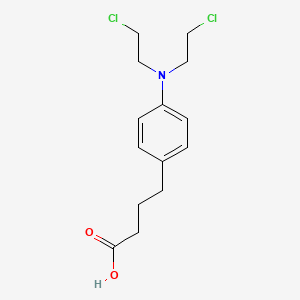
Chlorambucil
"A nitrogen mustard alkylating agent used as antineoplastic for chronic lymphocytic leukemia, Hodgkin's disease, and others. Although it is less toxic than most other nitrogen mustards, it has been listed as a known carcinogen in the Fourth Annual Report on Carcinogens (NTP 85-002, 1985). (Merck Index, 11th ed)" (MeSH 2013)
Found this page useful?
 Web Resources: Chlorambucil
Web Resources: Chlorambucil Latest Research Publications
Latest Research PublicationsWeb Resources: Chlorambucil (6 links)
Cancer Research UK
Macmillan Cancer Support
MedlinePlus
NHS Evidence
 Chlorambucil - Substance Summary
Chlorambucil - Substance Summary
PubChem
Irish Cancer Society
Latest Research Publications
This list of publications is regularly updated (Source: PubMed).
Fischer K, Al-Sawaf O, Bahlo J, et al.
Venetoclax and Obinutuzumab in Patients with CLL and Coexisting Conditions.
N Engl J Med. 2019; 380(23):2225-2236 [PubMed] Related Publications
Venetoclax and Obinutuzumab in Patients with CLL and Coexisting Conditions.
N Engl J Med. 2019; 380(23):2225-2236 [PubMed] Related Publications
BACKGROUND: The BCL2 inhibitor venetoclax has shown activity in patients with chronic lymphocytic leukemia (CLL), but its efficacy in combination with other agents in patients with CLL and coexisting conditions is not known.
METHODS: In this open-label, phase 3 trial, we investigated fixed-duration treatment with venetoclax and obinutuzumab in patients with previously untreated CLL and coexisting conditions. Patients with a score of greater than 6 on the Cumulative Illness Rating Scale (scores range from 0 to 56, with higher scores indicating more impaired function of organ systems) or a calculated creatinine clearance of less than 70 ml per minute were randomly assigned to receive venetoclax-obinutuzumab or chlorambucil-obinutuzumab. The primary end point was investigator-assessed progression-free survival. The safety of each regimen was also evaluated.
RESULTS: In total, 432 patients (median age, 72 years; median Cumulative Illness Rating Scale score, 8; median creatinine clearance, 66.4 ml per minute) underwent randomization, with 216 assigned to each group. After a median follow-up of 28.1 months, 30 primary end-point events (disease progression or death) had occurred in the venetoclax-obinutuzumab group and 77 had occurred in the chlorambucil-obinutuzumab group (hazard ratio, 0.35; 95% confidence interval [CI], 0.23 to 0.53; P<0.001). The Kaplan-Meier estimate of the percentage of patients with progression-free survival at 24 months was significantly higher in the venetoclax-obinutuzumab group than in the chlorambucil-obinutuzumab group: 88.2% (95% CI, 83.7 to 92.6) as compared with 64.1% (95% CI, 57.4 to 70.8). This benefit was also observed in patients with
CONCLUSIONS: Among patients with untreated CLL and coexisting conditions, venetoclax-obinutuzumab was associated with longer progression-free survival than chlorambucil-obinutuzumab. (Funded by F. Hoffmann-La Roche and AbbVie; ClinicalTrials.gov number, NCT02242942.).
METHODS: In this open-label, phase 3 trial, we investigated fixed-duration treatment with venetoclax and obinutuzumab in patients with previously untreated CLL and coexisting conditions. Patients with a score of greater than 6 on the Cumulative Illness Rating Scale (scores range from 0 to 56, with higher scores indicating more impaired function of organ systems) or a calculated creatinine clearance of less than 70 ml per minute were randomly assigned to receive venetoclax-obinutuzumab or chlorambucil-obinutuzumab. The primary end point was investigator-assessed progression-free survival. The safety of each regimen was also evaluated.
RESULTS: In total, 432 patients (median age, 72 years; median Cumulative Illness Rating Scale score, 8; median creatinine clearance, 66.4 ml per minute) underwent randomization, with 216 assigned to each group. After a median follow-up of 28.1 months, 30 primary end-point events (disease progression or death) had occurred in the venetoclax-obinutuzumab group and 77 had occurred in the chlorambucil-obinutuzumab group (hazard ratio, 0.35; 95% confidence interval [CI], 0.23 to 0.53; P<0.001). The Kaplan-Meier estimate of the percentage of patients with progression-free survival at 24 months was significantly higher in the venetoclax-obinutuzumab group than in the chlorambucil-obinutuzumab group: 88.2% (95% CI, 83.7 to 92.6) as compared with 64.1% (95% CI, 57.4 to 70.8). This benefit was also observed in patients with
CONCLUSIONS: Among patients with untreated CLL and coexisting conditions, venetoclax-obinutuzumab was associated with longer progression-free survival than chlorambucil-obinutuzumab. (Funded by F. Hoffmann-La Roche and AbbVie; ClinicalTrials.gov number, NCT02242942.).
Mendoza-Cardozo S, Pedro-Hernández LD, Organista-Mateos U, et al.
In vitro activity of resorcinarene-chlorambucil conjugates for therapy in human chronic myelogenous leukemia cells.
Drug Dev Ind Pharm. 2019; 45(4):683-688 [PubMed] Related Publications
In vitro activity of resorcinarene-chlorambucil conjugates for therapy in human chronic myelogenous leukemia cells.
Drug Dev Ind Pharm. 2019; 45(4):683-688 [PubMed] Related Publications
A possible way of improving the activity and selectivity profile of antitumor agents is to design drug carrier systems employing soluble macromolecules. Thus, four resorcinarene-PAMAM-dendrimer conjugates of chlorambucil with different groups in the lower part of the macrocycle and different length dendritic arms showed a good stability of the chemical link between drug and spacer. Evaluation of the cytotoxicity of the resorcinarene-PAMAM-dendrimer-chlorambucil conjugate employing a sulforhodamine B (SRB) assay in K-562 (human chronic myelogenous leukemia cells) demonstrated that the conjugate was more potent as an antiproliferative agent than chlorambucil.
Briani C, Visentin A, Salvalaggio A, et al.
Obinutuzumab, a new anti-CD20 antibody, and chlorambucil are active and effective in anti-myelin-associated glycoprotein antibody polyneuropathy.
Eur J Neurol. 2019; 26(2):371-375 [PubMed] Related Publications
Obinutuzumab, a new anti-CD20 antibody, and chlorambucil are active and effective in anti-myelin-associated glycoprotein antibody polyneuropathy.
Eur J Neurol. 2019; 26(2):371-375 [PubMed] Related Publications
BACKGROUND AND PURPOSE: Rituximab, a chimeric anti-CD20 monoclonal antibody, has been used in polyneuropathy associated with anti-myelin-associated glycoprotein (anti-MAG) antibody polyneuropathy with controversial results. Herein, two patients with anti-MAG antibody neuropathy and concurrent chronic lymphocytic leukemia (CLL) are reported, who dramatically responded to obinutuzumab, a novel glycoengineered humanized anti-CD20 monoclonal antibody.
METHODS: Patient 1 was an 82-year-old man with severe demyelinating sensory-motor neuropathy. He was wheelchair-bound, with loss of sensation up to the knees. He had a CLL, immunoglobulin M (IgM) lambda monoclonal gammopathy, with anti-MAG antibodies >70 000 Bühlmann titer units (BTU). Patient 2 was an 84-year-old woman with demyelinating neuropathy, paresthesias and gait instability. She had CLL and IgM kappa paraprotein with anti-MAG antibodies >70 000 BTU. Both patients were treated with obinutuzumab intravenously at 100 mg on day +1, 900 mg +2, then at 1000 mg on days 8 and 15 of cycle 1 and day 1 of cycles 2-6; chlorambucil was given orally at 0.5 mg/kg on days 1 and 15 of cycles 1-6.
RESULTS: Patient 1 at cycle 6 was able to stand, gait was possible with monolateral support, hypoesthesia and strength improved. M-protein and IgM level decreased. In patient 2, already after three cycles, the monoclonal component disappeared and there was dramatic improvement of symptoms and gait normalization. At the end of therapy anti-MAG antibody titer decreased to 5462 BTU. Neurophysiology also improved.
CONCLUSIONS: In our patients, obinutuzumab was effective as a first-line treatment of anti-MAG antibody polyneuropathy. CLL might have had a role in the response to therapy, but the associations might be considered in future trials.
