Found this page useful?
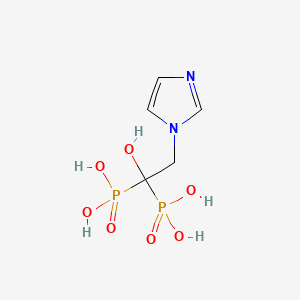
Zoledronic acid (Zometa)
 Web Resources: Zoledronic acid
Web Resources: Zoledronic acid Latest Research Publications
Latest Research PublicationsWeb Resources: Zoledronic acid (7 links)
Cancer Research UK![]() CancerHelp information is examined by both expert and lay reviewers. Content is reviewed every 12 to 18 months. Further info.
CancerHelp information is examined by both expert and lay reviewers. Content is reviewed every 12 to 18 months. Further info.
Macmillan Cancer Support![]() Content is developed by a team of information development nurses and content editors, and reviewed by health professionals. Further info.
Content is developed by a team of information development nurses and content editors, and reviewed by health professionals. Further info.
American Cancer Society
National Cancer Institute
Brief summary
 zoledronic acid - Compound Summary
zoledronic acid - Compound Summary
MedlinePlus
 About ZOMETA® (zoledronic acid)
About ZOMETA® (zoledronic acid)
Novartis Pharmaceuticals Corporation
Latest Research Publications
Liang W, Wang F, Chen Q, et al.
Targeting cathepsin K diminishes prostate cancer establishment and growth in murine bone.
J Cancer Res Clin Oncol. 2019; 145(8):1999-2012 [PubMed] Free Access to Full Article Related Publications
Targeting cathepsin K diminishes prostate cancer establishment and growth in murine bone.
J Cancer Res Clin Oncol. 2019; 145(8):1999-2012 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: The processes of prostate cancer (PCa) invasion and metastasis are facilitated by proteolytic cascade involving multiple proteases, such as matrix metalloproteinases, serine proteases and cysteine proteases including cathepsin K (CatK). CatK is predominantly secreted by osteoclasts and specifically degrades collagen I leading to bone destruction. PCa and breast cancer preferentially metastasize to the bone. Importantly, CatK expression level is greater in PCa bone metastatic sites compared to primary tumor and normal prostate tissues. However, the underlying mechanism of CatK during PCa metastases into the bone remains to be elucidated. We investigated the functional role of CatK during the PCa establishment and growth process in the murine bone.
METHODS: CatK mRNA expression was validated by RT-PCR, protein expression by immunoblotting in PCa LNCaP, C4-2B, and PC3 cells as well as in PCa tissues. Its protein production was measured using ELISA assay. The effect of both knockdowns via siRNA and CatK inhibitor was compared in regard to PCa cell invasion. We further studied the dose-dependent CatK inhibitor effect on conditioned media-induced bone resorption. In setting up an animal model, C4-2B cells were injected into the tibiae of SCID mice. The animals treated with either vehicle or CatK inhibitor for 8 weeks at the time of tumor cell injection (tumor establishment model; protocol I) or 4 weeks after tumor cell injection (tumor progression model; protocol II) were applied to histological and histomorphometric analyses.
RESULTS: We confirmed CatK expression in PCa LNCaP, C4-2B, and PC3 cells as well as in PCa tissues. Furthermore, we observed the inhibitory effects of a selective CatK inhibitor on PCa cell invasion. The CatK inhibitor dose-dependently inhibited PCa-conditioned media-induced bone resorption. Upon injection of C4-2B cells into the tibiae of SCID mice, the selective CatK inhibitor significantly prevented the tumor establishment in protocol I, and reduced the tumor growth in bone in protocol II. It also decreased serum PSA levels in both animal models. The inhibitory effects of the CatK inhibitor were enhanced in combination with zoledronic acid (ZA).
CONCLUSION: The selective CatK inhibitor may prevent the establishment and progression of PCa in bone, thus making it a novel therapeutic approach for advanced PCa.
METHODS: CatK mRNA expression was validated by RT-PCR, protein expression by immunoblotting in PCa LNCaP, C4-2B, and PC3 cells as well as in PCa tissues. Its protein production was measured using ELISA assay. The effect of both knockdowns via siRNA and CatK inhibitor was compared in regard to PCa cell invasion. We further studied the dose-dependent CatK inhibitor effect on conditioned media-induced bone resorption. In setting up an animal model, C4-2B cells were injected into the tibiae of SCID mice. The animals treated with either vehicle or CatK inhibitor for 8 weeks at the time of tumor cell injection (tumor establishment model; protocol I) or 4 weeks after tumor cell injection (tumor progression model; protocol II) were applied to histological and histomorphometric analyses.
RESULTS: We confirmed CatK expression in PCa LNCaP, C4-2B, and PC3 cells as well as in PCa tissues. Furthermore, we observed the inhibitory effects of a selective CatK inhibitor on PCa cell invasion. The CatK inhibitor dose-dependently inhibited PCa-conditioned media-induced bone resorption. Upon injection of C4-2B cells into the tibiae of SCID mice, the selective CatK inhibitor significantly prevented the tumor establishment in protocol I, and reduced the tumor growth in bone in protocol II. It also decreased serum PSA levels in both animal models. The inhibitory effects of the CatK inhibitor were enhanced in combination with zoledronic acid (ZA).
CONCLUSION: The selective CatK inhibitor may prevent the establishment and progression of PCa in bone, thus making it a novel therapeutic approach for advanced PCa.
von Moos R, Costa L, Gonzalez-Suarez E, et al.
Management of bone health in solid tumours: From bisphosphonates to a monoclonal antibody.
Cancer Treat Rev. 2019; 76:57-67 [PubMed] Related Publications
Management of bone health in solid tumours: From bisphosphonates to a monoclonal antibody.
Cancer Treat Rev. 2019; 76:57-67 [PubMed] Related Publications
Patients with solid tumours are at risk of impaired bone health from metastases and cancer therapy-induced bone loss (CTIBL). We review medical management of bone health in patients with solid tumours over the past 30 years, from first-generation bisphosphonates to the receptor activator of nuclear factor κB ligand (RANKL)-targeted monoclonal antibody, denosumab. In the 1980s, first-generation bisphosphonates were shown to reduce the incidence of skeletal-related events (SREs) in patients with breast cancer. Subsequently, more potent second- and third-generation bisphosphonates were developed, particularly zoledronic acid (ZA). Head-to-head studies showed that ZA was significantly more effective than pamidronate for reducing SREs in patients with breast and castrate-resistant prostate cancer (CRPC), becoming the standard of care for more than a decade. The RANKL inhibitor denosumab was licensed in 2010, and head-to-head studies and integrated analyses confirmed its superiority to ZA for preventing SREs, particularly in breast cancer and CRPC. Bisphosphonates and denosumab have also been investigated for prevention of CTIBL in patients receiving hormonal therapy for breast and prostate cancer, and denosumab is licensed in this indication. Despite advances in management of bone health, several issues remain, notably the optimal time to initiate therapy, duration of therapy, and dosing frequency, and how to avoid toxicity, particularly with long-term treatment. In summary, introduction of ZA and denosumab has protected patients with bone metastasis from serious bone complications and improved their quality of life. Ongoing research will hopefully guide the optimal use of these agents to help maintain bone health in patients with solid tumours.
Fong W, To KKW
Drug repurposing to overcome resistance to various therapies for colorectal cancer.
Cell Mol Life Sci. 2019; 76(17):3383-3406 [PubMed] Related Publications
Drug repurposing to overcome resistance to various therapies for colorectal cancer.
Cell Mol Life Sci. 2019; 76(17):3383-3406 [PubMed] Related Publications
Emergence of novel treatment modalities provides effective therapeutic options, apart from conventional cytotoxic chemotherapy, to fight against colorectal cancer. Unfortunately, drug resistance remains a huge challenge in clinics, leading to invariable occurrence of disease progression after treatment initiation. While novel drug development is unfavorable in terms of time frame and costs, drug repurposing is one of the promising strategies to combat resistance. This approach refers to the application of clinically available drugs to treat a different disease. With the well-established safety profile and optimal dosing of these approved drugs, their combination with current cancer therapy is suggested to provide an economical, safe and efficacious approach to overcome drug resistance and prolong patient survival. Here, we review both preclinical and clinical efficacy, as well as cellular mechanisms, of some extensively studied repurposed drugs, including non-steroidal anti-inflammatory drugs, statins, metformin, chloroquine, disulfiram, niclosamide, zoledronic acid and angiotensin receptor blockers. The three major treatment modalities in the management of colorectal cancer, namely classical cytotoxic chemotherapy, molecular targeted therapy and immunotherapy, are covered in this review.
Tesfamariam Y, Jakob T, Wöckel A, et al.
Adjuvant bisphosphonates or RANK-ligand inhibitors for patients with breast cancer and bone metastases: A systematic review and network meta-analysis.
Crit Rev Oncol Hematol. 2019; 137:1-8 [PubMed] Related Publications
Adjuvant bisphosphonates or RANK-ligand inhibitors for patients with breast cancer and bone metastases: A systematic review and network meta-analysis.
