2018; 19:973-977 [PubMed] Free Access to Full Article Related Publications
BACKGROUND Patients with malignancies often have electrolyte abnormalities. We present a case of a patient with central diabetes insipidus secondary to metastatic pituitary invasion complicated by hypercalcemic nephrogenic diabetes insipidus. CASE REPORT We present a case of 40-year-old female with a history of stage IV breast cancer with skeletal and leptomeningeal metastasis, who was admitted with polyuria, polydipsia, and recent onset of confusion. The patient was found to have profound hypernatremia and severe hypercalcemia with normal parathyroid and vitamin D serum levels. Urine studies showed low urine osmolality and high urine output, despite the higher serum osmolality. The patient received 5% dextrose for rehydration, 1 dose of intravenous (IV) pamidronate, 1 dose of IV desmopressin, and 4 days of subcutaneous calcitonin 200 international units Q12H. Initially, her urine output in the hospital was in the range of 350-400 milliliters/hour, which responded well to 1 dose of 1-desamino-8d-arginine vasopressin (DDAVP). In the subsequent days, her confusion resolved with normalization of serum sodium and calcium, but she died because of the extensive malignancy. CONCLUSIONS Our case emphasizes the importance of identification of causes and complications of electrolyte abnormalities associated with metastatic cancers. These electrolyte abnormalities can be primary or paraneoplastic and should be actively pursued and treated in such cases.
Basok AB, Rogachev B, Haviv YS, Vorobiov M
Treatment of extreme hypercalcaemia: the role of haemodialysis.
BMJ Case Rep. 2018; 2018 [PubMed] Free Access to Full Article Related Publications
Treatment of extreme hypercalcaemia: the role of haemodialysis.
BMJ Case Rep. 2018; 2018 [PubMed] Free Access to Full Article Related Publications
A patient with extremely high calcium level of 23.9 mg/dL (5.97 mmol/L) was admitted to our department unconscious with pathological ECG recording, demonstrating shortening of QT interval. The patient was treated by fluid resuscitation, bisphosphonates, salmon calcitonin and steroids. Haemodialysis with low calcium bath had been promptly provided with improvement of consciousness and calcium level. ECG changes disappeared. Subsequent investigations revealed hyperparathyroidism and a large parathyroid adenoma was then surgically removed. Extreme and rapid calcium elevation (parathyroid crisis) is rarely seen in primary hyperparathyroidism and usually is distinctive for malignancy. In the context of acute kidney injury and refractory hypercalcaemia with life-threatening complications (coma, ECG changes with impending danger of arrhythmia), haemodialysis may effectively decrease calcium levels. It should be pointed out that dialysis is an efficient method of treatment of refractory hypercalcaemia, parathyroid crisis, but it is rarely used due to its invasive nature.
Owosho AA, Liang STY, Sax AZ, et al.
Medication-related osteonecrosis of the jaw: An update on the memorial sloan kettering cancer center experience and the role of premedication dental evaluation in prevention.
Oral Surg Oral Med Oral Pathol Oral Radiol. 2018; 125(5):440-445 [PubMed] Related Publications
Medication-related osteonecrosis of the jaw: An update on the memorial sloan kettering cancer center experience and the role of premedication dental evaluation in prevention.
Oral Surg Oral Med Oral Pathol Oral Radiol. 2018; 125(5):440-445 [PubMed] Related Publications
OBJECTIVE: The aim of this study was to investigate the relationship between type of antiresorptive medication and medication-related osteonecrosis of the jaw (MRONJ) onset and the role of premedication dental evaluation (PMDE) in the prevention of MRONJ.
STUDY DESIGN: Our database of patients with MRONJ was reviewed. The Kruskal-Wallis test was used to analyze the onset dose of the 3 frequent medication types associated with MRONJ. To evaluate the role of PMDE in the prevention of MRONJ, all patients on antiresorptive and/or antiangiogenic medications seen in the Dental Service of Memorial Sloan Kettering Cancer Center during a 10-year period were subclassified into 2 groups. Group I comprised patients seen for PMDE before the commencement of A/A and group II patients seen after prior exposure to antiresorptive and/or antiangiogenic medications. Fischer's exact test was used to compare the incidence of MRONJ in both groups.
RESULTS: Patients on denosumab developed MRONJ earlier compared with zoledronate and pamidronate (P = .003). Group I had a significantly reduced incidence of MRONJ (0.9%) compared with group II (10.5%) (P < .0001). Dentoalveolar trauma as a precipitating factor between groups I and II was not statistically significant.
CONCLUSIONS: Denosumab was associated with an earlier occurrence of MRONJ compared with zoledronate and pamidronate. The role of PMDE may be an effective preventive strategy in reducing the incidence of MRONJ.
STUDY DESIGN: Our database of patients with MRONJ was reviewed. The Kruskal-Wallis test was used to analyze the onset dose of the 3 frequent medication types associated with MRONJ. To evaluate the role of PMDE in the prevention of MRONJ, all patients on antiresorptive and/or antiangiogenic medications seen in the Dental Service of Memorial Sloan Kettering Cancer Center during a 10-year period were subclassified into 2 groups. Group I comprised patients seen for PMDE before the commencement of A/A and group II patients seen after prior exposure to antiresorptive and/or antiangiogenic medications. Fischer's exact test was used to compare the incidence of MRONJ in both groups.
RESULTS: Patients on denosumab developed MRONJ earlier compared with zoledronate and pamidronate (P = .003). Group I had a significantly reduced incidence of MRONJ (0.9%) compared with group II (10.5%) (P < .0001). Dentoalveolar trauma as a precipitating factor between groups I and II was not statistically significant.
CONCLUSIONS: Denosumab was associated with an earlier occurrence of MRONJ compared with zoledronate and pamidronate. The role of PMDE may be an effective preventive strategy in reducing the incidence of MRONJ.
Kieser DC, Mazas S, Cawley DT, et al.
Bisphosphonate therapy for spinal aneurysmal bone cysts.
Eur Spine J. 2018; 27(4):851-858 [PubMed] Related Publications
Bisphosphonate therapy for spinal aneurysmal bone cysts.
Eur Spine J. 2018; 27(4):851-858 [PubMed] Related Publications
PURPOSE: To assess the efficacy of bisphosphonate therapy in the management of spinal aneurysmal bone cysts (ABCs).
METHODS: A prospective study of six consecutive patients aged between 7 and 22 years with spinal ABCs treated with pamidronate (1 mg/kg) or zoledronate (4 mg). A visual analogue scale (VAS) for pain and radiological (contrast-enhanced MRI and CT scan at 3 and 6 months, then yearly X-rays) follow-up was continued for a minimum of 6 years.