METHODS: Patient 1 was an 82-year-old man with severe demyelinating sensory-motor neuropathy. He was wheelchair-bound, with loss of sensation up to the knees. He had a CLL, immunoglobulin M (IgM) lambda monoclonal gammopathy, with anti-MAG antibodies >70 000 Bühlmann titer units (BTU). Patient 2 was an 84-year-old woman with demyelinating neuropathy, paresthesias and gait instability. She had CLL and IgM kappa paraprotein with anti-MAG antibodies >70 000 BTU. Both patients were treated with obinutuzumab intravenously at 100 mg on day +1, 900 mg +2, then at 1000 mg on days 8 and 15 of cycle 1 and day 1 of cycles 2-6; chlorambucil was given orally at 0.5 mg/kg on days 1 and 15 of cycles 1-6.
RESULTS: Patient 1 at cycle 6 was able to stand, gait was possible with monolateral support, hypoesthesia and strength improved. M-protein and IgM level decreased. In patient 2, already after three cycles, the monoclonal component disappeared and there was dramatic improvement of symptoms and gait normalization. At the end of therapy anti-MAG antibody titer decreased to 5462 BTU. Neurophysiology also improved.
CONCLUSIONS: In our patients, obinutuzumab was effective as a first-line treatment of anti-MAG antibody polyneuropathy. CLL might have had a role in the response to therapy, but the associations might be considered in future trials.
Ma ZY, Wang DB, Song XQ, et al.
Chlorambucil-conjugated platinum(IV) prodrugs to treat triple-negative breast cancer in vitro and in vivo.
Eur J Med Chem. 2018; 157:1292-1299 [PubMed] Related Publications
Chlorambucil-conjugated platinum(IV) prodrugs to treat triple-negative breast cancer in vitro and in vivo.
Eur J Med Chem. 2018; 157:1292-1299 [PubMed] Related Publications
Modification of platinum (II) into lipophilic platinum (IV) compounds by introducing biologically active molecules were widely employed to develop new platinum-based prodrugs in the past decade. In this paper, two chlorambucil platinum (IV) complexes, CLB-Pt and CLB-Pt-CLB, were synthesized and displayed very potent antiproliferative activity against all the tested cancer cell lines, such as A549, HeLa and MCF-7, especially to treat the well-known refractory triple-negative breast cancer. CLB-Pt-CLB significantly improved cell-killing effect in triple-negative subtype MDA-MB-231 cells, and showed much stronger cytotoxicity than either monotherapy or combination of cisplatin and chlorambucil. CLB-Pt-CLB prodrug entered cells in dramatically increased amount compared with cisplatin and enhanced DNA damage, inducing cancer cell apoptosis. It exhibited high anticancer activity and no observable toxicity in BALB/c nude mice bearing MDA-MB-231 tumors. The chlorambucil moiety not only greatly assisted the passive diffusion of CLB-Pt-CLB into cells, but also produced the synergism with cisplatin in targeting DNA.
Reese MJ, Knapp DW, Anderson KM, et al.
In vitro effect of chlorambucil on human glioma cell lines (SF767 and U87-MG), and human microvascular endothelial cell (HMVEC) and endothelial progenitor cells (ECFCs), in the context of plasma chlorambucil concentrations in tumor-bearing dogs.
PLoS One. 2018; 13(9):e0203517 [PubMed] Free Access to Full Article Related Publications
In vitro effect of chlorambucil on human glioma cell lines (SF767 and U87-MG), and human microvascular endothelial cell (HMVEC) and endothelial progenitor cells (ECFCs), in the context of plasma chlorambucil concentrations in tumor-bearing dogs.
PLoS One. 2018; 13(9):e0203517 [PubMed] Free Access to Full Article Related Publications
The objective of this study was to investigate a possible mechanism of action of metronomic chlorambucil on glioma by studying the in vitro cytotoxicity and anti-angiogenic effects on glioma and endothelial cells, respectively. The in vitro LD50 and IC50 of chlorambucil were determined using human SF767 and U87-MG glioma cell lines, human microvascular endothelial cells (HMVECs) and human endothelial colony forming cells (ECFCs). Results were analyzed in the context of chlorambucil concentrations measured in the plasma of tumor-bearing dogs receiving 4 mg m-2 metronomic chlorambucil. The LD50 and IC50 of chlorambucil were 270 μM and 114 μM for SF767, and 390 μM and 96 μM for U87-MG, respectively. The IC50 of chlorambucil was 0.53 μM and 145 μM for the HMVECs and ECFCs, respectively. In pharmacokinetic studies, the mean plasma Cmax of chlorambucil was 0.06 μM. Results suggest that metronomic chlorambucil in dogs does not achieve plasma concentrations high enough to cause direct cytotoxic or growth inhibitory effects on either glioma or endothelial cells.
Sinha R, Redekop WK
Cost-Effectiveness of Ibrutinib Compared With Obinutuzumab With Chlorambucil in Untreated Chronic Lymphocytic Leukemia Patients With Comorbidities in the United Kingdom.
Clin Lymphoma Myeloma Leuk. 2018; 18(2):e131-e142 [PubMed] Related Publications
Cost-Effectiveness of Ibrutinib Compared With Obinutuzumab With Chlorambucil in Untreated Chronic Lymphocytic Leukemia Patients With Comorbidities in the United Kingdom.
Clin Lymphoma Myeloma Leuk. 2018; 18(2):e131-e142 [PubMed] Related Publications
BACKGROUND: Ibrutinib shows superiority over obinutuzumab with chlorambucil (G-Clb) in untreated patients with chronic lymphocytic leukemia with comorbidities who cannot tolerate fludarabine-based therapy. However, ibrutinib is relatively more expensive than G-Clb. In this study we evaluated the cost-effectiveness of ibrutinib compared with G-Clb from the United Kingdom (UK) health care perspective.
MATERIALS AND METHODS: A 3-state semi-Markov model was parameterized to estimate the lifetime costs and benefits associated with ibrutinib compared with G-Clb as first-line treatment. Idelalisib with rituximab was considered as second-line treatment. Unit costs were derived from standard sources, (dis)utilities from UK elicitation studies, progression-free survival, progression, and death from clinical trials, and postprogression survival and background mortality from published sources. Additional analyses included threshold analyses with ibrutinib and idelalisib at various discount rates, and scenario analysis with ibrutinib as second-line treatment after G-Clb.
RESULTS: An average gain of 1.49 quality-adjusted life-years (QALYs) was estimated for ibrutinib compared with G-Clb at an average additional cost of £112,835 per patient. To be cost-effective as per the UK thresholds, ibrutinib needs to be discounted at 30%, 40%, and 50% if idelalisib is discounted at 0%, 25%, and 50% respectively. The incremental cost-effectiveness ratio was £75,648 and £-143,279 per QALY gained for the base-case and scenario analyses, respectively. Sensitivity analyses showed the robustness of the results.
CONCLUSION: As per base-case analyses, an adequate discount on ibrutinib is required to make it cost-effective as per the UK thresholds. The scenario analysis substantiates ibrutinib's cost-savings for the UK National Health Services and advocates patient's access to ibrutinib in the UK.
MATERIALS AND METHODS: A 3-state semi-Markov model was parameterized to estimate the lifetime costs and benefits associated with ibrutinib compared with G-Clb as first-line treatment. Idelalisib with rituximab was considered as second-line treatment. Unit costs were derived from standard sources, (dis)utilities from UK elicitation studies, progression-free survival, progression, and death from clinical trials, and postprogression survival and background mortality from published sources. Additional analyses included threshold analyses with ibrutinib and idelalisib at various discount rates, and scenario analysis with ibrutinib as second-line treatment after G-Clb.
RESULTS: An average gain of 1.49 quality-adjusted life-years (QALYs) was estimated for ibrutinib compared with G-Clb at an average additional cost of £112,835 per patient. To be cost-effective as per the UK thresholds, ibrutinib needs to be discounted at 30%, 40%, and 50% if idelalisib is discounted at 0%, 25%, and 50% respectively. The incremental cost-effectiveness ratio was £75,648 and £-143,279 per QALY gained for the base-case and scenario analyses, respectively. Sensitivity analyses showed the robustness of the results.
CONCLUSION: As per base-case analyses, an adequate discount on ibrutinib is required to make it cost-effective as per the UK thresholds. The scenario analysis substantiates ibrutinib's cost-savings for the UK National Health Services and advocates patient's access to ibrutinib in the UK.
Tam C, Kuss B, Opat S, et al.
Management of patients with previously untreated chronic lymphocytic leukaemia with obinutuzumab and chlorambucil.