Crit Rev Oncol Hematol. 2019; 137:1-8 [PubMed] Related Publications
Bone-modifying agents like bisphosphonates and receptor activator of nuclear factor kappaβ ligand (RANK-L) inhibitors are used as supportive treatments in breast cancer patients with bone metastases to prevent skeletal-related events (SREs). Due to missing head-to-head comparisons, a network meta-analysis was performed to provide a hierarchy of these therapeutic options. Through a systematic literature search, 21 randomized controlled trials (RCTs) that fulfilled the inclusion criteria were identified. To prevent SREs, the ranking through P-scores showed denosumab (RR: 0.62; 95%CI: 0.50-0.76), zoledronic acid (RR: 0.72; 95%CI: 0.61-0.84) and pamidronate (RR: 0.76; 95%CI: 0.67-0.85) to be significantly superior to placebo. Due to insufficient or heterogeneous data, overall survival, quality of life, pain response and adverse events were not able to be analyzed within the network. Although data were sparse on adverse events, the risk of significant adverse events appeared low. The results of this review can therefore be used to formulate clinical studies more precisely in order to standardise and focus on patient-relevant outcomes.
Guo X, Cui J, Zhao Y, et al.
The therapeutic value of cerebrospinal fluid ctDNA detection by next-generation sequencing for meningeal carcinomatosis: a case report.
BMC Neurol. 2019; 19(1):38 [PubMed] Free Access to Full Article Related Publications
The therapeutic value of cerebrospinal fluid ctDNA detection by next-generation sequencing for meningeal carcinomatosis: a case report.
BMC Neurol. 2019; 19(1):38 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: It is usually very complicated to treat meningeal carcinomatosis, and it is important to treat it as soon as possible.
CASE PRESENTATION: The 19-Del mutation was found in the exon for the epidermal growth factor receptor gene in the pleural effusion of a patient on March 11th, 2015. He took 250 mg of oral gefitinib once a day for 11 months beginning in December of 2015. On the 3rd of November 2016, he arrived at the hospital and presented with dizziness, headache and transient blurred vision. At this time, he began to take 4 mg of oral zoledronic acid once a month to prevent bone metastases. The result of a cytology exam of the cerebrospinal fluid showed that the man had meningeal carcinomatosis. The 19-Del mutation and the 20-T790 M mutation in the exon of the epidermal growth factor receptor gene was found by the next generation sequencing of the CSF. Then, he discontinued taking gefitinib and began to take 90-100 mg of oral AZD9291 once a day in November 2016. After adjusting the medication dose based on the NGS, his headache was noticeably reduced, and his condition gradually stabilized.
CONCLUSIONS: Cerebrospinal fluid ctDNA detection by next generation sequencing may become a suitable biomarker to monitor clinical treatment response in meningeal carcinomatosis.
CASE PRESENTATION: The 19-Del mutation was found in the exon for the epidermal growth factor receptor gene in the pleural effusion of a patient on March 11th, 2015. He took 250 mg of oral gefitinib once a day for 11 months beginning in December of 2015. On the 3rd of November 2016, he arrived at the hospital and presented with dizziness, headache and transient blurred vision. At this time, he began to take 4 mg of oral zoledronic acid once a month to prevent bone metastases. The result of a cytology exam of the cerebrospinal fluid showed that the man had meningeal carcinomatosis. The 19-Del mutation and the 20-T790 M mutation in the exon of the epidermal growth factor receptor gene was found by the next generation sequencing of the CSF. Then, he discontinued taking gefitinib and began to take 90-100 mg of oral AZD9291 once a day in November 2016. After adjusting the medication dose based on the NGS, his headache was noticeably reduced, and his condition gradually stabilized.
CONCLUSIONS: Cerebrospinal fluid ctDNA detection by next generation sequencing may become a suitable biomarker to monitor clinical treatment response in meningeal carcinomatosis.
Wen L, Yao J, Valderrama A
Evaluation of Treatment Patterns and Costs in Patients with Prostate Cancer and Bone Metastases.
J Manag Care Spec Pharm. 2019; 25(3-b Suppl):S1-S11 [PubMed] Related Publications
Evaluation of Treatment Patterns and Costs in Patients with Prostate Cancer and Bone Metastases.
J Manag Care Spec Pharm. 2019; 25(3-b Suppl):S1-S11 [PubMed] Related Publications
BACKGROUND: There are a lack of guideline recommendations for patients with metastatic castration-resistant prostate cancer (mCRPC) undergoing treatment progression and sequencing. Understanding treatment patterns and associated utilization and costs may help inform stakeholders and guide decision making.
OBJECTIVE: To describe treatment patterns and health care costs in prostate cancer (PC) patients with bone metastases treated with agents approved by the FDA for mCRPC.
METHODS: 2 large integrated claims databases (MarketScan and PharMetrics) were used to identify males aged ≥ 18 years who were diagnosed and treated for PC (ICD-9-CM code 185.xx or 233.4) with bone metastases (ICD-9-CM code 198.5) from June 2013 to September 2014. Patients were required to be continuously enrolled for ≥ 6 months before and after initiation of treatment with abiraterone, cabazitaxel, docetaxel, enzalutamide, mitoxantrone, radium-223, sipuleucel-T, or other chemotherapy. Study endpoints included lines of therapy, health care resource utilization per patient per month (PPPM), PPPM costs, and mortality rate. Descriptive analysis was completed for the study sample, and survival function was calculated via Kaplan-Meier estimates.
RESULTS: There were 953 patients meeting all inclusion criteria in the MarketScan database and 565 patients in the PharMetrics database. The median follow-up time was 18 months (interquartile range [IQR] = 14-23) for MarketScan and 14 months (IQR = 11-18) for PharMetrics. Mean age (SD) was 71 (± 10.7) and 66 (± 9.3) years, respectively. Before mCRPC treatment initiation, patients received palliative radiation therapy and bone antiresorptive therapy. For MarketScan and PharMetrics, respectively, 14.0% and 18.2% of patients received radiation therapy, 36.1% and 40.0% received denosumab; 16.5% and 16.8% received zoledronic acid; and 0.2% and 0.8% received pamidronate. Across both databases, abiraterone was the most commonly received bone metastasis treatment agent across all lines of therapy, except fourth line. Radium-223, cabazitaxel, and mitoxantrone were the least utilized therapies. The median cost PPPM during the post-index period was $10,916 (IQR=$5,334-$13,457) in MarketScan and $10,292 (IQR = $7,245-$14,699) in PharMetrics. The cost PPPM during the 6-month pre-index period was $2,643 (IQR = $850-$4,357) in MarketScan and $2,742 (IQR = $1,484-$4,730) in PharMetrics.
CONCLUSIONS: Patients were treated mainly with abiraterone across most lines of care, with radium-223, cabazitaxel, and mitoxantrone as the least utilized therapies. Median costs PPPM increased by approximately $8,900 after initiation of FDA-approved agents for mCRPC, with the largest increase in cost stemming from oral medications.
DISCLOSURES: Funding for this study was provided by Bayer HealthCare Pharmaceuticals. All authors were employees at Bayer HealthCare Pharmaceuticals at the time this study was conducted. This study was presented as a poster at the 2017 American Society of Clinical Oncology (ASCO) Genitourinary Cancers Symposium; February 16-18, 2017; Orlando, FL.
OBJECTIVE: To describe treatment patterns and health care costs in prostate cancer (PC) patients with bone metastases treated with agents approved by the FDA for mCRPC.
METHODS: 2 large integrated claims databases (MarketScan and PharMetrics) were used to identify males aged ≥ 18 years who were diagnosed and treated for PC (ICD-9-CM code 185.xx or 233.4) with bone metastases (ICD-9-CM code 198.5) from June 2013 to September 2014. Patients were required to be continuously enrolled for ≥ 6 months before and after initiation of treatment with abiraterone, cabazitaxel, docetaxel, enzalutamide, mitoxantrone, radium-223, sipuleucel-T, or other chemotherapy. Study endpoints included lines of therapy, health care resource utilization per patient per month (PPPM), PPPM costs, and mortality rate. Descriptive analysis was completed for the study sample, and survival function was calculated via Kaplan-Meier estimates.
RESULTS: There were 953 patients meeting all inclusion criteria in the MarketScan database and 565 patients in the PharMetrics database. The median follow-up time was 18 months (interquartile range [IQR] = 14-23) for MarketScan and 14 months (IQR = 11-18) for PharMetrics. Mean age (SD) was 71 (± 10.7) and 66 (± 9.3) years, respectively. Before mCRPC treatment initiation, patients received palliative radiation therapy and bone antiresorptive therapy. For MarketScan and PharMetrics, respectively, 14.0% and 18.2% of patients received radiation therapy, 36.1% and 40.0% received denosumab; 16.5% and 16.8% received zoledronic acid; and 0.2% and 0.8% received pamidronate. Across both databases, abiraterone was the most commonly received bone metastasis treatment agent across all lines of therapy, except fourth line. Radium-223, cabazitaxel, and mitoxantrone were the least utilized therapies. The median cost PPPM during the post-index period was $10,916 (IQR=$5,334-$13,457) in MarketScan and $10,292 (IQR = $7,245-$14,699) in PharMetrics. The cost PPPM during the 6-month pre-index period was $2,643 (IQR = $850-$4,357) in MarketScan and $2,742 (IQR = $1,484-$4,730) in PharMetrics.
CONCLUSIONS: Patients were treated mainly with abiraterone across most lines of care, with radium-223, cabazitaxel, and mitoxantrone as the least utilized therapies. Median costs PPPM increased by approximately $8,900 after initiation of FDA-approved agents for mCRPC, with the largest increase in cost stemming from oral medications.
DISCLOSURES: Funding for this study was provided by Bayer HealthCare Pharmaceuticals. All authors were employees at Bayer HealthCare Pharmaceuticals at the time this study was conducted. This study was presented as a poster at the 2017 American Society of Clinical Oncology (ASCO) Genitourinary Cancers Symposium; February 16-18, 2017; Orlando, FL.
Thavarajah M, Jayaram R
Uncommon presentation of medication-related osteonecrosis of the mandible in a patient with metastatic prostate cancer.
