Found this page useful?
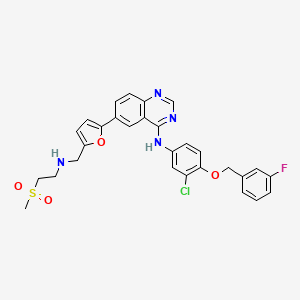
Lapatinib (Tyverb)
 Web Resources: Lapatinib (Tyverb)
Web Resources: Lapatinib (Tyverb) Latest Research Publications
Latest Research PublicationsWeb Resources: Lapatinib (Tyverb) (7 links)
Elsevier
An international, multidisciplinary journal which is focused on advancing research in the treatment and survivorship issues of older adults with cancer.
MedlinePlus.gov
NHS Evidence
PubChem
Macmillan Cancer Support
Cancer Research UK
Irish Cancer Society
Latest Research Publications
Kroeze SG, Fritz C, Hoyer M, et al.
Toxicity of concurrent stereotactic radiotherapy and targeted therapy or immunotherapy: A systematic review.
Cancer Treat Rev. 2017; 53:25-37 [PubMed] Related Publications
Toxicity of concurrent stereotactic radiotherapy and targeted therapy or immunotherapy: A systematic review.
Cancer Treat Rev. 2017; 53:25-37 [PubMed] Related Publications
BACKGROUND AND PURPOSE: Both stereotactic radiotherapy (SRT) and immune- or targeted therapy play an increasingly important role in personalized treatment of metastatic disease. Concurrent application of both therapies is rapidly expanding in daily clinical practice. In this systematic review we summarize severe toxicity observed after concurrent treatment.
MATERIAL AND METHODS: PubMed and EMBASE databases were searched for English literature published up to April 2016 using keywords "radiosurgery", "local ablative therapy", "gamma knife" and "stereotactic", combined with "bevacizumab", "cetuximab", "crizotinib", "erlotinib", "gefitinib", "ipilimumab", "lapatinib", "sorafenib", "sunitinib", "trastuzumab", "vemurafenib", "PLX4032", "panitumumab", "nivolumab", "pembrolizumab", "alectinib", "ceritinib", "dabrafenib", "trametinib", "BRAF", "TKI", "MEK", "PD1", "EGFR", "CTLA-4" or "ALK". Studies performing SRT during or within 30days of targeted/immunotherapy, reporting severe (⩾Grade 3) toxicity were included.
RESULTS: Concurrent treatment is mostly well tolerated in cranial SRT, but high rates of severe toxicity were observed for the combination with BRAF-inhibitors. The relatively scarce literature on extra-cranial SRT shows a potential risk of increased toxicity when SRT is combined with EGFR-targeting tyrosine kinase inhibitors and bevacizumab, which was not observed for cranial SRT.
CONCLUSIONS: This review gives a best-possible overview of current knowledge and its limitations and underlines the need for a timely generation of stronger evidence in this rapidly expanding field.
MATERIAL AND METHODS: PubMed and EMBASE databases were searched for English literature published up to April 2016 using keywords "radiosurgery", "local ablative therapy", "gamma knife" and "stereotactic", combined with "bevacizumab", "cetuximab", "crizotinib", "erlotinib", "gefitinib", "ipilimumab", "lapatinib", "sorafenib", "sunitinib", "trastuzumab", "vemurafenib", "PLX4032", "panitumumab", "nivolumab", "pembrolizumab", "alectinib", "ceritinib", "dabrafenib", "trametinib", "BRAF", "TKI", "MEK", "PD1", "EGFR", "CTLA-4" or "ALK". Studies performing SRT during or within 30days of targeted/immunotherapy, reporting severe (⩾Grade 3) toxicity were included.
RESULTS: Concurrent treatment is mostly well tolerated in cranial SRT, but high rates of severe toxicity were observed for the combination with BRAF-inhibitors. The relatively scarce literature on extra-cranial SRT shows a potential risk of increased toxicity when SRT is combined with EGFR-targeting tyrosine kinase inhibitors and bevacizumab, which was not observed for cranial SRT.
CONCLUSIONS: This review gives a best-possible overview of current knowledge and its limitations and underlines the need for a timely generation of stronger evidence in this rapidly expanding field.
Joensuu H
Escalating and de-escalating treatment in HER2-positive early breast cancer.
Cancer Treat Rev. 2017; 52:1-11 [PubMed] Related Publications
Escalating and de-escalating treatment in HER2-positive early breast cancer.
Cancer Treat Rev. 2017; 52:1-11 [PubMed] Related Publications
The current standard adjuvant systemic treatment of early HER2-positive breast cancer consists of chemotherapy plus 12months of trastuzumab, with or without endocrine therapy. Several trials have investigated modifications of the standard treatment that are shorter and less resource-demanding (de-escalation) or regimens that aim at dual HER2 inhibition or include longer than 12months of HER2-targeted treatment (escalation). Seven randomized trials investigate shorter than 12months of trastuzumab treatment duration. The shorter durations were not statistically inferior to the 1-year duration in the 3 trials with survival results available, but 2 of the trials were small and 1 had a relatively short follow-up time of the patients at the time of reporting. The pathological complete response (pCR) rates were numerically higher in all 9 randomized trials that compared chemotherapy plus dual HER2 inhibition consisting of trastuzumab plus either lapatinib, neratinib, or pertuzumab with chemotherapy plus trastuzumab as neoadjuvant treatments, but the superiority of chemotherapy plus dual HER2-inhibition over chemotherapy plus trastuzumab remains to be demonstrated in the adjuvant setting. One year of adjuvant trastuzumab was as effective as 2years of trastuzumab in the HERA trial, and was associated with fewer side-effects. Extending 1-year adjuvant trastuzumab treatment with 1year of neratinib improved disease-free survival in the ExteNET trial, but the patient follow-up times are still short, and no overall survival benefit was reported. Several important trials are expected to report results in the near future and may modify the current standard.
Azadi S, Tafazzoli-Shadpour M, Omidvar R, et al.
Epidermal growth factor receptor targeting alters gene expression and restores the adhesion function of cancerous cells as measured by single cell force spectroscopy.
Mol Cell Biochem. 2016; 423(1-2):129-139 [PubMed] Related Publications
Epidermal growth factor receptor targeting alters gene expression and restores the adhesion function of cancerous cells as measured by single cell force spectroscopy.
Mol Cell Biochem. 2016; 423(1-2):129-139 [PubMed] Related Publications
Loss of cell-cell adhesion function is a common characteristic of many human epithelial carcinomas that is frequently due to loss of E-cadherin expression. In cancer progression, loss of E-cadherin is associated with invasion and metastasis potential, hence restoration of its function may contribute to the metastasis inhibition. This study examined effect of Epidermal Growth Factor Receptor (EGFR/Her1) blockade on the E-cadherin expression, cellular adherence, and cell elasticity in two human epithelial cancer cell lines, MCF7 and A431. EGFR blocking agents as antibodies or small molecules target EGFR directly. Furthermore, due to intracellular signaling pathways they influence cell behavior and activities. The idea here is to investigate the effect of reduced activity of this signaling pathway using anti-EGFR Antibody (Cetuximab) and tyrosine kinase inhibitor (Lapatinib) on cell-cell adhesion and cell mechanical properties. Real-Time PCR analysis demonstrated that treatment of cells with considered drugs increased the expression of E-cadherin gene among samples. The atomic force microscopy-based single cell force spectroscopy technique was used to measure adhesive force of cancerous cells. Results indicated that inhibition of EGFR activity elevated cell-cell adhesion force, accompanied by stiffening of the cell bodies. In summary, Cetuximab and Lapatinib have been found to mediate cell-cell adhesion by restoration of E-cadherin expression and function. Our data suggest possible therapeutic potential for inhibition of metastasis via the blockade of EGFR signaling.
Zhang C, Xu B, Liu P
Addition of the p110α inhibitor BYL719 overcomes targeted therapy resistance in cells from Her2-positive-PTEN-loss breast cancer.
Tumour Biol. 2016; 37(11):14831-14839 [PubMed] Related Publications
Addition of the p110α inhibitor BYL719 overcomes targeted therapy resistance in cells from Her2-positive-PTEN-loss breast cancer.
Tumour Biol. 2016; 37(11):14831-14839 [PubMed] Related Publications
Breast cancer is one of the leading causes of death for women worldwide. Among various subtypes of breast cancer, human epidermal growth factor receptor 2 (HER2)-positive and phosphatase and tensin homolog (PTEN) loss breast cancer is a cause of great concern in terms of its resistance to HER2-targeted therapies and its poor prognosis. Phosphatidylinositol 3-kinase (PI3K)/AKT hyperphosphorylation is considered one of key mechanisms leading to this resistance, thus combination therapy of PI3K inhibitors and HER2 antibodies is promising for overcoming this problem, and more specific regimens should be designed in this age of precision medicine. In this study, we established an HER2-positive and PTEN loss cell line and confirmed it by western blot analysis. This cell line and its orthotopic xenograft models were exposed to p110α-specific inhibitor BYL719, p110β-specific inhibitor AZD6482, or pan-PI3K inhibitor BKM120, respectively, and the results showed sensitivity to both BYL719 and BKM120 but not AZD6482, which indicated a p110α-reliance for HER2-positive-PTEN-loss breast cancer. Then, the addition of BYL719 to HER2 antibody greatly reduced tumor growth both in vitro and in vivo, accompanied by inhibited PI3K effector phosphorylation. Therefore, our findings suggest that the combination of p110α-selective inhibitor BYL719 with HER2 antibody could be a potential strategy for more personalized treatment of HER2-posistive-PTEN-loss breast cancer; and in addition, the optimal schedule of this combination therapy needs to be further explored.