RESULTS: One patient with an unstable C2/3 failed to respond to a single dose of bisphosphonate and required surgical resection and stabilisation with autologous bone grafting. Another, with a thoraco-lumbar ABC, experienced progression of neurological dysfunction after one cycle of bisphosphonate and, therefore, required surgical resection and stabilisation. In all other patients pain progressively improved and was resolved after two to four cycles (VAS 7.3-0). These patients all showed reduction in peri-lesional oedema and increased ossification by 3 months. No patients have had a recurrence within the timeframe of this study.
CONCLUSIONS: Bisphosphonate therapy can be used as the definitive treatment of spinal ABCs, except in patients with instability or progressive neurology, where surgical intervention is required. Clinicians should expect a patients symptoms to rapidly improve, their bone oedema to resolve by 3 months and their lesion to partially or completely ossify by 6-12 months.
METHODS: A prospective study of six consecutive patients aged between 7 and 22 years with spinal ABCs treated with pamidronate (1 mg/kg) or zoledronate (4 mg). A visual analogue scale (VAS) for pain and radiological (contrast-enhanced MRI and CT scan at 3 and 6 months, then yearly X-rays) follow-up was continued for a minimum of 6 years.
RESULTS: One patient with an unstable C2/3 failed to respond to a single dose of bisphosphonate and required surgical resection and stabilisation with autologous bone grafting. Another, with a thoraco-lumbar ABC, experienced progression of neurological dysfunction after one cycle of bisphosphonate and, therefore, required surgical resection and stabilisation. In all other patients pain progressively improved and was resolved after two to four cycles (VAS 7.3-0). These patients all showed reduction in peri-lesional oedema and increased ossification by 3 months. No patients have had a recurrence within the timeframe of this study.
CONCLUSIONS: Bisphosphonate therapy can be used as the definitive treatment of spinal ABCs, except in patients with instability or progressive neurology, where surgical intervention is required. Clinicians should expect a patients symptoms to rapidly improve, their bone oedema to resolve by 3 months and their lesion to partially or completely ossify by 6-12 months.
Anderson K, Ismaila N, Flynn PJ, et al.
Role of Bone-Modifying Agents in Multiple Myeloma: American Society of Clinical Oncology Clinical Practice Guideline Update.
J Clin Oncol. 2018; 36(8):812-818 [PubMed] Related Publications
Role of Bone-Modifying Agents in Multiple Myeloma: American Society of Clinical Oncology Clinical Practice Guideline Update.
J Clin Oncol. 2018; 36(8):812-818 [PubMed] Related Publications
Purpose To update guideline recommendations on the role of bone-modifying agents in multiple myeloma. Methods An update panel conducted a targeted systematic literature review by searching PubMed and the Cochrane Library for randomized controlled trials, systematic reviews, meta-analyses, clinical practice guidelines, and observational studies. Results Thirty-five relevant studies were identified, and updated evidence supports the current recommendations. Recommendations For patients with active symptomatic multiple myeloma that requires systemic therapy with or without evidence of lytic destruction of bone or compression fracture of the spine from osteopenia on plain radiograph(s) or other imaging studies, intravenous administration of pamidronate 90 mg over at least 2 hours or zoledronic acid 4 mg over at least 15 minutes every 3 to 4 weeks is recommended. Denosumab has shown to be noninferior to zoledronic acid for the prevention of skeletal-related events and provides an alternative. Fewer adverse events related to renal toxicity have been noted with denosumab compared with zoledronic acid and may be preferred in this setting. The update panel recommends that clinicians consider reducing the initial pamidronate dose in patients with preexisting renal impairment. Zoledronic acid has not been studied in patients with severe renal impairment and is not recommended in this setting. The update panel suggests that bone-modifying treatment continue for up to 2 years. Less frequent dosing has been evaluated and should be considered in patients with responsive or stable disease. Continuous use is at the discretion of the treating physician and the risk of ongoing skeletal morbidity. Retreatment should be initiated at the time of disease relapse. The update panel discusses measures regarding osteonecrosis of the jaw. Additional information is available at www.asco.org/hematologic-malignancies-guidelines and www.asco.org/guidelineswiki .
Schiodt M, Vadhan-Raj S, Chambers MS, et al.
A multicenter case registry study on medication-related osteonecrosis of the jaw in patients with advanced cancer.
Support Care Cancer. 2018; 26(6):1905-1915 [PubMed] Free Access to Full Article Related Publications
A multicenter case registry study on medication-related osteonecrosis of the jaw in patients with advanced cancer.
Support Care Cancer. 2018; 26(6):1905-1915 [PubMed] Free Access to Full Article Related Publications
PURPOSE: This observational case registry study was designed to describe the natural history of cancer patients with medication-related osteonecrosis of the jaw (ONJ) and evaluate the ONJ resolution rate.
METHODS: Adults with a diagnosis of cancer and with a new diagnosis of ONJ were enrolled and evaluated by a dental specialist at baseline and every 3 months for 2 years and then every 6 months for 3 years until death, consent withdrawal, or loss to follow-up. The primary endpoint was the rate and time course of ONJ resolution. Secondary endpoints included frequency of incident ONJ risk factors, ONJ treatment patterns, and treatment patterns of antiresorptive agents for subsequent ONJ.
RESULTS: Overall, 327 patients were enrolled; 207 (63%) were continuing on study at data cutoff. Up to 69% of evaluable patients with ONJ had resolution or improvement during the study. ONJ resolution (AAOMS ONJ staging criteria) was observed in 114 patients (35%); median (interquartile range) time from ONJ onset to resolution was 7.3 (4.5-11.4) months. Most patients (97%) had received antiresorptive medication before ONJ development, 9 patients (3%) had not; 68% had received zoledronic acid, 38% had received denosumab, and 10% had received pamidronate (56% had received bisphosphonates only, 18% had received denosumab only, and 21% had exposure to both).
CONCLUSIONS: These results are consistent with those observed in clinical trials evaluating skeletal-related events in patients with advanced malignancy involving bone. Longer follow-up will provide further information on ONJ recurrence and resolution rates between medically and surgically managed patients.
METHODS: Adults with a diagnosis of cancer and with a new diagnosis of ONJ were enrolled and evaluated by a dental specialist at baseline and every 3 months for 2 years and then every 6 months for 3 years until death, consent withdrawal, or loss to follow-up. The primary endpoint was the rate and time course of ONJ resolution. Secondary endpoints included frequency of incident ONJ risk factors, ONJ treatment patterns, and treatment patterns of antiresorptive agents for subsequent ONJ.
RESULTS: Overall, 327 patients were enrolled; 207 (63%) were continuing on study at data cutoff. Up to 69% of evaluable patients with ONJ had resolution or improvement during the study. ONJ resolution (AAOMS ONJ staging criteria) was observed in 114 patients (35%); median (interquartile range) time from ONJ onset to resolution was 7.3 (4.5-11.4) months. Most patients (97%) had received antiresorptive medication before ONJ development, 9 patients (3%) had not; 68% had received zoledronic acid, 38% had received denosumab, and 10% had received pamidronate (56% had received bisphosphonates only, 18% had received denosumab only, and 21% had exposure to both).