BMJ Case Rep. 2019; 12(2) [PubMed] Related Publications
Uncommon presentation of medication-related osteonecrosis of the mandible in a patient with metastatic prostate cancer.
BMJ Case Rep. 2019; 12(2) [PubMed] Related Publications
An 82-year-old man with a background of prostate carcinoma and bony metastases presented with bilateral discharging neck fistulae. Two years prior to presentation, the patient had been treated with intravenous zoledronic acid for 1 year as part of chemotherapy. Intraoral examination revealed extensive bilateral medication-related osteonecrosis, with orocutaneous fistulae within the neck. Treatment comprised removal of loose necrotic bone sequestrae, debridement of the fistulae and long-term administration of antibiotics, vitamin E and pentoxifylline. Four weeks later, the orocutaneous fistulae had healed.
Liu H, Wang SH, Chen SC, et al.
Zoledronic acid blocks the interaction between breast cancer cells and regulatory T-cells.
BMC Cancer. 2019; 19(1):176 [PubMed] Free Access to Full Article Related Publications
Zoledronic acid blocks the interaction between breast cancer cells and regulatory T-cells.
BMC Cancer. 2019; 19(1):176 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Zoledronic acid (ZA), a nitrogen-containing bisphosphonate, inhibits osteoclastogenesis. Emerging evidence suggests that ZA has anti-tumor and anti-metastatic properties for breast cancer cells. In a mouse model of ZA-related osteonecrosis of the jaw, ZA administration was found to suppress regulatory T-cells (Tregs) function. Our previous reports also demonstrated ZA acted as an immune modulator to block Tregs. Manipulation of Tregs represents a new strategy for cancer treatment. However, the relationship among ZA, Tregs, and cancer cells remains unclear. In this study, we investigated the effects of ZA on the interaction of breast cancer cells and Tregs.
METHODS: The anti-tumor effect of ZA on triple negative breast cancer cell lines were validated by XTT, wound healing and apoptosis analysis. A flow cytometry-based assay was used to analyze the immunosuppressive effect of Tregs treated with media conditioned by breast cancer cells, and a transwell assay was used to evaluate the chemotactic migration of Tregs. Differential gene expression profile on MDA-MB-231 treated with ZA (25 μM) was analyzed by. microarrays to describe the molecular basis of actions of ZA for possible direct anti-tumor effects. Enzyme-linked immunosorbent assays and quantitative real-time PCR were used to investigate the effect of ZA on the expression of cytokines/factors by breast cancer cells.
RESULTS: ZA was found to inhibit the proliferation and migration of breast cancer cells. Media conditioned by the MDA-MB-231 cells promoted the expansion, chemotactic migration, and immunosuppressive activity of Tregs, and these effects were attenuated in a dose-dependent manner by ZA treatment, and the attenuation was due to reduced expression of selected breast cancer cell factors (CCL2, CCL5, and IDO).
CONCLUSIONS: ZA can significantly affect the interaction between breast cancer cells and Tregs. Our findings indicate that ZA is a potential therapeutic agent that can be used to reduce cancer aggressiveness by abolishing the supportive role of Tregs.
METHODS: The anti-tumor effect of ZA on triple negative breast cancer cell lines were validated by XTT, wound healing and apoptosis analysis. A flow cytometry-based assay was used to analyze the immunosuppressive effect of Tregs treated with media conditioned by breast cancer cells, and a transwell assay was used to evaluate the chemotactic migration of Tregs. Differential gene expression profile on MDA-MB-231 treated with ZA (25 μM) was analyzed by. microarrays to describe the molecular basis of actions of ZA for possible direct anti-tumor effects. Enzyme-linked immunosorbent assays and quantitative real-time PCR were used to investigate the effect of ZA on the expression of cytokines/factors by breast cancer cells.
RESULTS: ZA was found to inhibit the proliferation and migration of breast cancer cells. Media conditioned by the MDA-MB-231 cells promoted the expansion, chemotactic migration, and immunosuppressive activity of Tregs, and these effects were attenuated in a dose-dependent manner by ZA treatment, and the attenuation was due to reduced expression of selected breast cancer cell factors (CCL2, CCL5, and IDO).
CONCLUSIONS: ZA can significantly affect the interaction between breast cancer cells and Tregs. Our findings indicate that ZA is a potential therapeutic agent that can be used to reduce cancer aggressiveness by abolishing the supportive role of Tregs.
Li S, Chen P, Pei Y, et al.
Addition of Zoledronate to Chemotherapy in Patients with Osteosarcoma Treated with Limb-Sparing Surgery: A Phase III Clinical Trial.
Med Sci Monit. 2019; 25:1429-1438 [PubMed] Free Access to Full Article Related Publications
Addition of Zoledronate to Chemotherapy in Patients with Osteosarcoma Treated with Limb-Sparing Surgery: A Phase III Clinical Trial.
Med Sci Monit. 2019; 25:1429-1438 [PubMed] Free Access to Full Article Related Publications
BACKGROUND Zoledronate has anti-bone resorption activity and is reported to reduce skeletal-related events. The objective of this study was to test the hypothesis that addition of zoledronate in chemotherapy is safe and effective in osteosarcoma. MATERIAL AND METHODS A total of 798 patients, age 25 years and above, with newly diagnosed high-grade surgically salvageable malignant osteosarcoma, were included in the trial. All patients had received standard chemotherapies (n=399). In addition, in a standard chemotherapy regimen, patients enrolled in the zoledronate group also received 10 courses of 4 mg intravenous infusions of zoledronate (n=399). Limb-sparing surgery was performed by orthopedic surgeons (n=798). Clinical assessment, laboratory monitoring, overall survival, event-free survival, and treatment-emergent adverse effects were evaluated. The chi-square independence-samples test was used for statistical analysis at 95% confidence level. RESULTS The histopathological response was the same for both groups (p=0.12). Addition of zoledronate to chemotherapy improved skeletal event-free survival (p=0.04) but decreased overall survival (p=0.02). Zoledronate induced hypocalcemia (p<0.0001), hypophosphatemia (p<0.0001), cardiotoxicity (p<0.0001), lung metastases (p=0.03), flu-like syndrome (p<0.0001), and ototoxicity (p=0.02), and elevated serum aspartate aminotransferase (p<0.0001) and serum alanine aminotransferase (p<0.0001). CONCLUSIONS The addition of zoledronate to standard chemotherapy in high-grade resectable osteosarcoma is detrimental and is not advised.
Wang L, Liu Y, Zhou Y, et al.
Zoledronic acid inhibits the growth of cancer stem cell derived from cervical cancer cell by attenuating their stemness phenotype and inducing apoptosis and cell cycle arrest through the Erk1/2 and Akt pathways.
J Exp Clin Cancer Res. 2019; 38(1):93 [PubMed] Free Access to Full Article Related Publications
Zoledronic acid inhibits the growth of cancer stem cell derived from cervical cancer cell by attenuating their stemness phenotype and inducing apoptosis and cell cycle arrest through the Erk1/2 and Akt pathways.
J Exp Clin Cancer Res. 2019; 38(1):93 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Zoledronic acid is the most potent osteoclast inhibitor and is widely used for advanced cancer patients with bone metastasis, but its role on cancer stem cells (CSCs) remains unclear. In the present study, we aimed to identify the stemness phenotypic characteristics of CSCs derived from cervical cancer cells and explore the anti-cancer efficiency of zoledronic acid on these cells, as well as the possible molecular mechanisms.
METHODS: Stemness phenotypic identification of cervical cancer cells derived CSCs was performed via sphere formation efficiency (SFE), tumorigenesis, immunofluorescence staining, Transwell assay, and western blot. Anti-cancer efficiency of zoledronic acid on these cells (including proliferation, stemness phenotype, apoptosis, and cell cycle) was carried out through MTT assay, SFE, transwell, DAPI staining, flow cytometry, immunofluorescence, TUNEL staining, and western blot, both in vitro and in vivo.
RESULTS: Enhanced self-renewal ability, including SFE and tumorigenesis, was verified in cervical cancer cells derived CSCs compared to parental cervical cancer cells. Specifically, the expression of ALDH1, Sox2, CD49f, Nanog, and Oct4 was significantly up-regulated in cervical cancer cells derived CSCs. Furthermore, enhanced migratory ability was observed in these cells along with up-regulated N-cadherin and Vimentin and down-regulated E-cadherin. Zoledronic acid inhibited cervical cancer cells derived CSCs proliferation in vitro and in vivo. The stemness phenotype of these CSCs including tumor sphere formation, migration, as well as the expression of the aforementioned associated markers was also suppressed. In addition, zoledronic acid significantly induced apoptosis and cell cycle arrest of cervical cancer cells derived CSCs in a dose-dependent manner. Mechanistically, the expression of phosphorylated Erk1/2 and Akt was significantly increased in cervical cancer cells derived CSCs compared to parental cervical cancer cells. Zoledronic acid inhibited phosphorylated Erk1/2 and Akt in cervical cancer cells derived CSCs. IGF-1, a potent stimulator for Erk1/2 and PI3K/Akt, attenuated the aforementioned anti-cancer effect of zoledronic acid.
CONCLUSIONS: Zoledronic acid inhibited the growth of cervical cancer cells derived CSCs through attenuating their stemness phenotype, inducing apoptosis, and arresting cell cycle. The suppression of phosphorylated Erk1/2 and Akt was involved in this process.
METHODS: Stemness phenotypic identification of cervical cancer cells derived CSCs was performed via sphere formation efficiency (SFE), tumorigenesis, immunofluorescence staining, Transwell assay, and western blot. Anti-cancer efficiency of zoledronic acid on these cells (including proliferation, stemness phenotype, apoptosis, and cell cycle) was carried out through MTT assay, SFE, transwell, DAPI staining, flow cytometry, immunofluorescence, TUNEL staining, and western blot, both in vitro and in vivo.