Intern Med J. 2017; 47 Suppl 4:5-10 [PubMed] Related Publications
Management of patients with previously untreated chronic lymphocytic leukaemia with obinutuzumab and chlorambucil.
Intern Med J. 2017; 47 Suppl 4:5-10 [PubMed] Related Publications
Patients with chronic lymphocytic leukaemia (CLL) are generally older, with many considered 'unfit' for fludarabine-cyclophosphamide-rituximab therapy. In these patients, the combination of obinutuzumab-chlorambucil may be an appropriate therapeutic choice. Obinutuzumab-chlorambucil has been demonstrated to improve overall survival rates compared to chlorambucil alone and to improve progression-free survival and overall response rates compared to rituximab-chlorambucil. This combination can lead to certain toxicities that need to be addressed through appropriate patient selection, pre-medication and management. In this paper, we discuss evidence-based and author-recommended practical management of first-line CLL patients receiving obinutuzumab-chlorambucil.
Van Sanden S, Baculea S, Diels J, Cote S
Comparative Efficacy of Ibrutinib Versus Obinutuzumab + Chlorambucil in First-Line Treatment of Chronic Lymphocytic Leukemia: A Matching-Adjusted Indirect Comparison.
Adv Ther. 2017; 34(7):1650-1661 [PubMed] Free Access to Full Article Related Publications
Comparative Efficacy of Ibrutinib Versus Obinutuzumab + Chlorambucil in First-Line Treatment of Chronic Lymphocytic Leukemia: A Matching-Adjusted Indirect Comparison.
Adv Ther. 2017; 34(7):1650-1661 [PubMed] Free Access to Full Article Related Publications
INTRODUCTION: Ibrutinib (ibr) monotherapy and the combination of obinutuzumab plus chlorambucil (obi) are approved for previously untreated chronic lymphocytic leukemia (CLL). No trials directly comparing their efficacy are available. Therefore a matching-adjusted indirect comparison (MAIC) was performed to provide insight into their relative efficacy in terms of progression-free survival (PFS) and overall survival (OS). MAIC attempts to adjust for between-trial differences in factors known or suspected to influence treatment effects, to minimize bias.
METHODS: A MAIC within a Bayesian framework was conducted using individual patient data from the RESONATE-2 study of ibr versus chlorambucil and published data from the CLL11 study of obi versus chlorambucil. Both studies were conducted in patients ineligible for full-dose fludarabine-based therapy. After matching, the reweighted adjusted relative efficacy measure of ibr versus chlorambucil from RESONATE-2 [hazard ratio (HR), 95% credible interval (CrI)] was compared with that of obi versus chlorambucil from CLL11 for each endpoint, using a Bayesian indirect comparison.
RESULTS: Our results suggest that in a population with similar average baseline characteristics to CLL11, ibr would improve PFS and OS outcomes compared to obi. Before matching, the HRs for ibr versus obi were 0.48 [CrI = 0.22-1.02, p(HR <1) = 97%], 0.85 [CrI = 0.44-1.63, p(HR <1) = 69%], and 0.40 [CrI = 0.10-1.54, p(HR <1) = 91%] for PFS by investigator assessment, PFS by independent review committee, and OS, respectively. After matching on all available characteristics the HRs decreased to 0.12 [CrI = 0.02-0.97, p(HR <1) = 98%], 0.24 [CrI = 0.04-1.35, p(HR <1) = 95%], and 0.21 [CrI = <0.01-8.89, p(HR <1) = 79%], respectively. There was a large variance around the treatment effect for OS due to the low number of deaths.
CONCLUSION: Our analysis suggests that ibrutinib is highly likely to provide greater PFS benefit than obinutuzumab plus chlorambucil in older or less fit patients with previously untreated CLL. There is also an indication of improvement in OS, albeit with a higher uncertainty due to the low number of events.
FUNDING: Janssen-Cilag Ltd.
METHODS: A MAIC within a Bayesian framework was conducted using individual patient data from the RESONATE-2 study of ibr versus chlorambucil and published data from the CLL11 study of obi versus chlorambucil. Both studies were conducted in patients ineligible for full-dose fludarabine-based therapy. After matching, the reweighted adjusted relative efficacy measure of ibr versus chlorambucil from RESONATE-2 [hazard ratio (HR), 95% credible interval (CrI)] was compared with that of obi versus chlorambucil from CLL11 for each endpoint, using a Bayesian indirect comparison.
RESULTS: Our results suggest that in a population with similar average baseline characteristics to CLL11, ibr would improve PFS and OS outcomes compared to obi. Before matching, the HRs for ibr versus obi were 0.48 [CrI = 0.22-1.02, p(HR <1) = 97%], 0.85 [CrI = 0.44-1.63, p(HR <1) = 69%], and 0.40 [CrI = 0.10-1.54, p(HR <1) = 91%] for PFS by investigator assessment, PFS by independent review committee, and OS, respectively. After matching on all available characteristics the HRs decreased to 0.12 [CrI = 0.02-0.97, p(HR <1) = 98%], 0.24 [CrI = 0.04-1.35, p(HR <1) = 95%], and 0.21 [CrI = <0.01-8.89, p(HR <1) = 79%], respectively. There was a large variance around the treatment effect for OS due to the low number of deaths.
CONCLUSION: Our analysis suggests that ibrutinib is highly likely to provide greater PFS benefit than obinutuzumab plus chlorambucil in older or less fit patients with previously untreated CLL. There is also an indication of improvement in OS, albeit with a higher uncertainty due to the low number of events.
FUNDING: Janssen-Cilag Ltd.
Zhang Q, Zhang L, Li Z, et al.
Inducing Controlled Release and Increased Tumor-Targeted Delivery of Chlorambucil via Albumin/Liposome Hybrid Nanoparticles.
AAPS PharmSciTech. 2017; 18(8):2977-2986 [PubMed] Related Publications
Inducing Controlled Release and Increased Tumor-Targeted Delivery of Chlorambucil via Albumin/Liposome Hybrid Nanoparticles.
AAPS PharmSciTech. 2017; 18(8):2977-2986 [PubMed] Related Publications
Liposomes possess good biocompatibility and excellent tumor-targeting capacity. However, the rapid premature release of lipophilic drugs from the lipid bilayer of liposomes has negative effect on the tumor-targeted drug delivery of liposomes. In this study, a lipophilic antitumor drug-chlorambucil (CHL)-was encapsulated into the aqueous interior of liposomes with the aid of albumin to obtain the CHL-loaded liposomes/albumin hybrid nanoparticles (CHL-Hybrids). The in vitro accumulative release rate of CHL from CHL-Hybrids was less than 50% within 48 h, while the accumulative CHL release was more than 80% for CHL-loaded liposomes (CHL-Lip). After intravenous injection into rats, the half-life (t
Zucca E, Conconi A, Martinelli G, et al.
Final Results of the IELSG-19 Randomized Trial of Mucosa-Associated Lymphoid Tissue Lymphoma: Improved Event-Free and Progression-Free Survival With Rituximab Plus Chlorambucil Versus Either Chlorambucil or Rituximab Monotherapy.
J Clin Oncol. 2017; 35(17):1905-1912 [PubMed] Related Publications
Final Results of the IELSG-19 Randomized Trial of Mucosa-Associated Lymphoid Tissue Lymphoma: Improved Event-Free and Progression-Free Survival With Rituximab Plus Chlorambucil Versus Either Chlorambucil or Rituximab Monotherapy.
J Clin Oncol. 2017; 35(17):1905-1912 [PubMed] Related Publications
Purpose There is no consensus on the optimal systemic treatment of patients with extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue. The IELSG-19 phase III study, to our knowledge, was the first such study to address the question of first-line treatment in a randomized trial. Patients and Methods Eligible patients were initially randomly assigned (1:1 ratio) to receive either chlorambucil monotherapy (6 mg/m
Kaur J, Tsvetkova Y, Arroub K, et al.
Synthesis, characterization, and relaxation studies of Gd-DO3A conjugate of chlorambucil as a potential theranostic agent.
Chem Biol Drug Des. 2017; 89(2):269-276 [PubMed] Related Publications
Synthesis, characterization, and relaxation studies of Gd-DO3A conjugate of chlorambucil as a potential theranostic agent.