Zhang B, Hurvitz S
Long-term outcomes of neoadjuvant treatment of HER2-positive breast cancer.
Clin Adv Hematol Oncol. 2016; 14(7):520-30 [PubMed] Related Publications
Long-term outcomes of neoadjuvant treatment of HER2-positive breast cancer.
Clin Adv Hematol Oncol. 2016; 14(7):520-30 [PubMed] Related Publications
Long-term outcomes for women with a diagnosis of human epidermal growth factor receptor 2 (HER2)-driven early-stage breast cancer have significantly improved since the advent of HER2-targeted therapy. Although the first studies in the early-stage setting focused on the adjuvant use of trastuzumab plus chemotherapy, clinical trials increasingly are using a neoadjuvant design to evaluate novel HER2-targeted therapies. Neoadjuvant therapy downstages locally advanced breast cancer, improves rates of breast conservation, and provides information regarding the responsiveness of a cancer to systemic therapy; in addition, studies have shown that the pathologic response to neoadjuvant therapy is correlated with event-free and overall survival. Given these advantages, multiple studies of neoadjuvant therapy, several of which have reported longer-term outcomes, have been conducted to evaluate HER2-targeted therapies. This review summarizes available data from prior and ongoing neoadjuvant trials in HER2-positive breast cancer, focusing on those studies that have reported not only pathologic response rates but also event-free, disease-free, and/or overall survival. The long-term outcomes associated with the achievement of a pathologic complete response are explored, and the comparisons of pathologic complete response rates, event-free survival, and overall survival reported for different HER2-targeted regimens are reviewed.
Prat A, Cheang MC, Galván P, et al.
Prognostic Value of Intrinsic Subtypes in Hormone Receptor-Positive Metastatic Breast Cancer Treated With Letrozole With or Without Lapatinib.
JAMA Oncol. 2016; 2(10):1287-1294 [PubMed] Related Publications
Prognostic Value of Intrinsic Subtypes in Hormone Receptor-Positive Metastatic Breast Cancer Treated With Letrozole With or Without Lapatinib.
JAMA Oncol. 2016; 2(10):1287-1294 [PubMed] Related Publications
Importance: The value of the intrinsic subtypes of breast cancer (luminal A, luminal B, human epidermal growth factor receptor 2 [currently known as ERBB2, but referred to as HER2 in this study]-enriched, and basal-like) in the metastatic setting is currently unknown.
Objective: To evaluate the association of the intrinsic subtypes of breast cancer with outcome and/or benefit in hormone receptor (HR)-positive metastatic breast cancer.
Design, Setting, and Participants: Unplanned retrospective analysis of 821 tumor samples (85.7% primary and 14.3% metastatic) from the EGF30008 phase 3 clinical trial (NCT00073528), in which postmenopausal women with HR-positive invasive breast cancer and no prior therapy for advanced or metastatic disease were randomized to letrozole with or without lapatinib, an epidermal growth factor receptor (EGFR)/HER2 tyrosine kinase inhibitor. Tumor samples were classified into each subtype using the research-based PAM50 classifier. Prior neoadjuvant/adjuvant antiestrogen therapy was allowed. Patients with extensive symptomatic visceral disease were excluded. Treatment effects were evaluated using interaction tests.
Main Outcomes and Measures: Primary and secondary end points were progression-free survival and overall survival.
Results: The median (range) age was 62 (31-94) years. Intrinsic subtype was the strongest prognostic factor independently associated with progression-free survival and overall survival in all patients, and in patients with HER2-negative (n = 644) or HER2-positive (n = 157) diseases. Median progression-free survival differed across the intrinsic subtypes of clinically HER2-negative disease: luminal A (16.9 [95% CI, 14.1-19.9] months), luminal B (11.0 [95% CI, 9.6-13.6] months), HER2-enriched (4.7 [95% CI, 2.7-10.8] months), and basal-like (4.1 [95% CI, 2.5-13.8] months). Median OS also differed across the intrinsic subtypes: luminal A (45 [95% CI, 41-not applicable {NA}] months), luminal B (37 [95% CI, 31-42] months), HER2-enriched (16 [95% CI, 10-NA] months), and basal-like (23 [95% CI, 12-NA] months). Patients with HER2-negative/HER2-enriched disease benefited from lapatinib therapy (median PFS, 6.49 vs 2.60 months; progression-free survival hazard ratio, 0.238 [95% CI, 0.066-0.863]; interaction P = .02).
Conclusions and Relevance: This is the first study to reveal an association between intrinsic subtype and outcome in first-line HR-positive metastatic breast cancer. Patients with HR-positive/HER2-negative disease with a HER2-enriched profile may benefit from lapatinib in combination with endocrine therapy. The clinical value of intrinsic subtyping in hormone receptor-positive metastatic breast cancer warrants further investigation, but patients with luminal A/HER2-negative metastatic breast cancer might be good candidates for letrozole monotherapy in the first-line setting regardless of visceral disease and number of metastases.
Objective: To evaluate the association of the intrinsic subtypes of breast cancer with outcome and/or benefit in hormone receptor (HR)-positive metastatic breast cancer.
Design, Setting, and Participants: Unplanned retrospective analysis of 821 tumor samples (85.7% primary and 14.3% metastatic) from the EGF30008 phase 3 clinical trial (NCT00073528), in which postmenopausal women with HR-positive invasive breast cancer and no prior therapy for advanced or metastatic disease were randomized to letrozole with or without lapatinib, an epidermal growth factor receptor (EGFR)/HER2 tyrosine kinase inhibitor. Tumor samples were classified into each subtype using the research-based PAM50 classifier. Prior neoadjuvant/adjuvant antiestrogen therapy was allowed. Patients with extensive symptomatic visceral disease were excluded. Treatment effects were evaluated using interaction tests.
Main Outcomes and Measures: Primary and secondary end points were progression-free survival and overall survival.
Results: The median (range) age was 62 (31-94) years. Intrinsic subtype was the strongest prognostic factor independently associated with progression-free survival and overall survival in all patients, and in patients with HER2-negative (n = 644) or HER2-positive (n = 157) diseases. Median progression-free survival differed across the intrinsic subtypes of clinically HER2-negative disease: luminal A (16.9 [95% CI, 14.1-19.9] months), luminal B (11.0 [95% CI, 9.6-13.6] months), HER2-enriched (4.7 [95% CI, 2.7-10.8] months), and basal-like (4.1 [95% CI, 2.5-13.8] months). Median OS also differed across the intrinsic subtypes: luminal A (45 [95% CI, 41-not applicable {NA}] months), luminal B (37 [95% CI, 31-42] months), HER2-enriched (16 [95% CI, 10-NA] months), and basal-like (23 [95% CI, 12-NA] months). Patients with HER2-negative/HER2-enriched disease benefited from lapatinib therapy (median PFS, 6.49 vs 2.60 months; progression-free survival hazard ratio, 0.238 [95% CI, 0.066-0.863]; interaction P = .02).
Conclusions and Relevance: This is the first study to reveal an association between intrinsic subtype and outcome in first-line HR-positive metastatic breast cancer. Patients with HR-positive/HER2-negative disease with a HER2-enriched profile may benefit from lapatinib in combination with endocrine therapy. The clinical value of intrinsic subtyping in hormone receptor-positive metastatic breast cancer warrants further investigation, but patients with luminal A/HER2-negative metastatic breast cancer might be good candidates for letrozole monotherapy in the first-line setting regardless of visceral disease and number of metastases.
Martin M, López-Tarruella S
Emerging Therapeutic Options for HER2-Positive Breast Cancer.
Am Soc Clin Oncol Educ Book. 2016; 35:e64-70 [PubMed] Related Publications
Emerging Therapeutic Options for HER2-Positive Breast Cancer.
Am Soc Clin Oncol Educ Book. 2016; 35:e64-70 [PubMed] Related Publications
The natural history of HER2-positive breast cancer has progressively improved since the introduction of the first anti-HER2 directed therapy (trastuzumab). Trastuzumab has significantly increased survival of patients with HER2-positive metastatic breast cancer and, after the standardization of the use of this drug in the adjuvant setting in 2005, has also avoided many disease recurrences and, consequently, saved many lives. Later on, the introduction of lapatinib offered new choices for patients with advanced HER2-positive breast cancer, although the drug has failed to show a clear efficacy in the adjuvant setting. New promising drugs have been approved to broaden the horizon of HER2-positive breast cancer such as pertuzumab or T-DM1, but we need new options to further improve the management of these diseases. In this review, we cover new strategies that are currently under evaluation for the treatment of patients with HER2-positive breast cancer, including new tyrosine kinase inhibitors (neratinib, ONT-380), new antibody-drug conjugates targeting HER2 (MM-302), and new indications of already approved drugs (T-DM1), as well as the potential dual combinations of anti-HER2 therapy with phosphoinositide 3-kinase/mTOR or cell cycle inhibitors (palbociclib, abemaciclib). Last but not least, we briefly review a new paradigm of emerging approaches that involve the host immune response, HER2 breast cancer vaccines, and other immune strategies, including immune checkpoint inhibition.
Fontanella C, De Carlo E, Cinausero M, et al.
Central nervous system involvement in breast cancer patients: Is the therapeutic landscape changing too slowly?
