Found this page useful?
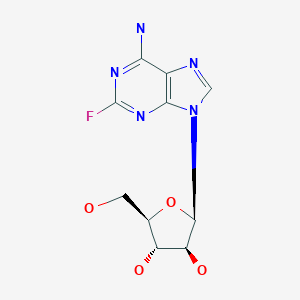
Fludarabine
 Web Resources: Fludarabine
Web Resources: Fludarabine Recent Research Publications
Recent Research PublicationsWeb Resources: Fludarabine (6 links)
Cancer Research UK
Macmillan Cancer Support
NHS Evidence
 Fludarabine - Substance Summary
Fludarabine - Substance Summary
PubChem
Irish Cancer Society
MedlinePlus
Recent Research Publications
Shanafelt TD, Wang XV, Kay NE, et al.
Ibrutinib-Rituximab or Chemoimmunotherapy for Chronic Lymphocytic Leukemia.
N Engl J Med. 2019; 381(5):432-443 [PubMed] Related Publications
Ibrutinib-Rituximab or Chemoimmunotherapy for Chronic Lymphocytic Leukemia.
N Engl J Med. 2019; 381(5):432-443 [PubMed] Related Publications
BACKGROUND: Data regarding the efficacy of treatment with ibrutinib-rituximab, as compared with standard chemoimmunotherapy with fludarabine, cyclophosphamide, and rituximab, in patients with previously untreated chronic lymphocytic leukemia (CLL) have been limited.
METHODS: In a phase 3 trial, we randomly assigned (in a 2:1 ratio) patients 70 years of age or younger with previously untreated CLL to receive either ibrutinib and rituximab for six cycles (after a single cycle of ibrutinib alone), followed by ibrutinib until disease progression, or six cycles of chemoimmunotherapy with fludarabine, cyclophosphamide, and rituximab. The primary end point was progression-free survival, and overall survival was a secondary end point. We report the results of a planned interim analysis.
RESULTS: A total of 529 patients underwent randomization (354 patients to the ibrutinib-rituximab group, and 175 to the chemoimmunotherapy group). At a median follow-up of 33.6 months, the results of the analysis of progression-free survival favored ibrutinib-rituximab over chemoimmunotherapy (89.4% vs. 72.9% at 3 years; hazard ratio for progression or death, 0.35; 95% confidence interval [CI], 0.22 to 0.56; P<0.001), and the results met the protocol-defined efficacy threshold for the interim analysis. The results of the analysis of overall survival also favored ibrutinib-rituximab over chemoimmunotherapy (98.8% vs. 91.5% at 3 years; hazard ratio for death, 0.17; 95% CI, 0.05 to 0.54; P<0.001). In a subgroup analysis involving patients without immunoglobulin heavy-chain variable region (
CONCLUSIONS: The ibrutinib-rituximab regimen resulted in progression-free survival and overall survival that were superior to those with a standard chemoimmunotherapy regimen among patients 70 years of age or younger with previously untreated CLL. (Funded by the National Cancer Institute and Pharmacyclics; E1912 ClinicalTrials.gov number, NCT02048813.).
METHODS: In a phase 3 trial, we randomly assigned (in a 2:1 ratio) patients 70 years of age or younger with previously untreated CLL to receive either ibrutinib and rituximab for six cycles (after a single cycle of ibrutinib alone), followed by ibrutinib until disease progression, or six cycles of chemoimmunotherapy with fludarabine, cyclophosphamide, and rituximab. The primary end point was progression-free survival, and overall survival was a secondary end point. We report the results of a planned interim analysis.
RESULTS: A total of 529 patients underwent randomization (354 patients to the ibrutinib-rituximab group, and 175 to the chemoimmunotherapy group). At a median follow-up of 33.6 months, the results of the analysis of progression-free survival favored ibrutinib-rituximab over chemoimmunotherapy (89.4% vs. 72.9% at 3 years; hazard ratio for progression or death, 0.35; 95% confidence interval [CI], 0.22 to 0.56; P<0.001), and the results met the protocol-defined efficacy threshold for the interim analysis. The results of the analysis of overall survival also favored ibrutinib-rituximab over chemoimmunotherapy (98.8% vs. 91.5% at 3 years; hazard ratio for death, 0.17; 95% CI, 0.05 to 0.54; P<0.001). In a subgroup analysis involving patients without immunoglobulin heavy-chain variable region (
CONCLUSIONS: The ibrutinib-rituximab regimen resulted in progression-free survival and overall survival that were superior to those with a standard chemoimmunotherapy regimen among patients 70 years of age or younger with previously untreated CLL. (Funded by the National Cancer Institute and Pharmacyclics; E1912 ClinicalTrials.gov number, NCT02048813.).