RESULTS: Enhanced self-renewal ability, including SFE and tumorigenesis, was verified in cervical cancer cells derived CSCs compared to parental cervical cancer cells. Specifically, the expression of ALDH1, Sox2, CD49f, Nanog, and Oct4 was significantly up-regulated in cervical cancer cells derived CSCs. Furthermore, enhanced migratory ability was observed in these cells along with up-regulated N-cadherin and Vimentin and down-regulated E-cadherin. Zoledronic acid inhibited cervical cancer cells derived CSCs proliferation in vitro and in vivo. The stemness phenotype of these CSCs including tumor sphere formation, migration, as well as the expression of the aforementioned associated markers was also suppressed. In addition, zoledronic acid significantly induced apoptosis and cell cycle arrest of cervical cancer cells derived CSCs in a dose-dependent manner. Mechanistically, the expression of phosphorylated Erk1/2 and Akt was significantly increased in cervical cancer cells derived CSCs compared to parental cervical cancer cells. Zoledronic acid inhibited phosphorylated Erk1/2 and Akt in cervical cancer cells derived CSCs. IGF-1, a potent stimulator for Erk1/2 and PI3K/Akt, attenuated the aforementioned anti-cancer effect of zoledronic acid.
CONCLUSIONS: Zoledronic acid inhibited the growth of cervical cancer cells derived CSCs through attenuating their stemness phenotype, inducing apoptosis, and arresting cell cycle. The suppression of phosphorylated Erk1/2 and Akt was involved in this process.
Finianos A, Aragon-Ching JB
Zoledronic acid for the treatment of prostate cancer.
Expert Opin Pharmacother. 2019; 20(6):657-666 [PubMed] Related Publications
Zoledronic acid for the treatment of prostate cancer.
Expert Opin Pharmacother. 2019; 20(6):657-666 [PubMed] Related Publications
INTRODUCTION: Prostate cancer remains the most common solid tumor afflicting men in the developed world. Metastatic prostate cancer is a source of great morbidity and mortality especially due to osseous involvement that gives rise to significant symptoms of pain or pathologic fractures or cord compression. Bisphosphonates had been widely used in the treatment of metastatic prostate bone metastases given their demonstrated benefit with a delay of skeletal-related events (SREs) but without prostate-specific antigen (PSA) response or overall survival benefit. Areas covered: In this review, the authors summarize the available literature on the clinical studies that led to the development and regulatory approval of zoledronic acid in men with metastatic prostate cancer. The authors also provide their expert opinion and future perspectives on this therapeutic. Expert opinion: Zoledronic acid is an established adjunctive treatment and bone-targeted therapy for the supportive care of men with metastatic castration-resistant prostate cancer. Efforts to study its utility in earlier phases of metastatic hormone-sensitive prostate cancer has not shown superior outcomes compared with standard androgen deprivation therapy (ADT) or docetaxel alone.
Domae E, Hirai Y, Ikeo T, et al.
Human Vγ9Vδ2 T cells show potent antitumor activity against zoledronate-sensitized OSCC cell lines.
J BUON. 2018; 23(7):132-138 [PubMed] Related Publications
Human Vγ9Vδ2 T cells show potent antitumor activity against zoledronate-sensitized OSCC cell lines.
J BUON. 2018; 23(7):132-138 [PubMed] Related Publications
PURPOSE: Vγ9Vδ2 T cells exhibit potent antitumor effects against multiple types of tumors in preclinical models. In the present study, we examined whether human Vγ9Vδ2 T cells can be effective against oral squamous cell carcinoma (OSCC) cell lines in vitro because the interaction between OSCC and Vγ9Vδ2 T cells has not been explored previously.
METHODS: Eight OSCC cell lines were analyzed for their expression of ligands that potentially activate Vγ9Vδ2 T cells. Vγ9Vδ2 T cells were expanded in vitro from peripheral blood mononuclear cells (PBMCs) using zoledronate and IL-2. Expanded Vγ9Vδ2 T cells were tested for IFNγ production and cytotoxicity in response to zoledronate-treated OSCC cell lines. Flow cytometry was used to obtain and analyze data.
RESULTS: All OSCC cell lines expressed CD277. The cell lines also expressed at least one type of NKG2D ligand. Zoledronate-treated OSCC cell lines induced IFNγ expression in Vγ9Vδ2 T cells. We thus found that Vγ9Vδ2 T cells efficiently kill zoledronate-sensitized OSCC cell lines.
CONCLUSIONS: We found that zoledronate-treated OSCC cell lines are effectively killed by Vγ9Vδ2 T cells. Our results indicate that developing Vγ9Vδ2 T cell-based immunotherapy will be promising in treating patients with OSCC.
METHODS: Eight OSCC cell lines were analyzed for their expression of ligands that potentially activate Vγ9Vδ2 T cells. Vγ9Vδ2 T cells were expanded in vitro from peripheral blood mononuclear cells (PBMCs) using zoledronate and IL-2. Expanded Vγ9Vδ2 T cells were tested for IFNγ production and cytotoxicity in response to zoledronate-treated OSCC cell lines. Flow cytometry was used to obtain and analyze data.
RESULTS: All OSCC cell lines expressed CD277. The cell lines also expressed at least one type of NKG2D ligand. Zoledronate-treated OSCC cell lines induced IFNγ expression in Vγ9Vδ2 T cells. We thus found that Vγ9Vδ2 T cells efficiently kill zoledronate-sensitized OSCC cell lines.
CONCLUSIONS: We found that zoledronate-treated OSCC cell lines are effectively killed by Vγ9Vδ2 T cells. Our results indicate that developing Vγ9Vδ2 T cell-based immunotherapy will be promising in treating patients with OSCC.
Suto A, Kudo D, Yoshida E, et al.
Increase of Tumor Infiltrating γδ T-cells in Pancreatic Ductal Adenocarcinoma Through Remodeling of the Extracellular Matrix by a Hyaluronan Synthesis Suppressor, 4-Methylumbelliferone.
Pancreas. 2019; 48(2):292-298 [PubMed] Related Publications
Increase of Tumor Infiltrating γδ T-cells in Pancreatic Ductal Adenocarcinoma Through Remodeling of the Extracellular Matrix by a Hyaluronan Synthesis Suppressor, 4-Methylumbelliferone.
Pancreas. 2019; 48(2):292-298 [PubMed] Related Publications
OBJECTIVES: Desmoplastic changes of extracellular matrix (ECM) containing large amounts of hyaluronan (HA) are of interest in chemo- and immunoresistance of pancreatic ductal adenocarcinoma (PDAC). The goal of this study was to evaluate the effects of 4-methylumbelliferone (MU), a selective inhibitor of HA, on ECM and to examine how MU affects adoptive immunotherapy.
METHODS: The effect of MU on cell proliferation, HA synthesis and formation of ECM were investigated in four PDAC cell lines. In addition, the cytotoxicity of γδ T-cell-rich peripheral blood mononuclear cells (PBMCs) collected from healthy donors and stimulated with zoledronate and interleukin-2 was examined in the presence of MU. The amount of HA and tumor-infiltrating lymphocytes were also investigated in mice xenograft models.
RESULTS: In vitro, 1.0 mM MU inhibited cell proliferation by 45-70% and HA synthesis by 55-80% in all four PDAC cell lines, and enhanced γδ T-cell-rich PBMC-mediated cytotoxicity against PDAC cells. In vivo, MU reduced intratumoral HA and promoted infiltration of inoculated γδ T-cells into tumor tissue, and consequently suppressed tumor growth.
CONCLUSIONS: 4-methylumbelliferone may be an effective immunosensitizer against PDAC through induction of structural changes in the ECM.
METHODS: The effect of MU on cell proliferation, HA synthesis and formation of ECM were investigated in four PDAC cell lines. In addition, the cytotoxicity of γδ T-cell-rich peripheral blood mononuclear cells (PBMCs) collected from healthy donors and stimulated with zoledronate and interleukin-2 was examined in the presence of MU. The amount of HA and tumor-infiltrating lymphocytes were also investigated in mice xenograft models.
RESULTS: In vitro, 1.0 mM MU inhibited cell proliferation by 45-70% and HA synthesis by 55-80% in all four PDAC cell lines, and enhanced γδ T-cell-rich PBMC-mediated cytotoxicity against PDAC cells. In vivo, MU reduced intratumoral HA and promoted infiltration of inoculated γδ T-cells into tumor tissue, and consequently suppressed tumor growth.
CONCLUSIONS: 4-methylumbelliferone may be an effective immunosensitizer against PDAC through induction of structural changes in the ECM.
Yap KK, Wong W, Ji L, et al.
Impact of timing of administration of bone supportive therapy on pain palliation from radium-223.
Cancer Treat Res Commun. 2019; 18:100114 [PubMed] Related Publications
Impact of timing of administration of bone supportive therapy on pain palliation from radium-223.
Cancer Treat Res Commun. 2019; 18:100114 [PubMed] Related Publications
BACKGROUND: Skeletal-related events cause significant morbidity in patients with metastatic castration-resistant prostate cancer. In the ALSYMPCA study, radium-223 (Ra223) was found to provide pain palliation in addition to prolonged survival and reduced skeletal-related events (SREs). Given previous evidence that bisphosphonates impacted pain relief from the radiopharmaceutical samarium-153, we evaluated whether the timing of bone supportive therapy (BST) such as zoledronic acid or denosumab affected pain palliation from Ra223.