CONCLUSIONS: These results are consistent with those observed in clinical trials evaluating skeletal-related events in patients with advanced malignancy involving bone. Longer follow-up will provide further information on ONJ recurrence and resolution rates between medically and surgically managed patients.
Mhaskar R, Kumar A, Miladinovic B, Djulbegovic B
Bisphosphonates in multiple myeloma: an updated network meta-analysis.
Cochrane Database Syst Rev. 2017; 12:CD003188 [PubMed] Free Access to Full Article Related Publications
Bisphosphonates in multiple myeloma: an updated network meta-analysis.
Cochrane Database Syst Rev. 2017; 12:CD003188 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Bisphosphonates are specific inhibitors of osteoclastic activity and are used in the treatment of patients with multiple myeloma (MM). While bisphosphonates are shown to be effective in reducing vertebral fractures and pain, their role in improving overall survival (OS) remains unclear. This is an update of a Cochrane review first published in 2002 and previously updated in 2010 and 2012.
OBJECTIVES: To assess the evidence related to benefits and harms associated with use of various types of bisphosphonates (aminobisphosphonates versus non-aminobisphosphonates) in the management of patients with MM. Our primary objective was to determine whether adding bisphosphonates to standard therapy in MM improves OS and progression-free survival (PFS), and decreases skeletal-related morbidity. Our secondary objectives were to determine the effects of bisphosphonates on pain, quality of life, incidence of hypercalcemia, incidence of bisphosphonate-related gastrointestinal toxicities, osteonecrosis of jaw (ONJ) and hypocalcemia.
SEARCH METHODS: We searched MEDLINE, Embase (September 2011 to July 2017) and the CENTRAL (2017, Issue 7) to identify all randomized controlled trial (RCT) in MM up to July 2017 using a combination of text and MeSH terms.
SELECTION CRITERIA: Any randomized controlled trial (RCT) comparing bisphosphonates versus placebo/no treatment/bisphosphonates and observational studies or case reports examining bisphosphonate-related ONJ in patients with MM were eligible for inclusion.
DATA COLLECTION AND ANALYSIS: Two review authors extracted the data. Data were pooled and reported as hazard ratio (HR) or risk ratio (RR) using a random-effects model. We used meta-regression to explore statistical heterogeneity. Network meta-analysis using Bayesian approach was conducted.
MAIN RESULTS: In this update, we included four new studies (601 participants), resulting in a total of 24 included studies.Twenty RCTs compared bisphosphonates with either placebo or no treatment and four RCTs involved another bisphosphonate as a comparator. The 24 included RCTs enrolled 7293 participants. Pooled results showed that there was moderate-quality evidence of a reduction in mortality with on OS from 41% to 31%, but the confidence interval is consistent with a larger reduction and small increase in mortality compared with placebo or no treatment (HR 0.90, 95% CI 0.76 to 1.07; 14 studies; 2706 participants). There was substantial heterogeneity among the included RCTs (I
AUTHORS' CONCLUSIONS: Use of bisphosphonates in participants with MM reduces pathological vertebral fractures, SREs and pain. Bisphosphonates were associated with an increased risk of developing ONJ. For every 1000 participants treated with bisphosphonates, about one patient will suffer from the ONJ. We found no evidence of superiority of any specific aminobisphosphonate (zoledronate, pamidronate or ibandronate) or non-aminobisphosphonate (etidronate or clodronate) for any outcome. However, zoledronate was found to be better than placebo and first-generation bisposphonate (etidronate) in pooled direct and indirect analyses for improving OS and other outcomes such as vertebral fractures. Direct head-to-head trials of the second-generation bisphosphonates are needed to settle the issue if zoledronate is truly the most efficacious bisphosphonate currently used in practice.
OBJECTIVES: To assess the evidence related to benefits and harms associated with use of various types of bisphosphonates (aminobisphosphonates versus non-aminobisphosphonates) in the management of patients with MM. Our primary objective was to determine whether adding bisphosphonates to standard therapy in MM improves OS and progression-free survival (PFS), and decreases skeletal-related morbidity. Our secondary objectives were to determine the effects of bisphosphonates on pain, quality of life, incidence of hypercalcemia, incidence of bisphosphonate-related gastrointestinal toxicities, osteonecrosis of jaw (ONJ) and hypocalcemia.
SEARCH METHODS: We searched MEDLINE, Embase (September 2011 to July 2017) and the CENTRAL (2017, Issue 7) to identify all randomized controlled trial (RCT) in MM up to July 2017 using a combination of text and MeSH terms.
SELECTION CRITERIA: Any randomized controlled trial (RCT) comparing bisphosphonates versus placebo/no treatment/bisphosphonates and observational studies or case reports examining bisphosphonate-related ONJ in patients with MM were eligible for inclusion.
DATA COLLECTION AND ANALYSIS: Two review authors extracted the data. Data were pooled and reported as hazard ratio (HR) or risk ratio (RR) using a random-effects model. We used meta-regression to explore statistical heterogeneity. Network meta-analysis using Bayesian approach was conducted.
MAIN RESULTS: In this update, we included four new studies (601 participants), resulting in a total of 24 included studies.Twenty RCTs compared bisphosphonates with either placebo or no treatment and four RCTs involved another bisphosphonate as a comparator. The 24 included RCTs enrolled 7293 participants. Pooled results showed that there was moderate-quality evidence of a reduction in mortality with on OS from 41% to 31%, but the confidence interval is consistent with a larger reduction and small increase in mortality compared with placebo or no treatment (HR 0.90, 95% CI 0.76 to 1.07; 14 studies; 2706 participants). There was substantial heterogeneity among the included RCTs (I
AUTHORS' CONCLUSIONS: Use of bisphosphonates in participants with MM reduces pathological vertebral fractures, SREs and pain. Bisphosphonates were associated with an increased risk of developing ONJ. For every 1000 participants treated with bisphosphonates, about one patient will suffer from the ONJ. We found no evidence of superiority of any specific aminobisphosphonate (zoledronate, pamidronate or ibandronate) or non-aminobisphosphonate (etidronate or clodronate) for any outcome. However, zoledronate was found to be better than placebo and first-generation bisposphonate (etidronate) in pooled direct and indirect analyses for improving OS and other outcomes such as vertebral fractures. Direct head-to-head trials of the second-generation bisphosphonates are needed to settle the issue if zoledronate is truly the most efficacious bisphosphonate currently used in practice.
Qian Y, Bhowmik D, Kachru N, et al.
Utilization of agents to prevent skeletal-related events among patients with multiple myeloma: analysis of real-world data.