Chem Biol Drug Des. 2017; 89(2):269-276 [PubMed] Related Publications
DO3A-based macrocycles serve as attractive templates from which clinically useful theranostic agents can be obtained after coupling with molecular targeted therapeutic drugs. In this study, we describe the chemical synthesis, relaxation, and cytotoxicity studies of a new DO3A conjugate of chlorambucil (CHL) as a magnetic resonance imaging (MRI) theranostic agent. A convenient route of synthesis is reported, which allowed conjugation of the macrocyclic ligand (DO3A) to the chemotherapeutic drug (CHL) via tyrosine for the preparation of an attractive chelate-drug ensemble (DO3A-TR-CHL). The structures of all intermediates and final compound have been determined by
Hillmen P, Janssens A, Babu KG, et al.
Health-related quality of life and patient-reported outcomes of ofatumumab plus chlorambucil versus chlorambucil monotherapy in the COMPLEMENT 1 trial of patients with previously untreated CLL.
Acta Oncol. 2016 Sep - Oct; 55(9-10):1115-1120 [PubMed] Related Publications
Health-related quality of life and patient-reported outcomes of ofatumumab plus chlorambucil versus chlorambucil monotherapy in the COMPLEMENT 1 trial of patients with previously untreated CLL.
Acta Oncol. 2016 Sep - Oct; 55(9-10):1115-1120 [PubMed] Related Publications
BACKGROUND: Patients diagnosed with chronic lymphocytic leukemia (CLL) are usually elderly and frequently have a number of comorbidities. Health-related quality of life (HRQoL) for these patients is of utmost importance and should be taken into consideration when assessing new treatment options. The combination of ofatumumab with chlorambucil has shown longer progression-free survival compared with chlorambucil alone. In this study, we aim to assess how this treatment combination affects patients' health-related quality of life and patient-reported symptoms.
MATERIAL AND METHODS: In this open-label phase III trial, patients with previously untreated CLL for whom fludarabine-based treatment was contra-indicated, were randomized 1:1 to receive oral chlorambucil (10 mg/m
RESULTS: Patient-reported improvements from baseline in Global Health Status (GHS)/HRQoL scores and fatigue scores were recorded during treatment with both chlorambucil monotherapy and ofatumumab in combination with chlorambucil. There were no significant differences between the two treatment arms for GHS/HRQoL (p = 0.667) or fatigue (p = 0.103). Following treatment, numerical improvements to GHS/HRQoL and fatigue scores were reported, with no significant differences between the two treatment arms.
CONCLUSION: Small but detectable improvements in patients' quality of life were reported as a result of treatment. The addition of ofatumumab to chlorambucil did not negatively impact HRQoL. Quality of life was maintained in the months following treatment.
MATERIAL AND METHODS: In this open-label phase III trial, patients with previously untreated CLL for whom fludarabine-based treatment was contra-indicated, were randomized 1:1 to receive oral chlorambucil (10 mg/m
RESULTS: Patient-reported improvements from baseline in Global Health Status (GHS)/HRQoL scores and fatigue scores were recorded during treatment with both chlorambucil monotherapy and ofatumumab in combination with chlorambucil. There were no significant differences between the two treatment arms for GHS/HRQoL (p = 0.667) or fatigue (p = 0.103). Following treatment, numerical improvements to GHS/HRQoL and fatigue scores were reported, with no significant differences between the two treatment arms.
CONCLUSION: Small but detectable improvements in patients' quality of life were reported as a result of treatment. The addition of ofatumumab to chlorambucil did not negatively impact HRQoL. Quality of life was maintained in the months following treatment.
Becker U, Briggs AH, Moreno SG, et al.
Cost-Effectiveness Model for Chemoimmunotherapy Options in Patients with Previously Untreated Chronic Lymphocytic Leukemia Unsuitable for Full-Dose Fludarabine-Based Therapy.
Value Health. 2016; 19(4):374-82 [PubMed] Related Publications
Cost-Effectiveness Model for Chemoimmunotherapy Options in Patients with Previously Untreated Chronic Lymphocytic Leukemia Unsuitable for Full-Dose Fludarabine-Based Therapy.
Value Health. 2016; 19(4):374-82 [PubMed] Related Publications
OBJECTIVES: To evaluate the cost-effectiveness of treatment with anti-CD20 monoclonal antibody obinutuzumab plus chlorambucil (GClb) in untreated patients with chronic lymphocytic leukemia unsuitable for full-dose fludarabine-based therapy.
METHODS: A Markov model was used to assess the cost-effectiveness of GClb versus other chemoimmunotherapy options. The model comprised three mutually exclusive health states: "progression-free survival (with/without therapy)", "progression (refractory/relapsed lines)", and "death". Each state was assigned a health utility value representing patients' quality of life and a specific cost value. Comparisons between GClb and rituximab plus chlorambucil or only chlorambucil were performed using patient-level clinical trial data; other comparisons were performed via a network meta-analysis using information gathered in a systematic literature review. To support the model, a utility elicitation study was conducted from the perspective of the UK National Health Service.
RESULTS: There was good agreement between the model-predicted progression-free and overall survival and that from the CLL11 trial. On incorporating data from the indirect treatment comparisons, it was found that GClb was cost-effective with a range of incremental cost-effectiveness ratios below a threshold of £30,000 per quality-adjusted life-year gained, and remained so during deterministic and probabilistic sensitivity analyses under various scenarios.
CONCLUSIONS: GClb was estimated to increase both quality-adjusted life expectancy and treatment costs compared with several commonly used therapies, with incremental cost-effectiveness ratios below commonly referenced UK thresholds. This article offers a real example of how to combine direct and indirect evidence in a cost-effectiveness analysis of oncology drugs.
METHODS: A Markov model was used to assess the cost-effectiveness of GClb versus other chemoimmunotherapy options. The model comprised three mutually exclusive health states: "progression-free survival (with/without therapy)", "progression (refractory/relapsed lines)", and "death". Each state was assigned a health utility value representing patients' quality of life and a specific cost value. Comparisons between GClb and rituximab plus chlorambucil or only chlorambucil were performed using patient-level clinical trial data; other comparisons were performed via a network meta-analysis using information gathered in a systematic literature review. To support the model, a utility elicitation study was conducted from the perspective of the UK National Health Service.
RESULTS: There was good agreement between the model-predicted progression-free and overall survival and that from the CLL11 trial. On incorporating data from the indirect treatment comparisons, it was found that GClb was cost-effective with a range of incremental cost-effectiveness ratios below a threshold of £30,000 per quality-adjusted life-year gained, and remained so during deterministic and probabilistic sensitivity analyses under various scenarios.
CONCLUSIONS: GClb was estimated to increase both quality-adjusted life expectancy and treatment costs compared with several commonly used therapies, with incremental cost-effectiveness ratios below commonly referenced UK thresholds. This article offers a real example of how to combine direct and indirect evidence in a cost-effectiveness analysis of oncology drugs.
Herling CD, Klaumünzer M, Rocha CK, et al.
Complex karyotypes and KRAS and POT1 mutations impact outcome in CLL after chlorambucil-based chemotherapy or chemoimmunotherapy.
Blood. 2016; 128(3):395-404 [PubMed] Related Publications
Complex karyotypes and KRAS and POT1 mutations impact outcome in CLL after chlorambucil-based chemotherapy or chemoimmunotherapy.
Blood. 2016; 128(3):395-404 [PubMed] Related Publications
Genetic instability is a feature of chronic lymphocytic leukemia (CLL) with adverse prognosis. We hypothesized that chromosomal translocations or complex karyotypes and distinct somatic mutations may impact outcome after first-line chemoimmunotherapy of CLL patients. We performed metaphase karyotyping and next-generation sequencing (NGS) of 85 genes in pretreatment blood samples obtained from 161 patients registered for CLL11, a 3-arm phase 3 trial comparing frontline chlorambucil (Clb) vs Clb plus rituximab (Clb-R) or Clb plus obinutuzumab in CLL patients with significant comorbidity. Chromosomal aberrations as assessed by karyotyping were observed in 68.8% of 154 patients, 31.2% carried translocations, and 19.5% showed complex karyotypes. NGS revealed 198 missense/nonsense mutations and 76 small indels in 76.4% of patients. The most frequently mutated genes were NOTCH1, SF3B1, ATM, TP53, BIRC3, POT1, XPO1, and KRAS Sole chemotherapy, treatment with Clb-R, or genetic lesions in TP53 (9.9% of patients) and KRAS (6.2% of patients) were significantly associated with nonresponse to study therapy. In multivariate models, complex karyotypes and POT1 mutations (8.1% of patients) represented significant prognostic factors for an unfavorable survival, independently of IGHV mutation status, Binet stage, and serum β-2-microglobuline. Patients with the copresence of complex karyotypes and deletions/mutations involving TP53 demonstrated a particularly short survival. In summary, this is the first prospective, controlled study in CLL patients that shows a role of complex karyotype aberrations as an independent prognostic factor for survival after front-line therapy. Moreover, the study identifies mutations in KRAS and POT1 as novel determinants of outcome after chemoimmunotherapy using chlorambucil and anti-CD20 treatment.