Barrenetxea Lekue C, Grasso Cicala S, Leppä S, et al.
Pixantrone beyond monotherapy: a review.
Ann Hematol. 2019; 98(9):2025-2033 [PubMed] Free Access to Full Article Related Publications
Pixantrone beyond monotherapy: a review.
Ann Hematol. 2019; 98(9):2025-2033 [PubMed] Free Access to Full Article Related Publications
Outcomes for patients with non-Hodgkin's lymphoma (NHL) that proves refractory to treatment remain poor. Treatment of such patients is individualized and can include enrolment in a clinical trial of novel agents or use of one of a wide array of drug regimens. Initial treatment with anthracyclines such as doxorubicin limits options at later stages of treatment because of anthracycline-related cumulative cardiotoxicity. The aza-anthracenedione pixantrone was developed to reduce the likelihood of cardiotoxicity without compromising efficacy and is currently conditionally approved for use as monotherapy in patients with multiply-relapsed or refractory aggressive B cell NHL. The use of pixantrone in combination therapy, often to replace doxorubicin or mitoxantrone, has or is currently being investigated in numerous studies in patients with aggressive or indolent NHL and is the focus of this review. These include the R-CPOP regimen (rituximab, cyclophosphamide, pixantrone, vincristine, prednisone) for aggressive NHL in the first-line setting, including a study in elderly patients with limited cardiac function, and for patients with relapsed NHL with prior anthracycline exposure; the PSHAP regimen (pixantrone, cytarabine, prednisone, cisplatin), also in the latter setting; the PREBen/PEBen regimen (pixantrone, bendamustine and etoposide with or without rituximab) as salvage therapy; and pixantrone in combination with fludarabine, dexamethasone, and rituximab (FPD-R) for relapsed indolent NHL.
Gao XN, Lin J, Wang LJ, et al.
Risk factors and clinical outcomes of Epstein-Barr virus DNAemia and post-transplant lymphoproliferative disorders after haploidentical and matched-sibling PBSCT in patients with hematologic malignancies.
Ann Hematol. 2019; 98(9):2163-2177 [PubMed] Related Publications
Risk factors and clinical outcomes of Epstein-Barr virus DNAemia and post-transplant lymphoproliferative disorders after haploidentical and matched-sibling PBSCT in patients with hematologic malignancies.
Ann Hematol. 2019; 98(9):2163-2177 [PubMed] Related Publications
In allogeneic hematopoietic stem cell transplantation recipients, reactivation of Epstein-Barr virus (EBV) can cause post-transplantation lymphoproliferative disorder (PTLD), which may rapidly progress to multiorgan failure and even death. Development of EBV PTLD correlates very closely with use of anti-thymocyte globulin (ATG) and type of transplant. To assess the incidences and clinical features of EBV DNAemia and PTLD in the setting of stem cell transplantation using unmanipulated G-CSF-primed allogeneic peripheral blood stem cells as graft, we performed a retrospective analysis of stem cell transplantation from HLA-matched sibling donors (MSD-SCT, n = 90) or HLA-haploidentical related donors (HID-SCT, n = 110) in patients with hematological malignancies. All of HID-SCT recipients and 27.8% of MSD-SCT recipients received an ATG-containing conditioning regimen. One-year cumulative incidence of EBV DNAemia was 44.1%, ranging from 4.8% in MSD-SCT recipients not using ATG to 20.0% in MSD-SCT recipients using ATG, and 73.7% in HID-SCT recipients. Risk factors for EBV reactivation included use of ATG (p = 0.008), male donor (p = 0.034), and cytomegalovirus DNAemia (p < 0.001). One-year incidence of EBV PTLD was 11.9%, ranging from 1.8% in recipients of MSD-SCT not using ATG to 4.4% in recipients of MSD-SCT using ATG, and 23.5% in recipients of HID-SCT. Risk factors for PTLD after HID-SCT included in fludarabine-containing conditioning regimen (p = 0.010), cytomegalovirus DNAemia (p = 0.036), and patient's age < 40-yr (p = 0.032). Two-year non-relapse mortality was higher for patients with EBV DNAemia than those without EBV DNAemia (35.8% vs. 15.3%, p = 0.002). One-year relapse-free survival and overall survival among patients with PTLD were 40.2% and 44.9%, respectively, as opposed to 63.4% and 68.4% among patients without PTLD (both p < 0.05). In multivariate analyses, EBV DNAemia predicted a lower risk of relapse (p = 0.025), while PTLD was a marginally significant predictor of relapse (p = 0.092). This study identified patients at risk of EBV reactivation and PTLD after unmanipulated allogeneic peripheral blood stem cell transplantation.
