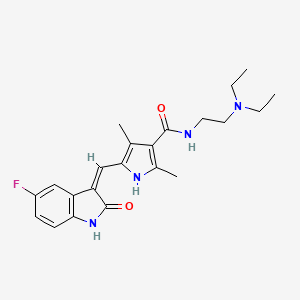
Sunitinib (Sutent)
Sunitinib is a 'multi-kinase inhibitor'. It blocks kinases, are which important in the regulatation of how normal and cancer cells grow and divide. Sunitinib is also an angiogenesis inhibitor, which means it prevents developing the new blood vessels that tumours need in order to grow.
Found this page useful?
 Web Resources: Sunitinib (Sutent)
Web Resources: Sunitinib (Sutent) Latest Research Publications
Latest Research PublicationsWeb Resources: Sunitinib (Sutent) (6 links)
MedlinePlus.gov
NHS Evidence
PubChem
Macmillan Cancer Support
Cancer Research UK
Irish Cancer Society
Latest Research Publications
Yuan A, Kurtz SL, Barysauskas CM, et al.
Oral adverse events in cancer patients treated with VEGFR-directed multitargeted tyrosine kinase inhibitors.
Oral Oncol. 2015; 51(11):1026-33 [PubMed] Related Publications
Oral adverse events in cancer patients treated with VEGFR-directed multitargeted tyrosine kinase inhibitors.
Oral Oncol. 2015; 51(11):1026-33 [PubMed] Related Publications
OBJECTIVES: This study characterized the incidence and clinical features of oral adverse events among cancer patients who received VEGFR-directed multitargeted tyrosine kinase inhibitor (VR-TKI) therapies.
METHODS: Electronic medical records of adult cancer patients treated with sunitinib, sorafenib, regorafenib, pazopanib, cabozantinib, imatinib, and bevacizumab therapy at Dana-Farber Cancer Institute from 2009 to 2012 were reviewed. Data collected included patient characteristics, oral and non-oral adverse events, and time to onset. Time oral adverse event-free was the primary outcome.
RESULTS: A total of 747 patients with 806 individual courses of therapy were treated for a median of 3.9months with sunitinib (n=161), sorafenib (n=172), regorafenib (n=15), pazopanib (n=132), cabozantinib (n=23), imatinib (n=144), or bevacizumab (n=159) for lung cancer (21%), gastrointestinal stromal tumor (15%), and metastatic renal cell carcinoma (13%). An oral adverse event was reported in 23.7% of patients at a median of 1.9months after starting therapy. The most commonly reported oral adverse event was oral mucosal sensitivity (dysesthesia), occurring in 12% of patients, typically without clinical findings. Multivariate models showed patients who received VR-TKI therapy were at greater risk of any oral adverse event compared with patients treated with imatinib or bevacizumab. Patients receiving VR-TKI therapy who developed an oral adverse event were also at increased risk for hand-foot skin reaction (15.9%).
CONCLUSIONS: VR-TKI associated oral adverse events are characterized primarily by dysesthesia with lack of clinical signs. Oral dysesthesia is more commonly associated with VR-TKIs than with bevacizumab or imatinib. Management is largely empirical and requires further investigation.
METHODS: Electronic medical records of adult cancer patients treated with sunitinib, sorafenib, regorafenib, pazopanib, cabozantinib, imatinib, and bevacizumab therapy at Dana-Farber Cancer Institute from 2009 to 2012 were reviewed. Data collected included patient characteristics, oral and non-oral adverse events, and time to onset. Time oral adverse event-free was the primary outcome.
RESULTS: A total of 747 patients with 806 individual courses of therapy were treated for a median of 3.9months with sunitinib (n=161), sorafenib (n=172), regorafenib (n=15), pazopanib (n=132), cabozantinib (n=23), imatinib (n=144), or bevacizumab (n=159) for lung cancer (21%), gastrointestinal stromal tumor (15%), and metastatic renal cell carcinoma (13%). An oral adverse event was reported in 23.7% of patients at a median of 1.9months after starting therapy. The most commonly reported oral adverse event was oral mucosal sensitivity (dysesthesia), occurring in 12% of patients, typically without clinical findings. Multivariate models showed patients who received VR-TKI therapy were at greater risk of any oral adverse event compared with patients treated with imatinib or bevacizumab. Patients receiving VR-TKI therapy who developed an oral adverse event were also at increased risk for hand-foot skin reaction (15.9%).
CONCLUSIONS: VR-TKI associated oral adverse events are characterized primarily by dysesthesia with lack of clinical signs. Oral dysesthesia is more commonly associated with VR-TKIs than with bevacizumab or imatinib. Management is largely empirical and requires further investigation.
Kleibeuker EA, Ten Hooven MA, Verheul HM, et al.
Combining radiotherapy with sunitinib: lessons (to be) learned.
Angiogenesis. 2015; 18(4):385-95 [PubMed] Free Access to Full Article Related Publications
Combining radiotherapy with sunitinib: lessons (to be) learned.
Angiogenesis. 2015; 18(4):385-95 [PubMed] Free Access to Full Article Related Publications
To improve the efficacy of radiotherapy (RTx), there is a growing interest in combining RTx with drugs that inhibit angiogenesis, i.e., the process of neo-vessel formation out of preexisting capillaries. A frequently used drug to inhibit angiogenesis is sunitinib (Sutent, SU11248), a receptor tyrosine kinase inhibitor that is currently FDA approved for the treatment of several cancer types. The current review presents an overview of the preclinical studies and clinical trials that combined sunitinib with RTx. We discuss the findings from preclinical and clinical observations with a focus on dose scheduling and commonly reported toxicities. In addition, the effects of combination therapy on tumor response and patient survival are described. Finally, the lessons learned from preclinical and clinical studies are summarized and opportunities and pitfalls for future clinical trials are presented.
Pilotte AP
Current management of patients with gastrointestinal stromal tumor receiving the multitargeted tyrosine kinase inhibitor sunitinib.
Curr Med Res Opin. 2015; 31(7):1363-76 [PubMed] Related Publications
Current management of patients with gastrointestinal stromal tumor receiving the multitargeted tyrosine kinase inhibitor sunitinib.
Curr Med Res Opin. 2015; 31(7):1363-76 [PubMed] Related Publications
BACKGROUND: Gastrointestinal stromal tumor (GIST), a form of soft tissue sarcoma, is often detected incidentally or at an advanced stage. The tyrosine kinase inhibitor sunitinib malate (Sutent * ) is established as second-line treatment for the management of GIST after disease progression on, or intolerance to, first-line imatinib treatment. Several published reviews give guidance on management of side effects in patients with advanced renal cell carcinoma treated with sunitinib, but fewer publications cover side-effect management in patients with GIST.
SCOPE: Using published articles and abstracts, prescribing information, and personal experience in managing patients with GIST at a specialized center of excellence for cancer care, I review side-effect management recommendations for patients with GIST treated with sunitinib and provide an overview of GIST.
FINDINGS: Sunitinib has a well described side-effect profile: most side effects occurring in patients with GIST can be easily managed by standard medical intervention and/or dose modification.
CONCLUSION: Care of patients with GIST can be enhanced through communication, support, knowledge, and education, with the goal of providing effective therapy and optimal symptom control.
SCOPE: Using published articles and abstracts, prescribing information, and personal experience in managing patients with GIST at a specialized center of excellence for cancer care, I review side-effect management recommendations for patients with GIST treated with sunitinib and provide an overview of GIST.
FINDINGS: Sunitinib has a well described side-effect profile: most side effects occurring in patients with GIST can be easily managed by standard medical intervention and/or dose modification.