Stíbal D, Therrien B, Süss-Fink G, et al.
Chlorambucil conjugates of dinuclear p-cymene ruthenium trithiolato complexes: synthesis, characterization and cytotoxicity study in vitro and in vivo.
J Biol Inorg Chem. 2016; 21(4):443-52 [PubMed] Related Publications
Chlorambucil conjugates of dinuclear p-cymene ruthenium trithiolato complexes: synthesis, characterization and cytotoxicity study in vitro and in vivo.
J Biol Inorg Chem. 2016; 21(4):443-52 [PubMed] Related Publications
Four diruthenium trithiolato chlorambucil conjugates have been prepared via Steglich esterification from chlorambucil and the corresponding trithiolato precursors. All conjugates are highly cytotoxic towards human ovarian A2780 and A2780cisR cancer cell lines with IC50 values in the nanomolar range. The conjugates exhibit selectivity towards A2780 cells as compared to non-cancerous HEK293 cells, while being only slightly selective for RF24 and A2780cisR cells. In vivo, the conjugate [10]BF4 suppressed the growth of a solid Ehrlich tumor in immunocompetent NMRI mice but did not prolong their overall survival. The reactivity of the chlorambucil conjugates with glutathione, a potential target of the dinuclear ruthenium motive, and with the 2-deoxyguanosine 5'-monophosphate (dGMP-a model target of chlorambucil) was studied by mass spectrometry and NMR spectroscopy. The conjugates did not show catalytic activity for the oxidation of glutathione nor binding to nucleotides, indicating that glutathione oxidation and DNA alkylation are not key mechanisms of action. Four highly cytotoxic diruthenium trithiolato chlorambucil conjugates have been prepared. All conjugates exhibit selectivity towards A2780 cells as compared to HEK293 cells, while being only slightly active in RF24 and A2780cisR cells. In vivo, the best candidate suppressed the growth of a solid Ehrlich tumor in immunocompetent NMRI mice but did not prolong their overall survival.
Vidal L, Gurion R, Ram R, et al.
Chlorambucil for the treatment of patients with chronic lymphocytic leukemia (CLL) - a systematic review and meta-analysis of randomized trials.
Leuk Lymphoma. 2016; 57(9):2047-57 [PubMed] Related Publications
Chlorambucil for the treatment of patients with chronic lymphocytic leukemia (CLL) - a systematic review and meta-analysis of randomized trials.
Leuk Lymphoma. 2016; 57(9):2047-57 [PubMed] Related Publications
Randomized clinical trials that compared chlorambucil to different regimens, for patients with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) do not support an overall survival (OS) benefit. To assess the efficacy and safety of chlorambucil as frontline treatment, we conducted a systematic review and meta-analysis of randomized controlled trials. OS was the primary outcome. Meta-analysis of 18 trials that compared purine analogs, alkylators, alemtuzumab and ibrutinib to chlorambucil demonstrated no OS benefit for therapy without chlorambucil over chlorambucil (pooled HR 0.99, 95% CI 0.91-1.08; 4133 patients). PFS was longer with purine analogs compared with chlorambucil with an increased risk of infection. The risk of secondary malignancies was not increased with chlorambucil. In conclusion, our study showed that chlorambucil is an acceptable chemotherapy backbone for unfit patients with CLL. Purine analogs should be preferred in fit younger patients because of longer PFS. Future trials should focus on unfit patients who are underrepresented in clinical trials.
Ho SH, Ali A, Chin TM, Go ML
Dioxonaphthoimidazoliums AB1 and YM155 disrupt phosphorylation of p50 in the NF-κB pathway.
Oncotarget. 2016; 7(10):11625-36 [PubMed] Free Access to Full Article Related Publications
Dioxonaphthoimidazoliums AB1 and YM155 disrupt phosphorylation of p50 in the NF-κB pathway.
Oncotarget. 2016; 7(10):11625-36 [PubMed] Free Access to Full Article Related Publications
The NF-κB pathway is overexpressed in non-small cell lung cancers (NSCLC) and contributes to the poor prognosis and high mortality characterizing this malignancy. Silencing the p50 and p65 NF-κB subunits in the NSCLC H1299 cell line led to profound loss in cell viability and downregulated anti-apoptotic proteins survivin and Mcl1. We also showed that a survivin suppressant, the dioxonaphthoimidazolium YM155, and its structural analog AB1 arrested the growth of H1299 cells at nanomolar concentrations. Both compounds were apoptogenic and suppressed survivin and other anti-apoptotic proteins (Mcl1, Bcl-2, Bcl-xl) in a dose- and/or time-dependent manner. YM155 and AB1 did not affect the expression of key proteins (IκBα, p65, p50) involved in NF-κB signaling. Stable IκBα levels suggest that the NF-κB/IκB complex and proteins upstream of IκBα, were not targeted. Neither did the compounds intercept the nuclear translocation of the p50 and p65 subunits. On the other hand, YM155 and AB1 suppressed the phosphorylation of the p50 subunit at Ser337 which is critical in promoting the binding of NF-κB dimers to DNA. Both compounds duly impeded the binding of NF-κB dimers to DNA and attenuated transcriptional activity of luciferase-transfected HEK293 cells controlled by NF-κB response elements. We propose that the "silencing" the NF-κB pathway effected by these compounds contributed to their potent apoptogenic effects on H1299. Notwithstanding, the mechanism(s) involved in their ability to abolish phosphorylation of p50 remains to be elucidated. Taken together, these results disclose a novel facet of functionalized dioxonaphthoimidazoliums that could account for their potent cell killing property.
Clark E, Boffa M, Magri C, Muscat V
Chlorambucil-Induced Radiation Recall Dermatitis.
Skinmed. 2015 Jul-Aug; 13(4):317-9 [PubMed] Related Publications
Chlorambucil-Induced Radiation Recall Dermatitis.
Skinmed. 2015 Jul-Aug; 13(4):317-9 [PubMed] Related Publications
A 65-year-old woman was diagnosed with low-grade non-Hodgkin lymphoma (Figure 1). She was treated with six cycles of cyclophosphamide, hydroxydaunorubicin, oncovin (vincristine), and prednisolone (CHOP) and three cycles of fludarabine and mitoxantrone. Ten months later she received radiotherapy to the left groin (total dose of 50 Gy in 25 fractions over 5 weeks) without complications.
Burger JA, Tedeschi A, Barr PM, et al.
Ibrutinib as Initial Therapy for Patients with Chronic Lymphocytic Leukemia.
N Engl J Med. 2015; 373(25):2425-37 [PubMed] Free Access to Full Article Related Publications
Ibrutinib as Initial Therapy for Patients with Chronic Lymphocytic Leukemia.
N Engl J Med. 2015; 373(25):2425-37 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Chronic lymphocytic leukemia (CLL) primarily affects older persons who often have coexisting conditions in addition to disease-related immunosuppression and myelosuppression. We conducted an international, open-label, randomized phase 3 trial to compare two oral agents, ibrutinib and chlorambucil, in previously untreated older patients with CLL or small lymphocytic lymphoma.
METHODS: We randomly assigned 269 previously untreated patients who were 65 years of age or older and had CLL or small lymphocytic lymphoma to receive ibrutinib or chlorambucil. The primary end point was progression-free survival as assessed by an independent review committee.
RESULTS: The median age of the patients was 73 years. During a median follow-up period of 18.4 months, ibrutinib resulted in significantly longer progression-free survival than did chlorambucil (median, not reached vs. 18.9 months), with a risk of progression or death that was 84% lower with ibrutinib than that with chlorambucil (hazard ratio, 0.16; P<0.001). Ibrutinib significantly prolonged overall survival; the estimated survival rate at 24 months was 98% with ibrutinib versus 85% with chlorambucil, with a relative risk of death that was 84% lower in the ibrutinib group than in the chlorambucil group (hazard ratio, 0.16; P=0.001). The overall response rate was higher with ibrutinib than with chlorambucil (86% vs. 35%, P<0.001). The rates of sustained increases from baseline values in the hemoglobin and platelet levels were higher with ibrutinib. Adverse events of any grade that occurred in at least 20% of the patients receiving ibrutinib included diarrhea, fatigue, cough, and nausea; adverse events occurring in at least 20% of those receiving chlorambucil included nausea, fatigue, neutropenia, anemia, and vomiting. In the ibrutinib group, four patients had a grade 3 hemorrhage and one had a grade 4 hemorrhage. A total of 87% of the patients in the ibrutinib group are continuing to take ibrutinib.