Cancer Treat Rev. 2016; 46:80-8 [PubMed] Related Publications
Central nervous system involvement in breast cancer patients: Is the therapeutic landscape changing too slowly?
Cancer Treat Rev. 2016; 46:80-8 [PubMed] Related Publications
Central nervous system (CNS) involvement from breast cancer (BC) has been historically considered a relatively rare event. However, the development of new therapeutic strategies with a better control of extra-cranial disease and a longer overall survival (OS) has determined an increased incidence of brain metastases. Patients with HER2-positive or triple negative BC have higher occurrence of CNS involvement than patients with luminal-like disease. Moreover, after development of brain metastases, the prognosis is highly influenced by biological subtype. In patients with multiple brain metastases who experience important neurological symptoms, palliative treatment, with or without whole brain radiation therapy (WBRT), needs to be considered the first step of a multidisciplinary therapeutic approach. Patients with a good performance status and 1-3 brain lesions should be considered for radical surgery; patients technically inoperable with 4-5 metastases smaller than 3cm may undergo stereotactic radiosurgery. The role of systemic therapy in the management of patients with brain metastases is controversial. Preliminary data suggest that systemic therapy after WBRT may improve survival in BC patients with brain lesions. In patients with HER2-positive disease, several retrospective or post hoc analyses showed a longer brain progression-free survival with trastuzumab in combination with or followed by other anti-HER2 drugs (such as pertuzumab, lapatinib, and T-DM1). Until now, no new strategies or drugs are available for triple-negative and luminal-like BC.
Kaczyńska A, Herman-Antosiewicz A
Combination of lapatinib with isothiocyanates overcomes drug resistance and inhibits migration of HER2 positive breast cancer cells.
Breast Cancer. 2017; 24(2):271-280 [PubMed] Related Publications
Combination of lapatinib with isothiocyanates overcomes drug resistance and inhibits migration of HER2 positive breast cancer cells.
Breast Cancer. 2017; 24(2):271-280 [PubMed] Related Publications
BACKGROUND: Lapatinib is a commonly used drug that interrupts signaling from the epidermal growth factor receptors, EGFR and HER2/neu. Long-term exposure to lapatinib during therapy eliminates cells that are sensitive to the drug; however, at the same time it increases probability of lapatinib-resistant cell selection. The aim of this study was to verify whether combinations of lapatinib with one of isothiocyanates (sulforaphane, erucin or sulforaphene), targeting different levels of HER2 signaling pathway, exert stronger cytotoxic effect than therapy targeting the receptor only, using heterogeneous populations consisting of lapatinib-sensitive and lapatinib-resistant breast cancer cells.
METHODS: Lapatinib-sensitive HER2 overproducing SKBR-3 breast cancer cells and their lapatinib-resistant derivatives were combined at different proportions to simulate enrichment of cancer cell population in a drug-resistant fraction during lapatinib therapy. Effects of treatments on cell survival (MTT), apoptosis induction (PARP cleavage), prosurvival signaling (p-Akt, p-S6) as well as cell motility (wound healing assay) and invasion (Boyden chamber assay) were investigated.
RESULTS: Combination of lapatinib with any of isothiocyanates significantly decreased cell viability and inhibited migration of populations consisting of different amounts of drug-sensitive and drug-resistant cells. In case of population entirely composed of lapatinib-resistant cells the most effective was combination of lapatinib with erucin which decreased cell viability and motility, phosphorylation of Akt, S6 and VEGF level more efficiently than each agent alone.
CONCLUSIONS: Combination of lapatinib and isothiocyanates, especially erucin, might be considered as an effective treatment reducing metastatic potential of breast cancer cells, even these with the drug resistance phenotype.
METHODS: Lapatinib-sensitive HER2 overproducing SKBR-3 breast cancer cells and their lapatinib-resistant derivatives were combined at different proportions to simulate enrichment of cancer cell population in a drug-resistant fraction during lapatinib therapy. Effects of treatments on cell survival (MTT), apoptosis induction (PARP cleavage), prosurvival signaling (p-Akt, p-S6) as well as cell motility (wound healing assay) and invasion (Boyden chamber assay) were investigated.
RESULTS: Combination of lapatinib with any of isothiocyanates significantly decreased cell viability and inhibited migration of populations consisting of different amounts of drug-sensitive and drug-resistant cells. In case of population entirely composed of lapatinib-resistant cells the most effective was combination of lapatinib with erucin which decreased cell viability and motility, phosphorylation of Akt, S6 and VEGF level more efficiently than each agent alone.
CONCLUSIONS: Combination of lapatinib and isothiocyanates, especially erucin, might be considered as an effective treatment reducing metastatic potential of breast cancer cells, even these with the drug resistance phenotype.
Awada A, Colomer R, Inoue K, et al.
Neratinib Plus Paclitaxel vs Trastuzumab Plus Paclitaxel in Previously Untreated Metastatic ERBB2-Positive Breast Cancer: The NEfERT-T Randomized Clinical Trial.
JAMA Oncol. 2016; 2(12):1557-1564 [PubMed] Related Publications
Neratinib Plus Paclitaxel vs Trastuzumab Plus Paclitaxel in Previously Untreated Metastatic ERBB2-Positive Breast Cancer: The NEfERT-T Randomized Clinical Trial.
JAMA Oncol. 2016; 2(12):1557-1564 [PubMed] Related Publications
Importance: Efficacious ERBB2 (formerly HER2 or HER2/neu)-directed treatments, in addition to trastuzumab and lapatinib, are needed.
Objective: To determine whether neratinib, an irreversible pan-ERBB tyrosine kinase inhibitor, plus paclitaxel improves progression-free survival compared with trastuzumab plus paclitaxel in the first-line treatment of recurrent and/or metastatic ERBB2-positive breast cancer.
Design, Setting, and Participants: In the randomized, controlled, open-label NEfERT-T trial conducted from August 2009 to December 2014 at 188 centers in 34 countries in Europe, Asia, Africa, and North America, 479 women with previously untreated recurrent and/or metastatic ERBB2-positive breast cancer were randomized to 1 of 2 treatment arms (neratinib-paclitaxel [n = 242] or trastuzumab-paclitaxel [n = 237]). Women with asymptomatic central nervous system metastases were eligible, and randomization was stratified by prior trastuzumab and lapatinib exposure, hormone-receptor status, and region.
Interventions: Women received neratinib (240 mg/d orally) or trastuzumab (4 mg/kg then 2 mg/kg weekly), each combined with paclitaxel (80 mg/m2 on days 1, 8, and 15 every 28 days). Primary prophylaxis for diarrhea was not mandatory.
Main Outcome and Measures: The primary outcome was progression-free survival. Secondary end points were response rate, clinical benefit rate, duration of response, frequency, and time to symptomatic and/or progressive central nervous system lesions, and safety.
Results: The intent-to-treat population comprised 479 women 18 years or older (neratinib-paclitaxel, n = 242; trastuzumab-paclitaxel, n = 237) randomized and stratified in their respective treatment arms by prior trastuzumab and lapatinib exposure, hormone-receptor status, and region. Median progression-free survival was 12.9 months (95% CI, 11.1-14.9) with neratinib-paclitaxel and 12.9 months (95% CI, 11.1-14.8) with trastuzumab-paclitaxel (hazard ratio [HR], 1.02; 95% CI, 0.81-1.27; P =.89). With neratinib-paclitaxel, the incidence of central nervous system recurrences was lower (relative risk, 0.48; 95% CI, 0.29-0.79; P = .002) and time to central nervous system metastases delayed (HR, 0.45; 95% CI, 0.26-0.78; P = .004). Common grade 3 to 4 adverse events were diarrhea (73 of 240 patients [30.4%] with neratinib-paclitaxel and 9 of 234 patients [3.8%] with trastuzumab-paclitaxel), neutropenia (31 patients [12.9%] vs 34 patients [14.5%]) and leukopenia (19 patients [7.9%] vs 25 patients [10.7%]); no grade 4 diarrhea was observed.
Conclusions and Relevance: In first-line ERBB2-positive metastatic breast cancer, neratinib-paclitaxel was not superior to trastuzumab-paclitaxel in terms of progression-free survival. In spite of similar overall efficacy, neratinib-paclitaxel may delay the onset and reduce the frequency of central nervous system progression, a finding that requires a larger study to confirm.
Trial Registration: clinicaltrials.gov Identifier: NCT00915018.
Objective: To determine whether neratinib, an irreversible pan-ERBB tyrosine kinase inhibitor, plus paclitaxel improves progression-free survival compared with trastuzumab plus paclitaxel in the first-line treatment of recurrent and/or metastatic ERBB2-positive breast cancer.
Design, Setting, and Participants: In the randomized, controlled, open-label NEfERT-T trial conducted from August 2009 to December 2014 at 188 centers in 34 countries in Europe, Asia, Africa, and North America, 479 women with previously untreated recurrent and/or metastatic ERBB2-positive breast cancer were randomized to 1 of 2 treatment arms (neratinib-paclitaxel [n = 242] or trastuzumab-paclitaxel [n = 237]). Women with asymptomatic central nervous system metastases were eligible, and randomization was stratified by prior trastuzumab and lapatinib exposure, hormone-receptor status, and region.
Interventions: Women received neratinib (240 mg/d orally) or trastuzumab (4 mg/kg then 2 mg/kg weekly), each combined with paclitaxel (80 mg/m2 on days 1, 8, and 15 every 28 days). Primary prophylaxis for diarrhea was not mandatory.
Main Outcome and Measures: The primary outcome was progression-free survival. Secondary end points were response rate, clinical benefit rate, duration of response, frequency, and time to symptomatic and/or progressive central nervous system lesions, and safety.