CONCLUSION: Care of patients with GIST can be enhanced through communication, support, knowledge, and education, with the goal of providing effective therapy and optimal symptom control.
Sato H, Siddig S, Uzu M, et al.
Elacridar enhances the cytotoxic effects of sunitinib and prevents multidrug resistance in renal carcinoma cells.
Eur J Pharmacol. 2015; 746:258-66 [PubMed] Related Publications
Elacridar enhances the cytotoxic effects of sunitinib and prevents multidrug resistance in renal carcinoma cells.
Eur J Pharmacol. 2015; 746:258-66 [PubMed] Related Publications
Intrinsic drug resistance occurs in many renal carcinomas and is associated with increased expression of multidrug resistant proteins, which inhibits intracellular drug accumulation. Multidrug resistant protein 1, also known as P-glycoprotein, is a membrane drug efflux pump belonging to the ATP-binding cassette (ABC) transporter superfamily. ABC Sub-family B Member 2 (ABCG2) is widely distributed and is involved in the multidrug resistant phenotype. Sunitinib is a tyrosine kinase inhibitor used to treat kidney cancer that disrupts signaling pathways responsible for abnormal cancer cell proliferation and tumor angiogenesis. Multiple drug resistance is important in tyrosine kinase inhibitor-induced resistance. We hypothesized that inhibition of multidrug resistant transporters by elacridar (dual inhibitor of P-glycoprotein and ABCG 2) might overcome sunitinib resistance in experimental renal cell carcinoma. Human renal carcinoma cell lines 786-O, ACHN, and Caki-1 were treated with sunitinib or elacridar alone, or in combination. We showed that elacridar significantly enhanced sunitinib cytotoxicity in 786-O cells. P-glycoprotein activity, confirmed by P-glycoprotein function assay, was found to be inhibited by elacridar. ABCG2 expression was low in all renal carcinoma cell lines, and was suppressed only by combination treatment in 786-O cells. ABCG2 function was inhibited by sunitinib alone or combination with elacridar but not elacridar alone. These findings suggest that sunitinib resistance involves multidrug resistance transporters, and in combination with elacridar, can be reversed in renal carcinoma cells by P-glycoprotein inhibition.
Guida FM, Santoni M, Conti A, et al.
Alternative dosing schedules for sunitinib as a treatment of patients with metastatic renal cell carcinoma.
Crit Rev Oncol Hematol. 2014; 92(3):208-17 [PubMed] Related Publications
Alternative dosing schedules for sunitinib as a treatment of patients with metastatic renal cell carcinoma.
Crit Rev Oncol Hematol. 2014; 92(3):208-17 [PubMed] Related Publications
Sunitinib malate (Sutent; Pfizer, Inc., New York, NY) is an oral multitargeted tyrosine kinase inhibitor that inhibits VEGF receptors (VEGFR-1, VEGFR-2, and VEGFR-3) among a family of kinase targets and have a central role in first-line treatment of metastatic renal cell carcinoma (mRCC). The approved schedule for sunitinib is 50mg/day oid in the so called "4 weeks on and two weeks off" (4/2 schedule). Since treatment with sunitinib can be maintained for years, adequate treatment of adverse events (AEs) and care for quality of life is essential. For this reason, several alternative schedules have been proposed in order to personalize sunitinib administration and reduce related toxicity. This review discusses the efficacy and tolerability of alternative regimens to the standard 4/2 schedule that have been investigated in RCC patients including schedule of 50mg/day 2-weeks on/1-week off, continuous schedule of 37.5mg daily and the "Stop and Go strategy".
Subbiah V, Meric-Bernstam F, Mills GB, et al.
Next generation sequencing analysis of platinum refractory advanced germ cell tumor sensitive to Sunitinib (Sutent®) a VEGFR2/PDGFRβ/c-kit/ FLT3/RET/CSF1R inhibitor in a phase II trial.
J Hematol Oncol. 2014; 7:52 [PubMed] Free Access to Full Article Related Publications
Next generation sequencing analysis of platinum refractory advanced germ cell tumor sensitive to Sunitinib (Sutent®) a VEGFR2/PDGFRβ/c-kit/ FLT3/RET/CSF1R inhibitor in a phase II trial.
J Hematol Oncol. 2014; 7:52 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Germ cell tumors (GCT) are the most common solid tumors in adolescent and young adult males (age 15 and 35 years) and remain one of the most curable of all solid malignancies. However a subset of patients will have tumors that are refractory to standard chemotherapy agents. The management of this refractory population remains challenging and approximately 400 patients continue to die every year of this refractory disease in the United States.
METHODS: Given the preclinical evidence implicating vascular endothelial growth factor (VEGF) signaling in the biology of germ cell tumors, we hypothesized that the vascular endothelial growth factor receptor (VEGFR) inhibitor sunitinib (Sutent) may possess important clinical activity in the treatment of this refractory disease. We proposed a Phase II efficacy study of sunitinib in seminomatous and non-seminomatous metastatic GCT's refractory to first line chemotherapy treatment (ClinicalTrials.gov Identifier: NCT00912912). Next generation targeted exome sequencing using HiSeq 2000 (Illumina Inc., San Diego, CA, USA) was performed on the tumor sample of the unusual responder.
RESULTS: Five patients are enrolled into this Phase II study. Among them we report here the clinical course of a patient (Patient # 5) who had an exceptional response to sunitinib. Next generation sequencing to understand this patient's response to sunitinib revealed RET amplification, EGFR and KRAS amplification as relevant aberrations. Oncoscan MIP array were employed to validate the copy number analysis that confirmed RET gene amplification.
CONCLUSION: Sunitinib conferred clinical benefit to this heavily pre-treated patient. Next generation sequencing of this 'exceptional responder' identified the first reported case of a RET amplification as a potential basis of sensitivity to sunitinib (VEGFR2/PDGFRβ/c-kit/ FLT3/RET/CSF1R inhibitor) in a patient with refractory germ cell tumor. Further characterization of GCT patients using biomarkers for clinical response and patient selection is warranted.
TRIAL REGISTRATION: ClinicalTrials.gov Identifier: NCT00912912.
METHODS: Given the preclinical evidence implicating vascular endothelial growth factor (VEGF) signaling in the biology of germ cell tumors, we hypothesized that the vascular endothelial growth factor receptor (VEGFR) inhibitor sunitinib (Sutent) may possess important clinical activity in the treatment of this refractory disease. We proposed a Phase II efficacy study of sunitinib in seminomatous and non-seminomatous metastatic GCT's refractory to first line chemotherapy treatment (ClinicalTrials.gov Identifier: NCT00912912). Next generation targeted exome sequencing using HiSeq 2000 (Illumina Inc., San Diego, CA, USA) was performed on the tumor sample of the unusual responder.
RESULTS: Five patients are enrolled into this Phase II study. Among them we report here the clinical course of a patient (Patient # 5) who had an exceptional response to sunitinib. Next generation sequencing to understand this patient's response to sunitinib revealed RET amplification, EGFR and KRAS amplification as relevant aberrations. Oncoscan MIP array were employed to validate the copy number analysis that confirmed RET gene amplification.
CONCLUSION: Sunitinib conferred clinical benefit to this heavily pre-treated patient. Next generation sequencing of this 'exceptional responder' identified the first reported case of a RET amplification as a potential basis of sensitivity to sunitinib (VEGFR2/PDGFRβ/c-kit/ FLT3/RET/CSF1R inhibitor) in a patient with refractory germ cell tumor. Further characterization of GCT patients using biomarkers for clinical response and patient selection is warranted.
TRIAL REGISTRATION: ClinicalTrials.gov Identifier: NCT00912912.
Pal SK, Hu A, Chang M, Figlin RA
Programmed death-1 inhibition in renal cell carcinoma: clinical insights and future directions.