CONCLUSIONS: Ibrutinib was superior to chlorambucil in previously untreated patients with CLL or small lymphocytic lymphoma, as assessed by progression-free survival, overall survival, response rate, and improvement in hematologic variables. (Funded by Pharmacyclics and others; RESONATE-2 ClinicalTrials.gov number, NCT01722487.).
METHODS: We randomly assigned 269 previously untreated patients who were 65 years of age or older and had CLL or small lymphocytic lymphoma to receive ibrutinib or chlorambucil. The primary end point was progression-free survival as assessed by an independent review committee.
RESULTS: The median age of the patients was 73 years. During a median follow-up period of 18.4 months, ibrutinib resulted in significantly longer progression-free survival than did chlorambucil (median, not reached vs. 18.9 months), with a risk of progression or death that was 84% lower with ibrutinib than that with chlorambucil (hazard ratio, 0.16; P<0.001). Ibrutinib significantly prolonged overall survival; the estimated survival rate at 24 months was 98% with ibrutinib versus 85% with chlorambucil, with a relative risk of death that was 84% lower in the ibrutinib group than in the chlorambucil group (hazard ratio, 0.16; P=0.001). The overall response rate was higher with ibrutinib than with chlorambucil (86% vs. 35%, P<0.001). The rates of sustained increases from baseline values in the hemoglobin and platelet levels were higher with ibrutinib. Adverse events of any grade that occurred in at least 20% of the patients receiving ibrutinib included diarrhea, fatigue, cough, and nausea; adverse events occurring in at least 20% of those receiving chlorambucil included nausea, fatigue, neutropenia, anemia, and vomiting. In the ibrutinib group, four patients had a grade 3 hemorrhage and one had a grade 4 hemorrhage. A total of 87% of the patients in the ibrutinib group are continuing to take ibrutinib.
CONCLUSIONS: Ibrutinib was superior to chlorambucil in previously untreated patients with CLL or small lymphocytic lymphoma, as assessed by progression-free survival, overall survival, response rate, and improvement in hematologic variables. (Funded by Pharmacyclics and others; RESONATE-2 ClinicalTrials.gov number, NCT01722487.).
Herring W, Pearson I, Purser M, et al.
Cost Effectiveness of Ofatumumab Plus Chlorambucil in First-Line Chronic Lymphocytic Leukaemia in Canada.
Pharmacoeconomics. 2016; 34(1):77-90 [PubMed] Related Publications
Cost Effectiveness of Ofatumumab Plus Chlorambucil in First-Line Chronic Lymphocytic Leukaemia in Canada.
Pharmacoeconomics. 2016; 34(1):77-90 [PubMed] Related Publications
OBJECTIVE: Our objective was to estimate the cost effectiveness of ofatumumab plus chlorambucil (OChl) versus chlorambucil in patients with chronic lymphocytic leukaemia for whom fludarabine-based therapies are considered inappropriate from the perspective of the publicly funded healthcare system in Canada.
METHODS: A semi-Markov model (3-month cycle length) used survival curves to govern progression-free survival (PFS) and overall survival (OS). Efficacy and safety data and health-state utility values were estimated from the COMPLEMENT-1 trial. Post-progression treatment patterns were based on clinical guidelines, Canadian treatment practices and published literature. Total and incremental expected lifetime costs (in Canadian dollars [$Can], year 2013 values), life-years and quality-adjusted life-years (QALYs) were computed. Uncertainty was assessed via deterministic and probabilistic sensitivity analyses.
RESULTS: The discounted lifetime health and economic outcomes estimated by the model showed that, compared with chlorambucil, first-line treatment with OChl led to an increase in QALYs (0.41) and total costs ($Can27,866) and to an incremental cost-effectiveness ratio (ICER) of $Can68,647 per QALY gained. In deterministic sensitivity analyses, the ICER was most sensitive to the modelling time horizon and to the extrapolation of OS treatment effects beyond the trial duration. In probabilistic sensitivity analysis, the probability of cost effectiveness at a willingness-to-pay threshold of $Can100,000 per QALY gained was 59 %.
CONCLUSIONS: Base-case results indicated that improved overall response and PFS for OChl compared with chlorambucil translated to improved quality-adjusted life expectancy. Sensitivity analysis suggested that OChl is likely to be cost effective subject to uncertainty associated with the presence of any long-term OS benefit and the model time horizon.
METHODS: A semi-Markov model (3-month cycle length) used survival curves to govern progression-free survival (PFS) and overall survival (OS). Efficacy and safety data and health-state utility values were estimated from the COMPLEMENT-1 trial. Post-progression treatment patterns were based on clinical guidelines, Canadian treatment practices and published literature. Total and incremental expected lifetime costs (in Canadian dollars [$Can], year 2013 values), life-years and quality-adjusted life-years (QALYs) were computed. Uncertainty was assessed via deterministic and probabilistic sensitivity analyses.
RESULTS: The discounted lifetime health and economic outcomes estimated by the model showed that, compared with chlorambucil, first-line treatment with OChl led to an increase in QALYs (0.41) and total costs ($Can27,866) and to an incremental cost-effectiveness ratio (ICER) of $Can68,647 per QALY gained. In deterministic sensitivity analyses, the ICER was most sensitive to the modelling time horizon and to the extrapolation of OS treatment effects beyond the trial duration. In probabilistic sensitivity analysis, the probability of cost effectiveness at a willingness-to-pay threshold of $Can100,000 per QALY gained was 59 %.
CONCLUSIONS: Base-case results indicated that improved overall response and PFS for OChl compared with chlorambucil translated to improved quality-adjusted life expectancy. Sensitivity analysis suggested that OChl is likely to be cost effective subject to uncertainty associated with the presence of any long-term OS benefit and the model time horizon.
Fan M, Liang X, Li Z, et al.
Chlorambucil gemcitabine conjugate nanomedicine for cancer therapy.
Eur J Pharm Sci. 2015; 79:20-6 [PubMed] Related Publications
Chlorambucil gemcitabine conjugate nanomedicine for cancer therapy.
Eur J Pharm Sci. 2015; 79:20-6 [PubMed] Related Publications
Self-assembly of anticancer small molecules into nanostructures may represent an attractive approach to improve the treatment of experimental solid tumors. As a proof of concept, we designed and synthesized the conjugate prodrug of hydrophilic gemcitabine by its covalent coupling to hydrophobic chlorambucil via a hydrolyzable ester linkage. The resulting amphiphilic conjugates self-assembled into nanoparticles in water and exhibited significant anticancer activity in vitro against a variety of human cancer cells. In vivo anticancer activity of these nanoparticles has been tested on subcutaneous grafted SMMC-7721 hepatocellular carcinoma model. Such chlorambucil gemcitabine conjugate nanomedicine should have potential applications in cancer therapy.
Lepretre S, Dartigeas C, Feugier P, et al.
Systematic review of the recent evidence for the efficacy and safety of chlorambucil in the treatment of B-cell malignancies.
Leuk Lymphoma. 2016; 57(4):852-65 [PubMed] Related Publications
Systematic review of the recent evidence for the efficacy and safety of chlorambucil in the treatment of B-cell malignancies.
Leuk Lymphoma. 2016; 57(4):852-65 [PubMed] Related Publications
Emergence of new agents has deeply modified treatment options and the role of chlorambucil (CLB) in B-cell malignancies. We conducted a systematic review of prospective, randomized, controlled trials (RCTs) investigating the benefits and harms of CLB used alone or in combination with other treatment in patients suffering from chronic lymphocytic leukemia (CLL), low-grade non-Hodgkin lymphoma (NHL) or Waldenström macroglobulinemia (WM). For CLL, review of the nine RCTs showed that the main advantage of CLB is its low toxicity in comparison with purine nucleoside analogs like fludarabine in either CLL or NHL. In CLL, the major disadvantage is the very low rate of complete response, except when combining an anti-CD20 antibody. For B-cell lymphoma and WM, six RCTs were summarized. Results according to the usual criteria are presented and the role of CLB, used mostly in combination with an anti-CD20 antibody, is discussed for each indication, in particular for unfit patients.
Fang S, Niu Y, Zhang W, et al.
Liposome-like nanocapsules of dual drug-tailed betaine for cancer therapy.
Int J Pharm. 2015; 493(1-2):460-5 [PubMed] Related Publications
Liposome-like nanocapsules of dual drug-tailed betaine for cancer therapy.