Results: The intent-to-treat population comprised 479 women 18 years or older (neratinib-paclitaxel, n = 242; trastuzumab-paclitaxel, n = 237) randomized and stratified in their respective treatment arms by prior trastuzumab and lapatinib exposure, hormone-receptor status, and region. Median progression-free survival was 12.9 months (95% CI, 11.1-14.9) with neratinib-paclitaxel and 12.9 months (95% CI, 11.1-14.8) with trastuzumab-paclitaxel (hazard ratio [HR], 1.02; 95% CI, 0.81-1.27; P =.89). With neratinib-paclitaxel, the incidence of central nervous system recurrences was lower (relative risk, 0.48; 95% CI, 0.29-0.79; P = .002) and time to central nervous system metastases delayed (HR, 0.45; 95% CI, 0.26-0.78; P = .004). Common grade 3 to 4 adverse events were diarrhea (73 of 240 patients [30.4%] with neratinib-paclitaxel and 9 of 234 patients [3.8%] with trastuzumab-paclitaxel), neutropenia (31 patients [12.9%] vs 34 patients [14.5%]) and leukopenia (19 patients [7.9%] vs 25 patients [10.7%]); no grade 4 diarrhea was observed.
Conclusions and Relevance: In first-line ERBB2-positive metastatic breast cancer, neratinib-paclitaxel was not superior to trastuzumab-paclitaxel in terms of progression-free survival. In spite of similar overall efficacy, neratinib-paclitaxel may delay the onset and reduce the frequency of central nervous system progression, a finding that requires a larger study to confirm.
Trial Registration: clinicaltrials.gov Identifier: NCT00915018.
Ravind R, Kumar PV, Prabaharan S
Inflammatory breast cancer in a previously treated case of breast cancer: a diagnostic dilemma for the clinician.
BMJ Case Rep. 2016; 2016 [PubMed] Related Publications
Inflammatory breast cancer in a previously treated case of breast cancer: a diagnostic dilemma for the clinician.
BMJ Case Rep. 2016; 2016 [PubMed] Related Publications
Inflammatory breast cancer (IBC) is a relatively rare and aggressive subtype, accounting for nearly 2.5% of all diagnosed breast cancers worldwide. It is usually characterised by an acute onset, rapid clinical progression, poor prognosis and micrometastasis at the time of presentation. Prompt recognition of clinical symptoms and identification of warning signs are vital in diagnosing and appropriately treating a patient with IBC.
Phelps-Polirer K, Abt MA, Smith D, Yeh ES
Co-Targeting of JNK and HUNK in Resistant HER2-Positive Breast Cancer.
PLoS One. 2016; 11(4):e0153025 [PubMed] Free Access to Full Article Related Publications
Co-Targeting of JNK and HUNK in Resistant HER2-Positive Breast Cancer.
PLoS One. 2016; 11(4):e0153025 [PubMed] Free Access to Full Article Related Publications
Strategies for successful primary treatment of HER2-positive breast cancer include use of the HER2 inhibitors trastuzumab or lapatinib in combination with standard chemotherapy. While successful, many patients develop resistance to these HER2 inhibitors indicating an unmet need. Consequently, current research efforts are geared toward understanding mechanisms of resistance and the signaling modalities that regulate these mechanisms. We have undertaken a study to examine whether signaling molecules downstream of epidermal growth factor receptor, which often act as compensatory signaling outlets to circumvent HER2 inhibition, can be co-targeted to overcome resistance. We identified JNK signaling as a potential area of intervention and now show that inhibiting JNK using the pan-JNK inhibitor, SP600125, is effective in the HER2-positive, resistant JIMT-1 xenograft mammary tumor model. We also investigate potential combination strategies to bolster the effects of JNK inhibition and find that co-targeting of JNK and the protein kinase HUNK can prohibit tumor growth of resistant HER2-positive mammary tumors in vivo.
Göksu SS, Bozcuk H, Koral L, et al.
Factors predicting lapatinib efficacy in HER-2+ metastatic breast carcinoma: Does it work better in different histologic subtypes?
Indian J Cancer. 2015 Oct-Dec; 52(4):517-9 [PubMed] Related Publications
Factors predicting lapatinib efficacy in HER-2+ metastatic breast carcinoma: Does it work better in different histologic subtypes?
Indian J Cancer. 2015 Oct-Dec; 52(4):517-9 [PubMed] Related Publications
CONTEXT: Introduction of trastuzumab, a recombinant monoclonal antibody against the extracellular domain of HER-2, is a cornerstone in the treatment of HER-2+ breast carcinoma. However, many cancers that have an initial response to trastuzumab will progress some time later. After progression on trastuzumab-based first-line treatment, there are several options. Although TDM-1 (Trastuzumab emtansine) has prolonged progression-free survival (PFS) and overall survival in patients previously treated with trastuzumab and taxane, it is still not available in Turkey. Patients may be switched to lapatinib (an oral tyrosine kinase inhibitor targeting both HER-1 and HER-2), or they may re-challenge with trastuzumab. There is no clear definition of the patients who should be switched to lapatinib.
AIM: In this study, we investigated the factors predicting the efficacy of lapatinib.
SUBJECTS AND METHODS: Totally, 94 patients treated with lapatinib for metastatic breast carcinoma was included in our study. Retrospective data including pathology, treatments and treatment results, metastatic sites, and laboratory tests were collected.
RESULTS: Progression-free survival was 9.1 months. Histologic subtypes other than invasive ductal carcinoma and liver metastasis were inversely related with PFS. Overall survival was 22.1 months, and patients with histologic subtypes other than invasive ductal carcinoma and who progress with brain metastasis had a worse prognosis.
CONCLUSION: Clinicians should give attention to histologic subtype and metastatic sites when choosing patients for lapatinib treatment.
AIM: In this study, we investigated the factors predicting the efficacy of lapatinib.
SUBJECTS AND METHODS: Totally, 94 patients treated with lapatinib for metastatic breast carcinoma was included in our study. Retrospective data including pathology, treatments and treatment results, metastatic sites, and laboratory tests were collected.
RESULTS: Progression-free survival was 9.1 months. Histologic subtypes other than invasive ductal carcinoma and liver metastasis were inversely related with PFS. Overall survival was 22.1 months, and patients with histologic subtypes other than invasive ductal carcinoma and who progress with brain metastasis had a worse prognosis.
CONCLUSION: Clinicians should give attention to histologic subtype and metastatic sites when choosing patients for lapatinib treatment.
Zheng YB, Yu Y, Chen B, et al.
Inhibitor Response to HER2 G776(YVMA) In-frame Insertion in HER2-positive Breast Cancer.
Cancer Invest. 2016; 34(3):123-9 [PubMed] Related Publications
Inhibitor Response to HER2 G776(YVMA) In-frame Insertion in HER2-positive Breast Cancer.
Cancer Invest. 2016; 34(3):123-9 [PubMed] Related Publications
Human epidermal growth factor receptor 2 (HER2/neu or HER2) has long been recognized as an attractive therapeutic target for breast cancer. The YVMA in-frame insertion at the residue G776 (G776(YVMA)) of HER2 kinase domain is a frequently observed mutation that can largely shift drug sensitivity in targeted therapy of HER2-positive breast cancer. Here, the molecular mechanism and biological significance of tyrosine kinase inhibitor (TKI) response to HER2 G776(YVMA) insertion were investigated in detail. An established protocol that integrated bioinformatics modeling and kinase inhibition assay was employed to examine the structural basis, energetic property, and biological implication underlying the intermolecular interaction between HER2 kinase domain and three representative TKIs, i.e. two FDA-approved drugs lapatinib and gefitinib as well as a pan-kinase inhibitor staurosporine. It was found that the insertion mutation can moderately sensitize lapatinib, but cannot influence the inhibitory capability of staurosporine essentially, suggesting that the two inhibitors exhibit differentiated selectivity between the wild-type HER2 (HER2(WT)) and HER2 G776(YVMA) (HER2(YVMA)) variant. In addition, the gefitinib, which was originally developed as EGFR inhibitor, only possesses modest potency against its noncogate target HER2(WT), and the insertion can further impair the potency, causing a strong resistance for the agent to HER2(YVMA) variant.
Dermawan JK, Hitomi M, Silver DJ, et al.
Pharmacological Targeting of the Histone Chaperone Complex FACT Preferentially Eliminates Glioblastoma Stem Cells and Prolongs Survival in Preclinical Models.
Cancer Res. 2016; 76(8):2432-42 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
Pharmacological Targeting of the Histone Chaperone Complex FACT Preferentially Eliminates Glioblastoma Stem Cells and Prolongs Survival in Preclinical Models.