Clin Adv Hematol Oncol. 2014; 12(2):90-9 [PubMed] Related Publications
Programmed death-1 inhibition in renal cell carcinoma: clinical insights and future directions.
Clin Adv Hematol Oncol. 2014; 12(2):90-9 [PubMed] Related Publications
The treatment of metastatic renal cell carcinoma (mRCC) has evolved markedly over the past decade, broaden- ing beyond immune-based strategies (eg, interleukin-2 and interferon-α) to include targeted agents (eg, sunitinib [Sutent, Pfizer] and sorafenib [Nexavar, Bayer]). Recently, there has been a renewed interest in immune-based strategies, with clinical trials underway to assess vaccines and other immunomodulatory agents. Of particular interest are agents that inhibit the interaction between the programmed death-1 (PD-1) receptor and its ligand (PD-L1) at the T-cell/antigen-presenting cell interface. This interaction produces T-cell anergy and therefore stifles the antitumor immune response. Monoclonal antibodies to PD-1 (eg, nivolumab, lambrolizumab, and pidilizumab) and PD-L1 (MPDL3280A and BMS-936559) are in various stages of clinical development. The clinical trajectory of these agents is discussed herein, with specific attention to the potential placement of PD-1/ PD-L1 inhibition in the crowded therapeutic landscape of mRCC.
Leone Roberti Maggiore U, Valenzano Menada M, Venturini PL, Ferrero S
The potential of sunitinib as a therapy in ovarian cancer.
Expert Opin Investig Drugs. 2013; 22(12):1671-86 [PubMed] Related Publications
The potential of sunitinib as a therapy in ovarian cancer.
Expert Opin Investig Drugs. 2013; 22(12):1671-86 [PubMed] Related Publications
INTRODUCTION: Sunitinib malate (SU11248; Sutent®; Pfizer, Inc., New York) is a multi-kinase inhibitor currently approved for use in advanced renal cell carcinoma (RCC), imatinib-resistant/-intolerant gastrointestinal stromal tumours and progressive, well-differentiated pancreatic neuroendocrine tumours in patients with unresectable, locally advanced or metastatic disease.
AREAS COVERED: This article describes the mechanism of action and of the pharmacokinetics of sunitinib; further, it summarizes Phase I and II trials on the clinical efficacy, tolerability and safety of this agent in the setting of ovarian cancer (OC) treatment.
EXPERT OPINION: On the basis of the current literature, sunitinib has shown modest antitumour activity and acceptable toxicity. Studies investigating the impact of horizontal and vertical combinations should represent a priority of future research. Although clinical Phase II trials on the use of sunitinib in the treatment of OC demonstrated an acceptable profile of AEs, a greater comprehension of the toxicity of this compound is recommended.
AREAS COVERED: This article describes the mechanism of action and of the pharmacokinetics of sunitinib; further, it summarizes Phase I and II trials on the clinical efficacy, tolerability and safety of this agent in the setting of ovarian cancer (OC) treatment.
EXPERT OPINION: On the basis of the current literature, sunitinib has shown modest antitumour activity and acceptable toxicity. Studies investigating the impact of horizontal and vertical combinations should represent a priority of future research. Although clinical Phase II trials on the use of sunitinib in the treatment of OC demonstrated an acceptable profile of AEs, a greater comprehension of the toxicity of this compound is recommended.
Tekisogullari K, Topcul M
The effects of sunitinib malate used in targeted therapy on the proliferation of HeLa cells in vitro.
J BUON. 2013 Jan-Mar; 18(1):253-60 [PubMed] Related Publications
The effects of sunitinib malate used in targeted therapy on the proliferation of HeLa cells in vitro.
J BUON. 2013 Jan-Mar; 18(1):253-60 [PubMed] Related Publications
PURPOSE: In this study, the antiproliferative and apoptotic effects of sunitinib (SU-11248, Sutent) which is used for targeted therapy was evaluated on HeLa cell line originated from human cervix carcinoma.
METHODS: Three different doses of sutent (D1= 1 μM, D2= 5 μM, D3= 10 μM) were administered to cells for 72 h to determine the optimal dose.
RESULTS: Increase in apoptotic index (AI), decrease in mitotic index (MI) of cells and slow down in proliferation rate were achieved at the dose level of 10 μM, especially at 72 h. All these findings were statistically significant (p<0.001). In addition, anaphase bridges and existence of tripolar metaphase cells that were observed at 72 h were possibly attributable to a chromosomal instability arising from shortening of telomere.
CONCLUSION: In this study, sutent effected cell kinetic parameters significantly. These results are consistent with other studies in the literature. In addition, anaphase bridges which were seen in mitosis preparations were interpreted as shortening or degradation of the telomere.
METHODS: Three different doses of sutent (D1= 1 μM, D2= 5 μM, D3= 10 μM) were administered to cells for 72 h to determine the optimal dose.
RESULTS: Increase in apoptotic index (AI), decrease in mitotic index (MI) of cells and slow down in proliferation rate were achieved at the dose level of 10 μM, especially at 72 h. All these findings were statistically significant (p<0.001). In addition, anaphase bridges and existence of tripolar metaphase cells that were observed at 72 h were possibly attributable to a chromosomal instability arising from shortening of telomere.
CONCLUSION: In this study, sutent effected cell kinetic parameters significantly. These results are consistent with other studies in the literature. In addition, anaphase bridges which were seen in mitosis preparations were interpreted as shortening or degradation of the telomere.
Neri A, Lambert Y, Marrelli D, et al.
Gastro-pleuro-pericardial fistula following combined radiation and chemotherapy for lung metastases from renal cell carcinoma: report of a case.
Surg Today. 2013; 43(12):1457-60 [PubMed] Related Publications
Gastro-pleuro-pericardial fistula following combined radiation and chemotherapy for lung metastases from renal cell carcinoma: report of a case.
Surg Today. 2013; 43(12):1457-60 [PubMed] Related Publications
Gastropleural and gastropericardial fistulas are abnormal communications between the stomach and the pleural cavity or pericardium. They are rare and life-threatening complications, which require prompt surgical intervention. We report the case of a gastro-pleuro-pericardial fistula that developed in a patient treated with radiotherapy and then Sunitinib (Sutent(®)), a novel tyrosine-kinase inhibitor, for lung metastases from renal cell carcinoma. To our knowledge, this is the first case of a gastro-pleuro-pericardial fistula developing as a consequence of combined radiation and chemotherapy.
Hörsch D, Bert T, Schrader J, et al.
Pancreatic neuroendocrine neoplasms.
Minerva Gastroenterol Dietol. 2012; 58(4):401-26 [PubMed] Related Publications
Pancreatic neuroendocrine neoplasms.
Minerva Gastroenterol Dietol. 2012; 58(4):401-26 [PubMed] Related Publications
Pancreatic neuroendocrine tumors originate from the diffuse neuroendocrine system in the pancreatic region. These tumors exhibit a rising incidence despite their rareness and due to their benign behavior a considerable prevalence. Pathogenesis of pancreatic neuroendocrine tumors is characterized by common pathways of hereditary and sporadic tumors. Pancreatic neuroendocrine tumors may secrete peptide hormones or biogenic amines in an autonomous fashion as functional active tumors. Pathological grading and staging by TNM systems has been established in recent years classifying well and moderately differentiated pancreatice neuroendocrine tumors and poorly differentiated neuroendocrine carcinomas. Chromogranin A and less so pancreatic polypeptide are suitable tumor markers for pancreatic neuroendocrine tumors. Expression of receptors for somatostatin is the basis of treatment of pancreatic neuroendocrine tumors with somatostatin analogues as antisecretive and antiproliferative agents. In addition, somatostatin scintigraphy or PET/CT allows comprehensive diagnosis of pancreatic neuroendocrine tumors, which should be supported by (endoscopic and contrast enhanced) ultrasound, CT and MRI. Therapy of pancreatic neuroendocrine tumors consists of somatostatin analogues, chemotherapy, targeted therapy and peptide receptor radionuclide therapy. Two molecular substances hav been registered for pancreatic neuroendocrine tumors recently, sunitinib (Sutent®) and everolimus (Afinitor®). Predominant tumor load in the liver may be treated by local ablative therapy or liver transplantation. These treatment options have been included in guidelines of several professional societies and weighted for sequential therapy of patients with pancreatic neuroendocrine tumors according to effects and side effects.
