Found this page useful?
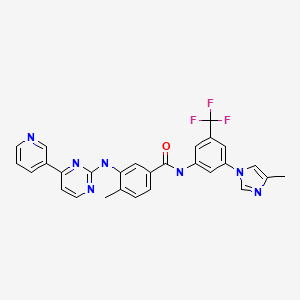
Nilotinib (Tasigna)
 Web Resources: Nilotinib (Tasigna)
Web Resources: Nilotinib (Tasigna) Latest Research Publications: Nilotinib (Tasigna)
Latest Research Publications: Nilotinib (Tasigna)Web Resources: Nilotinib (Tasigna) (6 links)
American Cancer Society
MedlinePlus.gov
NHS Evidence
PubChem
Macmillan Cancer Support
Cancer Research UK
Latest Research Publications: Nilotinib (Tasigna)
Yamada T, Nannya Y, Shimizu M, et al.
Symptomatic Acute Pancreatitis Induced by Nilotinib: A Report of Two Cases.
Intern Med. 2016; 55(23):3495-3497 [PubMed] Free Access to Full Article Related Publications
Symptomatic Acute Pancreatitis Induced by Nilotinib: A Report of Two Cases.
Intern Med. 2016; 55(23):3495-3497 [PubMed] Free Access to Full Article Related Publications
Nilotinib is a selective tyrosine kinase inhibitor for the treatment of Philadelphia chromosome-positive leukemias. An elevation of the pancreatic enzyme level is one of the major adverse events associated with nilotinib, but whether or not nilotinib induces symptomatic pancreatitis remains to be elucidated. The cases of two chronic myeloid leukemia patients treated with nilotinib who developed symptomatic acute pancreatitis on the third and fifth day of nilotinib administration are herein presented. Since both patients had no other etiologies for pancreatitis, nilotinib was considered to be the causal agent. The withdrawal of nilotinib resulted in a prompt recovery. These cases underline the importance of recognizing pancreatitis as a possible adverse event associated with nilotinib.
Fujimi A, Sakamoto H, Kanisawa Y, et al.
Pneumatosis intestinalis during chemotherapy with nilotinib in a patient with chronic myeloid leukemia who tested positive for anti-topoisomerase I antibodies.
Clin J Gastroenterol. 2016; 9(6):358-364 [PubMed] Related Publications
Pneumatosis intestinalis during chemotherapy with nilotinib in a patient with chronic myeloid leukemia who tested positive for anti-topoisomerase I antibodies.
Clin J Gastroenterol. 2016; 9(6):358-364 [PubMed] Related Publications
A 55-year-old man with several comorbidities including idiopathic interstitial pneumonia under long-term corticosteroid therapy, longstanding myocardial infarction, chronic heart failure, paroxysmal atrial fibrillation, gastro-esophageal reflux disease, constipation, and history of paralytic ileus, was diagnosed with chronic myelogenous leukemia (CML) in the chronic phase. He also tested positive for anti-topoisomerase I antibodies without clinical diagnosis of any connective tissue disease, including systemic sclerosis. Approximately 5 months after the initiation of nilotinib for CML, he developed upper abdominal distension with intermitting abdominal pain, and based on abdominal computed tomography findings, a diagnosis of pneumatosis intestinalis (PI) was made. Five courses of hyperbaric oxygen therapy quickly eliminated the PI and related symptoms without the cessation of nilotinib and, thereafter, additional oral prokinetic agents and non-absorbable antibiotics ensured the non-recurrence of PI. At 6 and 18 months after commencing nilotinib therapy, major and complete molecular response were achieved, respectively. It is suspected that both gastrointestinal hypokinesis related to the presence of anti-topoisomerase I antibodies and mucosal permeability due to corticosteroid therapy had existed. Thus, subsequent administration of nilotinib may have triggered PI by depressing gastrointestinal motility via the inhibition of c-kit.
Katagiri S, Tauchi T, Saito Y, et al.
Musculoskeletal pain after stopping tyrosine kinase inhibitor in patients with chronic myeloid leukemia: a questionnaire survey.
Rinsho Ketsueki. 2016; 57(7):873-6 [PubMed] Related Publications
Musculoskeletal pain after stopping tyrosine kinase inhibitor in patients with chronic myeloid leukemia: a questionnaire survey.
Rinsho Ketsueki. 2016; 57(7):873-6 [PubMed] Related Publications
We conducted a questionnaire survey to assess the state of patients with CML after discontinuation of TKI therapy. Nine of 27 patients developed musculoskeletal pain after TKI discontinuation. One had discontinued nilotinib and eight had discontinued imatinib therapy. Median time to symptom development after discontinuation was 2 weeks. Four experienced grade 3 symptoms as per the CTCAE ver. 4.0. One had pain persisting over a period of 21 months. There was a significant difference between patients with and without symptoms as regards female gender and the probability of persistent MMR. Awareness of this withdrawal syndrome after TKI discontinuation is imperative.
Neuendorff NR, Burmeister T, Dörken B, Westermann J
BCR-ABL-positive acute myeloid leukemia: a new entity? Analysis of clinical and molecular features.
Ann Hematol. 2016; 95(8):1211-21 [PubMed] Related Publications
BCR-ABL-positive acute myeloid leukemia: a new entity? Analysis of clinical and molecular features.
Ann Hematol. 2016; 95(8):1211-21 [PubMed] Related Publications
BCR-ABL-positive acute myeloid leukemia (AML) is a rare subtype of AML that is now included as a provisional entity in the 2016 revised WHO classification of myeloid malignancies. Since a clear distinction between de novo BCR-ABL+ AML and chronic myeloid leukemia (CML) blast crisis is challenging in many cases, the existence of de novo BCR-ABL+ AML has been a matter of debate for a long time. However, there is increasing evidence suggesting that BCR-ABL+ AML is in fact a distinct subgroup of AML. In this study, we analyzed all published cases since 1975 as well as cases from our institution in order to present common clinical and molecular features of this rare disease. Our analysis shows that BCR-ABL predominantly occurs in AML-NOS, CBF leukemia, and AML with myelodysplasia-related changes. The most common BCR-ABL transcripts (p190 and p210) are nearly equally distributed. Based on the analysis of published data, we provide a clinical algorithm for the initial differential diagnosis of BCR-ABL+ AML. The prognosis of BCR-ABL+ AML seems to depend on the cytogenetic and/or molecular background rather than on BCR-ABL itself. A therapy with tyrosine kinase inhibitors (TKIs) such as imatinib, dasatinib, or nilotinib is reasonable, but-due to a lack of systematic clinical data-their use cannot be routinely recommended in first-line therapy. Beyond first-line treatment of AML, the use of TKI remains an individual decision, both in combination with intensive chemotherapy and/or as a bridge to allogeneic stem cell transplantation. In each single case, potential benefits have to be weighed against potential risks.
Kramer B, Hock C, Birk R, et al.
Targeted Therapies in HPV-positive and -negative HNSCC - Alteration of EGFR and VEGFR-2 Expression In Vitro.
Anticancer Res. 2016; 36(6):2799-807 [PubMed] Related Publications
Targeted Therapies in HPV-positive and -negative HNSCC - Alteration of EGFR and VEGFR-2 Expression In Vitro.
Anticancer Res. 2016; 36(6):2799-807 [PubMed] Related Publications
BACKGROUND: Angiogenesis plays a crucial role in the formation and progression of tumor growth in head and neck squamous cell carcinoma (HNSCC). The tyrosine kinase receptors epidermal growth factor receptor (EGFR) and vascular endothelial growth factor receptor (VEGFR) are essential for mediation of pro-angiogenic signals. Nilotinib, dasatinib, erlotinib and gefitinib are tyrosine kinase inhibitors and approved as targeted therapies for several tumor entities other than HNSCC. In this study, we sought to evaluate the alteration of EGFR and VEGFR-2 expression by these tyrosine kinase inhibitors with respect to the human papillomavirus (HPV)-status in squamous cell carcinoma (SCC) tumor cells.
MATERIALS AND METHODS: Expression patterns of EGFR and VEGFR-2 were determined by enzyme linked immunosorbent assay (ELISA) in HNSCC 11A, HNSCC 14C and p-16-positive CERV196 tumor cell lines. These cells were incubated with nilotinib, dasatinib, erlotinib and gefitinib (5-20μmol/l) and compared to a chemonaive control. The incubation time was 24, 48, 72 and 96 h.