Support Care Cancer. 2018; 26(3):807-812 [PubMed] Related Publications
Utilization of agents to prevent skeletal-related events among patients with multiple myeloma: analysis of real-world data.
Support Care Cancer. 2018; 26(3):807-812 [PubMed] Related Publications
PURPOSE: This study examined real-world utilization patterns of bone-targeted agents (BTA) in patients with multiple myeloma (MM).
METHODS: In this retrospective cohort study, adults with an MM diagnosis recorded in 2012-2014 were identified from electronic health records in the Oncology Services Comprehensive Electronic Records (OSCER) database. Patients received zoledronic acid (ZA) or pamidronate (PA) on/after first MM diagnosis recorded in the study period, had no BTA use in prior 6 months, and were followed through earliest of May 31, 2015 or last clinic visit. Patients with any solid tumor diagnosis were excluded. Time to BTA initiation, compliance (≥ 12 administrations in a year), switching, and non-persistence (switch or ≥ 90-day gap in therapy) were described by agent and follow-up period.
RESULTS: Among 9,617 patients with MM, 3,735 (38.8%) received a BTA. Most patients (90.9%) received ZA, with first BTA use generally seen within 3 months of first observed MM diagnosis (ZA 76.1%, PA 75.1%). A minority of ZA (27.4%) and PA (23.0%) patients were compliant in Year 1, with lower compliance in Year 2 (19.8% and 15.6%, respectively). The median time to non-persistence was 16.2 (95% confidence interval [CI] 15.4-17.4) months for ZA and 13.8 (95% CI 11.5-15.4) months for PA. Persistence was 86% at 6 months and 34% at 24 months for ZA, and 77% and 30% for PA, respectively.
CONCLUSIONS: These results highlight the possibility of suboptimal prevention of skeletal-related events due to non-compliant dosing and non-persistence after patients initiate BTA therapy.
METHODS: In this retrospective cohort study, adults with an MM diagnosis recorded in 2012-2014 were identified from electronic health records in the Oncology Services Comprehensive Electronic Records (OSCER) database. Patients received zoledronic acid (ZA) or pamidronate (PA) on/after first MM diagnosis recorded in the study period, had no BTA use in prior 6 months, and were followed through earliest of May 31, 2015 or last clinic visit. Patients with any solid tumor diagnosis were excluded. Time to BTA initiation, compliance (≥ 12 administrations in a year), switching, and non-persistence (switch or ≥ 90-day gap in therapy) were described by agent and follow-up period.
RESULTS: Among 9,617 patients with MM, 3,735 (38.8%) received a BTA. Most patients (90.9%) received ZA, with first BTA use generally seen within 3 months of first observed MM diagnosis (ZA 76.1%, PA 75.1%). A minority of ZA (27.4%) and PA (23.0%) patients were compliant in Year 1, with lower compliance in Year 2 (19.8% and 15.6%, respectively). The median time to non-persistence was 16.2 (95% confidence interval [CI] 15.4-17.4) months for ZA and 13.8 (95% CI 11.5-15.4) months for PA. Persistence was 86% at 6 months and 34% at 24 months for ZA, and 77% and 30% for PA, respectively.
CONCLUSIONS: These results highlight the possibility of suboptimal prevention of skeletal-related events due to non-compliant dosing and non-persistence after patients initiate BTA therapy.
Van Poznak C, Somerfield MR, Barlow WE, et al.
Role of Bone-Modifying Agents in Metastatic Breast Cancer: An American Society of Clinical Oncology-Cancer Care Ontario Focused Guideline Update.
J Clin Oncol. 2017; 35(35):3978-3986 [PubMed] Related Publications
Role of Bone-Modifying Agents in Metastatic Breast Cancer: An American Society of Clinical Oncology-Cancer Care Ontario Focused Guideline Update.
J Clin Oncol. 2017; 35(35):3978-3986 [PubMed] Related Publications
Purpose To update, in collaboration with Cancer Care Ontario (CCO), key recommendations of the American Society of Clinical Oncology (ASCO) guideline on the role of bone-modifying agents (BMAs) in metastatic breast cancer. This focused update addressed the new data on intervals between dosing and the role of BMAs in control of bone pain. Methods A joint ASCO-CCO Update Committee conducted targeted systematic literature reviews to identify relevant studies. Results The Update Committee reviewed three phase III noninferiority trials of dosing intervals, one systematic review and meta-analysis of studies of de-escalation of BMAs, and two randomized trials of BMAs in control of pain secondary to bone metastases. Recommendations Patients with breast cancer who have evidence of bone metastases should be treated with BMAs. Options include denosumab, 120 mg subcutaneously, every 4 weeks; pamidronate, 90 mg intravenously, every 3 to 4 weeks; or zoledronic acid, 4 mg intravenously every 12 weeks or every 3 to 4 weeks. The analgesic effects of BMAs are modest, and they should not be used alone for bone pain. The Update Committee recommends that the current standard of care for supportive care and pain management-analgesia, adjunct therapies, radiotherapy, surgery, systemic anticancer therapy, and referral to supportive care and pain management-be applied. Evidence is insufficient to support the use of one BMA over another. Additional information is available at www.asco.org/breast-cancer-guidelines and www.asco.org/guidelineswiki .
Bousson V, Leturcq T, Ea HK, et al.
An open-label, prospective, observational study of the efficacy of bisphosphonate therapy for painful osteoid osteoma.
Eur Radiol. 2018; 28(2):478-486 [PubMed] Related Publications
An open-label, prospective, observational study of the efficacy of bisphosphonate therapy for painful osteoid osteoma.
Eur Radiol. 2018; 28(2):478-486 [PubMed] Related Publications
OBJECTIVES: To assess the efficacy of bisphosphonate therapy on bone pain in patients with osteoid osteoma (OO) (main objective), and to describe bisphosphonate-induced changes in nidus mineralisation and regional bone-marrow oedema (BMO).
METHODS: A prospective, observational study was conducted from 2011 to 2014. Patients with risk factors for complications of percutaneous or surgical ablation or recurrence after ablation, were offered once monthly intravenous bisphosphonate treatment until significant pain alleviation was achieved.
RESULTS: We included 23 patients. The first two patients received pamidronate and the next 21 zoledronic acid (mean, 2.95 infusions per patient). Bisphosphonate therapy was successful in 19 patients (83%), whose mean pain visual analogue scale score decreased by 76.7%; this pain-relieving effect persisted in 17 patients (74%) with a mean follow-up time of 36 months. Computed tomography (CT) demonstrated a mean nidus density increase of 177.7% (p = 0.001). By magnetic resonance imaging (MRI), mean decreases were 38.4% for BMO surface area and 30.3% for signal intensity (p = 0.001 and p = 0.000, respectively).
CONCLUSIONS: In 17/23 patients with painful OO managed conservatively with bisphosphonates, long-term final success was achieved. Bisphosphonates may accelerate the spontaneous healing of OO.