Huang J, Zhang J, Dong B, et al.
Primitive neuroectodermal tumor of the kidney: a single-institute series of six patients from China.
Urol Int. 2013; 90(2):174-8 [PubMed] Related Publications
Primitive neuroectodermal tumor of the kidney: a single-institute series of six patients from China.
Urol Int. 2013; 90(2):174-8 [PubMed] Related Publications
OBJECTIVE: Renal primitive neuroectodermal tumor (PNET) is a rare and highly malignant neoplasm. Our study aims to present the clinical findings and prognosis of 6 patients with renal PNET from China.
MATERIAL AND METHODS: From January 2003 to February 2012, 6 patients with renal PNET confirmed by immunohistochemical staining and fluorescence in situ hybridization (FISH) treated in our institution were reviewed retrospectively and our data compared with the literature.
RESULTS: There were 4 male and 2 female patients with a mean age of 35.0 years. The mean diameter was 13.3 cm. Five of the masses had renal vein thrombosis, and 3 extended into the inferior vena cava. A lymph node metastasis was detected in 1 patient and a liver metastasis in another patient. Radical nephrectomy was performed in all cases, with 5 patients following chemotherapy and 1 receiving Sutent treatment. Within a median follow-up of 7.5 months (range 1-71), median overall survival was 22.1 months.
CONCLUSIONS: The diagnosis of renal PNET should be considered in young patients presenting with renal mass and venous thrombosis. It seems that Asian renal PNET patients had a higher rate of venous thrombosis than Caucasian populations. CD99 positivity on immunohistochemistry and EWS-FL1 chimera gene detected by FISH support the diagnosis. The prognosis is poor despite multimodal treatment.
MATERIAL AND METHODS: From January 2003 to February 2012, 6 patients with renal PNET confirmed by immunohistochemical staining and fluorescence in situ hybridization (FISH) treated in our institution were reviewed retrospectively and our data compared with the literature.
RESULTS: There were 4 male and 2 female patients with a mean age of 35.0 years. The mean diameter was 13.3 cm. Five of the masses had renal vein thrombosis, and 3 extended into the inferior vena cava. A lymph node metastasis was detected in 1 patient and a liver metastasis in another patient. Radical nephrectomy was performed in all cases, with 5 patients following chemotherapy and 1 receiving Sutent treatment. Within a median follow-up of 7.5 months (range 1-71), median overall survival was 22.1 months.
CONCLUSIONS: The diagnosis of renal PNET should be considered in young patients presenting with renal mass and venous thrombosis. It seems that Asian renal PNET patients had a higher rate of venous thrombosis than Caucasian populations. CD99 positivity on immunohistochemistry and EWS-FL1 chimera gene detected by FISH support the diagnosis. The prognosis is poor despite multimodal treatment.
Casciano R, Chulikavit M, Perrin A, et al.
Cost-effectiveness of everolimus vs sunitinib in treating patients with advanced, progressive pancreatic neuroendocrine tumors in the United States.
J Med Econ. 2012; 15 Suppl 1:55-64 [PubMed] Related Publications
Cost-effectiveness of everolimus vs sunitinib in treating patients with advanced, progressive pancreatic neuroendocrine tumors in the United States.
J Med Econ. 2012; 15 Suppl 1:55-64 [PubMed] Related Publications
BACKGROUND: Everolimus (Afinitor) and sunitinib (Sutent) were recently approved to treat patients with advanced, progressive pancreatic neuroendocrine tumors (pNETs). (Afinitor is a registered trademark of Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA; Sutent is a registered trademark of Pfizer Inc., New York, NY, USA.) This analysis examined the projected cost-effectiveness of everolimus vs sunitinib in this setting from a US payer perspective.
METHODS: A semi-Markov model was developed to simulate a cohort of patients with advanced, progressive pNET and to estimate the cost per life-year gained (LYG) and per quality-adjusted life-year (QALY) gained when treating with everolimus vs sunitinib. Efficacy data were based on a weight-adjusted indirect comparison of the agents using phase 3 trial data. Model health states included: stable disease with no adverse events, stable disease with adverse events, disease progression, and death. Therapy costs were based on wholesale acquisition cost. Other costs such as physician visits, tests, hospitalizations, and adverse event costs were obtained from literature and/or primary research. Utility inputs were based on primary research. Sensitivity analyses were conducted to test the model's robustness.
RESULTS: In the base-case analysis, everolimus was associated with an incremental 0.448 LYG (0.304 QALYs) at an incremental cost of $12,673, resulting in an incremental cost-effectiveness ratio (ICER) of $28,281/LYG ($41,702/QALY gained). The ICER fell within the cost per QALY range for many widely used oncology drugs. Sensitivity analyses demonstrated that, overall, there is a trend that everolimus is cost-effective compared to sunitinib in this setting.
LIMITATIONS: Results of the indirect analysis were not statistically significant (p > 0.05). Assumptions that treatment patterns are the same across therapies may not represent real-world practice.
CONCLUSIONS: While the analysis is limited by its reliance on an indirect comparison of two phase 3 studies, everolimus is expected to be cost-effective relative to sunitinib in advanced, progressive pNET.
METHODS: A semi-Markov model was developed to simulate a cohort of patients with advanced, progressive pNET and to estimate the cost per life-year gained (LYG) and per quality-adjusted life-year (QALY) gained when treating with everolimus vs sunitinib. Efficacy data were based on a weight-adjusted indirect comparison of the agents using phase 3 trial data. Model health states included: stable disease with no adverse events, stable disease with adverse events, disease progression, and death. Therapy costs were based on wholesale acquisition cost. Other costs such as physician visits, tests, hospitalizations, and adverse event costs were obtained from literature and/or primary research. Utility inputs were based on primary research. Sensitivity analyses were conducted to test the model's robustness.
RESULTS: In the base-case analysis, everolimus was associated with an incremental 0.448 LYG (0.304 QALYs) at an incremental cost of $12,673, resulting in an incremental cost-effectiveness ratio (ICER) of $28,281/LYG ($41,702/QALY gained). The ICER fell within the cost per QALY range for many widely used oncology drugs. Sensitivity analyses demonstrated that, overall, there is a trend that everolimus is cost-effective compared to sunitinib in this setting.
LIMITATIONS: Results of the indirect analysis were not statistically significant (p > 0.05). Assumptions that treatment patterns are the same across therapies may not represent real-world practice.
CONCLUSIONS: While the analysis is limited by its reliance on an indirect comparison of two phase 3 studies, everolimus is expected to be cost-effective relative to sunitinib in advanced, progressive pNET.
Blumenthal GM, Cortazar P, Zhang JJ, et al.
FDA approval summary: sunitinib for the treatment of progressive well-differentiated locally advanced or metastatic pancreatic neuroendocrine tumors.
Oncologist. 2012; 17(8):1108-13 [PubMed] Free Access to Full Article Related Publications
FDA approval summary: sunitinib for the treatment of progressive well-differentiated locally advanced or metastatic pancreatic neuroendocrine tumors.