RESULTS: All tested substances led to a statistically significant reduction (p<0.05) of EGFR protein expression levels in HPV-negative cells compared to the negative control. Surprisingly, a statistically significant increase in VEGFR-2 expression was observed after exposure to all tested substances especially after exposure to erlotinib treatment.
CONCLUSION: Nilotinib, dasatinib, erlotinib and gefitinib cause significant changes in protein expression of EGFR and VEGFR-2 in vitro. Besides the anti-angiogenic impact of the substances, as shown for the decrease of EGFR expression, we also observed an increase of VEGFR-2 expression. These contradictive effects could be interpreted as a compensatory up-regulation by the tumor cell.
MATERIALS AND METHODS: Expression patterns of EGFR and VEGFR-2 were determined by enzyme linked immunosorbent assay (ELISA) in HNSCC 11A, HNSCC 14C and p-16-positive CERV196 tumor cell lines. These cells were incubated with nilotinib, dasatinib, erlotinib and gefitinib (5-20μmol/l) and compared to a chemonaive control. The incubation time was 24, 48, 72 and 96 h.
RESULTS: All tested substances led to a statistically significant reduction (p<0.05) of EGFR protein expression levels in HPV-negative cells compared to the negative control. Surprisingly, a statistically significant increase in VEGFR-2 expression was observed after exposure to all tested substances especially after exposure to erlotinib treatment.
CONCLUSION: Nilotinib, dasatinib, erlotinib and gefitinib cause significant changes in protein expression of EGFR and VEGFR-2 in vitro. Besides the anti-angiogenic impact of the substances, as shown for the decrease of EGFR expression, we also observed an increase of VEGFR-2 expression. These contradictive effects could be interpreted as a compensatory up-regulation by the tumor cell.
Hino Y, Doki N, Yamamoto K, et al.
Chronic myeloid leukemia relapsing ten years after allogenic bone marrow transplantation.
Rinsho Ketsueki. 2016; 57(5):608-12 [PubMed] Related Publications
Chronic myeloid leukemia relapsing ten years after allogenic bone marrow transplantation.
Rinsho Ketsueki. 2016; 57(5):608-12 [PubMed] Related Publications
A 58-year-old female was diagnosed with Philadelphia chromosome positive chronic myeloid leukemia (CML) in blast crisis (BC) in 2004. The patient received imatinib, which quickly induced molecular remission, and subsequently underwent bone marrow transplantation (BMT) from an unrelated human leukocyte antigen (HLA)-identical donor. The post-transplant clinical course was essentially uneventful. In 2014, ten years after the BMT, the patient was admitted to our hospital complaining of lymphadenopathy, and blasts were observed in peripheral blood. The patient was diagnosed as having a CML relapse in myeloid BC, with leukemic infiltration in lymph nodes, and was treated with dasatinib. Subsequently, pleural effusion developed and nilotinib was administered, which induced normal blood counts without blasts and partial cytogenetic remission, one month after administration. Six months after the relapse, this patient underwent a second BMT from an HLA-matched unrelated donor. Recent studies have demonstrated the cumulative incidence of CML relapse more than five years after allogeneic hematopoietic stem cell transplantation (allo-HSCT) to be higher than in acute myeloid leukemia. Although rare, the possibility of late relapse should be considered in patients diagnosed with CML after allo-HSCT.
Tantiworawit A, Kongjarern S, Rattarittamrong E, et al.
Diagnosis and Monitoring of Chronic Myeloid Leukemia: Chiang Mai University Experience.
Asian Pac J Cancer Prev. 2016; 17(4):2159-64 [PubMed] Related Publications
Diagnosis and Monitoring of Chronic Myeloid Leukemia: Chiang Mai University Experience.
Asian Pac J Cancer Prev. 2016; 17(4):2159-64 [PubMed] Related Publications
BACKGROUND: A diagnosis of chronic myeloid leukemia (CML) is made on discovery of the presence of a Philadelphia (Ph) chromosome. The success of the treatment of this form of leukemia with tyrosine kinase inhibitor (TKI) is monitored by reduction of the Ph chromosome.
OBJECTIVE: To compare the role of conventional cytogenetic (CC) methods with a real time quantitative polymerase chain reaction (RQ-PCR) and fluorescence in situ hybridization (FISH) for diagnosis and treatment monitoring of CML patients. The secondary outcome was to analyze the treatment responses to TKI in CML patients.
MATERIALS AND METHODS: This was a retrospective study of CML patients who attended the Hematology clinic at Chiang Mai University Hospital from 2005-2010. Medical records were reviewed for demographic data, risk score, treatment response and the results of CC methods, FISH and RQ-PCR.
RESULTS: One hundred and twenty three cases were included in the study, 57.7% of whom were male with a mean age of 46.9 years. Most of the patients registered as intermediate to high risk on the Sokal score. At diagnosis, 121 patients were tested using the CC method and 118 (95.9%) were identified as positive. Five patients failed to be diagnosed by CC methods but were positive for BCR-ABL1 using the FISH method. Imatinib was the first-line treatment used in 120 patients (97.6%). In most patients (108 out of 122, 88.5%), a complete cytogenetic response (CCyR) was achieved after TKI therapy and in 86 patients (70.5%) CCyR was achieved long term by the CC method. Five out of the 35 analyzed patients in which CCyR was achieved by the CC method had a positive FISH result. Out of the 76 patients in which CCyR was achieved, RQ-PCR classified patients to only CCyR in 17 patients (22.4%) with a deeper major molecular response (MMR) in 4 patients (5.3%) and complete molecular response (CMR) in 55 patients (72.4%). In the case of initial therapy, CCyR was achieved in 95 patients (79.1%) who received imatinib and in both patients who received dasatinib (100%). For the second line treatment, nilotinib were used in 30 patients and in 19 of them (63.3%) CCyR was achieved. In half of the 6 patients (50%) who received dasatinib as second line or third line treatment CCyR was also achieved.
CONCLUSIONS: CML patients had a good response to TKI treatment. FISH could be useful for diagnosis in cases where CC analysis failed to detect the Ph chromosome. RQ-PCR was helpful in detecting any residual disease and determining the depth of the treatment response at levels greater than the CC methods.
OBJECTIVE: To compare the role of conventional cytogenetic (CC) methods with a real time quantitative polymerase chain reaction (RQ-PCR) and fluorescence in situ hybridization (FISH) for diagnosis and treatment monitoring of CML patients. The secondary outcome was to analyze the treatment responses to TKI in CML patients.
MATERIALS AND METHODS: This was a retrospective study of CML patients who attended the Hematology clinic at Chiang Mai University Hospital from 2005-2010. Medical records were reviewed for demographic data, risk score, treatment response and the results of CC methods, FISH and RQ-PCR.
RESULTS: One hundred and twenty three cases were included in the study, 57.7% of whom were male with a mean age of 46.9 years. Most of the patients registered as intermediate to high risk on the Sokal score. At diagnosis, 121 patients were tested using the CC method and 118 (95.9%) were identified as positive. Five patients failed to be diagnosed by CC methods but were positive for BCR-ABL1 using the FISH method. Imatinib was the first-line treatment used in 120 patients (97.6%). In most patients (108 out of 122, 88.5%), a complete cytogenetic response (CCyR) was achieved after TKI therapy and in 86 patients (70.5%) CCyR was achieved long term by the CC method. Five out of the 35 analyzed patients in which CCyR was achieved by the CC method had a positive FISH result. Out of the 76 patients in which CCyR was achieved, RQ-PCR classified patients to only CCyR in 17 patients (22.4%) with a deeper major molecular response (MMR) in 4 patients (5.3%) and complete molecular response (CMR) in 55 patients (72.4%). In the case of initial therapy, CCyR was achieved in 95 patients (79.1%) who received imatinib and in both patients who received dasatinib (100%). For the second line treatment, nilotinib were used in 30 patients and in 19 of them (63.3%) CCyR was achieved. In half of the 6 patients (50%) who received dasatinib as second line or third line treatment CCyR was also achieved.
CONCLUSIONS: CML patients had a good response to TKI treatment. FISH could be useful for diagnosis in cases where CC analysis failed to detect the Ph chromosome. RQ-PCR was helpful in detecting any residual disease and determining the depth of the treatment response at levels greater than the CC methods.
Fajardo S, Zook F, Dotson E
Specialty pharmacy for hematologic malignancies.