METHODS: We identified patients who received Ra223 at University of Southern California or Mayo Clinic Arizona. Patients were evaluable for pain response if they had baseline pain score > 0 and at least 1 pain score documented after Ra223 with pain medication use data. Patients were evaluable for pain flare if they had known baseline pain score and at least 2 pain scores documented after Ra223. Pain response was defined as > 2 point decrease in pain on a 10-point scale; flare was defined as > 2 point increase followed by return to baseline or lower.
RESULTS: Of 65 patients, 22 (34%) received BST. Median number of doses Ra223 was 5 (range 2-6). Fourteen patients were evaluable for pain response and 34 for pain flare. Eighteen patients received concurrent abiraterone (abi) or enzalutamide (enza), and 16 did not. Pain response occurred in 6/6 (100%) patients who received BST within 1 month prior to first Ra223 dose and 4/8 (50%) patients who did not receive BST. Pain flare occurred in 6/21 patients (29%) without BST and 2/13 (15%) with BST (p = 0.44). 6/10 (60%) patients with pain response had a decline in alkaline phosphatase (ALP) level, but there was no consistent pattern of ALP changes in patients with flare. 8/8 patients with pain response had no PSA decline. 6/8 (75%) and 2/18 (11%) patients on abi/enza had pain response and flare respectively, and 4/6 (67%) and 6/16 (38%) patients without concurrent abi/enza had response/flare.
CONCLUSIONS: BST within 1 month prior to first Ra223 dose was associated with increased likelihood of pain palliation and might prevent pain flare. Concurrent use of abi/enza was not associated with increased likelihood of pain response but was associated with decreased likelihood of pain flare.
METHODS: We identified patients who received Ra223 at University of Southern California or Mayo Clinic Arizona. Patients were evaluable for pain response if they had baseline pain score > 0 and at least 1 pain score documented after Ra223 with pain medication use data. Patients were evaluable for pain flare if they had known baseline pain score and at least 2 pain scores documented after Ra223. Pain response was defined as > 2 point decrease in pain on a 10-point scale; flare was defined as > 2 point increase followed by return to baseline or lower.
RESULTS: Of 65 patients, 22 (34%) received BST. Median number of doses Ra223 was 5 (range 2-6). Fourteen patients were evaluable for pain response and 34 for pain flare. Eighteen patients received concurrent abiraterone (abi) or enzalutamide (enza), and 16 did not. Pain response occurred in 6/6 (100%) patients who received BST within 1 month prior to first Ra223 dose and 4/8 (50%) patients who did not receive BST. Pain flare occurred in 6/21 patients (29%) without BST and 2/13 (15%) with BST (p = 0.44). 6/10 (60%) patients with pain response had a decline in alkaline phosphatase (ALP) level, but there was no consistent pattern of ALP changes in patients with flare. 8/8 patients with pain response had no PSA decline. 6/8 (75%) and 2/18 (11%) patients on abi/enza had pain response and flare respectively, and 4/6 (67%) and 6/16 (38%) patients without concurrent abi/enza had response/flare.
CONCLUSIONS: BST within 1 month prior to first Ra223 dose was associated with increased likelihood of pain palliation and might prevent pain flare. Concurrent use of abi/enza was not associated with increased likelihood of pain response but was associated with decreased likelihood of pain flare.
Murata T, Kutsuna T, Kurohara K, et al.
Evaluation of a New Hydroxyapatite Nanoparticle as a Drug Delivery System to Oral Squamous Cell Carcinoma Cells.
Anticancer Res. 2018; 38(12):6715-6720 [PubMed] Related Publications
Evaluation of a New Hydroxyapatite Nanoparticle as a Drug Delivery System to Oral Squamous Cell Carcinoma Cells.
Anticancer Res. 2018; 38(12):6715-6720 [PubMed] Related Publications
BACKGROUND/AIM: Due to its abilities of substance adsorption and intracellular transportation, hydroxyapatite is a potential carrier in drug delivery systems (DDS). This in vitro study investigated whether newly-developed, highly-dispersive calcined hydroxyapatite nanoparticles with an average grain diameter of 20 nm (nano-SHAP) were suitable as a DDS for the drugs zoledronic acid (ZA), cisplatin, and carboplatin.
MATERIAL AND METHODS: The effects of drug-bearing nano-SHAP on cell proliferation were assessed using three human oral squamous cell carcinoma cell lines (HSC-4, KOSC, and SAS) and one human breast cancer cell line (MCF-7).
RESULTS: Nano-SHAP alone did not affect proliferation of any cell line until a concentration of 1 μg/ml was reached. Although the effective concentration of ZA in ZA-bearing nano-SHAP differed, it inhibited cell proliferation better than ZA alone. Cisplatin and carboplatin-bearing nano-SHAP had the same effect as these drugs alone.
CONCLUSION: The nano-SHAP system is of potential use as a drug delivery system.
MATERIAL AND METHODS: The effects of drug-bearing nano-SHAP on cell proliferation were assessed using three human oral squamous cell carcinoma cell lines (HSC-4, KOSC, and SAS) and one human breast cancer cell line (MCF-7).
RESULTS: Nano-SHAP alone did not affect proliferation of any cell line until a concentration of 1 μg/ml was reached. Although the effective concentration of ZA in ZA-bearing nano-SHAP differed, it inhibited cell proliferation better than ZA alone. Cisplatin and carboplatin-bearing nano-SHAP had the same effect as these drugs alone.
CONCLUSION: The nano-SHAP system is of potential use as a drug delivery system.
Zhang C, Zhang F, Liang G, et al.
Denosumab versus zoledronic acid for preventing symptomatic skeletal events in Asian postmenopausal women with oestrogen-receptor-positive advanced breast cancer: an outcome analyses with a mean follow-up of 3 years.
BMC Musculoskelet Disord. 2018; 19(1):424 [PubMed] Free Access to Full Article Related Publications
Denosumab versus zoledronic acid for preventing symptomatic skeletal events in Asian postmenopausal women with oestrogen-receptor-positive advanced breast cancer: an outcome analyses with a mean follow-up of 3 years.
BMC Musculoskelet Disord. 2018; 19(1):424 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: The purpose of this study was to evaluate the efficacy of denosumab or zoledronic acid (ZA) using symptomatic skeletal events (SSEs) as the primary endpoint in Asian postmenopausal women with oestrogen-receptor-positive advanced breast cancer.
METHODS: Asian postmenopausal women with oestrogen-receptor-positive advanced breast cancer receiving subcutaneous denosumab 120 mg Q4W, or intravenous ZA 4 mg Q4W until the primary analysis cut-off date were retrospectively analysed in the Hong Kong Practice-Based Cancer Research Center(HKCRC) from March 2011 to March 2013. The time to first on-study SSE that was assessed either clinically or through routine radiographic scans was the primary endpoint.
RESULTS: 242 patients received denosumab or ZA treatment (n = 120, mean age of 64.9 years (SD 3.01) and n = 122, 65.4 years (3.44), respectively). The median times to first on-study SSE were 14.7 months (12.9-45.6) and 11.7 months (9.9-45.6) for denosumab and ZA, respectively (hazard ratio, HR 0.44, 95% CI 0.71-2.95; p = 0·0002). Compared with the ZA group, denosumab-treated patients had a significantly delayed time to first SSE (HR 0.65 [95% CI 0.29-1.45], p < 0.0001). An increased incidence of SSE was found in the 16-month follow-up with rates of 2.1 and 10.7% for denosumab and ZA, respectively (P = 0.033). The difference persisted with time with rates of 8.3 and 17.2% at the final follow-up, respectively (P < 0.05).
CONCLUSION: In postmenopausal women aged ≥60 years with oestrogen-receptor-positive advanced breast cancer, denosumab significantly reduced the risk of developing SSEs compared with ZA. The findings of this pilot trial justify a larger study to determine whether the result is more generally applicable to a broader population.
METHODS: Asian postmenopausal women with oestrogen-receptor-positive advanced breast cancer receiving subcutaneous denosumab 120 mg Q4W, or intravenous ZA 4 mg Q4W until the primary analysis cut-off date were retrospectively analysed in the Hong Kong Practice-Based Cancer Research Center(HKCRC) from March 2011 to March 2013. The time to first on-study SSE that was assessed either clinically or through routine radiographic scans was the primary endpoint.
RESULTS: 242 patients received denosumab or ZA treatment (n = 120, mean age of 64.9 years (SD 3.01) and n = 122, 65.4 years (3.44), respectively). The median times to first on-study SSE were 14.7 months (12.9-45.6) and 11.7 months (9.9-45.6) for denosumab and ZA, respectively (hazard ratio, HR 0.44, 95% CI 0.71-2.95; p = 0·0002). Compared with the ZA group, denosumab-treated patients had a significantly delayed time to first SSE (HR 0.65 [95% CI 0.29-1.45], p < 0.0001). An increased incidence of SSE was found in the 16-month follow-up with rates of 2.1 and 10.7% for denosumab and ZA, respectively (P = 0.033). The difference persisted with time with rates of 8.3 and 17.2% at the final follow-up, respectively (P < 0.05).
CONCLUSION: In postmenopausal women aged ≥60 years with oestrogen-receptor-positive advanced breast cancer, denosumab significantly reduced the risk of developing SSEs compared with ZA. The findings of this pilot trial justify a larger study to determine whether the result is more generally applicable to a broader population.
Cheung FY
Revisiting the role of bone-modifying agents in the management of metastatic prostate cancer.
Asia Pac J Clin Oncol. 2018; 14 Suppl 5:13-15 [PubMed] Related Publications
Revisiting the role of bone-modifying agents in the management of metastatic prostate cancer.