Oncologist. 2012; 17(8):1108-13 [PubMed] Free Access to Full Article Related Publications
On May 20, 2011, the U.S. Food and Drug Administration (FDA) approved sunitinib malate capsules (Sutent®; Pfizer, Inc., New York) for the treatment of progressive, well-differentiated pancreatic neuroendocrine tumors (pNETs) in patients with unresectable locally advanced or metastatic disease. In a phase III randomized trial, 171 patients received either sunitinib (37.5 mg) or placebo once daily. The progression-free survival (PFS) interval was the primary efficacy endpoint. Secondary endpoints included the overall survival (OS) time, objective response rate (ORR), patient-reported outcomes, and safety. Based on early results favoring sunitinib, the independent data monitoring committee recommended trial termination prior to the prespecified interim analysis. This premature analysis may have led to an overestimate of the treatment effect. In the FDA analysis of investigator-assessed PFS times, the median values for the sunitinib and placebo arms were 10.2 months and 5.4 months, respectively. The ORRs were 9.3% and 0% in the sunitinib and placebo arms, respectively. The OS data were not mature at the time of approval and were confounded by 69% crossover. Common adverse reactions in patients receiving sunitinib included diarrhea, nausea, asthenia, fatigue, neutropenia, hypertension, and palmar-plantar erythrodysesthesia syndrome. Two patients on sunitinib died as a result of cardiac failure. The Oncologic Drugs Advisory Committee voted eight to two that, despite residual uncertainty about the magnitude of the PFS effect because of early trial termination, sunitinib demonstrated a favorable benefit-risk profile in pNET patients. The FDA concurred with the committee's assessment and granted sunitinib regular approval for this rare malignancy with few available therapies.
Wu CL, Ping SY, Yu CP, Yu DS
Tyrosine kinase receptor inhibitor-targeted combined chemotherapy for metastatic bladder cancer.
Kaohsiung J Med Sci. 2012; 28(4):194-203 [PubMed] Related Publications
Tyrosine kinase receptor inhibitor-targeted combined chemotherapy for metastatic bladder cancer.
Kaohsiung J Med Sci. 2012; 28(4):194-203 [PubMed] Related Publications
Overexpression of hypoxia-inducible factor-1 alpha is noted during the invasive and metastatic process of transitional cell carcinoma. It will upregulate vascular endothelial growth factor (VEGF) and drive proliferation, invasiveness, metastasis, and antiapoptotic ability of cancer cells. We proposed that tyrosine kinase receptor inhibitor, sunitinib malate-(Sutent; Pfizer Inc., Taiwan), combined with chemotherapeutic drug may present synergistic cytotoxic enhancement to transitional cell carcinoma cells with subsequent inhibition of their cellular behaviors, including proliferation, invasiveness, and metastatic activity. The contents of VEGF-A in mouse bladder tumor cells (MBT-2) and culture medium were detected by quantification-polymerase chain reaction and Western blot individually. The inhibitory concentrations of various chemotherapeutic drugs, sunitinib, and their combination treatment in MBT-2 were determined by 3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide (MTT) assay. Microchamber transmembrane migration assay was applied in evaluation of the inhibitory effects of different dosages of sunitinib and combination treatment on tumor cells. The cell cycle and apoptosis were analyzed after combination therapy by flow cytometry. Variation in apoptotic pathway was elucidated by Western blot using specific antibodies with cleaved PARP and caspase-3. Metastatic animal model mimicked by tail vein injection of MBT-2 cells was used to evaluate the treatment efficiency in tumor weight and survival rate. The mRNA and protein level of VEGF-A in MBT-2 cells increased by 70% at 48 hours interval under hypoxia stress condition. In MTT assay, MBT-2 cells had shown the highest sensitivity to epirubicin. Sunitinib combined with epirubicin had shown a synergistic cytotoxic effect to MBT-2 cells. Sunitinib and its combination with epirubicin showed significant inhibition on MBT-2 cells migration in microchambers. G2/M phase arrest and increased subG1 in cell cycle was seen in the epirubicin and sunitinib combination treatment group. The activation of apoptosis pathway was confirmed by increased cleaved caspase-3 and cleaved PARP in MBT-2 cells. In tail vein tumor inoculation C3H mice model, epirubicin alone and sunitinib combination therapy decreased tumor growth in lungs with marginal effect. Sunitinib and epirubicin combination had shown a synergistic cytotoxic effect and inhibited cell migration ability in MBT-2 cells. The combination can induce cell cycle arrest at G2/M phase and increase subG1 cells. Metastatic animal study also showed that sunitinib combined with epirubicin has a marginal effect on inhibition of tumor growth of lungs. The tyrosine kinase receptor inhibitor-targeted combined chemotherapy regimen may provide as a new treatment modality for advanced bladder cancer in the future.
Capurso G, Di Florio A, Sette C, Delle Fave G
Signalling pathways passing Src in pancreatic endocrine tumours: relevance for possible combined targeted therapies.
Neuroendocrinology. 2013; 97(1):67-73 [PubMed] Related Publications
Signalling pathways passing Src in pancreatic endocrine tumours: relevance for possible combined targeted therapies.
Neuroendocrinology. 2013; 97(1):67-73 [PubMed] Related Publications
The most frequent molecular abnormalities in pancreatic endocrine tumours (PETs) are mutations of the MEN1 gene, deregulation of the PI3K/AKT/mTOR signalling pathway and overactivation of growth factors and their receptors, such as the VEGF. On this basis, everolimus (Afinitor®; Novartis) and sunitinib (Sutent®; Pfizer) have both been approved by the FDA for the treatment of progressive, unresectable, locally advanced or metastatic PETs. However, molecular or surrogate markers able to predict the response of PET patients to treatment with these drugs are not available, and cancer cells treated with targeted therapies might develop escape pathways that evoke pro-survival feedback responses. The existence of cross-talk between different molecular pathways in PETs has been poorly investigated. In the present review, we present data supporting an important role for Src family kinases (SFKs) in PETs, together with the recent observation of a novel role for SFK in modulating the mTOR pathway activity. Of note, while treatment with everolimus triggered the activation of a survival response dependent on PI3K/AKT signalling in vitro, the simultaneous inhibition of SFKs blocked the activation of this unwanted escape signal. These studies might set the ground for the investigation of combined treatment of PETs with SFK and mTOR inhibitors.
Zhou C, Zhang J, Zheng Y, Zhu Z
Pancreatic neuroendocrine tumors: a comprehensive review.
Int J Cancer. 2012; 131(5):1013-22 [PubMed] Related Publications
Pancreatic neuroendocrine tumors: a comprehensive review.
Int J Cancer. 2012; 131(5):1013-22 [PubMed] Related Publications
Pancreatic neuroendocrine tumors (NETs) are a heterogeneous group of tumors. Despite being relatively rare, representing just 1-2% of all pancreatic neoplasms, the incidence of pancreatic NET has increased over the past two decades. Although the primary treatment for localized NET is surgical resection, there is still a lack of effective therapeutic options for patients with advanced unresectable pancreatic NET. Recently, the targeted agents sunitinib malate (SUTENT®, Pfizer Inc, NYC) and everolimus (AFINITOR®, Novartis, Basel, Switzerland)-both with different mechanisms of action-received United States Food and Drug Administration approval for the treatment of progressive, well-differentiated, pancreatic NET in patients with unresectable, locally advanced or metastatic disease. SUTENT® also received approval for this indication by the European Commission in 2010. Our article presents an overview of pancreatic NET, with a focus on their diagnostic work-up, clinical presentation and treatment options. Topics for further investigation of targeted therapy are also discussed.