Am J Health Syst Pharm. 2016; 73(11):797-809 [PubMed] Related Publications
Specialty pharmacy for hematologic malignancies.
Am J Health Syst Pharm. 2016; 73(11):797-809 [PubMed] Related Publications
PURPOSE: The oral oncology medications used in the treatment of chronic lymphocytic leukemia, chronic myeloid leukemia, multiple myeloma, and non-Hodgkin's lymphoma are reviewed, and the specialty pharmacy services at three large academic medical centers are described.
SUMMARY: More than one dozen oral oncology medications are being used for hematologic malignancies and afford patients increased convenience and the potential to improve their quality of life. These agents include ibrutinib, idelalisib, imatinib, dasatinib, nilotinib, bosutinib, ponatinib, thalidomide, lenalidomide, pomalidomide, panobinostat, ixazomib, and vorinostat. Despite the benefits of an autonomous-driven patient care plan, these high-risk, high-cost treatments are not without their challenges. Oral oncology medications are associated with significant barriers to adherence, including low health literacy, patient forgetfulness, complex administration instructions, troublesome adverse effects, and high copayments. Many outpatient cancer center pharmacies associated with large academic medical centers are now applying for specialty pharmacy designation. This affords the onsite dispensing pharmacy access to once-limited oral oncology medications that can be dispensed to clinic patients. In addition, the specialty pharmacy services offered within these cancer centers bridge an important gap in patient care and improve the care provided to oncology patients.
CONCLUSION: As oral oncology agents continue to be approved by FDA, oncology treatment teams must establish a comprehensive plan for their management. Because of their pharmacologic expertise, access to patients' medical records, and unique position within ambulatory care oncology teams, pharmacists can play an important role in patient education, laboratory monitoring, medication adherence, and cost saving.
SUMMARY: More than one dozen oral oncology medications are being used for hematologic malignancies and afford patients increased convenience and the potential to improve their quality of life. These agents include ibrutinib, idelalisib, imatinib, dasatinib, nilotinib, bosutinib, ponatinib, thalidomide, lenalidomide, pomalidomide, panobinostat, ixazomib, and vorinostat. Despite the benefits of an autonomous-driven patient care plan, these high-risk, high-cost treatments are not without their challenges. Oral oncology medications are associated with significant barriers to adherence, including low health literacy, patient forgetfulness, complex administration instructions, troublesome adverse effects, and high copayments. Many outpatient cancer center pharmacies associated with large academic medical centers are now applying for specialty pharmacy designation. This affords the onsite dispensing pharmacy access to once-limited oral oncology medications that can be dispensed to clinic patients. In addition, the specialty pharmacy services offered within these cancer centers bridge an important gap in patient care and improve the care provided to oncology patients.
CONCLUSION: As oral oncology agents continue to be approved by FDA, oncology treatment teams must establish a comprehensive plan for their management. Because of their pharmacologic expertise, access to patients' medical records, and unique position within ambulatory care oncology teams, pharmacists can play an important role in patient education, laboratory monitoring, medication adherence, and cost saving.
Jiang Q, Liu ZC, Zhang SX, Gale RP
Young age and high cost are associated with future preference for stopping tyrosine kinase inhibitor therapy in Chinese with chronic myeloid leukemia.
J Cancer Res Clin Oncol. 2016; 142(7):1539-47 [PubMed] Related Publications
Young age and high cost are associated with future preference for stopping tyrosine kinase inhibitor therapy in Chinese with chronic myeloid leukemia.
J Cancer Res Clin Oncol. 2016; 142(7):1539-47 [PubMed] Related Publications
PURPOSE: To explore therapy-goals and patients' expectations regarding discontinuing tyrosine kinase inhibitors (TKIs) therapy in Chinese with chronic myeloid leukemia (CML). To identify variables associated with these expectations and preferences.
METHODS: Noninterventional, cross-sectional study using questionnaires distributed to persons with CML and answered anonymously.
RESULTS: With CML in chronic phase, 888 respondents were evaluable. In total, 513 respondents (58 %) were male. Median age was 41 years (range 18-88 years). Median TKI therapy duration was 3 years (range <1-13 years). In total, 735 respondents (83 %) paid part or all of the cost of TKI. As their treatment goal, 430 of 888 respondents (48 %) reported treatment-free remission (TFR). In the future, 734 respondents (83 %) expected to discontinue TKI. Multivariate analyses confirmed younger age [HR = 1.3; (1.1, 1.4); P < 0.001] and higher out-of-pocket expense [HR = 1.2; (1.1, 1.4); P < 0.001] were associated with TFR as a therapy-goal. Both variables were also associated with patients' hope to stop TKI therapy in the future: HR = 1.4; (0.8, 1.7; P < 0.001) and HR = 1.5; (1.3, 1.8; P < 0.001). Achieving a complete molecular response [HR = 1.8 (1.1, 2.9); P = 0.017] and decreased quality of life resulting from adverse effects [HR = 1.2; (1.0, 1.5); P = 0.021] were factors associated with the expectation of discontinuing TKI therapy.
CONCLUSIONS: Younger age and higher out-of-pocket cost are associated with patients' preference for stopping TKI therapy.
METHODS: Noninterventional, cross-sectional study using questionnaires distributed to persons with CML and answered anonymously.
RESULTS: With CML in chronic phase, 888 respondents were evaluable. In total, 513 respondents (58 %) were male. Median age was 41 years (range 18-88 years). Median TKI therapy duration was 3 years (range <1-13 years). In total, 735 respondents (83 %) paid part or all of the cost of TKI. As their treatment goal, 430 of 888 respondents (48 %) reported treatment-free remission (TFR). In the future, 734 respondents (83 %) expected to discontinue TKI. Multivariate analyses confirmed younger age [HR = 1.3; (1.1, 1.4); P < 0.001] and higher out-of-pocket expense [HR = 1.2; (1.1, 1.4); P < 0.001] were associated with TFR as a therapy-goal. Both variables were also associated with patients' hope to stop TKI therapy in the future: HR = 1.4; (0.8, 1.7; P < 0.001) and HR = 1.5; (1.3, 1.8; P < 0.001). Achieving a complete molecular response [HR = 1.8 (1.1, 2.9); P = 0.017] and decreased quality of life resulting from adverse effects [HR = 1.2; (1.0, 1.5); P = 0.021] were factors associated with the expectation of discontinuing TKI therapy.
CONCLUSIONS: Younger age and higher out-of-pocket cost are associated with patients' preference for stopping TKI therapy.
Žáčková M, Macháčková-Lopotová T, Ondráčková Z, et al.
Simplifying procedure for prediction of resistance risk in CML patients - Test of sensitivity to TKI ex vivo.
Blood Cells Mol Dis. 2016; 58:67-75 [PubMed] Related Publications
Simplifying procedure for prediction of resistance risk in CML patients - Test of sensitivity to TKI ex vivo.
Blood Cells Mol Dis. 2016; 58:67-75 [PubMed] Related Publications
Tyrosine kinase inhibitors (TKIs) targeting BCR-ABL have dramatically improved chronic myeloid leukemia therapy. While imatinib remains to be the first line therapy, about 30% of patients develop resistance or intolerance to this drug and are recommended to switch to other TKIs. Nilotinib and dasatinib are currently implemented into the first line therapy and other inhibitors have already entered the clinical practice. This opens further questions on how to select the best TKI for each patient not only during the therapy but also at diagnosis. The individualized therapy concept requires a reliable establishment of prognosis and prediction of response to the available TKIs. We tested the ex vivo sensitivity of patient primary leukocytes to imatinib, nilotinib and dasatinib - two concentrations of each inhibitor for 48h incubation - and we evaluated the usefulness of such tests for the clinical practice. Besides reflecting the actual sensitivity to the therapy, our optimized simple tests were able to predict the outcome in 90/87% of patients, for the next 12/24months, respectively. According to these results, the presented ex vivo testing could help clinicians to select the appropriate drug for each patient at diagnosis and also at any time of the therapy.
Karthikeyan C, Malla R, Ashby CR, et al.
Pyrimido[1″,2″:1,5]pyrazolo[3,4-b]quinolines: Novel compounds that reverse ABCG2-mediated resistance in cancer cells.
Cancer Lett. 2016; 376(1):118-26 [PubMed] Related Publications
Pyrimido[1″,2″:1,5]pyrazolo[3,4-b]quinolines: Novel compounds that reverse ABCG2-mediated resistance in cancer cells.