Cancer Res. 2016; 76(8):2432-42 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
The nearly universal recurrence of glioblastoma (GBM) is driven in part by a treatment-resistant subpopulation of GBM stem cells (GSC). To identify improved therapeutic possibilities, we combined the EGFR/HER2 inhibitor lapatinib with a novel small molecule, CBL0137, which inhibits FACT (facilitates chromatin transcription), a histone chaperone complex predominantly expressed in undifferentiated cells. Lapatinib and CBL0137 synergistically inhibited the proliferation of patient-derived GBM cells. Compared with non-stem tumor cells (NSTC) enriched from the same specimens, the GSCs were extremely sensitive to CBL0137 monotherapy or FACT knockdown. FACT expression was elevated in GSCs compared with matched NSTCs and decreased in GSCs upon differentiation. Acute exposure of GSCs to CBL0137 increased asymmetric cell division, decreased GSC marker expression, and decreased the capacity of GSCs to form tumor spheres in vitro and to initiate tumors in vivo Oral administration of CBL0137 to mice bearing orthotopic GBM prolonged their survival. Knockdown of FACT reduced the expression of genes encoding several core stem cell transcription factors (SOX2, OCT4, NANOG, and OLIG2), and FACT occupied the promoters of these genes. FACT expression was elevated in GBM tumors compared with non-neoplastic brain tissues, portended a worse prognosis, and positively correlated with GSC markers and stem cell gene expression signatures. Preferential targeting of GSCs by CBL0137 and synergy with EGFR inhibitors support the development of clinical trials combining these two agents in GBM. Cancer Res; 76(8); 2432-42. ©2016 AACR.
Sivagnanam K, Rahman ZU, Paul T
Cardiomyopathy Associated With Targeted Therapy for Breast Cancer.
Am J Med Sci. 2016; 351(2):194-9 [PubMed] Related Publications
Cardiomyopathy Associated With Targeted Therapy for Breast Cancer.
Am J Med Sci. 2016; 351(2):194-9 [PubMed] Related Publications
BACKGROUND: Chemotherapeutic agents directed against human epidermal growth factor receptor 2 (HER-2) have significantly improved the prognosis of patients who are positive for this receptor. However, cardiomyopathy remains as a common adverse effect of using these agents.
MATERIALS AND METHODS: Literature search was conducted via PubMed using the keywords of "Trastuzumab Cardiomyopathy," "Lapatinib Cardiomyopathy" and "Pertuzumab Cardiomyopathy," which provided 104 results. These articles were then screened for relevance to the targeted subject based on their title and abstracts. Case reports and articles that were not discussing any aspect of cardiomyopathy secondary to targeted therapy for breast cancer and articles not in English were eliminated. After elimination, a bibliography search among selected articles was done and a total of 46 articles were identified. The collected articles were then meticulously analyzed and summarized.
RESULTS: The use of human epidermal growth factor receptor 2 (HER-2) receptor targeted chemotherapy in breast cancer is limited because of a higher incidence (19-22%) of cardiomyopathy. The incidence of cardiomyopathy is not dose dependent and in most cases it is reversible after discontinuation of the drug and treatment with heart failure medications. Severe adverse outcomes including death or permanent disability are rare.
CONCLUSION: HER-2 targeted chemotherapy for breast cancer has a higher incidence of associated reversible cardiomyopathy. Patients should be monitored by serial echocardiography starting at the beginning of the treatment and followed by every 3 months until the completion of chemotherapy. Co-ordination between oncologists and cardiologists is needed to develop evidence-based protocols to prevent, identify, monitor and treat trastuzumab-induced cardiomyopathy.
MATERIALS AND METHODS: Literature search was conducted via PubMed using the keywords of "Trastuzumab Cardiomyopathy," "Lapatinib Cardiomyopathy" and "Pertuzumab Cardiomyopathy," which provided 104 results. These articles were then screened for relevance to the targeted subject based on their title and abstracts. Case reports and articles that were not discussing any aspect of cardiomyopathy secondary to targeted therapy for breast cancer and articles not in English were eliminated. After elimination, a bibliography search among selected articles was done and a total of 46 articles were identified. The collected articles were then meticulously analyzed and summarized.
RESULTS: The use of human epidermal growth factor receptor 2 (HER-2) receptor targeted chemotherapy in breast cancer is limited because of a higher incidence (19-22%) of cardiomyopathy. The incidence of cardiomyopathy is not dose dependent and in most cases it is reversible after discontinuation of the drug and treatment with heart failure medications. Severe adverse outcomes including death or permanent disability are rare.
CONCLUSION: HER-2 targeted chemotherapy for breast cancer has a higher incidence of associated reversible cardiomyopathy. Patients should be monitored by serial echocardiography starting at the beginning of the treatment and followed by every 3 months until the completion of chemotherapy. Co-ordination between oncologists and cardiologists is needed to develop evidence-based protocols to prevent, identify, monitor and treat trastuzumab-induced cardiomyopathy.
Maximiano S, Magalhães P, Guerreiro MP, Morgado M
Trastuzumab in the Treatment of Breast Cancer.
BioDrugs. 2016; 30(2):75-86 [PubMed] Related Publications
Trastuzumab in the Treatment of Breast Cancer.
BioDrugs. 2016; 30(2):75-86 [PubMed] Related Publications
Breast cancer (BC) is the most common cancer in women worldwide, and has an undeniable negative impact on public health. The advent of molecular biology and immunotherapy has made targeted therapeutic interventions possible, providing treatments tailored to the individual characteristics of the patient and the disease. The over-expression of human epidermal growth factor receptor (HER) 2 is implicated in the pathophysiology of BC and represents a clinically relevant biomarker for its treatment. Trastuzumab, a recombinant antibody targeting HER2, was the first biological drug approved for the treatment of HER2-positive BC. Although there are currently other anti-HER2 agents available (e.g. pertuzumab and lapatinib), trastuzumab remains the gold standard for treatment of this disease subtype. Nonetheless, concerns have been raised regarding potential cardiotoxicity and treatment resistance. Moreover, several other therapeutic issues remain unclear and have been addressed in an inconsistent way. The current literature lacks a comprehensive review of trastuzumab providing useful information for clinical practice, including pharmacokinetic and pharmacodynamic aspects, its clinical use, existing controversies and future advances. This detailed review of trastuzumab in the pharmacotherapy of BC attempts to fill this gap.
Santa-Maria CA, Nye L, Mutonga MB, et al.
Management of Metastatic HER2-Positive Breast Cancer: Where Are We and Where Do We Go From Here?
Oncology (Williston Park). 2016; 30(2):148-55 [PubMed] Related Publications
Management of Metastatic HER2-Positive Breast Cancer: Where Are We and Where Do We Go From Here?
Oncology (Williston Park). 2016; 30(2):148-55 [PubMed] Related Publications
Human epidermal growth factor receptor 2 (HER2)/neu-positive breast cancer has changed from being an aggressive disease with a poor prognosis to a disease that is highly treatable, with prolonged survival possible even in patients with metastatic disease. A better understanding of HER2 biology has led to the development of powerful targeted therapies, and four drugs are already approved by the US Food and Drug Administration for treatment in the metastatic setting (trastuzumab, pertuzumab, lapatinib, and trastuzumab emtansine). Optimizing how these drugs are delivered and in what sequence is an important part of modern management of HER2-positive breast cancer. However, while the prognosis has improved, metastatic disease is still not curable; newer, better drugs are needed. This review will summarize the current standard of care; key issues that arise when treating patients with HER2-positive disease; and developments in novel therapeutics, including small-molecule inhibitors, nanoparticles, immunotherapy, and agents targeting resistance pathways.
Thallinger C, Lang I, Kuhar CG, et al.
Phase II study on the efficacy and safety of Lapatinib administered beyond disease progression and combined with vinorelbine in HER-2/neu- positive advanced breast cancer: results of the CECOG LaVie trial.
BMC Cancer. 2016; 16:121 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
Phase II study on the efficacy and safety of Lapatinib administered beyond disease progression and combined with vinorelbine in HER-2/neu- positive advanced breast cancer: results of the CECOG LaVie trial.
BMC Cancer. 2016; 16:121 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
BACKGROUND: Vinorelbine constitutes effective chemotherapy for metastatic breast cancer (MBC) and acts synergistically with trastuzumab in HER-2/neu positive disease. The present study was set out to evaluate the efficacy and safety of vinorelbine when combined with lapatinib, an anti-HER2 tyrosine-kinase inhibitor, as late-line regimen administered beyond previous disease progression on prior lapatinib in patients with HER-2/neu- positive MBC.
METHODS: The CECOG LaVie study was designed as open-labeled, single-arm, multicenter phase II trial. Patients had to be pretreated with lapatinib plus chemotherapy, and received lapatinib at a daily dose of 1250 mg in combination with vinorelbine 20 mg/m(2) i.v. on days 1 and 8 of a three-week cycle until disease progression, intolerable toxicity or withdrawal of consent. Progression-free survival (PFS) was defined as primary study endpoint; secondary endpoints included overall survival (OS), response rate according to RECIST 1.1, and safety. The study was terminated early due to poor accrual.
RESULTS: A total number of nine patients were included; lapatinib administered beyond disease progression combined with vinorelbine resulted in a median PFS of 7.7 months (95% CI 0.56-14.91) and a median OS of 23.4 months (95% CI 16.61-30.13), respectively. Partial remission was seen in one of nine patients, three patients had stable disease of > six months, whereas the remaining five patients had primary disease progression. In two patients, modification of vinorelbine dose due to toxicity became necessary; no dose modification was needed for lapatinib. The majority of reported adverse events (AE) were grade 1 and 2 in severity with diarrhea being the most commonly observed AE CONCLUSION: In this heavily pretreated patient population, combination of vinorelbine plus lapatinib showed encouraging activity and was characterized by an acceptable safety profile. Despite the low patient number, lapatinib plus vinorelbine may constitute a potential treatment option in heavily pretreated patients with HER-2/neu-positive MBC previously exposed to lapatinib.
TRIAL REGISTRATION: EudraCT number 2009-016826-15, (15. 10.2009).