Reidy-Lagunes D, Thornton R
Pancreatic neuroendocrine and carcinoid tumors: what's new, what's old, and what's different?
Curr Oncol Rep. 2012; 14(3):249-56 [PubMed] Related Publications
Pancreatic neuroendocrine and carcinoid tumors: what's new, what's old, and what's different?
Curr Oncol Rep. 2012; 14(3):249-56 [PubMed] Related Publications
Well-differentiated neuroendocrine tumors (NETs) can be subdivided into carcinoid and pancreatic NETs (panNETs). Recently, two therapies have been FDA approved for progressive well-differentiated pancreatic NETs but have not been submitted for use in carcinoid tumors (Yao, Shah, Ito, et al. N Engl J Med 364:514-23, 2011••; Raymond, Dahan, Raoul, et al. N Engl J Med 364:501-13, 2011••). The first is sunitinib (Sutent(®), Pfizer, Inc.), an orally administered, multitargeted receptor kinase inhibitor. The second targeted agent is everolimus (Afinitor(®), Novartis Pharmaceuticals), a mammalian target of rapamycin (mTOR) inhibitor (Yao, Shah, Ito, et al. N Engl J Med 364:514-23, 2011••). Both agents demonstrated improved progression-free survival but can also result in non-trivial toxicities and therefore, should only be considered in patients with progressing or symptomatic pancreatic NET. This review will discuss "new" NET therapies and provides an overview of liver directed and "older" cytotoxic treatment options. We also briefly outline "what's different" by describing a recent genetics report identifying genetic mutations in panNETs. Such a discovery could potentially be used to stratify treatment and such studies are currently being investigated.
Siraj MA, Pichon C, Radu A, Ghinea N
Endothelial follicle stimulating hormone receptor in primary kidney cancer correlates with subsequent response to sunitinib.
J Cell Mol Med. 2012; 16(9):2010-6 [PubMed] Free Access to Full Article Related Publications
Endothelial follicle stimulating hormone receptor in primary kidney cancer correlates with subsequent response to sunitinib.
J Cell Mol Med. 2012; 16(9):2010-6 [PubMed] Free Access to Full Article Related Publications
Sunitinib is an anti-angiogenic receptor tyrosine kinase inhibitor used to treat advanced metastatic renal cell carcinoma and other types of cancer. Sutent is effective in only approximately 70% of clear cell renal cell carcinoma (CCRCC) patients, has significant adverse side effects and no method is available to predict which patients will not respond. Our purpose was to explore the possibility of introducing an effective prediction method based on a marker of the tumour vasculature, the follicle stimulating hormone receptor (FSHR). Fifty patients diagnosed with advanced metastatic CCRCC have been subjected to surgery for removal of the primary tumour and were subsequently treated with sunitinib. After three months of therapy the patients were categorized as 'responsive', 'stable' or 'non-responsive' based on the RECIST guidelines. The blood vessel density and the percentage of FSHR-positive vessels were determined by immunofluorescence on sections from the primary tumours removed by surgery, prior to the sunitinib treatment. The percentage of FSHR-stained vessels was on average fivefold higher for the patients who responded to the treatment in comparison with the stable group and almost eightfold higher than in the non-responsive group. The percentage allowed the detection of responders with 87-100% sensitivity and specificity. No significant differences were detected in the total density of vessels among the three groups. The data suggest that FSHR expression levels in the blood vessels of CCRCC primary tumours can be used to predict, with high sensitivity and specificity, the patients who will respond to sunitinib therapy.
Hubner RA, Valle JW
Sunitinib for advanced pancreatic neuroendocrine tumors.
Expert Rev Anticancer Ther. 2011; 11(12):1817-27 [PubMed] Related Publications
Sunitinib for advanced pancreatic neuroendocrine tumors.
Expert Rev Anticancer Ther. 2011; 11(12):1817-27 [PubMed] Related Publications
Recent recognition of the high prevalence of neuroendocrine tumors in combination with a sustained failure to improve outcomes for patients with advanced disease has elevated their priority for research and drug development. Sunitinib (SU11248, Sutent; Pfizer Inc. NY, USA) potently inhibits multiple-receptor tyrosine kinases, resulting in antiangiogenic effects. A growing body of evidence indicates angiogenesis is a clinically relevant therapeutic target in pancreatic neuroendocrine tumors, culminating in a Phase III randomized study of sunitinib in patients with advanced progressive pancreatic neuroendocrine tumors. Sunitinib has recently gained regulatory approval as a single agent in this setting, and future studies will investigate most appropriate patient selection, and sequencing and combination with other targeted and cytotoxic agents. Here, we discuss in detail the molecular properties, clinical efficacy and safety of sunitinib in the context of pancreatic neuroendocrine tumors.
Tyrosine kinase inhibitors for metastatic renal cell carcinoma.
Drug Ther Bull. 2011; 49(11):129-32 [PubMed] Related Publications
Renal cell carcinoma accounts for 2-3% of all adult malignancies worldwide, and around 30% of patients with the condition present with advanced or metastatic disease.1,2 Until recently, cytokine therapy (e.g. interleukin-2 or interferon-alfa) was the standard treatment for metastatic renal cell carcinoma but provided only a small survival advantage (e.g. extending life by a median of 2.5 months).3 A key development has been the introduction of drugs known as receptor tyrosine kinase inhibitors, which include ▾sunitinib (Sutent-Pfizer), ▾sorafenib (Nexavar-Bayer) and ▾pazopanib (Votrient-GlaxoSmithKline). Here we review the evidence on the efficacy, tolerability and cost-effectiveness of these treatments in renal cell carcinoma.
Antonescu C
Gastrointestinal stromal tumors.
Curr Top Microbiol Immunol. 2012; 355:41-57 [PubMed] Related Publications
Gastrointestinal stromal tumors.
Curr Top Microbiol Immunol. 2012; 355:41-57 [PubMed] Related Publications
Gastrointestinal stromal tumor (GIST) is the most common sarcoma of the intestinal tract. Nearly all tumors have a mutation in the KIT or, less often, platelet-derived growth factor receptor (PDGFRA) or B-rapidly Accelerated Fibrosarcoma (BRAF) gene. The discovery of constitutive KIT activation as the central mechanism of GIST pathogenesis, suggested that inhibiting or blocking KIT signaling might be the milestone in the targeted therapy of GISTs. Indeed, imatinib mesylate inhibits KIT kinase activity and represents the front line drug for the treatment of unresectable and advanced GISTs, achieving a partial response or stable disease in about 80% of patients with metastatic GIST. KIT mutation status has a significant impact on treatment response. Patients with the most common exon 11 mutation experience higher rates of tumor shrinkage and prolonged survival, as tumors with an exon 9 mutation or wild-type KIT are less likely to respond to imatinib. Although imatinib achieves a partial response or stable disease in the majority of GIST patients, complete and lasting responses are rare. About half of the patients who initially benefit from imatinib treatment eventually develop drug resistance. The most common mechanism of resistance is through polyclonal acquisition of second site mutations in the kinase domain, which highlights the future therapeutic challenges in salvaging these patients after failing kinase inhibitor monotherapies. More recently, sunitinib (Sutent, Pfizer, New York, NY), which inhibits vascular endothelial growth factor receptor (VEGFR) in addition to KIT and PDGFRA, has proven efficacious in patients who are intolerant or refractory to imatinib. This review summarizes the recent knowledge on targeted therapy in GIST, based on the central role of KIT oncogenic activation, as well as discussing mechanisms of resistance.
Kaushik A, Ho L
Thyroid metastasis from primary renal cell cancer on FDG PET/CT.