Cancer Lett. 2016; 376(1):118-26 [PubMed] Related Publications
Overexpression of ATP-binding cassette transporter (ABC) subfamily G2 in cancer cells is known to elicit a MDR phenotype, ultimately resulting in cancer chemotherapy failure. Here, we report, for the first time, the effect of eight novel pyrimido[1″,2″:1,5]pyrazolo[3,4-b]quinoline (IND) derivatives that inhibit ABCG2 transporter restoring cancer cell chemosensitivity. IND -4, -5, -6, -7, and -8, at 10 µM, and nilotinib at 5 µM, significantly potentiated (8-10 fold) the cytotoxicity of the ABCG2 substrates mitoxantrone (MX) and doxorubicin in HEK293 cells overexpressing ABCG2 transporter, MX (~14 fold) in MX-resistant NCI-H460/MX-20 small cell lung cancer, and of topotecan (~7 fold) in S1-M1-80 colon cancer cells which all stably expressing ABCG2. In contrast, cytotoxicity of cisplatin, which is not an ABCG2 substrate, was not altered. IND-5,-6,-7, and -8 significantly increased the accumulation of rhodamine-123 in multidrug resistant NCI-H460/MX-20 cells overexpressing ABCG2. Both IND-7 and -8, the most potent ABCG2 inhibitors, had the highest affinities for the binding sites of ABCG2 in modeling studies. In conclusion, the beneficial actions of new class of agents warrant further development as potential MDR reversal agents for clinical anticancer agents that suffer from ABCG2-mediated MDR insensitivity.
Alkeraye S, Dadban A, Lok C, et al.
C-Kit non-mutated metastatic melanoma showing positive response to Nilotinib.
Dermatol Online J. 2016; 22(1) [PubMed] Related Publications
C-Kit non-mutated metastatic melanoma showing positive response to Nilotinib.
Dermatol Online J. 2016; 22(1) [PubMed] Related Publications
Melanoma is an aggressive tumor with advanced disease characterized by widespread metastatic lesions and the tumor has traditionally been resistant to most forms of treatment. Indeed, metastatic melanoma has a very poor prognosis with a median survival time of 8-9 months and an estimated 3-year survival rate of less than 15%. Recent advances in our understanding of the genetic profile of melanoma cells and the molecular factors that drive malignant transformation have resulted in the identification of numerous new therapeutic targets. KIT is an established therapeutic target in cancers with activating mutations of KIT, such as gastrointestinal stromal tumors (GIST), and considerable efficacy has been achieved with various small molecule inhibitors of KIT including imatinib mesylate. Nilotinib is an inhibitor of ligand-induced PDGFRα and PDFGRβ kinase activity and autophosphorylation of constitutively activated KIT harboring exon 13 or exon 11 mutations (IC50 values of 0.2 and 0.027 μmol/L, respectively), with efficacy comparable to that of imatinib. We report a case of non-kit mutated metastatic vaginal melanoma showing impressive response to nilotinib.
Padula WV, Larson RA, Dusetzina SB, et al.
Cost-effectiveness of Tyrosine Kinase Inhibitor Treatment Strategies for Chronic Myeloid Leukemia in Chronic Phase After Generic Entry of Imatinib in the United States.
J Natl Cancer Inst. 2016; 108(7) [PubMed] Free Access to Full Article Related Publications
Cost-effectiveness of Tyrosine Kinase Inhibitor Treatment Strategies for Chronic Myeloid Leukemia in Chronic Phase After Generic Entry of Imatinib in the United States.
J Natl Cancer Inst. 2016; 108(7) [PubMed] Free Access to Full Article Related Publications
BACKGROUND: We analyzed the cost-effectiveness of treating incident chronic myeloid leukemia in chronic phase (CML-CP) with generic imatinib when it becomes available in United States in 2016. In the year following generic entry, imatinib's price is expected to drop 70% to 90%. We hypothesized that initiating treatment with generic imatinib in these patients and then switching to the other tyrosine-kinase inhibitors (TKIs), dasatinib or nilotinib, because of intolerance or lack of effectiveness ("imatinib-first") would be cost-effective compared with the current standard of care: "physicians' choice" of initiating treatment with any one of the three TKIs.
METHODS: We constructed Markov models to compare the five-year cost-effectiveness of imatinib-first vs physician's choice from a US commercial payer perspective, assuming 3% annual discounting ($US 2013). The models' clinical endpoint was five-year overall survival taken from a systematic review of clinical trial results. Per-person spending on incident CML-CP treatment overall care components was estimated using Truven's MarketScan claims data. The main outcome of the models was cost per quality-adjusted life-year (QALY). We interpreted outcomes based on a willingness-to-pay threshold of $100 000/QALY. A panel of European LeukemiaNet experts oversaw the study's conduct.
RESULTS: Both strategies met the threshold. Imatinib-first ($277 401, 3.87 QALYs) offered patients a 0.10 decrement in QALYs at a savings of $88 343 over five years to payers compared with physician's choice ($365 744, 3.97 QALYs). The imatinib-first incremental cost-effectiveness ratio was approximately $883 730/QALY. The results were robust to multiple sensitivity analyses.
CONCLUSION: When imatinib loses patent protection and its price declines, its use will be the cost-effective initial treatment strategy for CML-CP.
METHODS: We constructed Markov models to compare the five-year cost-effectiveness of imatinib-first vs physician's choice from a US commercial payer perspective, assuming 3% annual discounting ($US 2013). The models' clinical endpoint was five-year overall survival taken from a systematic review of clinical trial results. Per-person spending on incident CML-CP treatment overall care components was estimated using Truven's MarketScan claims data. The main outcome of the models was cost per quality-adjusted life-year (QALY). We interpreted outcomes based on a willingness-to-pay threshold of $100 000/QALY. A panel of European LeukemiaNet experts oversaw the study's conduct.
RESULTS: Both strategies met the threshold. Imatinib-first ($277 401, 3.87 QALYs) offered patients a 0.10 decrement in QALYs at a savings of $88 343 over five years to payers compared with physician's choice ($365 744, 3.97 QALYs). The imatinib-first incremental cost-effectiveness ratio was approximately $883 730/QALY. The results were robust to multiple sensitivity analyses.
CONCLUSION: When imatinib loses patent protection and its price declines, its use will be the cost-effective initial treatment strategy for CML-CP.
Malagola M, Papayannidis C, Baccarani M
Tyrosine kinase inhibitors in Ph+ acute lymphoblastic leukaemia: facts and perspectives.
Ann Hematol. 2016; 95(5):681-93 [PubMed] Related Publications
Tyrosine kinase inhibitors in Ph+ acute lymphoblastic leukaemia: facts and perspectives.
Ann Hematol. 2016; 95(5):681-93 [PubMed] Related Publications
Two tyrosine kinase inhibitors (TKIs), imatinib and dasatinib, are registered for the treatment of Philadelphia chromosome-positive (Ph+) acute lymphoblastic leukaemia (ALL) in adults. Other two TKIs (nilotinib and ponatinib) have been tested in the second-line, can offer an alternative in the patients who fail the first-line, and can acquire a role also in the first-line. Here, we provide a summary of the reports of TKIs, used alone, and in combination with chemotherapy. TKIs are very effective alone and with corticosteroids and are likely to improve substantially the outcome when they are combined with standard or dose-adapted chemotherapy. While the complete haematologic remission rate is always very high, close to 100 %, the cytogenetic and molecular remission rates are lower, so that TKIs are still considered as a complement to chemotherapy and as a bridge to allogeneic stem cell transplantation (allo-SCT). However, many patients relapse before transplant, and many patients still relapse, even if they have been submitted to allo-SCT. A proper use of TKIs, the introduction of ponatinib, and of "new generation" TKIs should improve further on the outcome of Ph+ ALL.
Liu B, Zhang W, Ma H
Complete cytogenetic response to Nilotinib in a chronic myeloid leukemia case with a rare e13a3(b2a3) BCR-ABL fusion transcript: A case report.
Mol Med Rep. 2016; 13(3):2635-8 [PubMed] Related Publications
Complete cytogenetic response to Nilotinib in a chronic myeloid leukemia case with a rare e13a3(b2a3) BCR-ABL fusion transcript: A case report.