Sachanas S, Pangalis GA, Fink AM, et al.
Small Lymphocytic Lymphoma: Analysis of Two Cohorts Including Patients in Clinical Trials of the German Chronic Lymphocytic Leukemia Study Group (GCLLSG) or in "Real-Life" Outside of Clinical Trials.
Anticancer Res. 2019; 39(5):2591-2598 [PubMed] Related Publications
Small Lymphocytic Lymphoma: Analysis of Two Cohorts Including Patients in Clinical Trials of the German Chronic Lymphocytic Leukemia Study Group (GCLLSG) or in "Real-Life" Outside of Clinical Trials.
Anticancer Res. 2019; 39(5):2591-2598 [PubMed] Related Publications
BACKGROUND: Only few studies have focused exclusively on patients with small lymphocytic lymphoma (SLL).
PATIENTS AND METHODS: In the present report, 103 SLL patients were analyzed from both, clinical trials of the German Chronic Lymphocytic Leukemia Study Group and Greek centers, and emphasis was placed on the therapeutic strategy. The impact of lymph node characteristics, such as the presence of proliferation centers (PCs) on response and survival was also assessed.
RESULTS: SLL patients included in clinical trials were treated mostly with fludarabine-based regimens while those in "real-life" were staged and treated mostly as patients with low-grade lymphomas. Our analysis showed a trend for better survival for patients with SLL without detectable PCs.
CONCLUSION: Patients with SLL outside of clinical trials are usually treated as cases of lymphoma. In addition, this analysis supports published data regarding the adverse prognostic value of the presence of PCs in lymphoid nodes in SLL.
PATIENTS AND METHODS: In the present report, 103 SLL patients were analyzed from both, clinical trials of the German Chronic Lymphocytic Leukemia Study Group and Greek centers, and emphasis was placed on the therapeutic strategy. The impact of lymph node characteristics, such as the presence of proliferation centers (PCs) on response and survival was also assessed.
RESULTS: SLL patients included in clinical trials were treated mostly with fludarabine-based regimens while those in "real-life" were staged and treated mostly as patients with low-grade lymphomas. Our analysis showed a trend for better survival for patients with SLL without detectable PCs.
CONCLUSION: Patients with SLL outside of clinical trials are usually treated as cases of lymphoma. In addition, this analysis supports published data regarding the adverse prognostic value of the presence of PCs in lymphoid nodes in SLL.
Matsuoka S, Tsutsumi Y, Kikuchi R, et al.
Gene Polymorphism of Tacrolimus-Metabolizing Enzymes Associated With Impaired Absorption of Tacrolimus Following Allogeneic Hematopoietic Stem Cell Transplantation: A Case Report.
Transplant Proc. 2019; 51(3):998-1001 [PubMed] Related Publications
Gene Polymorphism of Tacrolimus-Metabolizing Enzymes Associated With Impaired Absorption of Tacrolimus Following Allogeneic Hematopoietic Stem Cell Transplantation: A Case Report.
Transplant Proc. 2019; 51(3):998-1001 [PubMed] Related Publications
OBJECTIVE: To elucidate the mechanisms by which orally administered tacrolimus was not absorbed in a patient following allogeneic hematopoietic stem cell transplantation.
CLINICAL COURSE: A 17-year-old girl with acute myeloid leukemia underwent HLA-haploidentical peripheral blood stem cell transplantation following fludarabine, busulfan, and total-body irradiation. Graft-vs-host disease prophylaxis was post-transplant cyclophosphamide, followed by intravenous tacrolimus and mycophenolate mofetil. When tacrolimus was switched to oral administration, its blood level declined rapidly, resulting in development of acute graft-vs-host disease, which was ameliorated by switching back to intravenous administration.