KEY POINTS: • 19/23 patients with OO managed with bisphosphonates experienced significant pain relief • Pain relief was sustained in 17/23 patients, mean follow-up of 36 months • CT demonstrated a significant increase in nidus mineralisation • MRI demonstrated a significant decrease in bone marrow oedema • Bisphosphonate therapy may accelerate the spontaneous healing of OO.
METHODS: A prospective, observational study was conducted from 2011 to 2014. Patients with risk factors for complications of percutaneous or surgical ablation or recurrence after ablation, were offered once monthly intravenous bisphosphonate treatment until significant pain alleviation was achieved.
RESULTS: We included 23 patients. The first two patients received pamidronate and the next 21 zoledronic acid (mean, 2.95 infusions per patient). Bisphosphonate therapy was successful in 19 patients (83%), whose mean pain visual analogue scale score decreased by 76.7%; this pain-relieving effect persisted in 17 patients (74%) with a mean follow-up time of 36 months. Computed tomography (CT) demonstrated a mean nidus density increase of 177.7% (p = 0.001). By magnetic resonance imaging (MRI), mean decreases were 38.4% for BMO surface area and 30.3% for signal intensity (p = 0.001 and p = 0.000, respectively).
CONCLUSIONS: In 17/23 patients with painful OO managed conservatively with bisphosphonates, long-term final success was achieved. Bisphosphonates may accelerate the spontaneous healing of OO.
KEY POINTS: • 19/23 patients with OO managed with bisphosphonates experienced significant pain relief • Pain relief was sustained in 17/23 patients, mean follow-up of 36 months • CT demonstrated a significant increase in nidus mineralisation • MRI demonstrated a significant decrease in bone marrow oedema • Bisphosphonate therapy may accelerate the spontaneous healing of OO.
Lee OL, Horvath N, Lee C, et al.
Bisphosphonate guidelines for treatment and prevention of myeloma bone disease.
Intern Med J. 2017; 47(8):938-951 [PubMed] Related Publications
Bisphosphonate guidelines for treatment and prevention of myeloma bone disease.
Intern Med J. 2017; 47(8):938-951 [PubMed] Related Publications
Multiple myeloma (MM) is a haematological malignancy characterised by the clonal proliferation of plasma cells in the bone marrow. More than 80% of patients with MM display evidence of myeloma bone disease (MBD), characterised by the formation of osteolytic lesions throughout the axial and appendicular skeleton. MBD significantly increases the risk of skeletal-related events such as pathologic fracture, spinal cord compression and hypercalcaemia. MBD is the result of MM plasma cells-mediated activation of osteoclast activity and suppression of osteoblast activity. Bisphosphonates (BP), pyrophosphate analogues with high bone affinity, are the only pharmacological agents currently recommended for the treatment and prevention of MBD and remain the standard of care. Pamidronate and zoledronic acid are the most commonly used BP to treat MBD. Although generally safe, frequent high doses of BP are associated with adverse events such as renal toxicity and osteonecrosis of the jaw. As such, optimal duration and dosing of BP therapy is required in order to minimise BP-associated adverse events. The following guidelines provide currently available evidence for the adoption of a tailored approach when using BP for the management of MBD.
Chumbley EM. You're the flight surgeon: a case of bilateral leg pain and swelling in a loadmaster. Aerosp Med Hum Perform. 2017; 88(5):511-515.
Yin Y, Feng L, Zhou L, et al.
Effects of Yishengukang decoction on expression of bone-specific alkaline phosphatase, carboxyterminal propeptide of type Ⅰ procollagen, and carboxyterminal cross-linked telepeptide of type Ⅰ collagen in malignant tumor patients with bone metastasis.
J Tradit Chin Med. 2017; 37(1):30-4 [PubMed] Related Publications
Effects of Yishengukang decoction on expression of bone-specific alkaline phosphatase, carboxyterminal propeptide of type Ⅰ procollagen, and carboxyterminal cross-linked telepeptide of type Ⅰ collagen in malignant tumor patients with bone metastasis.
J Tradit Chin Med. 2017; 37(1):30-4 [PubMed] Related Publications
OBJECTIVE: To investigate the effect of Yishengukang decoction on the expression of the metabolic bone markers, bone-specific alkaline phosphatase (BAP), carboxyterminal propeptide of type Ⅰ procollagen (PICP), and arboxyterminal cross-linked telepeptide of type Ⅰ collagen (ICTP), in cancer patients with bone metastasis.
METHODS: Patients (n = 180) were divided into three groups: (a) bone metastasis patients treated with Yishengukang and pamidronate disodium injection (treatment group, n = 60); (b) bone metastasis patients treated with pamidronate disodium injection alone (control group, n = 60); (c) cancer patients without metastatic bone lesion (non-bone metastasis group, n = 60). Serum levels of the metabolic markers BAP, PICP, and ICTP were detected by enzyme-linked immunosorbent assay pre- and post-therapy.
RESULTS: A significant decrease in serum BAP level was observed in the treatment group compared with the control group. However there were no significant differences in serum levels of PICP and ICTP before or after treatment compared with the control group.
CONCLUSION: Yishengukang decoction combined with pamidronate disodium injection reduced serum BAP level to a greater extent that pamidronate disodium injection alone. Furthermore, the combined therapy was more beneficial in regulating imbalanced bone metabolism after bone metastasis, and may represent the molecular mechanism underpinning the effects of Yishengukang decoction.
METHODS: Patients (n = 180) were divided into three groups: (a) bone metastasis patients treated with Yishengukang and pamidronate disodium injection (treatment group, n = 60); (b) bone metastasis patients treated with pamidronate disodium injection alone (control group, n = 60); (c) cancer patients without metastatic bone lesion (non-bone metastasis group, n = 60). Serum levels of the metabolic markers BAP, PICP, and ICTP were detected by enzyme-linked immunosorbent assay pre- and post-therapy.
RESULTS: A significant decrease in serum BAP level was observed in the treatment group compared with the control group. However there were no significant differences in serum levels of PICP and ICTP before or after treatment compared with the control group.
CONCLUSION: Yishengukang decoction combined with pamidronate disodium injection reduced serum BAP level to a greater extent that pamidronate disodium injection alone. Furthermore, the combined therapy was more beneficial in regulating imbalanced bone metabolism after bone metastasis, and may represent the molecular mechanism underpinning the effects of Yishengukang decoction.
Hortobagyi GN, Van Poznak C, Harker WG, et al.
Continued Treatment Effect of Zoledronic Acid Dosing Every 12 vs 4 Weeks in Women With Breast Cancer Metastatic to Bone: The OPTIMIZE-2 Randomized Clinical Trial.