Mol Med Rep. 2016; 13(3):2635-8 [PubMed] Related Publications
In the present study, an atypical case of chronic myeloid leukemia (CML) in a 32-year-old male was reported. CML cases with e13a3 breakpoint cluster region (BCR)-ABL transcripts are extremely rare. Reverse transcription quantitative‑polymerase chain reaction (RT-qPCR) was initially negative due to the primer corresponding to ABL a2 sequences and diagnosis was based upon analysis of the bone marrow smear, fluorescence in situ hybridization and karyotype analysis. RT‑qPCR analysis with the ABL primer, which was located in ABL exon 3 to enable the detection of fusions with either ABL a2 or exon a3 demonstrated the presence of the BCR‑ABL fusion transcript e13a3. The patient responded well to Nilotinib and achieved a complete cytogenetic response after 3 months.
Jain P, Kantarjian H, Sasaki K, et al.
Analysis of 2013 European LeukaemiaNet (ELN) responses in chronic phase CML across four frontline TKI modalities and impact on clinical outcomes.
Br J Haematol. 2016; 173(1):114-26 [PubMed] Article available free on PMC after 01/04/2017 Related Publications
Analysis of 2013 European LeukaemiaNet (ELN) responses in chronic phase CML across four frontline TKI modalities and impact on clinical outcomes.
Br J Haematol. 2016; 173(1):114-26 [PubMed] Article available free on PMC after 01/04/2017 Related Publications
This study assessed the relevance of 2013 European LeukaemiaNet (ELN) response categories on patients treated with common frontline tyrosine kinase inhibitors (TKI) in chronic myeloid leukaemia in chronic phase (CML-CP). Four hundred and eighty-seven patients treated with imatinib (400 mg; IM 400, n = 70; 800 mg; IM800, n = 201), dasatinib (n = 107) or nilotinib (n = 109) were analysed. Intention to treat (ITT) analysis indicated that the proportion of patients falling into optimal, warning and failure ELN categories were 89%, 6%, 6% at 3 months, 78%, 17% and 6% at 6 months, and 75%, 13% and 13% at 12 months, respectively. Rates of optimal response at 3 months were 75% for IM400, 90% for IM800, 89% for dasatinib and 97% for nilotinib; 41%, 80%, 86% and 89% at 6 months; and 47%, 77%, 76% and 87% at 12 months, respectively. Patients achieving optimal response had longer eventfree (EFS), failurefree (FFS), transformationfree (TFS) and overall survival (OS) compared to warning and failure responses at all-time points. Treatment with imatinib 800, dasatinib or nilotinib predicted for achieving an optimal response. Optimal response predicted for significantly longer EFS, FFS, TFS and OS at 3, 6 and 12 months, irrespective of the TKI modality used. ELN response categories reliably predicted outcomes in CML patients receiving commonly used TKIs.
Pophali PA, Patnaik MM
The Role of New Tyrosine Kinase Inhibitors in Chronic Myeloid Leukemia.
Cancer J. 2016 Jan-Feb; 22(1):40-50 [PubMed] Article available free on PMC after 01/04/2017 Related Publications
The Role of New Tyrosine Kinase Inhibitors in Chronic Myeloid Leukemia.
Cancer J. 2016 Jan-Feb; 22(1):40-50 [PubMed] Article available free on PMC after 01/04/2017 Related Publications
Imatinib mesylate was the first tyrosine kinase inhibitor (TKI) approved for the management of chronic myeloid leukemia. Imatinib produces acceptable responses in approximately 60% of patients, with approximately 20% discontinuing therapy because of intolerance and approximately 20% developing drug resistance. The advent of newer TKIs, such as nilotinib, dasatinib, bosutinib, and ponatinib, has provided multiple options for patients. These agents are more potent, have unique adverse effect profiles, and are more likely to achieve relevant milestones, such as early molecular responses (3-6 months) and optimal molecular responses (12 months). The acquisition of BCR-ABL kinase domain mutations is also reportedly lower with these drugs. Thus far, none of the randomized phase III clinical trials have shown a clinically significant survival difference between frontline imatinib versus newer TKIs. Cost and safety issues with the newer TKIs, such as vascular disease with nilotinib and ponatinib and pulmonary hypertension with dasatinib, have dampened the enthusiasm of using these drugs as frontline options. While the utility of new TKIs in the setting of imatinib failure or intolerance is clear, their use as frontline agents should factor in the age of the patient, additional comorbidities, risk stratification (Sokal score), and cost. Combination therapies and newer agents with potential to eradicate quiescent chronic myeloid leukemia stem cells offers future hope.
Brahmi M, Vinceneux A, Cassier PA
Current Systemic Treatment Options for Tenosynovial Giant Cell Tumor/Pigmented Villonodular Synovitis: Targeting the CSF1/CSF1R Axis.
Curr Treat Options Oncol. 2016; 17(2):10 [PubMed] Related Publications
Current Systemic Treatment Options for Tenosynovial Giant Cell Tumor/Pigmented Villonodular Synovitis: Targeting the CSF1/CSF1R Axis.
Curr Treat Options Oncol. 2016; 17(2):10 [PubMed] Related Publications
OPINION STATEMENT: Adequate surgical resection remains the treatment of choice for tenosyovial giant cell tumor (TGCT). However, diffuse type TGCT (D-TGCT) is more difficult to resect and has a higher rate of recurrence (up to 50 %), which is often multiple. D-TGCT is rarely lethal and only rare cases of metastases have been described. Nevertheless, patients might have a significant decline in their quality of life due to multiple operations, which may sometimes result in a partial loss of function of the affected joint and may also be associated with perioperative morbidity and secondary arthrosis. As of today, no systemic treatment is approved for this rare disease. The aims of systemic therapy in the context of a non-lethal tumor are to reduce surgical morbidity and to preserve function and patient quality of life. Because TGCT is associated with characteristic cytogenetic abnormalities resulting in the overexpression of CSF1, systemic therapies targeting the CSF1/CSF1R axis (imatinib, nilotinib, emactuzumab, and PLX3397) have been tested in patients with locally advanced or relapsed D-TGCT. The more recent and more specific CSF1R inhibitors have shown a very interesting clinical activity with acceptable toxicity in early phase trials. These results will need to be confirmed in larger, ideally randomized, trials. But the high rate of clinical and functional improvement seen in some patients with advanced D-TGCT, often after multiple operations, suggests that these inhibitors will likely have a role in the management of patients with an inoperable disease; the definition of "inoperable TGCT" still requires refinement to reach a consensus. Another point that will need to be addressed is that of "the optimal duration of therapy" for these patients. Indeed, we and others have observed often prolonged clinical benefit and symptomatic relief even after treatment was stopped, with both monoclonal antibodies and tyrosine kinase inhibitors. Responses were observed very early on with emactuzumab and PLX3397, and patients experienced significant symptom improvement within a few weeks of starting therapy (2-4 weeks). Another possible application of CSF1R inhibitors could be used either as a preoperative or postoperative therapy for patients with operable TGCT. However, we currently lack sufficient follow-up to adequately address these questions which will each require specific trial designs. Overall, the striking clinical activity of CSF1R specific inhibitors in TGCT has created great enthusiasm among clinicians, and further development of these agents is clearly medically needed. Nevertheless, further investigations are necessary to validate those treatments and assess how to best incorporate them among other treatment modalities into the overall therapeutic strategy for a given patient.
Sang F, Ding Y, Wang J, et al.
Structure-Activity Relationship Study of Rakicidins: Overcoming Chronic Myeloid Leukemia Resistance to Imatinib with 4-Methylester-Rakicidin A.
J Med Chem. 2016; 59(3):1184-96 [PubMed] Related Publications
Structure-Activity Relationship Study of Rakicidins: Overcoming Chronic Myeloid Leukemia Resistance to Imatinib with 4-Methylester-Rakicidin A.
J Med Chem. 2016; 59(3):1184-96 [PubMed] Related Publications
Natural product rakicidin A induces cell death in TKI-resistant chronic myelogenous leukemia (CML) cells. Therefore, 14 rakicidin A analogues were synthesized via a highly efficient combinatorial strategy and were evaluated against CML cell lines. The conjugated diene moiety was found to be crucial for the anti-CML activity of rakicidin A, and the changes in the configuration(s) at C-2, C-3, C-14, C-15, and C-16 resulted in lower levels of anti-CML activity. The most promising compound was 4-methylester rakicidin A (1a). Compared with rakicidin A, 1a exhibited 2.8-fold greater potency against the imatinib-resistant cell line K562/G(+) and approximately 100-fold enhanced potency compared with that of imatinib. Furthermore, compound 1a demonstrated a significantly lower resistance index against Ba/F3 cells expressing BCR-ABL(T315I) than bosutinib, dasatinib, nilotinib, and ponatinib, while 1a exhibited less effect on normal hematopoietic cells. Preliminary results indicated that 1a down-regulated caspase-3 and PARP, which contributes to its K562 cell inhibitory activity.