Asia Pac J Clin Oncol. 2018; 14 Suppl 5:13-15 [PubMed] Related Publications
Bone metastases are a hallmark of advanced prostate cancer and may drive the morbidity and mortality of the disease in patients with a poor prognosis. The pathogenesis of bone metastasis involves the interaction between cancer cells, normal bone cells and the bone microenvironment. Targeting the bone microenvironment has become a promising therapy for patients with advanced prostate cancer and bone metastasis. This article reviews the use of the antiresorptive bone-targeted agents zoledronic acid and denosumab in the management of skeletal-related events (SREs) in patients with metastatic castration-resistant prostate cancer (mCRPC) and bone metastasis. In real-world clinical practice, these agents have been widely prescribed as a concomitant medication to novel mCRPC therapies, such as abiraterone, enzalutamide and radium-223. International guidelines have recommended zoledronic acid or denosumab for the prevention of SREs in patients with bone metastasis from mCRPC. Although there is currently no consensus regarding the optimal sequencing between the bone-targeted agents and novel anti-cancer therapies, future optimal treatments for patients with bone metastasis from prostate cancer may involve the combination of these agents.
Montgomery C, Couch C, Emory CL, Nicholas R
Giant Cell Tumor of Bone: Review of Current Literature, Evaluation, and Treatment Options.
J Knee Surg. 2019; 32(4):331-336 [PubMed] Related Publications
Giant Cell Tumor of Bone: Review of Current Literature, Evaluation, and Treatment Options.
J Knee Surg. 2019; 32(4):331-336 [PubMed] Related Publications
Giant cell tumor of bone is a benign albeit aggressive tumor commonly affecting the bones of the knee. Patients with these tumors present with pain, swelling, and inability to bear weight on the involved extremity. These destructive tumors typically arise in the metaphyseal region of the long bones in individuals in the second, third, and fourth generations of life. Histologically, the multinucleated giant cells are the hallmark of the lesion, easily recognized on histological review, which recently have become therapeutic targets for medical management of the disease. For decades, surgical management has been the primary treatment for giant cell tumor of the bone. Some tumors can be treated with excision and filling of the osseous void with bone cement or allograft. This is an effective treatment option with a low to moderate risk of local recurrence while preserving limb function. For more destructive tumors, wide excision and reconstruction with prosthetic, structural allograft or combined allograft prosthetic components are utilized. Advances in medical management of the disease have also demonstrated promise as an effective treatment; however, its use has usually been limited to the treatment of metastatic disease, recurrent disease or when advanced local disease would require surgical treatment felt to be overly morbid.
Choi J, Lee EJ, Yang SH, et al.
A prospective Phase II study for the efficacy of radiotherapy in combination with zoledronic acid in treating painful bone metastases from gastrointestinal cancers.
J Radiat Res. 2019; 60(2):242-248 [PubMed] Free Access to Full Article Related Publications
A prospective Phase II study for the efficacy of radiotherapy in combination with zoledronic acid in treating painful bone metastases from gastrointestinal cancers.
J Radiat Res. 2019; 60(2):242-248 [PubMed] Free Access to Full Article Related Publications
We investigated the efficacy of combined radiotherapy (RT) and zoledronic acid in treating painful bone metastases from gastrointestinal cancers. Sixty patients were prospectively enrolled between November 2014 and July 2016. The most common primary cancer type was hepatocellular carcinoma (HCC, n = 25), followed by colorectal cancer (n = 6). Patients received external beam RT of 30-54 Gy in 10-17 fractions or 20 Gy in 5 fractions for symptomatic bone metastases. On the first day of RT, patients received 4 mg intravenous zoledronic acid, which was repeated monthly for a total of six cycles. The mean pain score before treatment was 6.7, and it decreased to 2.8 at 1 month and 2.1 at 3 months (P < 0.001).The overall pain response rates at 1 and 3 months were 95% and 96%, respectively. Among the 24 patients who underwent magnetic resonance imaging, 71% were responders, with a complete response in 1 patient and partial in 16 patients. Combined treatment significantly decreased levels of macrophage inflammatory protein-1α and matrix metalloproteinase (MMP)-2 and -3 compared with baseline (all P < 0.05). In HCC patients, IL-6 and MMP-9 levels were significantly lower 1 month after treatment (P < 0.05). The mean quality of life (QOL) score improved from 66 to 56 at 1 month (P < 0.001) and 55 at 3 months (P = 0.016). The median survival was 7 months. In conclusion, RT with zoledronic acid decreased bone pain and improved QOL in patients with painful bone metastases from gastrointestinal cancers. Radiographic findings and serum biomarker measurements were closely correlated with therapeutic responses.
Mhaskar R, Djulbegovic B
Bisphosphonates for Patients Diagnosed With Multiple Myeloma.
JAMA. 2018; 320(14):1483-1484 [PubMed] Related Publications
Bisphosphonates for Patients Diagnosed With Multiple Myeloma.
JAMA. 2018; 320(14):1483-1484 [PubMed] Related Publications
Clinical Question: Among patients with multiple myeloma, is bisphosphonate therapy associated with lower rates of mortality, vertebral fractures, nonvertebral fractures, and skeletal-related events compared with placebo or no treatment?
Bottom Line: Among patients with myeloma, bisphosphonates were associated with lower rates of pathological fractures and skeletal-related events compared with placebo or no treatment. Direct meta-analysis showed no association between bisphosphonates and mortality. In network meta-analysis, zoledronate was associated with lower risk of mortality compared with placebo or no treatment.
Bottom Line: Among patients with myeloma, bisphosphonates were associated with lower rates of pathological fractures and skeletal-related events compared with placebo or no treatment. Direct meta-analysis showed no association between bisphosphonates and mortality. In network meta-analysis, zoledronate was associated with lower risk of mortality compared with placebo or no treatment.
Kanellias N, Gavriatopoulou M, Terpos E, Dimopoulos MA
Management of multiple myeloma bone disease: impact of treatment on renal function.
Expert Rev Hematol. 2018; 11(11):881-888 [PubMed] Related Publications
Management of multiple myeloma bone disease: impact of treatment on renal function.
Expert Rev Hematol. 2018; 11(11):881-888 [PubMed] Related Publications
INTRODUCTION: Bone disease (BD) is one of the most common features of multiple myeloma. Seventy to eighty percent of patients at diagnosis present with lytic lesions which may lead to skeletal-related events. Areas covered: The aim of this review is to present the possible adverse profile of bisphosphonates (BPs) on renal function, the underlying mechanisms by which BPs may affect renal function and the novel therapeutic approaches on myeloma bone disease management. Expert commentary: BPs remain the cornerstone in the management of myeloma-related BD. Zoledronic acid and Pamidronate are currently the gold standard, however cannot be used in patients with severe renal dysfunction. Renal impairment is another hallmark of myeloma with approximately 60% of the patients presenting with or developing renal dysfunction during the disease course. Although BPs rarely cause renal impairment, they should be administered with caution in patients with impaired renal function. The exact mechanism by which BPs cause renal impairment is yet to be elucidated. Another promising agent is denosumab, a RANKL inhibitor, which can be administrated regardless of renal function and does not need the relevant dose-adjustments.
Guillot A, Joly C, Barthélémy P, et al.
Denosumab Toxicity When Combined With Anti-angiogenic Therapies on Patients With Metastatic Renal Cell Carcinoma: A GETUG Study.
Clin Genitourin Cancer. 2019; 17(1):e38-e43 [PubMed] Related Publications
Denosumab Toxicity When Combined With Anti-angiogenic Therapies on Patients With Metastatic Renal Cell Carcinoma: A GETUG Study.
Clin Genitourin Cancer. 2019; 17(1):e38-e43 [PubMed] Related Publications
BACKGROUND: About one-third of patients with renal cell carcinoma (RCC) have detectable metastases at diagnosis. Among them, bone is the second most frequent metastatic site. Treatment of metastatic RCC mostly relies on anti-angiogenic (AA) therapies and, more recently, immunotherapy. Skeletal-related events (SREs) can be prevented with bone-targeted therapies such as denosumab (Dmab), which has demonstrated superiority when compared with zoledronic acid in solid tumors. However, there is limited available data on Dmab toxicity in combination with AA therapies in patients with kidney cancer. The objective of this study was to retrospectively analyze the toxicity profile (mainly osteonecrosis of the jaw [ONJ] and hypocalcemia) in patients with metastatic renal cell carcinoma (mRCC) treated with Dmab and AA therapy combination.
PATIENTS AND METHODS: We conducted a multicenter retrospective study among centers from the French Groupe d'Etudes des Tumeurs Uro Genitales (GETUG). Patients with bone metastases who received concurrently or sequentially AA therapy and Dmab were included in this study.
RESULTS: A total of 41 patients with mRCC were enrolled. Although no patient presented with severe hypocalcemia, ONJ occurred in 7 (17%) of 41 patients. Interestingly, all patients with ONJ received the Dmab and AA combination in the first line of treatment; among these patients, 3 patients had no risk factor other than the Dmab and AA combination.
CONCLUSION: The incidence of ONJ was high in this real-life population of patients with mRCC treated with AA therapies combined with Dmab. This toxicity signal should warn physicians about this combination in the mRCC population.
PATIENTS AND METHODS: We conducted a multicenter retrospective study among centers from the French Groupe d'Etudes des Tumeurs Uro Genitales (GETUG). Patients with bone metastases who received concurrently or sequentially AA therapy and Dmab were included in this study.
RESULTS: A total of 41 patients with mRCC were enrolled. Although no patient presented with severe hypocalcemia, ONJ occurred in 7 (17%) of 41 patients. Interestingly, all patients with ONJ received the Dmab and AA combination in the first line of treatment; among these patients, 3 patients had no risk factor other than the Dmab and AA combination.