METHODS: The CECOG LaVie study was designed as open-labeled, single-arm, multicenter phase II trial. Patients had to be pretreated with lapatinib plus chemotherapy, and received lapatinib at a daily dose of 1250 mg in combination with vinorelbine 20 mg/m(2) i.v. on days 1 and 8 of a three-week cycle until disease progression, intolerable toxicity or withdrawal of consent. Progression-free survival (PFS) was defined as primary study endpoint; secondary endpoints included overall survival (OS), response rate according to RECIST 1.1, and safety. The study was terminated early due to poor accrual.
RESULTS: A total number of nine patients were included; lapatinib administered beyond disease progression combined with vinorelbine resulted in a median PFS of 7.7 months (95% CI 0.56-14.91) and a median OS of 23.4 months (95% CI 16.61-30.13), respectively. Partial remission was seen in one of nine patients, three patients had stable disease of > six months, whereas the remaining five patients had primary disease progression. In two patients, modification of vinorelbine dose due to toxicity became necessary; no dose modification was needed for lapatinib. The majority of reported adverse events (AE) were grade 1 and 2 in severity with diarrhea being the most commonly observed AE CONCLUSION: In this heavily pretreated patient population, combination of vinorelbine plus lapatinib showed encouraging activity and was characterized by an acceptable safety profile. Despite the low patient number, lapatinib plus vinorelbine may constitute a potential treatment option in heavily pretreated patients with HER-2/neu-positive MBC previously exposed to lapatinib.
TRIAL REGISTRATION: EudraCT number 2009-016826-15, (15. 10.2009).
Murthy P, Kidwell KM, Schott AF, et al.
Clinical predictors of long-term survival in HER2-positive metastatic breast cancer.
Breast Cancer Res Treat. 2016; 155(3):589-95 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
Clinical predictors of long-term survival in HER2-positive metastatic breast cancer.
Breast Cancer Res Treat. 2016; 155(3):589-95 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
Prior to availability of anti-HER2 therapies, HER2-positive metastatic breast cancer (MBC) was associated with a poor prognosis. Prospective randomized trials have demonstrated survival benefit from anti-HER2 treatments. Anecdotal observations have suggested that a small but meaningful fraction of patients with HER2-positive MBC may be "exceptional responders" with long survival. We hypothesized that demographic and/or clinicopathologic characteristics can be identified to distinguish short-term from long-term survivors. A retrospective, single-institution review of 168 patients with HER2-positive MBC who received treatment with anti-HER2 therapy in the metastatic setting was performed. Cox proportional hazards analysis was used to assess factors associated with long-term survival. Median overall survival from the time of breast cancer recurrence was 3.9 years (95 % CI 3.4-5.2). From the time of diagnosis of MBC, 56 (33 %) survived for 5 or more years and 12 (7 %) survived more than 10 years. Of the 66 patients diagnosed with central nervous system metastases, 9 (14 %) survived more than 5 years following that diagnosis. Younger age at diagnosis, lower stage, hormone receptor positive status, and only having one organ involved at diagnosis were associated with longer survival. Four patients discontinued anti-HER2 therapy and are without evidence of progression of disease after a median 7.4 years (0.2-12.0) since stopping therapy. In a cohort of patients with HER2-positive MBC treated primarily with trastuzumab and lapatinib, 7 % of patients were "exceptional responders." Combining these clinical factors with molecular determinants of prolonged survival may provide insights for individualizing treatment selection.
Schwartz GK, Dickson MA, LoRusso PM, et al.
Preclinical and first-in-human phase I studies of KW-2450, an oral tyrosine kinase inhibitor with insulin-like growth factor receptor-1/insulin receptor selectivity.
Cancer Sci. 2016; 107(4):499-506 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
Preclinical and first-in-human phase I studies of KW-2450, an oral tyrosine kinase inhibitor with insulin-like growth factor receptor-1/insulin receptor selectivity.
Cancer Sci. 2016; 107(4):499-506 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
Numerous solid tumors overexpress or have excessively activated insulin-like growth factor receptor-1 (IGF-1R). We summarize preclinical studies and the first-in-human study of KW-2450, an oral tyrosine kinase inhibitor with IGF-1R and insulin receptor (IR) inhibitory activity. Preclinical activity of KW-2450 was evaluated in various in vitro and in vivo models. It was then evaluated in a phase I clinical trial in 13 patients with advanced solid tumors (NCT00921336). In vitro, KW-2450 inhibited human IGF-1R and IR kinases (IC50 7.39 and 5.64 nmol/L, respectively) and the growth of various human malignant cell lines. KW-2450 40 mg/kg showed modest growth inhibitory activity and inhibited IGF-1-induced signal transduction in the murine HT-29/GFP colon carcinoma xenograft model. The maximum tolerated dose of KW-2450 was 37.5 mg once daily continuously; dose-limiting toxicity occurred in two of six patients at 50 mg/day (both grade 3 hyperglycemia) and in one of seven patients at 37.5 mg/day (grade 3 rash). Four of 10 evaluable patients showed stable disease. Single-agent KW-2450 was associated with modest antitumor activity in heavily pretreated patients with solid tumors and is being further investigated in combination therapy with lapatinib/letrozole in patients with human epidermal growth factor receptor 2-postive metastatic breast cancer.
Gebhart G, Flamen P, De Vries EG, et al.
Imaging Diagnostic and Therapeutic Targets: Human Epidermal Growth Factor Receptor 2.
J Nucl Med. 2016; 57 Suppl 1:81S-8S [PubMed] Related Publications
Imaging Diagnostic and Therapeutic Targets: Human Epidermal Growth Factor Receptor 2.
J Nucl Med. 2016; 57 Suppl 1:81S-8S [PubMed] Related Publications
Since the approval of trastuzumab, a humanized monoclonal antibody against the extracellular domain of human epidermal growth factor receptor 2 (HER2), 3 other HER2-targeting agents have gained regulatory approval: lapatinib, pertuzumab, and trastuzumab-emtansine. These agents have revolutionized the management of HER2-positive breast cancer, highlighting the concept that targeted therapies are successful when patients exhibit tumor-selective expression of a molecular target-in this case, HER2. However, response prediction and innate or acquired resistance remain serious concerns. Predictive biomarkers of a response-which could help in the selection of patients who might benefit from a selected targeted therapy-are currently lacking. Molecular imaging with anti-HER2 probes allows the noninvasive, whole-body assessment of HER2 tumor burden and has the potential to improve patient selection, optimize the dose and schedule, and rationalize assessment of the response to anti-HER2 therapies. Furthermore, unlike biopsy-based HER2 assessment, this approach can reveal inter- or intratumoral heterogeneity as well as variations in HER2 expression over time. This review summarizes the available literature and the current status of molecular imaging as a tool for the assessment of HER2 (target) expression or the prediction of an early treatment response in early and advanced HER2-positive breast cancer.
Strasser-Weippl K, Horick N, Smith IE, et al.
Identification of early breast cancer patient cohorts who may benefit from lapatinib therapy.
Eur J Cancer. 2016; 56:85-92 [PubMed] Related Publications
Identification of early breast cancer patient cohorts who may benefit from lapatinib therapy.
Eur J Cancer. 2016; 56:85-92 [PubMed] Related Publications
In resource-constrained environments many patients with human epidermal growth factor receptor 2 (HER2)+ early breast cancer are currently not offered adjuvant anti-HER2 therapy. For patients who might be able to receive the tyrosine kinase inhibitor (TKI) lapatinib (e.g. after patent expiration), it is important to identify subgroups of patients for whom anti-HER2 TKI therapy could be beneficial. To do this, we used data from 2489 patients with centrally confirmed HER2+ disease enrolled in the adjuvant Tykerb Evaluation After Chemotherapy (TEACH) trial, investigating the effect of lapatinib in patients with HER2+ early breast cancer not treated with trastuzumab. We performed subgroup analyses and number-needed-to-treat (NNT) calculations using patient and tumour associated predictors. Hormone receptor negative (HR-) patients on lapatinib had a significantly prolonged disease-free survival (DFS) compared to HR- patients on placebo (hazard ratio 0.64, P=0.003). For patients with HR- disease, starting treatment with lapatinib ≤1 year from diagnosis improved DFS by 12.1% [2.1-22.1] at 2 years and 15.7% [4.1-27.2] at 5 years. Depending on lymph node status and time since diagnosis the NNT for recurrence (at 5 years) was between 5.9 (node positive patients <1 year from diagnosis) and 15.9. These numbers are in range with numbers reported for up-front adjuvant trastuzumab for HR unselected patients (e.g. 15.6 for DFS at 4 years in HERA). In a subgroup analysis of the adjuvant TEACH trial, we show that anti-HER2 monotherapy with a TKI is beneficial as adjuvant therapy in a subgroup of patients. NNT in HER2+ HR- patients are in range with those reported from up-front adjuvant trastuzumab trials.
Andrade JM, Brito LG, Moises EC, et al.
Trastuzumab use during pregnancy: long-term survival after locally advanced breast cancer and long-term infant follow-up.
Anticancer Drugs. 2016; 27(4):369-72 [PubMed] Related Publications
Trastuzumab use during pregnancy: long-term survival after locally advanced breast cancer and long-term infant follow-up.
Anticancer Drugs. 2016; 27(4):369-72 [PubMed] Related Publications
Here, we describe the case of a patient diagnosed with locally advanced breast cancer 8 years ago. Her treatment course was neoadjuvant chemotherapy, followed by mastectomy and then adjuvant radiotherapy and trastuzumab (TTZ). During the use of adjuvant targeted therapy, an incidental pregnancy was diagnosed. Four years later, she developed bone and cerebral metastases, and since then, she has received courses of TTZ, capecitabine, lapatinib, and radiotherapy with intermittent control of the disease. Her 7-year-old son presents a normal physical and long-term neurological developmental curve according to specialized evaluation. This case is unique for several reasons: the patient received the highest dose of TTZ yet described during pregnancy (4400 mg); there has been a long period of disease-free survival after treatment for locally advanced breast cancer and long overall survival despite successive disease progressions during the metastatic phase of the disease (97 months), and there was a monitored pediatric follow-up period (7 years).