Archibald M, Pritchard T, Nehoff H, et al.
A combination of sorafenib and nilotinib reduces the growth of castrate-resistant prostate cancer.
Int J Nanomedicine. 2016; 11:179-200 [PubMed] Article available free on PMC after 01/04/2017 Related Publications
A combination of sorafenib and nilotinib reduces the growth of castrate-resistant prostate cancer.
Int J Nanomedicine. 2016; 11:179-200 [PubMed] Article available free on PMC after 01/04/2017 Related Publications
Castrate-resistant prostate cancer (CRPC) remains incurable due to the lack of effective therapies. Several tyrosine kinases have been implicated in the development and growth of CRPC, as such targeting these kinases may offer an alternative therapeutic strategy. We established the combination of two tyrosine kinase inhibitors (TKIs), sorafenib and nilotinib, as the most cytotoxic. In addtion, to improve their bioavailability and reduce their metabolism, we encapsulated sorafenib and nilotinib into styrene-co-maleic acid micelles. The micelles' charge, size, and release rate were characterized. We assessed the effect of the combination on the cytotoxicity, cell cycle, apoptosis, protein expression, tumor spheroid integrity, migration, and invasion. The micelles exhibited a mean diameter of 100 nm, a neutral charge, and appeared highly stable. The micellar TKIs promoted greater cytotoxicity, decreased cell proliferation, and increased apoptosis relative to the free TKIs. In addition, the combination reduced the expression and activity of several tyrosine kinases and reduced tumor spheroid integrity and metastatic potential of CRPC cell lines more efficiently than the single treatments. The combination increased the therapeutic potential and demonstrated the relevance of a targeted combination therapy for the treatment of CRPC. In addition, the efficacy of the encapsulated drugs provides the basis for an in vivo preclinical testing.
Jabbour E, Kantarjian H
Chronic myeloid leukemia: 2016 update on diagnosis, therapy, and monitoring.
Am J Hematol. 2016; 91(2):252-65 [PubMed] Related Publications
Chronic myeloid leukemia: 2016 update on diagnosis, therapy, and monitoring.
Am J Hematol. 2016; 91(2):252-65 [PubMed] Related Publications
DISEASE OVERVIEW: Chronic Myeloid Leukemia (CML) is a myeloproliferative neoplasm with an incidence of 1-2 cases per 100,000 adults. It accounts for approximately 15% of newly diagnosed cases of leukemia in adults.
DIAGNOSIS: CML is characterized by a balanced genetic translocation, t(9;22)(q34;q11.2), involving a fusion of the Abelson gene (ABL1) from chromosome 9q34 with the breakpoint cluster region (BCR) gene on chromosome 22q11.2. This rearrangement is known as the Philadelphia chromosome. The molecular consequence of this translocation is the generation of a BCR-ABL1 fusion oncogene, which in turn translates into a BCR-ABL oncoprotein. Frontline therapy: Three tyrosine kinase inhibitors (TKIs), imatinib, nilotinib, and dasatinib are approved by the United States Food and Drug Administration for first-line treatment of patients with newly diagnosed CML in chronic phase (CML-CP). Clinical trials with 2nd generation TKIs reported significantly deeper and faster responses; their impact on long-term survival remains to be determined. Salvage therapy: For patients who fail frontline therapy, second-line options include second and third generation TKIs. Although second and third generation TKIs are potent and selective TKIs, they exhibit unique pharmacological profiles and response patterns relative to different patient and disease characteristics, such as patients' comorbidities, disease stage, and BCR-ABL1 mutational status. Patients who develop the T315I "gatekeeper" mutation display resistance to all currently available TKIs except ponatinib. Allogeneic stem cell transplantation remains an important therapeutic option for patients with CML-CP who have failed at least two TKIs, and for all patients in advanced phase disease.
DIAGNOSIS: CML is characterized by a balanced genetic translocation, t(9;22)(q34;q11.2), involving a fusion of the Abelson gene (ABL1) from chromosome 9q34 with the breakpoint cluster region (BCR) gene on chromosome 22q11.2. This rearrangement is known as the Philadelphia chromosome. The molecular consequence of this translocation is the generation of a BCR-ABL1 fusion oncogene, which in turn translates into a BCR-ABL oncoprotein. Frontline therapy: Three tyrosine kinase inhibitors (TKIs), imatinib, nilotinib, and dasatinib are approved by the United States Food and Drug Administration for first-line treatment of patients with newly diagnosed CML in chronic phase (CML-CP). Clinical trials with 2nd generation TKIs reported significantly deeper and faster responses; their impact on long-term survival remains to be determined. Salvage therapy: For patients who fail frontline therapy, second-line options include second and third generation TKIs. Although second and third generation TKIs are potent and selective TKIs, they exhibit unique pharmacological profiles and response patterns relative to different patient and disease characteristics, such as patients' comorbidities, disease stage, and BCR-ABL1 mutational status. Patients who develop the T315I "gatekeeper" mutation display resistance to all currently available TKIs except ponatinib. Allogeneic stem cell transplantation remains an important therapeutic option for patients with CML-CP who have failed at least two TKIs, and for all patients in advanced phase disease.
Sasaki K, Lahoti A, Jabbour E, et al.
Clinical Safety and Efficacy of Nilotinib or Dasatinib in Patients With Newly Diagnosed Chronic-Phase Chronic Myelogenous Leukemia and Pre-Existing Liver and/or Renal Dysfunction.
Clin Lymphoma Myeloma Leuk. 2016; 16(3):152-62 [PubMed] Free Access to Full Article Related Publications
Clinical Safety and Efficacy of Nilotinib or Dasatinib in Patients With Newly Diagnosed Chronic-Phase Chronic Myelogenous Leukemia and Pre-Existing Liver and/or Renal Dysfunction.
Clin Lymphoma Myeloma Leuk. 2016; 16(3):152-62 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: The safety and efficacy of front-line nilotinib and dasatinib in patients with newly diagnosed chronic-phase chronic myelogenous leukemia (CML-CP) with pre-existing liver and/or renal dysfunction are unknown.
PATIENTS AND METHODS: We analyzed the adverse event rates, response rates, and survival rates of 215 patients with CML-CP with or without renal and/or liver dysfunction who had been treated with front-line nilotinib (n = 108) or dasatinib (n = 107).
RESULTS: The overall median follow-up period was 49 months. At baseline, 6 dasatinib-treated patients (6%) had mild renal dysfunction and 13 (12%) had mild liver dysfunction. Also, 8 nilotinib-treated patients (7%) had mild renal dysfunction, 1 (1%) moderate renal dysfunction, and 9 (8%) mild liver dysfunction. No significant differences were found in the rate of complete cytogenetic response, major molecular response, or molecular response by a 4.5 log reduction on the international scale between the organ function cohorts. Dasatinib- or nilotinib-treated patients with baseline renal dysfunction had a greater incidence of transient reversible acute kidney injury (P = .011 and P < .001), and nilotinib-treated patients with renal dysfunction had a greater incidence of bleeding (P < .001).
CONCLUSION: Patients with CML-CP and mild to moderate renal or liver dysfunction can be safely treated with front-line dasatinib or nilotinib and can achieve response rates similar to those of patients with CML-CP without organ dysfunction.
PATIENTS AND METHODS: We analyzed the adverse event rates, response rates, and survival rates of 215 patients with CML-CP with or without renal and/or liver dysfunction who had been treated with front-line nilotinib (n = 108) or dasatinib (n = 107).
RESULTS: The overall median follow-up period was 49 months. At baseline, 6 dasatinib-treated patients (6%) had mild renal dysfunction and 13 (12%) had mild liver dysfunction. Also, 8 nilotinib-treated patients (7%) had mild renal dysfunction, 1 (1%) moderate renal dysfunction, and 9 (8%) mild liver dysfunction. No significant differences were found in the rate of complete cytogenetic response, major molecular response, or molecular response by a 4.5 log reduction on the international scale between the organ function cohorts. Dasatinib- or nilotinib-treated patients with baseline renal dysfunction had a greater incidence of transient reversible acute kidney injury (P = .011 and P < .001), and nilotinib-treated patients with renal dysfunction had a greater incidence of bleeding (P < .001).