CONCLUSION: The incidence of ONJ was high in this real-life population of patients with mRCC treated with AA therapies combined with Dmab. This toxicity signal should warn physicians about this combination in the mRCC population.
Body JJ, von Moos R, Niepel D, Tombal B
Hypocalcaemia in patients with prostate cancer treated with a bisphosphonate or denosumab: prevention supports treatment completion.
BMC Urol. 2018; 18(1):81 [PubMed] Free Access to Full Article Related Publications
Hypocalcaemia in patients with prostate cancer treated with a bisphosphonate or denosumab: prevention supports treatment completion.
BMC Urol. 2018; 18(1):81 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Most patients with advanced prostate cancer develop bone metastases, which often result in painful and debilitating skeletal-related events. Inhibitors of bone resorption, such as bisphosphonates and denosumab, can each reduce the incidence of skeletal-related events and delay the progression of bone pain. However, these agents are associated with an increased risk of hypocalcaemia, which, although often mild and transient, can be serious and life-threatening. Here we provide practical advice on managing the risk of hypocalcaemia in patients with advanced prostate cancer who are receiving treatment with bone resorption inhibitors. Relevant references for this review were identified through searches of PubMed with the search terms 'prostate cancer', 'bone-targeted agents', 'anti-resorptive agents', 'bisphosphonates', 'zoledronic acid', 'denosumab', 'hypocalcaemia', and 'hypocalcemia'. Additional references were suggested by the authors.
MAIN TEXT: Among patients with advanced cancer receiving a bisphosphonate or denosumab, hypocalcaemia occurs most frequently in those with prostate cancer, although it can occur in patients with any tumour type. Consistent with its greater ability to inhibit bone resorption, denosumab has shown superiority in the prevention of skeletal-related events in patients with bone metastases from solid tumours. Consequently, denosumab is more likely to induce hypocalcaemia than the bisphosphonates. Likewise, various bisphosphonates have differing potencies for the inhibition of bone resorption, and thus the risk of hypocalcaemia varies between different bisphosphonates. Other risk factors for the development of hypocalcaemia include the presence of osteoblastic metastases, vitamin D deficiency, and renal insufficiency. Hypocalcaemia can lead to treatment interruption, but it is both preventable and manageable. Serum calcium concentrations should be measured, and any pre-existing hypocalcaemia should be corrected, before starting treatment with inhibitors of bone resorption. Once treatment has started, concomitant administration of calcium and vitamin D supplements is essential. Calcium concentrations should be monitored during treatment with bisphosphonates or denosumab, particularly in patients at high risk of hypocalcaemia. If hypocalcaemia is diagnosed, patients should receive treatment with calcium and vitamin D.
CONCLUSION: With preventative strategies and treatment, patients with prostate cancer who are at risk of, or who develop, hypocalcaemia should be able to continue to benefit from treatment with bisphosphonates or denosumab.
MAIN TEXT: Among patients with advanced cancer receiving a bisphosphonate or denosumab, hypocalcaemia occurs most frequently in those with prostate cancer, although it can occur in patients with any tumour type. Consistent with its greater ability to inhibit bone resorption, denosumab has shown superiority in the prevention of skeletal-related events in patients with bone metastases from solid tumours. Consequently, denosumab is more likely to induce hypocalcaemia than the bisphosphonates. Likewise, various bisphosphonates have differing potencies for the inhibition of bone resorption, and thus the risk of hypocalcaemia varies between different bisphosphonates. Other risk factors for the development of hypocalcaemia include the presence of osteoblastic metastases, vitamin D deficiency, and renal insufficiency. Hypocalcaemia can lead to treatment interruption, but it is both preventable and manageable. Serum calcium concentrations should be measured, and any pre-existing hypocalcaemia should be corrected, before starting treatment with inhibitors of bone resorption. Once treatment has started, concomitant administration of calcium and vitamin D supplements is essential. Calcium concentrations should be monitored during treatment with bisphosphonates or denosumab, particularly in patients at high risk of hypocalcaemia. If hypocalcaemia is diagnosed, patients should receive treatment with calcium and vitamin D.
CONCLUSION: With preventative strategies and treatment, patients with prostate cancer who are at risk of, or who develop, hypocalcaemia should be able to continue to benefit from treatment with bisphosphonates or denosumab.
Han J, Han L, Zhang L, et al.
Comparison of clinical effect in treatment of bone tumor between zoledronic acid needle and ibandronate needle.
Pak J Pharm Sci. 2018; 31(4(Special)):1683-1686 [PubMed] Related Publications
Comparison of clinical effect in treatment of bone tumor between zoledronic acid needle and ibandronate needle.
Pak J Pharm Sci. 2018; 31(4(Special)):1683-1686 [PubMed] Related Publications
To observe and analyze the clinical effect of zoledronic acid needle and ibandronate needle in treatment of bone tumor. 100 patients who have been treated in our hospital for bone tumor were selected as research objects. They were randomly divided into research group and control group, each containing 50 patients. The research group was applied with ibandronate needle therapy, while the control group was given with zeledronic acid needle therapy. After treatment, the clinical effects of the two groups were observed and analyzed. Through comparing the pain relief rate after treatment between the two groups, it can be known that the pain relief rate of research group was relatively higher, P<0.05; the rate of adverse effect in research group was relatively lower, P<0.05; the quality of life score (QLS) of research group was significantly superior to that of control group, P<0.05. theibandronate needle therapy is a more reliable and superior method in treatment of bone tumor compared with zoledronic acid needle therapy, which should be promoted in clinical treatment.
Wang T, Zhang L, Han L, et al.
Clinical effect of intravenous infusion of zoledronic acid combined with oral medication of cinobufagin in the treatment of metastatic bone tumors.
Pak J Pharm Sci. 2018; 31(4(Special)):1609-1612 [PubMed] Related Publications
Clinical effect of intravenous infusion of zoledronic acid combined with oral medication of cinobufagin in the treatment of metastatic bone tumors.
Pak J Pharm Sci. 2018; 31(4(Special)):1609-1612 [PubMed] Related Publications
Aim of the study was to observe and analyze the clinical effect of intravenous infusion of zoledronic acid combined with oral medication of cinobufagin in treating metastatic bone tumors. The 120 patients who have been treated in the hospital for metastatic bone tumor from June 2014 to June 2017 were selected as research objects. They were randomly divided into research group and control group, each containing 60. The research group was treated with intravenous infusion of zoledronic acid combined with oral medication of cinobufagin. In the control group, only zoledronic acid intravenous infusion was administered. The overall treatment effect of the two groups was observed. The pain of two groups was evaluated using numerical rating scale (NRS). The results showed that compared with the control group, the research group achieved better clinical effect and had a higher quality of life, and the intergroup difference was of statistical significance, P<0.05. There was no difference in rate of adverse reactions between the two groups, P>0.05, without statistical significance. The combined therapy of intravenous infusion of zoledronic acid and oral medication of cinobufagin can obtain better therapeutic effect in treating metastatic bone tumors.
Wazzan T, Kashtwari D, Almaden WF, et al.
Radiographic bone loss and the risk of medication-related osteonecrosis of the jaw (MRONJ) in multiple myeloma patients-A retrospective case control study.
Spec Care Dentist. 2018; 38(6):356-361 [PubMed] Related Publications
Radiographic bone loss and the risk of medication-related osteonecrosis of the jaw (MRONJ) in multiple myeloma patients-A retrospective case control study.
Spec Care Dentist. 2018; 38(6):356-361 [PubMed] Related Publications
Risk factors for medication-related osteonecrosis of the jaws (MRONJ) include type and duration of antiresorptive drugs, dental trauma, local anatomy, systemic underlying conditions and therapy, smoking, and the presence of periodontal disease. However, there is a lack of studies elucidating the role of periodontal disease as risk predictor. In the present study, the dental charts of 100 multiple myeloma (MM) patients and 16 MM patients who developed MRONJ were studied. Information about age, gender, smoking history, diabetes, steroid drug intake, type and duration of bisphosphonate (BP) treatments, MRONJ status, missing teeth, periapical lesions, widening of the periodontal ligament, and periodontal status was collected. The periodontal status was determined as a percentage of missing bone at the mesial and distal surfaces of each tooth. Multivariable logistic regression was performed to identify risk factors associated with MRONJ. In the selected model, using the COX analysis, categorical bone loss percentage is significantly associated with MRONJ (P = 0.009), with hazard ratio 0.042 (high vs low) and 95% CI 0.004 to 0.453. Gender, steroid, Aredia BP type, and periapical are also significant in selected model. In conclusion, advanced alveolar bone loss and missing teeth were strongly related to the occurrence of MRONJ in MM patients.
de Fonseka D, Morley A, Stadon L, et al.
Zoledronic acid in the management of mesothelioma - a feasibility study (Zol-A Trial): study protocol for a randomised controlled trial.
Trials. 2018; 19(1):467 [PubMed] Free Access to Full Article Related Publications
Zoledronic acid in the management of mesothelioma - a feasibility study (Zol-A Trial): study protocol for a randomised controlled trial.
Trials. 2018; 19(1):467 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Nitrogen containing bisphosphonates such as zoledronic acid (ZA) are known to contain certain anti-cancer properties. These have been investigated in the past in various cancers such as breast, prostate and colon. ZA in particular has shown promising results in pre-clinical studies. We propose a multicentre double-blind randomised controlled feasibility study to assess the recruitment and acceptability of ZA/placebo alongside chemotherapy in malignant pleural mesothelioma (MPM).