Liu CY, Hu MH, Hsu CJ, et al.
Lapatinib inhibits CIP2A/PP2A/p-Akt signaling and induces apoptosis in triple negative breast cancer cells.
Oncotarget. 2016; 7(8):9135-49 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
Lapatinib inhibits CIP2A/PP2A/p-Akt signaling and induces apoptosis in triple negative breast cancer cells.
Oncotarget. 2016; 7(8):9135-49 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
We tested the efficacy of lapatinib, a dual tyrosine kinase inhibitor which interrupts the HER2 and epidermal growth factor receptor (EGFR) pathways, in a panel of triple-negative breast cancer (TNBC) cells, and examined the drug mechanism. Lapatinib showed an anti-proliferative effect in HCC 1937, MDA-MB-468, and MDA-MB-231 cell lines. Lapatinib induced significant apoptosis and inhibited CIP2A and p-Akt in a dose and time-dependent manner in the three TNBC cell lines. Overexpression of CIP2A reduced lapatinib-induced apoptosis in MDA-MB-468 cells. In addition, lapatinib increased PP2A activity (in relation to CIP2A inhibition). Moreover, lapatinib-induced apoptosis and p-Akt downregulation was attenuated by PP2A antagonist okadaic acid. Furthermore, lapatinib indirectly decreased CIP2A transcription by disturbing the binding of Elk1 to the CIP2A promoter. Importantly, lapatinib showed anti-tumor activity in mice bearing MDA-MB-468 xenograft tumors, and suppressed CIP2A as well as p-Akt in these xenografted tumors. In summary, inhibition of CIP2A determines the effects of lapatinib-induced apoptosis in TNBC cells. In addition to being a dual tyrosine kinase inhibitor of HER2 and EGFR, lapatinib also inhibits CIP2A/PP2A/p-Akt signaling in TNBC cells.
Hill A, Gotham D, Fortunak J, et al.
Target prices for mass production of tyrosine kinase inhibitors for global cancer treatment.
BMJ Open. 2016; 6(1):e009586 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
Target prices for mass production of tyrosine kinase inhibitors for global cancer treatment.
BMJ Open. 2016; 6(1):e009586 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
OBJECTIVE: To calculate sustainable generic prices for 4 tyrosine kinase inhibitors (TKIs).
BACKGROUND: TKIs have proven survival benefits in the treatment of several cancers, including chronic myeloid leukaemia, breast, liver, renal and lung cancer. However, current high prices are a barrier to treatment. Mass production of low-cost generic antiretrovirals has led to over 13 million people being on HIV/AIDS treatment worldwide. This analysis estimates target prices for generic TKIs, assuming similar methods of mass production.
METHODS: Four TKIs with patent expiry dates in the next 5 years were selected for analysis: imatinib, erlotinib, lapatinib and sorafenib. Chemistry, dosing, published data on per-kilogram pricing for commercial transactions of active pharmaceutical ingredient (API), and quotes from manufacturers were used to estimate costs of production. Analysis included costs of excipients, formulation, packaging, shipping and a 50% profit margin. Target prices were compared with current prices. Global numbers of patients eligible for treatment with each TKI were estimated.
RESULTS: API costs per kg were $347-$746 for imatinib, $2470 for erlotinib, $4671 for lapatinib, and $3000 for sorafenib. Basing on annual dose requirements, costs of formulation/packaging and a 50% profit margin, target generic prices per person-year were $128-$216 for imatinib, $240 for erlotinib, $1450 for sorafenib, and $4020 for lapatinib. Over 1 million people would be newly eligible to start treatment with these TKIs annually.
CONCLUSIONS: Mass generic production of several TKIs could achieve treatment prices in the range of $128-$4020 per person-year, versus current US prices of $75161-$139,138. Generic TKIs could allow significant savings and scaling-up of treatment globally, for over 1 million eligible patients.
BACKGROUND: TKIs have proven survival benefits in the treatment of several cancers, including chronic myeloid leukaemia, breast, liver, renal and lung cancer. However, current high prices are a barrier to treatment. Mass production of low-cost generic antiretrovirals has led to over 13 million people being on HIV/AIDS treatment worldwide. This analysis estimates target prices for generic TKIs, assuming similar methods of mass production.
METHODS: Four TKIs with patent expiry dates in the next 5 years were selected for analysis: imatinib, erlotinib, lapatinib and sorafenib. Chemistry, dosing, published data on per-kilogram pricing for commercial transactions of active pharmaceutical ingredient (API), and quotes from manufacturers were used to estimate costs of production. Analysis included costs of excipients, formulation, packaging, shipping and a 50% profit margin. Target prices were compared with current prices. Global numbers of patients eligible for treatment with each TKI were estimated.
RESULTS: API costs per kg were $347-$746 for imatinib, $2470 for erlotinib, $4671 for lapatinib, and $3000 for sorafenib. Basing on annual dose requirements, costs of formulation/packaging and a 50% profit margin, target generic prices per person-year were $128-$216 for imatinib, $240 for erlotinib, $1450 for sorafenib, and $4020 for lapatinib. Over 1 million people would be newly eligible to start treatment with these TKIs annually.
CONCLUSIONS: Mass generic production of several TKIs could achieve treatment prices in the range of $128-$4020 per person-year, versus current US prices of $75161-$139,138. Generic TKIs could allow significant savings and scaling-up of treatment globally, for over 1 million eligible patients.
Awada G, Gombos A, Aftimos P, Awada A
Emerging drugs targeting human epidermal growth factor receptor 2 (HER2) in the treatment of breast cancer.
Expert Opin Emerg Drugs. 2016; 21(1):91-101 [PubMed] Related Publications
Emerging drugs targeting human epidermal growth factor receptor 2 (HER2) in the treatment of breast cancer.
Expert Opin Emerg Drugs. 2016; 21(1):91-101 [PubMed] Related Publications
INTRODUCTION: Human epidermal growth factor 2 (HER2) overexpression is present in 20% of breast cancer patients. It is associated with more aggressive disease and worse clinical outcome. New drugs are thus needed. Approved and future treatments will be discussed in this review.
AREAS COVERED: The monoclonal antibodies trastuzumab and pertuzumab, the tyrosine kinase inhibitor lapatinib and the antibody-drug conjugate trastuzmab emtansine are approved for HER2 positive breast cancer. The combination of trastuzumab, pertuzumab and docetaxel is currently the first-line treatment in the metastatic setting. New therapies are still needed due to frequent relapse and resistance. These include mammalian target of rapamycin inhibitors, heat shock protein 90 inhibitors, pan-HER2 tyrosine kinase inhibitors, antibody-drug conjugates, immunotherapy agents (antibodies and vaccines), radioimmunotherapy and HER2 specific affinity proteins. Possible developmental issues are the complexity of the molecular biology of the HER2 positive cancer cell, the occurrence of resistance, toxicity and the high cost.
EXPERT OPINION: The determination of the right sequence of use of old and new therapies remains a challenging issue. The selection of patients who do or don't benefit from potentially toxic chemotherapy is also difficult. Central nervous system metastases are a common problem in HER2 positive breast cancer that needs to be addressed in future trials.
AREAS COVERED: The monoclonal antibodies trastuzumab and pertuzumab, the tyrosine kinase inhibitor lapatinib and the antibody-drug conjugate trastuzmab emtansine are approved for HER2 positive breast cancer. The combination of trastuzumab, pertuzumab and docetaxel is currently the first-line treatment in the metastatic setting. New therapies are still needed due to frequent relapse and resistance. These include mammalian target of rapamycin inhibitors, heat shock protein 90 inhibitors, pan-HER2 tyrosine kinase inhibitors, antibody-drug conjugates, immunotherapy agents (antibodies and vaccines), radioimmunotherapy and HER2 specific affinity proteins. Possible developmental issues are the complexity of the molecular biology of the HER2 positive cancer cell, the occurrence of resistance, toxicity and the high cost.
EXPERT OPINION: The determination of the right sequence of use of old and new therapies remains a challenging issue. The selection of patients who do or don't benefit from potentially toxic chemotherapy is also difficult. Central nervous system metastases are a common problem in HER2 positive breast cancer that needs to be addressed in future trials.
Lee CK, Davies L, Gebski VJ, et al.
Serum Human Epidermal Growth Factor 2 Extracellular Domain as a Predictive Biomarker for Lapatinib Treatment Efficacy in Patients With Advanced Breast Cancer.
J Clin Oncol. 2016; 34(9):936-44 [PubMed] Related Publications
Serum Human Epidermal Growth Factor 2 Extracellular Domain as a Predictive Biomarker for Lapatinib Treatment Efficacy in Patients With Advanced Breast Cancer.
J Clin Oncol. 2016; 34(9):936-44 [PubMed] Related Publications
PURPOSE: We examined the prognostic and predictive value of serum human epidermal growth factor 2 (HER2) extracellular domain (sHER2) in patients with advanced breast cancer treated with lapatinib using data from three randomized trials.