Int J Pharm. 2015; 493(1-2):460-5 [PubMed] Related Publications
A novel dual drug-tailed betaine conjugate amphiphile has been firstly synthesized in which the polar headgroup is derived from glycine betaine and the hydrophobic tails are chlorambucil molecules. The newly prepared conjugate undergoes self-assembly to form stable liposome-like nanocapsules as an effective carrier with high drug loading capacity. The nanocapsules showed higher cytotoxic effects to cancer cell lines than those of free chlorambucil in vitro, and inhibited tumor growth effectively in vivo. This strategy that utilizes new dual drug-tailed betaine conjugate amphiphile to construct a self-assembled nanoparticle drug delivery system may have great potential in cancer chemotherapy.
Li MH, Swenson R, Harel M, et al.
Antitumor Activity of a Novel Sphingosine-1-Phosphate 2 Antagonist, AB1, in Neuroblastoma.
J Pharmacol Exp Ther. 2015; 354(3):261-8 [PubMed] Free Access to Full Article Related Publications
Antitumor Activity of a Novel Sphingosine-1-Phosphate 2 Antagonist, AB1, in Neuroblastoma.
J Pharmacol Exp Ther. 2015; 354(3):261-8 [PubMed] Free Access to Full Article Related Publications
The bioactive lipid sphingosine-1-phosphate (S1P) and its receptors (S1P1-5) play critical roles in many pathologic processes, including cancer. The S1P axis has become a bona fide therapeutic target in cancer. JTE-013 [N-(2,6-dichloro-4-pyridinyl)-2-[1,3-dimethyl-4-(1-methylethyl)-1H-pyrazolo[3,4-b]pyridin-6-yl]-hydrazinecarboxamide], a known S1P2 antagonist, suffers from instability in vivo. Structurally modified, more potent, and stable S1P2 inhibitors would be desirable pharmacological tools. One of the JTE-013 derivatives, AB1 [N-(1H-4-isopropyl-1-allyl-3-methylpyrazolo[3,4-b]pyridine-6-yl)-amino-N'-(2,6-dichloropyridine-4-yl) urea], exhibited improved S1P2 antagonism compared with JTE-013. Intravenous pharmacokinetics indicated enhanced stability or slower clearance of AB1 in vivo. Migration assays in glioblastoma showed that AB1 was slightly more effective than JTE-013 in blocking S1P2-mediated inhibition of cell migration. Functional studies in the neuroblastoma (NB) cell line SK-N-AS showed that AB1 displayed potency at least equivalent to JTE-013 in affecting signaling molecules downstream of S1P2. Similarly, AB1 inhibition of the growth of SK-N-AS tumor xenografts was improved compared with JTE-013. Cell viability assays excluded that this enhanced AB1 effect is caused by inhibition of cancer cell survival. Both JTE-013 and AB1 trended to inhibit (C-C motif) ligand 2 expression and were able to significantly inhibit subsequent tumor-associated macrophage infiltration in NB xenografts. Interestingly, AB1 was more effective than JTE-013 in inhibiting the expression of the profibrotic mediator connective tissue growth factor. The terminal deoxynucleotidyl transferase-mediated digoxigenin-deoxyuridine nick-end labeling assay and cleaved caspase-3 detection further demonstrated that apoptosis was increased in AB1-treated NB xenografts compared with JTE-013. Overall, the modification of JTE-013 to produce the AB1 compound improved potency, intravenous pharmacokinetics, cellular activity, and antitumor activity in NB and may have enhanced clinical and experimental applicability.
Hillmen P, Robak T, Janssens A, et al.
Chlorambucil plus ofatumumab versus chlorambucil alone in previously untreated patients with chronic lymphocytic leukaemia (COMPLEMENT 1): a randomised, multicentre, open-label phase 3 trial.
Lancet. 2015; 385(9980):1873-83 [PubMed] Related Publications
Chlorambucil plus ofatumumab versus chlorambucil alone in previously untreated patients with chronic lymphocytic leukaemia (COMPLEMENT 1): a randomised, multicentre, open-label phase 3 trial.
Lancet. 2015; 385(9980):1873-83 [PubMed] Related Publications
BACKGROUND: Treatment for patients with chronic lymphocytic leukaemia who are elderly or who have comorbidities is challenging because fludarabine-based chemoimmunotherapies are mostly not suitable. Chlorambucil remains the standard of care in many countries. We aimed to investigate whether the addition of ofatumumab to chlorambucil could lead to better clinical outcomes than does treatment with chlorambucil alone, while also being tolerable for patients who have few treatment options.
METHODS: We carried out a randomised, open-label, phase 3 trial for treatment-naive patients with chronic lymphocytic leukaemia in 109 centres in 16 countries. We included patients who had active disease needing treatment, but in whom fludarabine-based treatment was not possible. We randomly assigned patients (1:1) to receive oral chlorambucil (10 mg/m(2)) on days 1-7 of a 28 day treatment course or to receive chlorambucil by this schedule plus intravenous ofatumumab (cycle 1: 300 mg on day 1 and 1000 mg on day 8; subsequent cycles: 1000 mg on day 1) for three to 12 cycles. Assignment was done with a randomisation list that was computer generated at GlaxoSmithKline, and was stratified, in a block size of two, by age, disease stage, and performance status. The primary endpoint was progression-free survival in the intention-to-treat population and assessment was done by an independent review committee that was masked to group assignment. The study is registered with ClinicalTrials.gov, number NCT00748189.
FINDINGS: We enrolled 447 patients, median age 69 years (range 35-92). Between Dec 22, 2008, and May 26, 2011, we randomly assigned 221 patients to chlorambucil plus ofatumumab and 226 patients to chlorambucil alone. Median progression-free survival was 22·4 months (95% CI 19·0-25·2) in the group assigned to chlorambucil plus ofatumumab compared with 13·1 months (10·6-13·8) in the group assigned to chlorambucil only (hazard ratio 0·57, 95% CI 0·45-0·72; p<0·0001). Grade 3 or greater adverse events were more common in the chlorambucil plus ofatumumab group (109 [50%] patients; vs 98 [43%] given chlorambucil alone), with neutropenia being the most common event (56 [26%] vs 32 [14%]). Grade 3 or greater infections had similar frequency in both groups. Grade 3 or greater infusion-related adverse events were reported in 22 (10%) patients given chlorambucil plus ofatumumab. Five (2%) patients died during treatment in each group.
INTERPRETATION: Addition of ofatumumab to chlorambucil led to clinically important improvements with a manageable side-effect profile in treatment-naive patients with chronic lymphocytic leukaemia who were elderly or had comorbidities. Chlorambucil plus ofatumumab is therefore an important treatment option for these patients who cannot tolerate more intensive therapy.
FUNDING: GlaxoSmithKline, Genmab A/S.
METHODS: We carried out a randomised, open-label, phase 3 trial for treatment-naive patients with chronic lymphocytic leukaemia in 109 centres in 16 countries. We included patients who had active disease needing treatment, but in whom fludarabine-based treatment was not possible. We randomly assigned patients (1:1) to receive oral chlorambucil (10 mg/m(2)) on days 1-7 of a 28 day treatment course or to receive chlorambucil by this schedule plus intravenous ofatumumab (cycle 1: 300 mg on day 1 and 1000 mg on day 8; subsequent cycles: 1000 mg on day 1) for three to 12 cycles. Assignment was done with a randomisation list that was computer generated at GlaxoSmithKline, and was stratified, in a block size of two, by age, disease stage, and performance status. The primary endpoint was progression-free survival in the intention-to-treat population and assessment was done by an independent review committee that was masked to group assignment. The study is registered with ClinicalTrials.gov, number NCT00748189.
FINDINGS: We enrolled 447 patients, median age 69 years (range 35-92). Between Dec 22, 2008, and May 26, 2011, we randomly assigned 221 patients to chlorambucil plus ofatumumab and 226 patients to chlorambucil alone. Median progression-free survival was 22·4 months (95% CI 19·0-25·2) in the group assigned to chlorambucil plus ofatumumab compared with 13·1 months (10·6-13·8) in the group assigned to chlorambucil only (hazard ratio 0·57, 95% CI 0·45-0·72; p<0·0001). Grade 3 or greater adverse events were more common in the chlorambucil plus ofatumumab group (109 [50%] patients; vs 98 [43%] given chlorambucil alone), with neutropenia being the most common event (56 [26%] vs 32 [14%]). Grade 3 or greater infections had similar frequency in both groups. Grade 3 or greater infusion-related adverse events were reported in 22 (10%) patients given chlorambucil plus ofatumumab. Five (2%) patients died during treatment in each group.