CONCLUSION: Patients with CML-CP and mild to moderate renal or liver dysfunction can be safely treated with front-line dasatinib or nilotinib and can achieve response rates similar to those of patients with CML-CP without organ dysfunction.
Kujak C, Kolesar JM
Treatment of chronic myelogenous leukemia.
Am J Health Syst Pharm. 2016; 73(3):113-20 [PubMed] Related Publications
Treatment of chronic myelogenous leukemia.
Am J Health Syst Pharm. 2016; 73(3):113-20 [PubMed] Related Publications
PURPOSE: Treatment options for chronic-phase chronic myelogenous leukemia (CML) based on medication-resistant mutations in BCR-ABL are reviewed.
SUMMARY: Imatinib, nilotinib, and dasatinib are first-line therapies for chronic-phase CML. Nilotinib or dasatinib can be used as first- or second-line treatment, with nilotinib preferred in patients with BCR-ABL F317 and V229 mutations and dasatinib in patients with Y253H, E255, and F359 mutations. All three medications are associated with neutropenia, thrombocytopenia, and anemia; the reported rates varied but ranged from 38% to 90% in Phase III studies. Although less data are available for bosutinib, the drug can be used as second-line therapy and is effective against F317L, Y253H, and F359 mutations. Mutations at position T315I are generally resistant to all of these tyrosine kinase inhibitors (TKIs) but may respond to ponatinib or omacetaxine. The choice of third-line therapy can be driven by mutational analysis or patient-specific characteristics. While ponatinib and omacetaxine have activity in patients with T351I mutations, they have not been directly compared. Differences in patient characteristics and adverse-effect profiles may also aid in the selection of appropriate therapy.
CONCLUSION: Several TKIs are effective in the treatment of chronic-phase CML. Imatinib, nilotinib, or dasatinib may be used as first-line therapy, while second- and third-line treatments are determined based on previous failed therapy as well as BCR-ABL mutation status.
SUMMARY: Imatinib, nilotinib, and dasatinib are first-line therapies for chronic-phase CML. Nilotinib or dasatinib can be used as first- or second-line treatment, with nilotinib preferred in patients with BCR-ABL F317 and V229 mutations and dasatinib in patients with Y253H, E255, and F359 mutations. All three medications are associated with neutropenia, thrombocytopenia, and anemia; the reported rates varied but ranged from 38% to 90% in Phase III studies. Although less data are available for bosutinib, the drug can be used as second-line therapy and is effective against F317L, Y253H, and F359 mutations. Mutations at position T315I are generally resistant to all of these tyrosine kinase inhibitors (TKIs) but may respond to ponatinib or omacetaxine. The choice of third-line therapy can be driven by mutational analysis or patient-specific characteristics. While ponatinib and omacetaxine have activity in patients with T351I mutations, they have not been directly compared. Differences in patient characteristics and adverse-effect profiles may also aid in the selection of appropriate therapy.
CONCLUSION: Several TKIs are effective in the treatment of chronic-phase CML. Imatinib, nilotinib, or dasatinib may be used as first-line therapy, while second- and third-line treatments are determined based on previous failed therapy as well as BCR-ABL mutation status.
Parker WT, Yeung DT, Yeoman AL, et al.
The impact of multiple low-level BCR-ABL1 mutations on response to ponatinib.
Blood. 2016; 127(15):1870-80 [PubMed] Free Access to Full Article Related Publications
The impact of multiple low-level BCR-ABL1 mutations on response to ponatinib.
Blood. 2016; 127(15):1870-80 [PubMed] Free Access to Full Article Related Publications
The third-generation tyrosine kinase inhibitor (TKI) ponatinib shows activity against all common BCR-ABL1 single mutants, including the highly resistant BCR-ABL1-T315I mutant, improving outcome for patients with refractory chronic myeloid leukemia (CML). However, responses are variable, and causal baseline factors have not been well-studied. The type and number of low-level BCR-ABL1 mutations present after imatinib resistance has prognostic significance for subsequent treatment with nilotinib or dasatinib as second-line therapy. We therefore investigated the impact of low-level mutations detected by sensitive mass-spectrometry before ponatinib initiation (baseline) on treatment response in 363 TKI-resistant patients enrolled in the PONATINIB for Chronic Myeloid Leukemia Evaluation and Ph(+)Acute Lymphoblastic Leukemia trial, including 231 patients in chronic phase (CP-CML). Low-level mutations were detected in 53 patients (15%, including low-level T315I in 14 patients); most, however, did not undergo clonal expansion during ponatinib treatment and, moreover, no specific individual mutations were associated with inferior outcome. We demonstrate however, that the number of mutations detectable by mass spectrometry after TKI resistance is associated with response to ponatinib treatment and could be used to refine the therapeutic approach. Although CP-CML patients with T315I (63/231, 27%) had superior responses overall, those with multiple mutations detectable by mass spectrometry (20, 32%) had substantially inferior responses compared with those with T315I as the sole mutation detected (43, 68%). In contrast, for CP-CML patients without T315I, the inferior responses previously observed with nilotinib/dasatinib therapy for imatinib-resistant patients with multiple mutations were not seen with ponatinib treatment, suggesting that ponatinib may prove to be particularly advantageous for patients with multiple mutations detectable by mass spectrometry after TKI resistance.
Jabbour E
Chronic myeloid leukemia: First-line drug of choice.
Am J Hematol. 2016; 91(1):59-66 [PubMed] Related Publications
Chronic myeloid leukemia: First-line drug of choice.
Am J Hematol. 2016; 91(1):59-66 [PubMed] Related Publications
The advent of tyrosine kinase inhibitors (TKIs) has drastically changed the treatment outcome of chronic myeloid leukemia (CML). Imatinib was the first TKI approved, and has been considered the standard of care for more than a decade. Second generation compounds, namely dasatinib and nilotinib, are highly effective in newly diagnosed patients as well as those who fail imatinib. Second generation TKIs have been demonstrated to induce deeper and faster responses compared to imatinib, however no survival advantage has been observed so far. Today, the expected survival of CML patients, if properly managed, is likely to be similar to the general population. Clinicians are faced the challenge of making decision for which TKI to choose upfront. Comorbidities of the patient, the side effect profile, and the cost of the TKI of interest should be an important consideration in decision making. Whatever TKI is chosen as frontline, noncompliance or treatment failure should be recognized early as a prompt intervention increases the chance of achieving best possible response. Herein, we review the frontline options for the management of patients with CML and how to best choose these agents.
Sayin I, Ayli M, Oğuz AK, Seval GC
Xanthelasma palpebrarum: a new side effect of nilotinib.
BMJ Case Rep. 2016; 2016 [PubMed] Related Publications
Xanthelasma palpebrarum: a new side effect of nilotinib.
BMJ Case Rep. 2016; 2016 [PubMed] Related Publications
Chronic myeloid leucaemia (CML) is a chronic myeloproliferative disorder characterised by a reciprocal translocation between the chromosomes 9 and 22 resulting in constitutionally active tyrosine kinase signalling. BCR-ABL tyrosine kinase inhibitors (TKIs) are highly effective molecules in the treatment of CML. Unfortunately, these novel therapeutic agents are accompanied by various side effects, and haematological, cutaneous and metabolic abnormalities are among the most prevalent. Nilotinib, a second-generation TKI, has been shown to cause both--cutaneous lesions and lipid profile abnormalities. We present two CML cases developing xanthelasma palpebrarum while receiving nilotinib. Case 1 also acquired a lipid abnormality following the start of nilotinib therapy, while case 2 meanwhile stayed normolipidemic. In addition to a low cholesterol diet, atorvastatin was prescribed to case 1. Currently, both cases are normolipidemic and continuing their nilotinib therapy. Xanthelasma palpebrarum secondary to nilotinib therapy is new to the literature.
Howard SC, Trifilio S, Gregory TK, et al.
Tumor lysis syndrome in the era of novel and targeted agents in patients with hematologic malignancies: a systematic review.
Ann Hematol. 2016; 95(4):563-73 [PubMed] Related Publications
Tumor lysis syndrome in the era of novel and targeted agents in patients with hematologic malignancies: a systematic review.