JAMA Oncol. 2017; 3(7):906-912 [PubMed] Free Access to Full Article Related Publications
Continued Treatment Effect of Zoledronic Acid Dosing Every 12 vs 4 Weeks in Women With Breast Cancer Metastatic to Bone: The OPTIMIZE-2 Randomized Clinical Trial.
JAMA Oncol. 2017; 3(7):906-912 [PubMed] Free Access to Full Article Related Publications
Importance: Zoledronic acid, a potent bisphosphonate, is commonly administered to patients with bone metastases to reduce the risk of skeletal-related events (SREs). However, there have been concerns regarding its long-term monthly administration.
Objective: To examine whether zoledronic acid every 12 weeks was noninferior to zoledronic acid every 4 weeks in patients with metastatic breast cancer that involved the bone who had previously received a standard dosing regimen of zoledronic acid and/or pamidronate disodium.
Design, Setting, and Participants: OPTIMIZE-2 was a prospective, randomized, double-blind, multicenter phase 3 trial of intention-to-treat (full analysis set), evaluable (per protocol), and safety populations. Patients were randomized (1:1) to receive 4.0 mg of intravenous zoledronic acid every 4 or every 12 weeks with placebo for interim infusions for 1 year. The study was conducted at 102 clinical trial centers in the United States from March 3, 2006, to July 25, 2013. Data analysis was performed from October 7, 2013, to March 24, 2014. The study randomized 416 women (≥18 years old) with bone metastases from breast cancer who previously received 9 or more doses of zoledronic acid and/or pamidronate during the first 10 to 15 months of therapy.
Main Outcomes and Measures: The primary end point was the proportion of patients with 1 or more SRE on study (SRE rate). The key secondary end points included time to first SRE and skeletal morbidity rate (SMR).
Results: A total of 416 women were randomized: 200 patients received zoledronic acid every 4 weeks (mean [SD] age, 59.2 [11.1] years; 173 were white [86.5%]), 203 patients received zoledronic acid every 12 weeks (mean [SD] age, 58.6 [11.2] years; 178 were white [87.7%]), and 13 patients received placebo (mean [SD] age, 60.8 [12.2] years; 13 were white [100%]). Baseline characteristics were similar in both zoledronic acid treatment arms. After 1 year of follow-up, SREs occurred in 44 patients (22.0%) in the zoledronic acid every 4 weeks group and 47 patients (23.2%) in the zoledronic acid every 12 weeks group (proportional difference of -1.2%; 1-sided 97.5% CI bound of the difference in SRE rate between arms, -9.8%; noninferiority P = .02). The time to first SRE between treatment groups was not statistically significantly different (hazard ratio [HR], 1.06; 95% CI, 0.70-1.60; P = .79). The mean (SD) SMR was 0.46 (1.06) vs 0.50 (1.50) events per year in the every 4 weeks vs every 12 weeks groups (P = .85). The safety profiles of the every 4 weeks and every 12 weeks groups were comparable, with 189 patients (95.5%) in the every 4 weeks group having at least 1 adverse event compared with 189 (93.5%) in the every 12 weeks group.
Conclusions and Relevance: The every 12 weeks regimen of zoledronic acid was noninferior to the every 4 weeks regimen for the proportion of patients experiencing 1 or more SRE. These results may have a substantial influence on current clinical practice for treatment of patients with bone metastasis from breast cancer.
Trial Registration: clinicaltrials.gov Identifier: NCT00320710.
Objective: To examine whether zoledronic acid every 12 weeks was noninferior to zoledronic acid every 4 weeks in patients with metastatic breast cancer that involved the bone who had previously received a standard dosing regimen of zoledronic acid and/or pamidronate disodium.
Design, Setting, and Participants: OPTIMIZE-2 was a prospective, randomized, double-blind, multicenter phase 3 trial of intention-to-treat (full analysis set), evaluable (per protocol), and safety populations. Patients were randomized (1:1) to receive 4.0 mg of intravenous zoledronic acid every 4 or every 12 weeks with placebo for interim infusions for 1 year. The study was conducted at 102 clinical trial centers in the United States from March 3, 2006, to July 25, 2013. Data analysis was performed from October 7, 2013, to March 24, 2014. The study randomized 416 women (≥18 years old) with bone metastases from breast cancer who previously received 9 or more doses of zoledronic acid and/or pamidronate during the first 10 to 15 months of therapy.
Main Outcomes and Measures: The primary end point was the proportion of patients with 1 or more SRE on study (SRE rate). The key secondary end points included time to first SRE and skeletal morbidity rate (SMR).
Results: A total of 416 women were randomized: 200 patients received zoledronic acid every 4 weeks (mean [SD] age, 59.2 [11.1] years; 173 were white [86.5%]), 203 patients received zoledronic acid every 12 weeks (mean [SD] age, 58.6 [11.2] years; 178 were white [87.7%]), and 13 patients received placebo (mean [SD] age, 60.8 [12.2] years; 13 were white [100%]). Baseline characteristics were similar in both zoledronic acid treatment arms. After 1 year of follow-up, SREs occurred in 44 patients (22.0%) in the zoledronic acid every 4 weeks group and 47 patients (23.2%) in the zoledronic acid every 12 weeks group (proportional difference of -1.2%; 1-sided 97.5% CI bound of the difference in SRE rate between arms, -9.8%; noninferiority P = .02). The time to first SRE between treatment groups was not statistically significantly different (hazard ratio [HR], 1.06; 95% CI, 0.70-1.60; P = .79). The mean (SD) SMR was 0.46 (1.06) vs 0.50 (1.50) events per year in the every 4 weeks vs every 12 weeks groups (P = .85). The safety profiles of the every 4 weeks and every 12 weeks groups were comparable, with 189 patients (95.5%) in the every 4 weeks group having at least 1 adverse event compared with 189 (93.5%) in the every 12 weeks group.
Conclusions and Relevance: The every 12 weeks regimen of zoledronic acid was noninferior to the every 4 weeks regimen for the proportion of patients experiencing 1 or more SRE. These results may have a substantial influence on current clinical practice for treatment of patients with bone metastasis from breast cancer.
Trial Registration: clinicaltrials.gov Identifier: NCT00320710.
Motilal Nehru V, Garcia G, Ding J, et al.
Humoral Hypercalcemia in Uterine Cancers: A Case Report and Literature Review.
Am J Case Rep. 2017; 18:22-25 [PubMed] Free Access to Full Article Related Publications
Humoral Hypercalcemia in Uterine Cancers: A Case Report and Literature Review.