Clin Nucl Med. 2011; 36(1):56-8 [PubMed] Related Publications
Thyroid metastasis from primary renal cell cancer on FDG PET/CT.
Clin Nucl Med. 2011; 36(1):56-8 [PubMed] Related Publications
We report the PET/CT appearance of metastasis from primary renal cancer to the thyroid in a 52-year-old man with a history of right renal cell carcinoma, status postright nephrectomy, recently presented biopsied-proven metastatic lesion in his left thyroid lobe. Restaging PET/CT study demonstrates a 1.4 × 0.9 cm hypodense, moderately active lesion in the left thyroid lobe with a maximum SUV of 2.8. No other abnormal hypermetabolic lesion is seen in the right renal surgical bed or the remaining body. The patient has subsequently treated with Sutent (Sunitinib).
Cheng H, Force T
Why do kinase inhibitors cause cardiotoxicity and what can be done about it?
Prog Cardiovasc Dis. 2010 Sep-Oct; 53(2):114-20 [PubMed] Related Publications
Why do kinase inhibitors cause cardiotoxicity and what can be done about it?
Prog Cardiovasc Dis. 2010 Sep-Oct; 53(2):114-20 [PubMed] Related Publications
Cancer growth and metastasis are often driven by activating mutations in, or gene amplications of, specific tyrosine or serine/threonine kinases. Kinase inhibitors (KIs) promised to provide targeted therapy-specifically inhibiting the causal or contributory kinases driving tumor progression while leaving function of other kinases intact. These inhibitors are of 2 general classes: (1) monoclonal antibodies that are typically directed against receptor tyrosine kinases or their ligands and (2) small molecules targeting specific kinases. The latter will be the focus of this review. This class of therapeutics has had some remarkable successes, including revolutionizing the treatment of some malignancies (eg, imatinib [Gleevec] in the management of chronic myeloid leukemia) and adding significantly to the management of other difficult to treat cancers (eg, sunitinib [Sutent] and sorafenib [Nexavar] in the management of renal cell carcinoma). But in some instances, cardiotoxicity, often manifest as left ventricular dysfunction and/or heart failure, has ensued after the use of KIs in patients. Herein we will explore the mechanisms underlying the cardiotoxicity of small-molecule KIs, hoping to explain how and why this happens, and will further examine strategies to deal with the problem.
Jeanniard-Malet O, Gravis G, Caillol F, et al.
Three cases of severe ulcerative esophagitis induced by SUTENT®.
J Gastrointest Cancer. 2012; 43(1):128-30 [PubMed] Related Publications
Three cases of severe ulcerative esophagitis induced by SUTENT®.
J Gastrointest Cancer. 2012; 43(1):128-30 [PubMed] Related Publications
INTRODUCTION: The development of SUTENT® revolutionized the care of metastatic renal carcinoma and of non-operable GIST. The tolerance is quite good with mostly mild side effects grade 1 or 2.
OBSERVATION: We report the case of three severe esophagitis stage 4 responsible for digestive bleeding. Two patients were taking anti-coagulant that could worsen the bleeding, but none were taking either antiplatelet or non-steroidal anti-inflammatory or corticosteroid that could favour erosion or ulceration of the digestive mucosa. It seems that SUTENT® is responsible for the digestive bleeding.
DISCUSSION: Cases of esophagitis induced by SUTENT® have already been reported but are rare and of mild severity. Our three cases of esophagitis are severe with SUTENT® treatment as only risk factor and worsened by anti-coagulant treatment for two patients. It might be of interest preventively to treat these patients with inhibitors of proton pump.
OBSERVATION: We report the case of three severe esophagitis stage 4 responsible for digestive bleeding. Two patients were taking anti-coagulant that could worsen the bleeding, but none were taking either antiplatelet or non-steroidal anti-inflammatory or corticosteroid that could favour erosion or ulceration of the digestive mucosa. It seems that SUTENT® is responsible for the digestive bleeding.
DISCUSSION: Cases of esophagitis induced by SUTENT® have already been reported but are rare and of mild severity. Our three cases of esophagitis are severe with SUTENT® treatment as only risk factor and worsened by anti-coagulant treatment for two patients. It might be of interest preventively to treat these patients with inhibitors of proton pump.
Fenton MS, Marion KM, Salem AK, et al.
Sunitinib inhibits MEK/ERK and SAPK/JNK pathways and increases sodium/iodide symporter expression in papillary thyroid cancer.
Thyroid. 2010; 20(9):965-74 [PubMed] Related Publications
Sunitinib inhibits MEK/ERK and SAPK/JNK pathways and increases sodium/iodide symporter expression in papillary thyroid cancer.
Thyroid. 2010; 20(9):965-74 [PubMed] Related Publications
BACKGROUND: Sunitinib malate (Sutent, Pfizer, Inc.; SU11248) is a selective, multitargeted inhibitor of receptor tyrosine kinases and has been shown to inhibit receptors for VEGF, PDGF, KIT, FLT3, and RET. The objective of this study was to determine the effects of sunitinib on signal transduction pathways and on gene expression of iodide-metabolizing proteins in papillary cancer cells with the RET/PTC1 rearrangement.
METHODS: We investigated the effects of sunitinib on cell growth, signal transduction pathways, and thyroid-specific gene expression in papillary thyroid cancer (PTC) cell lines that had the RET/PTC1 rearrangement.
RESULTS: Sunitinib inhibited proliferation of RET/PTC1 subclones in a time- and dose-related manner. The mean 50% lethal concentration in the RET/PTC1 subclones was 1.81 microM. Incubation of RET/PTC1 cells with 1 microM sunitinib inhibited their migration potential and transformed their morphology. Sunitinib inhibited RET autophosphorylation at Y1062 and the activation of signal transducer and activator of transcription 3 by blocking Y705 phosphorylation. Sunitinib caused cell cycle arrest in the G0/G1 phase and dephosphorylation of retinoblastoma protein, but did not induce apoptosis. Western blot analysis of the p38, MEK/ERK, and SAPK/JNK mitogen-activated protein kinase signal transduction pathways showed that sunitinib blocked ERK 1/2 and JNK phosphorylation in the cytoplasm. Sunitinib treatment of RET/PTC1 cell lines, in combination, with forskolin induced expression of the sodium (Na)/iodide (I) symporter (NIS) and the transcription factors that bind the NIS upstream enhancer. Mechanistically, the inhibition of both MEK/ERK and SAPK/JNK cytoplasmic pathways individually and in combination caused an increase in NIS gene expression.
CONCLUSION: Sunitinib appears to target the cytosolic MEK/ERK and SAPK/JNK pathways in the RET/PTC1 cell lines, suggesting that blocking these pathways is at least part of the mechanism by which sunitinib inhibits cell proliferation and causes stimulation of NIS gene expression in RET/PTC1 cells.
METHODS: We investigated the effects of sunitinib on cell growth, signal transduction pathways, and thyroid-specific gene expression in papillary thyroid cancer (PTC) cell lines that had the RET/PTC1 rearrangement.
RESULTS: Sunitinib inhibited proliferation of RET/PTC1 subclones in a time- and dose-related manner. The mean 50% lethal concentration in the RET/PTC1 subclones was 1.81 microM. Incubation of RET/PTC1 cells with 1 microM sunitinib inhibited their migration potential and transformed their morphology. Sunitinib inhibited RET autophosphorylation at Y1062 and the activation of signal transducer and activator of transcription 3 by blocking Y705 phosphorylation. Sunitinib caused cell cycle arrest in the G0/G1 phase and dephosphorylation of retinoblastoma protein, but did not induce apoptosis. Western blot analysis of the p38, MEK/ERK, and SAPK/JNK mitogen-activated protein kinase signal transduction pathways showed that sunitinib blocked ERK 1/2 and JNK phosphorylation in the cytoplasm. Sunitinib treatment of RET/PTC1 cell lines, in combination, with forskolin induced expression of the sodium (Na)/iodide (I) symporter (NIS) and the transcription factors that bind the NIS upstream enhancer. Mechanistically, the inhibition of both MEK/ERK and SAPK/JNK cytoplasmic pathways individually and in combination caused an increase in NIS gene expression.