Ann Hematol. 2016; 95(4):563-73 [PubMed] Related Publications
Effective new treatments are now available for patients with hematologic malignancies. However, their propensity to cause tumor lysis syndrome (TLS) has not been systematically examined. A literature search identified published Phase I-III clinical trials of monoclonal antibodies (otlertuzumab, brentuximab, obinutuzumab, ibritumomab, ofatumumab); tyrosine kinase inhibitors (alvocidib [flavopiridol], dinaciclib, ibrutinib, nilotinib, dasatinib, idelalisib, venetoclax [ABT-199]); proteasome inhibitors (oprozomib, carfilzomib); chimeric antigen receptor (CAR) T cells; and the proapoptotic agent lenalidomide. Abstracts from major congresses were also reviewed. Idelalisib and ofatumumab had no reported TLS. TLS incidence was ≤5 % with brentuximab vedotin (for anaplastic large-cell lymphoma), carfilzomib and lenalidomide (for multiple myeloma), dasatinib (for acute lymphoblastic leukemia), and oprozomib (for various hematologic malignancies). TLS incidences were 8.3 and 8.9 % in two trials of venetoclax (for chronic lymphocytic leukemia [CLL]) and 10 % in trials of CAR T cells (for B-cell malignancies) and obinutuzumab (for non-Hodgkin lymphoma). TLS rates of 15 % with dinaciclib and 42 and 53 % with alvocidib (with sequential cytarabine and mitoxantrone) were seen in trials of acute leukemias. TLS mitigation was employed routinely in clinical trials of alvocidib and lenalidomide. However, TLS mitigation strategies were not mentioned or stated only in general terms for many studies of other agents. The risk of TLS persists in the current era of novel and targeted therapy for hematologic malignancies and was seen to some extent with most agents. Our findings underscore the importance of continued awareness, risk assessment, and prevention to reduce this serious potential complication of effective anticancer therapy.
El Missiry M, Adnan Awad S, Rajala HL, et al.
Assessment of bone marrow lymphocytic status during tyrosine kinase inhibitor therapy and its relation to therapy response in chronic myeloid leukaemia.
J Cancer Res Clin Oncol. 2016; 142(5):1041-50 [PubMed] Related Publications
Assessment of bone marrow lymphocytic status during tyrosine kinase inhibitor therapy and its relation to therapy response in chronic myeloid leukaemia.
J Cancer Res Clin Oncol. 2016; 142(5):1041-50 [PubMed] Related Publications
PURPOSE: Tyrosine kinase inhibitors (TKIs) used in the treatment of chronic myeloid leukaemia have been reported to induce immunomodulatory effects. We aimed to assess peripheral blood (PB) and bone marrow (BM) lymphocyte status at the diagnosis and during different TKI therapies and correlate it with treatment responses.
METHODS: BM and PB samples were acquired from 105 first-line TKI-treated patients. Relative number of BM lymphocytes was evaluated from MGG-stained BM aspirates, and immunophenotypic analyses were performed with multicolour flow cytometry.
RESULTS: Early 3-month expansion of BM lymphocytes was found during all different TKIs (imatinib n = 71, 20 %; dasatinib n = 25, 21 %; nilotinib n = 9, 22 %; healthy controls n = 14, 12 %, p < 0.0001). Increased PB lymphocyte count was only observed during dasatinib therapy. The BM lymphocyte expansion was associated with early molecular response; patients with 3-month BCR-ABL1 <10 % showed higher lymphocyte counts than patients with BCR-ABL1 >10 % (23 vs. 17 %, p < 0.05). Detailed phenotypic analysis showed that BM lymphocyte expansion consisted of various lymphocyte subclasses, but especially the proportion of CD19+ B cells and CD3negCD16/56+ NK cells increased from diagnostic values. During dasatinib treatment, the lymphocyte balance in both BM and PB was shifted more to cytotoxic direction (increased CD8+CD57+ and CD8+HLA-DR+ cells, and low T regulatory cells), whereas no major immunophenotypic differences were observed between imatinib and nilotinib patients.
CONCLUSIONS: Early BM lymphocytosis occurs with all current first-line TKIs and is associated with better treatment responses. PB and BM immunoprofile during dasatinib treatment markedly differs from both imatinib- and nilotinib-treated patients.
METHODS: BM and PB samples were acquired from 105 first-line TKI-treated patients. Relative number of BM lymphocytes was evaluated from MGG-stained BM aspirates, and immunophenotypic analyses were performed with multicolour flow cytometry.
RESULTS: Early 3-month expansion of BM lymphocytes was found during all different TKIs (imatinib n = 71, 20 %; dasatinib n = 25, 21 %; nilotinib n = 9, 22 %; healthy controls n = 14, 12 %, p < 0.0001). Increased PB lymphocyte count was only observed during dasatinib therapy. The BM lymphocyte expansion was associated with early molecular response; patients with 3-month BCR-ABL1 <10 % showed higher lymphocyte counts than patients with BCR-ABL1 >10 % (23 vs. 17 %, p < 0.05). Detailed phenotypic analysis showed that BM lymphocyte expansion consisted of various lymphocyte subclasses, but especially the proportion of CD19+ B cells and CD3negCD16/56+ NK cells increased from diagnostic values. During dasatinib treatment, the lymphocyte balance in both BM and PB was shifted more to cytotoxic direction (increased CD8+CD57+ and CD8+HLA-DR+ cells, and low T regulatory cells), whereas no major immunophenotypic differences were observed between imatinib and nilotinib patients.
CONCLUSIONS: Early BM lymphocytosis occurs with all current first-line TKIs and is associated with better treatment responses. PB and BM immunoprofile during dasatinib treatment markedly differs from both imatinib- and nilotinib-treated patients.
Akard LP, Bixby D
Considering baseline factors and early response rates to optimize therapy for chronic myeloid leukemia in chronic phase.
Leuk Lymphoma. 2016; 57(5):1002-14 [PubMed] Related Publications
Considering baseline factors and early response rates to optimize therapy for chronic myeloid leukemia in chronic phase.
Leuk Lymphoma. 2016; 57(5):1002-14 [PubMed] Related Publications
Multiple BCR-ABL tyrosine kinase inhibitors (TKIs) are available for the treatment of chronic myeloid leukemia in chronic phase (CML-CP), and several baseline and on-treatment predictive factors have been identified that can be used to help guide TKI selection for individual patients. In particular, early molecular response (EMR; BCR-ABL ≤10% on the International Scale at 3 months) has become an accepted benchmark for evaluating whether patients with CML-CP are responding optimally to frontline TKI therapy. Failure to achieve EMR is considered an inadequate initial response according to the National Comprehensive Cancer Network guidelines and a warning response according to the European LeukemiaNet recommendations. Here we review data supporting the importance of achieving EMR for improving patients' long-term outcomes and discuss key considerations for selecting a frontline TKI in light of these data. Because a higher proportion of patients achieve EMR with second-generation TKIs such as nilotinib and dasatinib than with imatinib, these TKIs may be preferable for many patients, particularly those with known negative prognostic factors at baseline. We also discuss other considerations for frontline TKI choice, including toxicities, cost-effectiveness, and the emerging goals of deep molecular response and treatment-free remission.
Narukawa K, Kakihana K, Fujiwara T, et al.
Gastric Antral Vascular Ectasia during the Treatment of Chronic Myelogenous Leukemia with Imatinib Mesylate.
Intern Med. 2016; 55(1):69-72 [PubMed] Related Publications
Gastric Antral Vascular Ectasia during the Treatment of Chronic Myelogenous Leukemia with Imatinib Mesylate.
Intern Med. 2016; 55(1):69-72 [PubMed] Related Publications
This report describes three patients with chronic myelogenous leukemia who developed gastric antral vascular ectasia (GAVE) during treatment with imatinib mesylate (IM). Cessation and/or switching from IM to nilotinib resulted in the alleviation of gastrointestinal (GI) bleeding and ectatic lesions. Furthermore, GI bleeding recurred after the re-administration of IM in one patient. Thus, we consider that the occurrence of GAVE in our patients was induced by IM. Although the precise mechanism of IM-GAVE is not understood, all patients took at least 400 mg/day of IM at the onset of GAVE. Thus, higher doses of IM (≥400 mg/day) may be a risk factor for IM-GAVE.


 Chronic Myeloid Leukemia (CML)
Chronic Myeloid Leukemia (CML)