METHODS/RESULTS: To elucidate if impaired tacrolimus absorption could be related to genetic polymorphism of tacrolimus-metabolizing enzymes, we analyzed gene polymorphisms of cytochrome P450 3A4, cytochrome P450 3A5, and multidrug resistance 1 (MDR1). The patient had wild-type cytochrome P450 3A4 (*1/*1) and variant-type cytochrome P450 3A5 (*3/*3), while MDR1 genes (2677A/G, 3435C/C) were wild-type.
CONCLUSION: Wild-type MDR1 gene product P-glycoprotein expressed in the intestine reduces drug absorption from the gastrointestinal tract and may have contributed to low blood levels of tacrolimus in this patient when tacrolimus was orally administered.
CLINICAL COURSE: A 17-year-old girl with acute myeloid leukemia underwent HLA-haploidentical peripheral blood stem cell transplantation following fludarabine, busulfan, and total-body irradiation. Graft-vs-host disease prophylaxis was post-transplant cyclophosphamide, followed by intravenous tacrolimus and mycophenolate mofetil. When tacrolimus was switched to oral administration, its blood level declined rapidly, resulting in development of acute graft-vs-host disease, which was ameliorated by switching back to intravenous administration.
METHODS/RESULTS: To elucidate if impaired tacrolimus absorption could be related to genetic polymorphism of tacrolimus-metabolizing enzymes, we analyzed gene polymorphisms of cytochrome P450 3A4, cytochrome P450 3A5, and multidrug resistance 1 (MDR1). The patient had wild-type cytochrome P450 3A4 (*1/*1) and variant-type cytochrome P450 3A5 (*3/*3), while MDR1 genes (2677A/G, 3435C/C) were wild-type.
CONCLUSION: Wild-type MDR1 gene product P-glycoprotein expressed in the intestine reduces drug absorption from the gastrointestinal tract and may have contributed to low blood levels of tacrolimus in this patient when tacrolimus was orally administered.
Zhang W, Liang X, Gong Y, et al.
The Signal Transducer and Activator of Transcription 5B (STAT5B) Gene Promotes Proliferation and Drug Resistance of Human Mantle Cell Lymphoma Cells by Activating the Akt Signaling Pathway.
Med Sci Monit. 2019; 25:2599-2608 [PubMed] Free Access to Full Article Related Publications
The Signal Transducer and Activator of Transcription 5B (STAT5B) Gene Promotes Proliferation and Drug Resistance of Human Mantle Cell Lymphoma Cells by Activating the Akt Signaling Pathway.
Med Sci Monit. 2019; 25:2599-2608 [PubMed] Free Access to Full Article Related Publications
BACKGROUND Mantle cell lymphoma (MCL) is a high-grade B-cell lymphoma with poor prognosis. Fludarabine is used alone or in combination for relapsed and advanced-stage MCL. The expression of the signal transducer and activator of transcription 5B (STAT5B) gene is associated with tumorigenesis in solid tumors, but its role in MCL remains unknown. The aims of this study were to investigate the role of STAT5B in GRANTA-519 human mantle cell lymphoma cells and drug resistance. MATERIAL AND METHODS GRANTA-519 human mantle cell lymphoma cells were cultured with and without 10 μM fludarabine dephosphorylated 9-ß-D-arabinofuranosyl-2-fluoroadenine, (2-F-araA) or 10 μM 4-hydroperoxycyclophosphamide (4-HC). The MTT assay assessed cell proliferation. Flow cytometry was used to investigate the cell cycle in MCL cells treated with the specific inhibitor of the Akt pathway, LY294002, and assessed cell cycle and cell apoptosis. Western blot was used to detect the expression levels of p-Akt/Akt and STAT5B/p-STAT5B. The gene expression profiles of lymph node (LN)-derived MCL cells were compared with peripheral blood (PB)-derived lymphocytes using bioinformatics and hierarchical cluster analysis. Quantitative reverse transcription polymerase chain reaction (RT-qPCR) was performed to determine the expression of the marker of proliferation Ki-67 (MKI67) gene. RESULTS STAT5B was significantly upregulated in LN-derived MCL cells compared with PB lymphocytes. Increased expression of STAT5B was associated with increased MCL cell proliferation and reduced cell apoptosis and was associated with drug resistance and activation of Akt. CONCLUSIONS STAT5B promoted cell proliferation and drug resistance in human MCL cells by activating the Akt signaling pathway.
Ysebaert L, Larcher M, Compaci G, et al.
Oncology nurse phone calls halve the risk of reduced dose intensity of immunochemotherapy: results of the randomized FORTIS study in chronic lymphocytic leukemia.