INTERPRETATION: Addition of ofatumumab to chlorambucil led to clinically important improvements with a manageable side-effect profile in treatment-naive patients with chronic lymphocytic leukaemia who were elderly or had comorbidities. Chlorambucil plus ofatumumab is therefore an important treatment option for these patients who cannot tolerate more intensive therapy.
FUNDING: GlaxoSmithKline, Genmab A/S.
Wang X, Li J, Xu C, et al.
Scopine as a novel brain-targeting moiety enhances the brain uptake of chlorambucil.
Bioconjug Chem. 2014; 25(11):2046-54 [PubMed] Related Publications
Scopine as a novel brain-targeting moiety enhances the brain uptake of chlorambucil.
Bioconjug Chem. 2014; 25(11):2046-54 [PubMed] Related Publications
The blood brain barrier (BBB) represents the biggest challenge for therapeutic drugs to enter the brain. In our study, we selected chlorambucil (CHL), an alkylating agent, as the model therapeutic agent, and used scopine as a novel brain-targeting moiety. Here, we synthesized Chlorambucil-Scopine (CHLS) prodrug and evaluated its brain-targeting efficacy. The tissue distribution study after i.v. injection revealed that the AUC0-t and Cmax of CHLS in the brain were 14.25- and 12.20-fold of CHL, respectively. Specifically, CHLS accumulated in bEnd.3 and C6 cells in an energy-dependent manner. In C6 cells, superior anti-glioma activity with a significantly decreased IC50 of 65.42 nM/mL was observed for CHLS compared to CHL (IC50 > 400 nM/mL). The safety evaluation, including acute toxicity, pathology, and hematology study, showed minimal toxicity toward nontargeting tissues, and also reached a lower systemic toxicity at 5 mg/kg (i.v.). Our results suggested that scopine is a potential brain-targeting moiety for enhancing the brain uptake efficiency of CHL.
Goede V, Eichhorst B, Fischer K, et al.
Past, present and future role of chlorambucil in the treatment of chronic lymphocytic leukemia.
Leuk Lymphoma. 2015; 56(6):1585-92 [PubMed] Related Publications
Past, present and future role of chlorambucil in the treatment of chronic lymphocytic leukemia.
Leuk Lymphoma. 2015; 56(6):1585-92 [PubMed] Related Publications
For many decades, chlorambucil was the standard of care for chronic lymphocytic leukemia (CLL), but meanwhile has been replaced by purine analog-based chemoimmunotherapy. Monotherapy with the alkylator only retained significance in the treatment of older patients unfit for standard treatment. After successful phase II studies, recent phase III trials established combinations of chlorambucil with anti-CD20 antibodies such as rituximab, ofatumumab and obinutuzumab as a valuable treatment option for these patients. Today, chlorambucil therefore should be used as a chemotherapy backbone for antibody-based chemoimmunotherapy in this patient population rather than as monotherapy. Starting from the past role of chlorambucil in CLL treatment, we here review the most recent efforts to elaborate chlorambucil-based chemoimmunotherapy in CLL and discuss clinically relevant questions that arise from this approach.
Martinelli G, Montoro J, Vanazzi A, et al.
Chlorambucil-rituximab as first-line therapy in patients affected by follicular non-Hodgkin's lymphoma: a retrospective single-centre study.
Hematol Oncol. 2015; 33(4):129-35 [PubMed] Related Publications
Chlorambucil-rituximab as first-line therapy in patients affected by follicular non-Hodgkin's lymphoma: a retrospective single-centre study.
Hematol Oncol. 2015; 33(4):129-35 [PubMed] Related Publications
Rituximab, a chimeric monoclonal antibody directed against the CD20 antigen, has been shown to be active in newly diagnosed and relapsed patients with follicular lymphoma (FL), both as monotherapy and in combination with chemotherapy. Many studies suggest that the prognosis of patients with FL may improve when it is used in combination with chemotherapy. Despite these advances, the disease remains essentially incurable with standard therapy, and novel approaches to treatment are needed because optimal therapy is not defined. The combination of chlorambucil-rituximab is one of several standard treatment options for FL. Here, we considered data arising from 75 patients with newly diagnosed FL at the European Institute of Oncology treated with the combination of rituximab plus chlorambucil. The aim of this study was to evaluate the efficacy and safety of chlorambucil and rituximab, delivered 6 mg/m(2) /day orally for 6 weeks and 375 mg/m(2) in a standard 4-weekly schedule, respectively. Patients responding to the induction therapy received a prolonged therapy with four additional cycles of chlorambucil plus rituximab. Seventy-one patients (94.6%) completed the treatment; four patients discontinued treatment because of grade 3-4 hematological toxicity. The overall response rate was 97.3% including 74.7% of complete responses. Only two patients had a stable disease at revaluation after treatment. With a median follow-up of 57 months, 72 patients (96%) are alive. Median event-free survival (EFS) and median overall survival (OS) were not reached; 5-year OS rate was 98.4%. The 5-year EFS was 71.3%. By univariate and multivariate analyses, elevated beta-2 microglobulin levels and partial responses to therapy were correlated with worse EFS. These results suggest that the combination of chlorambucil and rituximab is an active and safe regimen in patients with newly diagnosed FL, principally in those with low tumour burden and favourable prognostic factors.
van den Broek EC, Oerlemans S, Nijziel MR, et al.
Impact of active surveillance, chlorambucil, and other therapy on health-related quality of life in patients with CLL/SLL in the Netherlands.
Ann Hematol. 2015; 94(1):45-56 [PubMed] Related Publications
Impact of active surveillance, chlorambucil, and other therapy on health-related quality of life in patients with CLL/SLL in the Netherlands.
Ann Hematol. 2015; 94(1):45-56 [PubMed] Related Publications
As survival of patients with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) increases and the number of patients who live long rises, health-related quality of life (HRQoL) becomes a relevant endpoint. Few studies investigated this, mainly as a secondary endpoint in randomized clinical trials where patients with early stage CLL/SLL, and elderly/frail patients were underrepresented. The aim of our study was to assess HRQoL in a population-based setting, including these previously underrepresented patients. Out of 175 patients diagnosed with CLL/SLL between 2004 and 2011, 136 (78 %) returned the HRQoL questionnaire. The outcomes were compared to an age- and sex-matched norm population. Detailed data on stage and treatment were extracted from a population-based hematological registry (PHAROS). Patients ever treated for CLL/SLL reported significantly poorer HRQoL than the norm population (p < 0.01 with large clinically important differences. Interestingly, no differences were observed between the norm population and patients under active surveillance. In contrast to our hypothesis, patients treated with chlorambucil reported the lowest HRQoL scores. Drastic, long-lasting negative effects of starting treatment on HRQoL cannot be excluded, whereas active surveillance does not seem to provoke worrying, anxiety, or depressive symptoms. Further elaborate research into the impact of starting therapy on HRQoL is needed, especially in patients that are underrepresented in most clinical trials, and thoroughly consider its results during revision of treatment guidelines.
Jean SR, Pereira MP, Kelley SO
Structural modifications of mitochondria-targeted chlorambucil alter cell death mechanism but preserve MDR evasion.
Mol Pharm. 2014; 11(8):2675-82 [PubMed] Related Publications
Structural modifications of mitochondria-targeted chlorambucil alter cell death mechanism but preserve MDR evasion.
Mol Pharm. 2014; 11(8):2675-82 [PubMed] Related Publications
Multidrug resistance (MDR) remains one of the major obstacles in chemotherapy, potentially rendering a multitude of drugs ineffective. Previously, we have demonstrated that mitochondrial targeting of DNA damaging agents is a promising tool for evading a number of common resistance factors that are present in the nucleus or cytosol. In particular, mitochondria-targeted chlorambucil (mt-Cbl) has increased potency and activity against resistant cancer cells compared to the parent compound chlorambucil (Cbl). However, it was found that, due to its high reactivity, mt-Cbl induces a necrotic type of cell death via rapid nonspecific alkylation of mitochondrial proteins. Here, we demonstrate that by tuning the alkylating activity of mt-Cbl via chemical modification, the rate of generation of protein adducts can be reduced, resulting in a shift of the cell death mechanism from necrosis to a more controlled apoptotic pathway. Moreover, we demonstrate that all of the modified mt-Cbl compounds effectively evade MDR resulting from cytosolic GST-μ upregulation by rapidly accumulating in mitochondria, inducing cell death directly from within. In this study, we systematically elucidated the advantages and limitations of targeting alkylating agents with varying reactivity to mitochondria.


 Chronic Lymphocytic Leukemia (CLL)
Chronic Lymphocytic Leukemia (CLL)