METHODS: Patients will be recruited for a 13-month period from October 2016 to November 2017. Eligible patients will be identified via the regional mesothelioma multidisciplinary team meeting. Those who receive chemotherapy will be randomised to receive either ZA or placebo alongside their chemotherapy. Those who decline chemotherapy will be offered to join the trial on the non-randomised open-labelled arm of the trial. Patients will receive a maximum of six cycles of ZA/placebo, at three-weekly cycles. All patients will be followed up for six months from randomisation. Semi-structured interviews to gather data on acceptability of trial procedures, tolerability of ZA and other relevant information will take place after the participants have completed their six cycles of treatment. For a better understanding about non-participation in mesothelioma trials we also aim to interview those who decline to take part in the trial.
DISCUSSION: The qualitative and quantitative data gathered in this feasibility trial will hopefully pave the way to designing a robust full phase III trial to investigate the potential synergistic effect of ZA and current standard treatment for MPM, cisplatin-pemetrexed combination chemotherapy.
TRIAL REGISTRATION: ISRCTN Registry, ISRCTN45536692 . Registered on 9 August 2016. EudraCT no. 2015-004433-26.
METHODS: Patients will be recruited for a 13-month period from October 2016 to November 2017. Eligible patients will be identified via the regional mesothelioma multidisciplinary team meeting. Those who receive chemotherapy will be randomised to receive either ZA or placebo alongside their chemotherapy. Those who decline chemotherapy will be offered to join the trial on the non-randomised open-labelled arm of the trial. Patients will receive a maximum of six cycles of ZA/placebo, at three-weekly cycles. All patients will be followed up for six months from randomisation. Semi-structured interviews to gather data on acceptability of trial procedures, tolerability of ZA and other relevant information will take place after the participants have completed their six cycles of treatment. For a better understanding about non-participation in mesothelioma trials we also aim to interview those who decline to take part in the trial.
DISCUSSION: The qualitative and quantitative data gathered in this feasibility trial will hopefully pave the way to designing a robust full phase III trial to investigate the potential synergistic effect of ZA and current standard treatment for MPM, cisplatin-pemetrexed combination chemotherapy.
TRIAL REGISTRATION: ISRCTN Registry, ISRCTN45536692 . Registered on 9 August 2016. EudraCT no. 2015-004433-26.
Wu C, Chen W, Huang X, et al.
Effect of Diphosphonates on Bone Mineral Density in Men Receiving Androgen Deprivation Therapy for Prostate Cancer.
Clin Genitourin Cancer. 2018; 16(6):e1243-e1250 [PubMed] Related Publications
Effect of Diphosphonates on Bone Mineral Density in Men Receiving Androgen Deprivation Therapy for Prostate Cancer.
Clin Genitourin Cancer. 2018; 16(6):e1243-e1250 [PubMed] Related Publications
Patients receiving androgen deprivation therapy are associated with increasing loss of bone mineral density (BMD) and higher risk of skeletal-related events. We reviewed and analyzed the influence of diphosphonates on BMD change. A systemic literature research was conducted in PubMed and related bibliographies. The focus of data extraction was BMD percentage change of lumbar spine, total hip, and femoral neck after 12 months. Standardized mean difference (SMD) was pooled with the random-effects model, and metaregression and subgroup analysis were performed to explore heterogeneity. Nine articles (n = 920) were included and finally analyzed after screening 118 articles. We found significant improvement in BMD percentage changes of the lumbar spine, total hip, and femoral neck at 1 year (respectively, SMD = 6.379, 95% confidence interval [CI] = 3.740-9.018, P < .001, I
Dumas M, Laly P, Gottlieb J, et al.
Osteopenia and fractures associated with long-term therapy with MEK inhibitors.
Melanoma Res. 2018; 28(6):641-644 [PubMed] Related Publications
Osteopenia and fractures associated with long-term therapy with MEK inhibitors.
Melanoma Res. 2018; 28(6):641-644 [PubMed] Related Publications
Targeted therapies have markedly improved the survival of patients with melanoma. We report the case of two patients with advanced melanoma controlled by long-term MEK inhibitor or combination of BRAF and MEK inhibitors, who developed fractures related to severe osteopenia. A 48-year-old woman was treated by pimasertib after the failure of two lines of chemotherapy, and a 42-year-old man was treated by an association of BRAFi (dabrafenib) and MEKi (trametinib) after the failure of one line of chemotherapy. During follow-up, both complained of buttock pain, revealing primary fractures of the pelvis and lumbar vertebra. In both patients, none had osteoporosis risk factors; DEXA scan revealed osteopenia, and analysis ruled out metastatic bone lesion or secondary osteoporosis. Zoledronic acid, cholecalciferol (vitamin D3), oral calcium, and pain killers were introduced, leading to no further bone event. Numerous pathways are involved in the homeostasis of bone turnover, and the effect of tyrosine kinase inhibitors on those pathways is not well known yet. The absence of usual causes of osteoporosis or metastatic bone lesion and kinetics of symptoms lead us to suggest that MEK inhibitors were responsible for the development of osteoporosis. To the best of our knowledge, this is the first report of fractures associated with osteopenia in patients treated with MEKi. Long-term survival owing to new targeted treatment could be associated with yet underestimated adverse effects such as osteopenia/osteoporosis that could impair patient's quality of life and should be investigated.
Seider MJ, Pugh SL, Langer C, et al.
Randomized phase III trial to evaluate radiopharmaceuticals and zoledronic acid in the palliation of osteoblastic metastases from lung, breast, and prostate cancer: report of the NRG Oncology RTOG 0517 trial.
Ann Nucl Med. 2018; 32(8):553-560 [PubMed] Article available free on PMC after 01/10/2019 Related Publications
Randomized phase III trial to evaluate radiopharmaceuticals and zoledronic acid in the palliation of osteoblastic metastases from lung, breast, and prostate cancer: report of the NRG Oncology RTOG 0517 trial.
Ann Nucl Med. 2018; 32(8):553-560 [PubMed] Article available free on PMC after 01/10/2019 Related Publications
BACKGROUND: Skeletal-related events (SREs), common sequelae of metastatic cancer, are reduced by bisphosphonates. In this study, it was postulated that radiopharmaceuticals, added to bisphosphonates, could further decrease the incidence of SREs.
METHODS: NRG Oncology RTOG 0517 randomized patients with breast, lung, and prostate cancer and blastic bone metastases to either zoledronic acid (ZA) alone or ZA plus radiopharmaceuticals (Sr-89 or Sm-153). The primary endpoint was time to development of SREs. Secondary objectives included quality of life (QOL), pain control, overall survival (OS), and toxicity.
RESULTS: 261 patients (median age 68; 62% male; 55% prostate, 35% breast, 10% lung) were accrued between July 2006 and February 2011. The study closed early due to a lower than expected rate of SREs. 52 (42%) patients in the ZA arm and 49 (40%) in the radiopharmaceutical arm experienced an SRE. Median time free of SREs was 29.9 and 27.4 months, respectively (p = 0.84). Median OS in the ZA arm and radiopharmaceutical arms was 32.1 and 26.9 months, respectively (p = 0.37). Cox proportional hazards regression model showed that primary disease site (lung) and number of bone metastases (> 2) had a negative impact on OS (p < 0.0001, p = 0.01, respectively). The addition of radiopharmaceuticals to ZA led to a significant reduction in pain at 1 month based on BPI worst score (p = 0.02). No other group differences were noted for QOL or toxicity.
CONCLUSION: The addition of radiopharmaceuticals to bisphosphonates did not alter time to SREs or OS for patients with breast, lung, prostate cancers and blastic bone metastases, although it was associated with significant pain reduction at 1 month.
CLINICAL TRIAL REGISTRY: This protocol (RTOG 0517) is registered with ClinicalTrials.gov (NCT00365105), and may be viewed online at http://www.clinicaltrials.gov/ct2/show/NCT00365105?term=RTOG+0517&rank=1 .
METHODS: NRG Oncology RTOG 0517 randomized patients with breast, lung, and prostate cancer and blastic bone metastases to either zoledronic acid (ZA) alone or ZA plus radiopharmaceuticals (Sr-89 or Sm-153). The primary endpoint was time to development of SREs. Secondary objectives included quality of life (QOL), pain control, overall survival (OS), and toxicity.
RESULTS: 261 patients (median age 68; 62% male; 55% prostate, 35% breast, 10% lung) were accrued between July 2006 and February 2011. The study closed early due to a lower than expected rate of SREs. 52 (42%) patients in the ZA arm and 49 (40%) in the radiopharmaceutical arm experienced an SRE. Median time free of SREs was 29.9 and 27.4 months, respectively (p = 0.84). Median OS in the ZA arm and radiopharmaceutical arms was 32.1 and 26.9 months, respectively (p = 0.37). Cox proportional hazards regression model showed that primary disease site (lung) and number of bone metastases (> 2) had a negative impact on OS (p < 0.0001, p = 0.01, respectively). The addition of radiopharmaceuticals to ZA led to a significant reduction in pain at 1 month based on BPI worst score (p = 0.02). No other group differences were noted for QOL or toxicity.
CONCLUSION: The addition of radiopharmaceuticals to bisphosphonates did not alter time to SREs or OS for patients with breast, lung, prostate cancers and blastic bone metastases, although it was associated with significant pain reduction at 1 month.
CLINICAL TRIAL REGISTRY: This protocol (RTOG 0517) is registered with ClinicalTrials.gov (NCT00365105), and may be viewed online at http://www.clinicaltrials.gov/ct2/show/NCT00365105?term=RTOG+0517&rank=1 .

 Prostate Cancer
Prostate Cancer