Am J Case Rep. 2017; 18:22-25 [PubMed] Free Access to Full Article Related Publications
BACKGROUND Paraneoplastic hypercalcemia is a well-described complication associated with a variety of malignancies. However, its incidence in gynecological malignancies is low. CASE REPORT A 53-year-old woman presented with progressive abdominal distention and irregular vaginal bleeding of several weeks' duration. A contrast CT abdomen and pelvis was significant for a mass in the lower uterine/cervical region, multiple peritoneal and omental masses, enlarged pelvic and paraaortic lymph nodes, and large-volume ascites. A pelvic exam revealed a fungating vaginal mass, with biopsy showing a high-grade tumor with immunohistochemical staining positive for vimentin, CD10, and cyclin D1, consistent with endometrial stromal sarcoma. During her hospitalization, the patient became increasingly lethargic. Workup showed severe hypercalcemia and evidence of acute kidney injury. The patient did not have evidence of bony metastatic disease on imaging studies. Further laboratory evaluation revealed an elevated PTHrP of 301 pg/mL (nl 14-27), a depressed PTH level of 3 pg/mL (nl 15-65), and a depressed 25-OH vitamin D level of 16 ng/mL (nl 30-100), consistent with humoral hypercalcemia of malignancy. The patient was treated with pamidronate, calcitonin, and intravenous fluids. She eventually required temporary hemodialysis and denosumab for refractory hypercalcemia, which improved her electrolyte abnormalities and clinical status. CONCLUSIONS Uterine malignancies of various histologies are increasingly recognized as a cause of humoral hypercalcemia. They are an important differential diagnosis in a woman with hypercalcemia and abnormal vaginal bleeding or abdominal symptoms.
Aredia F, Scovassi AI
A new function for miRNAs as regulators of autophagy.
Future Med Chem. 2017; 9(1):25-36 [PubMed] Related Publications
A new function for miRNAs as regulators of autophagy.
Future Med Chem. 2017; 9(1):25-36 [PubMed] Related Publications
Autophagy is a self-digestive process regulated by an intricate network of factors able either to ensure the prosurvival function of autophagy or to convert it in a death pathway. Recently, the involvement of miRNAs in the regulation of autophagy networks has been reported. This review will summarize the main features of these small noncoding endogenous RNAs, focusing on their relevance in cancer and finally addressing their impact on autophagy.
Aredia F, Scovassi AI
Manipulation of Intracellular pH in Cancer Cells by NHE1 Inhibitors.
Protein Pept Lett. 2016; 23(12):1123-1129 [PubMed] Related Publications
Manipulation of Intracellular pH in Cancer Cells by NHE1 Inhibitors.
Protein Pept Lett. 2016; 23(12):1123-1129 [PubMed] Related Publications
Cancer cells are characterized by a peculiar pH condition, being the extracellular compartment acidic and the intracellular one neutral or basic, i.e. the opposite of what happens in normal cells. The reversal of the pH contributes to cancer cell proliferation and drug resistance. Among the different enzymes regulating pH gradient, proton transporters Na+/H+ exchangers (NHEs) are considered as suitable targets for drugs that ultimately counteract cancer cell survival. This review will describe the properties of NHEs, focusing on the prototype NHE1 and on the effect of its inhibition on cancer cell metabolism.
Roderick MR, Shah R, Rogers V, et al.
Chronic recurrent multifocal osteomyelitis (CRMO) - advancing the diagnosis.
Pediatr Rheumatol Online J. 2016; 14(1):47 [PubMed] Free Access to Full Article Related Publications
Chronic recurrent multifocal osteomyelitis (CRMO) - advancing the diagnosis.
Pediatr Rheumatol Online J. 2016; 14(1):47 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Chronic recurrent multifocal osteomyelitis (CRMO) is a little known inflammatory bone disease occurring primarily in children and adolescents. Delays in referral and diagnosis may lead to prolonged courses of antibiotics with in-patient care, unnecessary radiation exposure from multiple plain radiographs or bone scans and repeated surgery including bone biopsies. Children (aged < 18 years) diagnosed with CRMO between January 2005 and December 2012, reviewed at Bristol Royal Hospital for Children were included and all available data collected. Information regarding CRMO was sent to all orthopaedic surgeons in the region in 2009. The aim of the study was to examine the features of the cohort, to examine the length of time to diagnosis and to explore the criteria used for diagnosis with and without biopsy.
FINDINGS: Over an 8 year period, 41 patients were diagnosed with CRMO. Symptom onset occurred at a median of 9 years of age and time to diagnosis had a median of 15 months (range 0-92). Correlation coefficient analysis for time to diagnosis by year showed statistical significance with a decreasing trend. From the cohort data, diagnostic criteria were developed; applied retrospectively, 34 (83 %) children may have been diagnosed using the criteria, without a biopsy.
CONCLUSIONS: The data suggest that increasing knowledge of this condition may shorten time to diagnosis. Use of the Bristol diagnostic criteria by an experienced clinician may obviate the need for biopsy in some patients.
FINDINGS: Over an 8 year period, 41 patients were diagnosed with CRMO. Symptom onset occurred at a median of 9 years of age and time to diagnosis had a median of 15 months (range 0-92). Correlation coefficient analysis for time to diagnosis by year showed statistical significance with a decreasing trend. From the cohort data, diagnostic criteria were developed; applied retrospectively, 34 (83 %) children may have been diagnosed using the criteria, without a biopsy.
CONCLUSIONS: The data suggest that increasing knowledge of this condition may shorten time to diagnosis. Use of the Bristol diagnostic criteria by an experienced clinician may obviate the need for biopsy in some patients.
Kaneko N, Kawano S, Matsubara R, et al.
Tongue squamous cell carcinoma producing both parathyroid hormone-related protein and granulocyte colony-stimulating factor: a case report and literature review.
World J Surg Oncol. 2016; 14(1):161 [PubMed] Free Access to Full Article Related Publications
Tongue squamous cell carcinoma producing both parathyroid hormone-related protein and granulocyte colony-stimulating factor: a case report and literature review.
World J Surg Oncol. 2016; 14(1):161 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Paraneoplastic syndrome generally results from tumor-derived hormones or peptides that cause metabolic derangements. Common metabolic conditions include hyponatremia, hypercalcemia, hypoglycemia, and Cushing's syndrome. Herein, we report a very rare case of tongue carcinoma presenting with leukocytosis and hypercalcemia.
CASE PRESENTATION: A 57-year-old man was admitted to our hospital with tongue squamous cell carcinoma (cT4aN0M0, stage IV). He underwent radical resection following preoperative chemoradiotherapy, but locoregional recurrence was detected 2 months after surgery. He presented with marked leukocytosis and hypercalcemia with elevated serum levels of granulocyte colony-stimulating factor (G-CSF) and parathyroid hormone-related protein (PTHrP). He was therefore managed with intravenous fluids, furosemide, prednisolone, elcatonin, and pamidronate. However, the patient died 1 month later of carcinomatous pleuritis following distant metastasis to the lung. Immunohistochemical analyses of the resected specimens revealed positive staining for PTHrP and G-CSF in the cancer cells.