PATIENTS AND METHODS: We analyzed sHER2 and tissue HER2 (tHER2) data from 1,902 patients (84%) who were randomly assigned to receive lapatinib or control in the trials EGF30001, EGF30008, and EGF100151. Cox regression analyses were performed to correlate both biomarkers with progression-free survival (PFS) and overall survival (OS).
RESULTS: Median sHER2 levels were 25.1 and 10.1 ng/mL in tHER2-amplified (tHER-positive) and nonamplified (tHER-negative) populations, respectively (r = 0.42 for sHER2-tHER2 correlation). Lapatinib had significant PFS benefit over control (hazard ratio [HR], 0.855; P = .004), but not OS (HR, 0.941; P = .33). Lapatinib PFS benefit is independently predicted by higher sHER2 values (HR per 10-ng/mL increase in sHER2: lapatinib-containing therapies, 1.009 v nonlapatinib-containing therapies, 1.044; P(interaction) < .001) and by positive tHER2 (HR [lapatinib v nonlapatinib]: tHER2 positive, 0.638 v tHER2 negative, 0.940; P(interaction) = .001). Within the tHER2-positive subpopulation (n = 515), higher sHER2 values still independently predicted lapatinib PFS benefit (HR per 10-ng/mL increase in sHER2: lapatinib-containing therapies, 1.017 v nonlapatinib-containing therapies, 1.041; P(interaction) = .008). In control arms (n = 936), higher sHER2 was associated with worse prognosis in multivariable analyses (PFS HR per 10 ng/mL: PFS, 1.024; P < .001; and OS, 1.018; P < .001).
CONCLUSION: Higher sHER2 predicts greater PFS benefit with lapatinib independent of tHER2 status. High sHER2 is also independently prognostic for worse survival in patients who received nonlapatinib-containing therapies. The predictive role of sHER2 for other anti-HER2 agents requires further research.
PATIENTS AND METHODS: We analyzed sHER2 and tissue HER2 (tHER2) data from 1,902 patients (84%) who were randomly assigned to receive lapatinib or control in the trials EGF30001, EGF30008, and EGF100151. Cox regression analyses were performed to correlate both biomarkers with progression-free survival (PFS) and overall survival (OS).
RESULTS: Median sHER2 levels were 25.1 and 10.1 ng/mL in tHER2-amplified (tHER-positive) and nonamplified (tHER-negative) populations, respectively (r = 0.42 for sHER2-tHER2 correlation). Lapatinib had significant PFS benefit over control (hazard ratio [HR], 0.855; P = .004), but not OS (HR, 0.941; P = .33). Lapatinib PFS benefit is independently predicted by higher sHER2 values (HR per 10-ng/mL increase in sHER2: lapatinib-containing therapies, 1.009 v nonlapatinib-containing therapies, 1.044; P(interaction) < .001) and by positive tHER2 (HR [lapatinib v nonlapatinib]: tHER2 positive, 0.638 v tHER2 negative, 0.940; P(interaction) = .001). Within the tHER2-positive subpopulation (n = 515), higher sHER2 values still independently predicted lapatinib PFS benefit (HR per 10-ng/mL increase in sHER2: lapatinib-containing therapies, 1.017 v nonlapatinib-containing therapies, 1.041; P(interaction) = .008). In control arms (n = 936), higher sHER2 was associated with worse prognosis in multivariable analyses (PFS HR per 10 ng/mL: PFS, 1.024; P < .001; and OS, 1.018; P < .001).
CONCLUSION: Higher sHER2 predicts greater PFS benefit with lapatinib independent of tHER2 status. High sHER2 is also independently prognostic for worse survival in patients who received nonlapatinib-containing therapies. The predictive role of sHER2 for other anti-HER2 agents requires further research.
Gudala S, Khan U, Kanungo N, et al.
Identification and Pharmacological Analysis of High Efficacy Small Molecule Inhibitors of EGF-EGFR Interactions in Clinical Treatment of Non-Small Cell Lung Carcinoma: a Computational Approach.
Asian Pac J Cancer Prev. 2015; 16(18):8191-6 [PubMed] Related Publications
Identification and Pharmacological Analysis of High Efficacy Small Molecule Inhibitors of EGF-EGFR Interactions in Clinical Treatment of Non-Small Cell Lung Carcinoma: a Computational Approach.
Asian Pac J Cancer Prev. 2015; 16(18):8191-6 [PubMed] Related Publications
Inhibition of EGFR-EGF interactions forms an important therapeutic rationale in treatment of non-small cell lung carcinoma. Established inhibitors have been successful in reducing proliferative processes observed in NSCLC, however patients suffer serious side effects. Considering the narrow therapeutic window of present EGFR inhibitors, the present study centred on identifying high efficacy EGFR inhibitors through structure based virtual screening strategies. Established inhibitors - Afatinib, Dacomitinib, Erlotinib, Lapatinib, Rociletinib formed parent compounds to retrieve similar compounds by linear fingerprint based tanimoto search with a threshold of 90%. The compounds (parents and respective similars) were docked at the EGF binding cleft of EGFR. Patch dock supervised protein-protein interactions were established between EGF and ligand (query and similar) bound and free states of EGFR. Compounds ADS103317, AKOS024836912, AGN-PC-0MXVWT, GNF-Pf-3539, SCHEMBL15205939 were retrieved respectively similar to Afatinib, Dacomitinib, Erlotinib, Lapatinib, Rociletinib. Compound- AGN-PC-0MXVWT akin to Erlotinib showed highest affinity against EGFR amongst all the compounds (parent and similar) assessed in the study. Further, AGN-PC-0MXVWT brought about significant blocking of EGFR-EGF interactions in addition showed appreciable ADMET properties and pharmacophoric features. In the study, we report AGN-PC-0MXVWT to be an efficient and high efficacy inhibitor of EGFR-EGF interactions identified through computational approaches.
Gschwantler-Kaulich D, Grunt TW, Muhr D, et al.
HER Specific TKIs Exert Their Antineoplastic Effects on Breast Cancer Cell Lines through the Involvement of STAT5 and JNK.
PLoS One. 2016; 11(1):e0146311 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
HER Specific TKIs Exert Their Antineoplastic Effects on Breast Cancer Cell Lines through the Involvement of STAT5 and JNK.
PLoS One. 2016; 11(1):e0146311 [PubMed] Article available free on PMC after 15/04/2017 Related Publications
BACKGROUND: HER-targeted tyrosine kinase inhibitors (TKIs) have demonstrated pro-apoptotic and antiproliferative effects in vitro and in vivo. The exact pathways through which TKIs exert their antineoplastic effects are, however, still not completely understood.
METHODS: Using Milliplex assays, we have investigated the effects of the three panHER-TKIs lapatinib, canertinib and afatinib on signal transduction cascade activation in SKBR3, T47D and Jurkat neoplastic cell lines. The growth-inhibitory effect of blockade of HER and of JNK and STAT5 signaling was measured by proliferation- and apoptosis-assays using formazan dye labeling of viable cells, Western blotting for cleaved PARP-1 and immunolabeling for active caspase 3, respectively.
RESULTS: All three HER-TKIs clearly inhibited proliferation and increased apoptosis in HER2 overexpressing SKBR3 cells, while their effect was less pronounced on HER2 moderately expressing T47D cells where they exerted only a weak antiproliferative and essentially no pro-apoptotic effect. Remarkably, phosphorylation/activation of JNK and STAT5A/B were inhibited by HER-TKIs only in the sensitive, but not in the resistant cells. In contrast, phosphorylation/activation of ERK/MAPK, STAT3, CREB, p70 S6 kinase, IkBa, and p38 were equally affected by HER-TKIs in both cell lines. Moreover, we demonstrated that direct pharmacological blockade of JNK and STAT5 abrogates cell growth in both HER-TKI-sensitive as well as -resistant breast cancer cells, respectively.
CONCLUSION: We have shown that HER-TKIs exert a HER2 expression-dependent anti-cancer effect in breast cancer cell lines. This involves blockade of JNK and STAT5A/B signaling, which have been found to be required for in vitro growth of these cell lines.
METHODS: Using Milliplex assays, we have investigated the effects of the three panHER-TKIs lapatinib, canertinib and afatinib on signal transduction cascade activation in SKBR3, T47D and Jurkat neoplastic cell lines. The growth-inhibitory effect of blockade of HER and of JNK and STAT5 signaling was measured by proliferation- and apoptosis-assays using formazan dye labeling of viable cells, Western blotting for cleaved PARP-1 and immunolabeling for active caspase 3, respectively.
RESULTS: All three HER-TKIs clearly inhibited proliferation and increased apoptosis in HER2 overexpressing SKBR3 cells, while their effect was less pronounced on HER2 moderately expressing T47D cells where they exerted only a weak antiproliferative and essentially no pro-apoptotic effect. Remarkably, phosphorylation/activation of JNK and STAT5A/B were inhibited by HER-TKIs only in the sensitive, but not in the resistant cells. In contrast, phosphorylation/activation of ERK/MAPK, STAT3, CREB, p70 S6 kinase, IkBa, and p38 were equally affected by HER-TKIs in both cell lines. Moreover, we demonstrated that direct pharmacological blockade of JNK and STAT5 abrogates cell growth in both HER-TKI-sensitive as well as -resistant breast cancer cells, respectively.
CONCLUSION: We have shown that HER-TKIs exert a HER2 expression-dependent anti-cancer effect in breast cancer cell lines. This involves blockade of JNK and STAT5A/B signaling, which have been found to be required for in vitro growth of these cell lines.




 Bevacizumab (Avastin)
Bevacizumab (Avastin)