Ann Hematol. 2019; 98(4):931-939 [PubMed] Related Publications
Oncology nurse phone calls halve the risk of reduced dose intensity of immunochemotherapy: results of the randomized FORTIS study in chronic lymphocytic leukemia.
Ann Hematol. 2019; 98(4):931-939 [PubMed] Related Publications
Delivering of > 80% planned relative dose intensity (RDI) of fludarabine-cyclophosphamide-rituximab (FCR) is key to benefit from longer progression free survival (PFS) and survivals in CLL. In this randomized trial, we sought to investigate whether a telephone intervention strategy (called AMA) delivered by an oncology nurse could reduce the risk of RDI < 80% by alleviating adverse events and supporting patients' adherence. Sixty FCR patients were randomized 1:1 for AMA (stratified on Binet stage C). As per guidelines, patients received pegfilgrastim as primary prophylaxis of febrile neutropenia. At the end of therapy, RDI < 80% was reported in 31% of patients, shortening PFS (median 26 months versus not reached, P = 0.021) and OS at 3 years (100 vs 70%, P = 0.0089). Oncology nurse interventions tended to significantly reduce this event (RDI < 80%: 41.4% in non-AMA versus 20.7% in AMA patients (p = 0.09)). By adjusting our logistic regression model on published parameters exposing to RDI < 80%, we found that AMA protected significantly against the risk of reduced RDI (OR = 0.22, IC95% 0.05-0.84, p = 0.04), independently of grade 3/4 neutropenia (< 15% per cycle) and febrile neutropenia (< 5% per cycle) events. As a conclusion, we confirmed that > 20% reduction of FCR dose-intensity was detrimental for PFS/OS, but that oncology nurse interventions reduced the risk of dose concessions.
Herishanu Y, Tadmor T, Braester A, et al.
Low-dose fludarabine and cyclophosphamide combined with standard dose rituximab (LD-FCR) is an effective and safe regimen for elderly untreated patients with chronic lymphocytic leukemia: The Israeli CLL study group experience.
Hematol Oncol. 2019; 37(2):185-192 [PubMed] Related Publications
Low-dose fludarabine and cyclophosphamide combined with standard dose rituximab (LD-FCR) is an effective and safe regimen for elderly untreated patients with chronic lymphocytic leukemia: The Israeli CLL study group experience.
Hematol Oncol. 2019; 37(2):185-192 [PubMed] Related Publications
Chronic lymphocytic leukemia (CLL) is a disease of elderly patients. The fludarabine, cyclophosphamide, and rituximab (FCR) regimen is considered the treatment of choice for young fit patients with CLL; however, this combination is toxic for older patients. At the time this study was first planned and initiated, there was no standard chemo-immunotherapy regimen regarded as standard therapy for the less fit elderly patient with CLL. Here, we conducted a single-arm, phase II trial to examine the efficacy and safety of lower-dose fludarabine and cyclophosphamide combined with a standard dose of rituximab (LD-FCR) in elderly patients with previously untreated CLL. Forty patients received LD-FCR and were included in the efficacy analysis. Two patients treated with FC alone were only included in the safety analysis. The median age was 72.7 years (range, 65.0 to 85.0). The overall response and complete response rates were 67.5% and 42.5%, respectively. Median progression-free survival (PFS) was 35.5 months (95% CI, 29.27-41.67). Two patients (4.8%) died during the study period. Hematological toxicities and infections were the most common complications encountered; grade 3 to 4 treatment-related neutropenia occurred in 20 (47.6%) patients. During the entire study follow-up, 26 patients (61.9%) had all grades of infection including six (14.3%) with neutropenic fever and eight (19%) with grade 3 to 4 non-neutropenic infections. In conclusion, LD-FCR is an effective and relatively safe regimen for previously untreated patients with CLL. It has the advantage of being both "time and cost limited" and, even in the era of novel agents, can still be considered when planning treatment for elderly patients without high-risk biomarkers. However, recent results in fit elderly patients using the combination of bendamustine and rituximab which have achieved longer PFS with good safety profile must be taken into consideration in this regard.
Hatsumi N, Miyawaki S, Yamauchi T, et al.
Phase II study of FLAGM (fludarabine + high-dose cytarabine + granulocyte colony-stimulating factor + mitoxantrone) for relapsed or refractory acute myeloid leukemia.