CONCLUSION: Sunitinib appears to target the cytosolic MEK/ERK and SAPK/JNK pathways in the RET/PTC1 cell lines, suggesting that blocking these pathways is at least part of the mechanism by which sunitinib inhibits cell proliferation and causes stimulation of NIS gene expression in RET/PTC1 cells.
Shin HW, Cho CH, Kim TY, Park JW
Sunitinib deregulates tumor adaptation to hypoxia by inhibiting HIF-1alpha synthesis in HT-29 colon cancer cells.
Biochem Biophys Res Commun. 2010; 398(2):205-11 [PubMed] Related Publications
Sunitinib deregulates tumor adaptation to hypoxia by inhibiting HIF-1alpha synthesis in HT-29 colon cancer cells.
Biochem Biophys Res Commun. 2010; 398(2):205-11 [PubMed] Related Publications
Sunitinib (SU11248, Sutent) is a class III/V receptor tyrosine kinase (RTK) inhibitor that exhibits potent anti-angiogenic and anticancer activities. Preclinical studies demonstrated that the sunitinib effects are attributed to inhibition of VEGFR and PDGFR phosphorylation. However, even in colon cancer cells lacking sunitinib-targeted RTKs, sunitinib effectively inhibits tumor growth in a xenograft model, and this raises a question about the mechanism underlying the in vivo anticancer action of sunitinib. Since hypoxia is a critical microenvironment that tumors face, we addressed the possibility that sunitinib deregulates tumor adaptation to hypoxia. First we found that sunitinib limits the colony growth of HT-29, which is a colon adenocarcinoma cell line lacking the RTKs, and that HIF-1alpha in the colonies is decreased by sunitinib. In cultured HT-29 cells, sunitinib suppressed HIF-1alpha under hypoxic conditions. Moreover, sunitinib repressed the activity of HIF-1alpha and subsequently decreased the expressions of HIF-1 downstream genes. Mechanistically, sunitinib blocked the 5'-UTR-dependent translation of HIF-1alpha. The HIF-1alpha suppression by sunitinib was also reproduced in a VHL-null renal cell carcinoma cell line, where HIF-1alpha is not degradable. In conclusion, the sunitinib inhibition of HIF-1 signaling could restrain tumor progression in hypoxic regions, which may contribute to anticancer effect of sunitinib.
Hanzer M, Nebl A, Spendel S, et al.
Necrosis of a skin autograft after short-term treatment with sunitinib in a 14-year-old girl with metastatic alveolar soft part sarcoma of the thigh.
Klin Padiatr. 2010; 222(3):184-6 [PubMed] Related Publications
Necrosis of a skin autograft after short-term treatment with sunitinib in a 14-year-old girl with metastatic alveolar soft part sarcoma of the thigh.
Klin Padiatr. 2010; 222(3):184-6 [PubMed] Related Publications
A 14-year-old girl was diagnosed with alveolar soft part sarcoma (ASPS) of the thigh and lung metastases. She underwent tumor resection and pulmonary metastasectomy followed by hyperfractionated local radiotherapy (44.8 Gy). A mesh graft transplant was used to cover the postoperative skin defect on the thigh. Since ASPS do not respond to conventional chemotherapy antiangiogenic treatment with peginterferon alfa-2b and thalidomide was started. Immunohistochemical analysis of tumor tissue showed expression of vascular endothelial growth factor receptors (VEGFR) 1, 2, 3, and platelet derived growth factor receptor (PDGFR)-alpha and -beta. Hence, additional treatment with multitargeted receptor tyrosine kinase inhibitor sunitinib (Sutent) was started on a compassionate use basis. 2 weeks later the patient presented with necrosis of the skin transplant requiring necrectomy and skin grafting. This case illustrates that drugs inhibiting vascular endothelial growth factor receptors have to be used very cautiously in cancer patients with severe pre-existing skin damage.
Kroeger N, Gajda M, Zanow J, et al.
Downsizing a tumor thrombus of advanced renal cell carcinoma with neoadjuvant systemic therapy and resulting histopathological effects.
Urol Int. 2010; 84(4):479-84 [PubMed] Related Publications
Downsizing a tumor thrombus of advanced renal cell carcinoma with neoadjuvant systemic therapy and resulting histopathological effects.
Urol Int. 2010; 84(4):479-84 [PubMed] Related Publications
BACKGROUND: We report a treatment option in surgical therapy of locally advanced renal cell carcinoma (RCC).
METHOD: A 63-year-old patient with locally advanced RCC including an atrial thrombus underwent 2 cycles of neoadjuvant therapy (Sutent 50 mg daily for 4 weeks followed by 2 weeks off) and then tumor surgery. Primary surgical therapy had to be delayed because of suspected bronchial carcinoma and additional diagnostics. After neoadjuvant therapy to downsize the tumor thrombus and exclusion of any additional malignant tumors, operation was done via abdominal access; no sternotomy was necessary.
RESULTS: Histopathological examinations of the primary tumor after tyrosine kinase inhibitor therapy were evaluated and compared to tumor biopsy material taken before therapy.
CONCLUSION: Neoadjuvant therapy with Sutent may represent a favorable treatment option in cases of locally advanced clear-cell RCC with extended tumor thrombus.
METHOD: A 63-year-old patient with locally advanced RCC including an atrial thrombus underwent 2 cycles of neoadjuvant therapy (Sutent 50 mg daily for 4 weeks followed by 2 weeks off) and then tumor surgery. Primary surgical therapy had to be delayed because of suspected bronchial carcinoma and additional diagnostics. After neoadjuvant therapy to downsize the tumor thrombus and exclusion of any additional malignant tumors, operation was done via abdominal access; no sternotomy was necessary.
RESULTS: Histopathological examinations of the primary tumor after tyrosine kinase inhibitor therapy were evaluated and compared to tumor biopsy material taken before therapy.
CONCLUSION: Neoadjuvant therapy with Sutent may represent a favorable treatment option in cases of locally advanced clear-cell RCC with extended tumor thrombus.
Escudier B
Sunitinib for the management of advanced renal cell carcinoma.
Expert Rev Anticancer Ther. 2010; 10(3):305-17 [PubMed] Related Publications
Sunitinib for the management of advanced renal cell carcinoma.
Expert Rev Anticancer Ther. 2010; 10(3):305-17 [PubMed] Related Publications
Targeted agents, such as sunitinib (SUTENT((R))) have become central to the management of advanced and/or metastatic renal cell carcinoma (mRCC). Sunitinib is an oral, multitargeted receptor tyrosine kinase inhibitor that has demonstrated efficacy for the treatment of mRCC in multiple clinical trials. In a Phase III trial in previously untreated patients with mRCC, sunitinib was associated with median progression-free survival of 11 months, which was more than double that observed with interferon-alpha (5 months; p < 0.001). As a result, sunitinib is recommended in international treatment guidelines and is considered a reference standard of care in the first-line setting for patients at favorable or intermediate prognostic risk. Sunitinib is generally well tolerated with a predictable adverse-event profile; the majority of adverse events can be managed with standard medical intervention. This paper presents an overview of data supporting the use of sunitinib for mRCC, and considers the optimal management of sunitinib in clinical practice.



 Cancer Prevention and Risk Reduction
Cancer Prevention and Risk Reduction