CONCLUSIONS: In this case, it was considered that tumor-derived G-CSF and PTHrP caused leukocytosis and hypercalcemia.
CASE PRESENTATION: A 57-year-old man was admitted to our hospital with tongue squamous cell carcinoma (cT4aN0M0, stage IV). He underwent radical resection following preoperative chemoradiotherapy, but locoregional recurrence was detected 2 months after surgery. He presented with marked leukocytosis and hypercalcemia with elevated serum levels of granulocyte colony-stimulating factor (G-CSF) and parathyroid hormone-related protein (PTHrP). He was therefore managed with intravenous fluids, furosemide, prednisolone, elcatonin, and pamidronate. However, the patient died 1 month later of carcinomatous pleuritis following distant metastasis to the lung. Immunohistochemical analyses of the resected specimens revealed positive staining for PTHrP and G-CSF in the cancer cells.
CONCLUSIONS: In this case, it was considered that tumor-derived G-CSF and PTHrP caused leukocytosis and hypercalcemia.
Greene LW, Asadipooya K, Corradi PF, Akin C
Endocrine manifestations of systemic mastocytosis in bone.
Rev Endocr Metab Disord. 2016; 17(3):419-431 [PubMed] Related Publications
Endocrine manifestations of systemic mastocytosis in bone.
Rev Endocr Metab Disord. 2016; 17(3):419-431 [PubMed] Related Publications
Systemic Mastocytosis (SM) is characterized by accumulation of clonal, neoplastic proliferations of abnormal mast cells (MC) in one or more organ system other than skin. Presence of these multifocal clusters of abnormal mast cells is an essential feature of SM. Frequently associated with D816V (KIT) mutation, the presence of this mutation and elevated serum tryptase are minor criteria for diagnosis. SM manifestations depend on the degree of mast cell proliferation, activation and degranulation. SM has a variable prognosis and presentation, from indolent to "smoldering" to life-threatening disease. Bone manifestations of SM include: osteopenia with or without lytic lesions, osteoporosis with or without atraumatic fracture, osteosclerosis with increased bone density, and isolated lytic lesions. Male sex, older age, higher bone resorption markers, lower DKK1 level, lower BMD, absence of urticaria pigmentosa, and alcohol intake are all associated with increased risk of fracture. Treatment of SM is generally palliative. Most therapy is symptom-directed; and, infrequently, chemotherapy for refractory symptoms is indicated. Anti-histamines may alleviate direct bone effects of histamine. Bisphosphonates, including alendronate, clodronate, pamidronate and zoledronic acid are recommended as a first line treatment of SM and osteoporosis. Interferon α may act synergistically with bisphosphonates. As elevation of RANKL and OPG is reported in SM, denosumab could be an effective therapy for bone manifestations of SM.
Tanaka R, Yonemori K, Hirakawa A, et al.
Risk Factors for Developing Skeletal-Related Events in Breast Cancer Patients With Bone Metastases Undergoing Treatment With Bone-Modifying Agents.
Oncologist. 2016; 21(4):508-13 [PubMed] Free Access to Full Article Related Publications
Risk Factors for Developing Skeletal-Related Events in Breast Cancer Patients With Bone Metastases Undergoing Treatment With Bone-Modifying Agents.
Oncologist. 2016; 21(4):508-13 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Bone-modifying agents (BMAs) reduce the incidence of skeletal-related events (SREs) and are thus recommended for breast cancer patients with bone metastases. However, the risk factors for SREs during BMA treatment are not well-understood. This study evaluated the number and timing of SREs from case studies to identify these factors.
METHODS: The medical records of 534 women with breast cancer who developed bone metastases between 1999 and 2011 were reviewed. SREs were defined as a pathologic fracture, spinal cord compression, or the need for bone irradiation or surgery. Multiple variables were assessed and were analyzed by using the Cox proportional hazard analyses and the Andersen and Gill method.
RESULTS: Multivariate analyses for both the time to the first SRE and the primary and subsequent SRE frequency demonstrated that significant baseline risk factors included luminal B type disease, a history of palliative radiation therapy, BMA treatment within 2 years, and elevated serum calcium levels at the time of the initial BMA dose. Additionally, for the time to the first SRE and for the primary and subsequent SRE frequency, the presence of extraskeletal metastases and BMA administration initiation ≥6 months after the detection of bone metastases were also significant risk factors, respectively.
CONCLUSION: In breast cancer patients with bone metastases, more vigilant observation should be considered for patients with the identified risk factors. To reduce the risk for SRE, BMAs should be administered within 6 months of bone metastases diagnosis and before palliative radiation therapy.
IMPLICATIONS FOR PRACTICE: Retrospectively, risk factors were identified for skeletal-related events (SREs) in breast cancer patients with bone metastasis who were treated with bone-modifying agents (BMAs). For the time to the first SRE and for the SRE frequency, presence of extraskeletal metastases and BMA initiation ≥6 months after the detection of bone metastases were risk factors, respectively. Luminal B type disease, a history of palliative radiation therapy, BMA treatment within 2 years, and elevated serum calcium levels at initial BMA dose were risk factors for both first SRE and SRE frequency. More vigilant observation should be considered for patients with these risk factors.
METHODS: The medical records of 534 women with breast cancer who developed bone metastases between 1999 and 2011 were reviewed. SREs were defined as a pathologic fracture, spinal cord compression, or the need for bone irradiation or surgery. Multiple variables were assessed and were analyzed by using the Cox proportional hazard analyses and the Andersen and Gill method.
RESULTS: Multivariate analyses for both the time to the first SRE and the primary and subsequent SRE frequency demonstrated that significant baseline risk factors included luminal B type disease, a history of palliative radiation therapy, BMA treatment within 2 years, and elevated serum calcium levels at the time of the initial BMA dose. Additionally, for the time to the first SRE and for the primary and subsequent SRE frequency, the presence of extraskeletal metastases and BMA administration initiation ≥6 months after the detection of bone metastases were also significant risk factors, respectively.
CONCLUSION: In breast cancer patients with bone metastases, more vigilant observation should be considered for patients with the identified risk factors. To reduce the risk for SRE, BMAs should be administered within 6 months of bone metastases diagnosis and before palliative radiation therapy.
IMPLICATIONS FOR PRACTICE: Retrospectively, risk factors were identified for skeletal-related events (SREs) in breast cancer patients with bone metastasis who were treated with bone-modifying agents (BMAs). For the time to the first SRE and for the SRE frequency, presence of extraskeletal metastases and BMA initiation ≥6 months after the detection of bone metastases were risk factors, respectively. Luminal B type disease, a history of palliative radiation therapy, BMA treatment within 2 years, and elevated serum calcium levels at initial BMA dose were risk factors for both first SRE and SRE frequency. More vigilant observation should be considered for patients with these risk factors.

 Breast Cancer
Breast Cancer