Int J Hematol. 2019; 109(4):418-425 [PubMed] Related Publications
Phase II study of FLAGM (fludarabine + high-dose cytarabine + granulocyte colony-stimulating factor + mitoxantrone) for relapsed or refractory acute myeloid leukemia.
Int J Hematol. 2019; 109(4):418-425 [PubMed] Related Publications
Given the poor prognosis of patients with relapsed/refractory acute myeloid leukemia (AML), better therapy is needed. Fludarabine enhances the efficacy of Ara-C (cytarabine) by increasing intracellular Ara-C-triphosphate. The FLAG (fludarabine, high-dose Ara-C, supported with granulocyte colony-stimulating factor) regimen has been tested for use in AML patients by other investigators. In the phase II study reported here, we evaluated the efficacy and toxicity of FLAGM therapy (FLAG with mitoxantrone), further intensified by adding mitoxantrone, based on the results of a phase I study by our group. The major endpoints were complete remission (CR) rate and early death. From June 2004 to February 2008, 41 patients (median age 52 years; range 18-64 years) were enrolled. Thirty (73% 95% CI 58-84%) patients achieved CR, which met the primary endpoint; there was a single case of early death from pneumonia. Two-year overall survival was 39.4% (95% CI 25.2-55.6%). Of those who achieved CR, 27 underwent allogeneic stem cell transplantation (SCT), and 12 SCT recipients showed long-term survival. Grade 3/4 non-hematological adverse events included infection (59%), nausea/vomiting (15%), diarrhea (7%), and elevated liver enzymes (7%). In conclusion, FLAGM is an effective and safe salvage therapy for patients with relapsed/refractory AML, and facilitated SCT for a large proportion of patients.
Hoogstad-van Evert J, Bekkers R, Ottevanger N, et al.
Intraperitoneal infusion of ex vivo-cultured allogeneic NK cells in recurrent ovarian carcinoma patients (a phase I study).
Medicine (Baltimore). 2019; 98(5):e14290 [PubMed] Free Access to Full Article Related Publications
Intraperitoneal infusion of ex vivo-cultured allogeneic NK cells in recurrent ovarian carcinoma patients (a phase I study).
Medicine (Baltimore). 2019; 98(5):e14290 [PubMed] Free Access to Full Article Related Publications
INTRODUCTION: Recurrent ovarian carcinoma has dismal prognosis, but control of disease and prolonged survival are possible in some patients. The estimated 5-year survival is 46% for all stages of ovarian cancer, and only 28% for metastasized disease. Notably, the majority of women with ovarian cancer are diagnosed with stage III or IV disease with a high recurrence rate. As most women with relapsed or metastatic cancer will die of progressive disease, there is an urgent need for novel therapeutic strategies. The primary aim of our study is to evaluate safety and toxicity of intraperitoneal infusion of ex vivo-expanded natural killer cells (NK), generated from CD34+ umbilical cord blood (UCB) progenitor cells, with and without a preceding non-myeloablative immunosuppressive conditioning regimen in patients suffering from recurrent ovarian cancer. The secondary objectives are to compare the in vivo lifespan, expansion, and biological activity of intraperitoneally infused NK cell products with or without preparative chemotherapy, as well as evaluate effects on disease load.
METHODS: In this phase I safety trial, 12 patients who are suffering from recurrent ovarian cancer, detected by a significant rise in serum level of CA-125 on two successive time points, will be included. Prior to UCB-NK cell infusion, a laparoscopy is performed to place a catheter in the peritoneal cavity. The first cohort of three patients will receive a single intraperitoneal infusion of 1.5-3×10 UCB-NK cells, generated ex vivo from CD34+ hematopoietic progenitor cells obtained from an allogeneic UCB unit, without a preparative chemotherapy regimen. The second group of three patients will be treated with a similar dose of UCB-NK cells following a preparative four days non-myeloablative immunosuppressive conditioning regimen with cyclophosphamide and fludarabine (Cy/Flu). If no severe toxicity is seen in these 6 patients, an extension cohort of 6 patients will be included to answer the secondary objectives.
DISCUSSION: This study investigates the safety of a promising new cellular therapy in a group of patients with a poor prognosis. Demonstration of safety and in vivo expansion capacity of allogeneic UCB-NK cells in the absence of Cy/Flu pretreatment will provide rationale for UCB-NK cell infusion after regular second-line chemotherapy.
METHODS: In this phase I safety trial, 12 patients who are suffering from recurrent ovarian cancer, detected by a significant rise in serum level of CA-125 on two successive time points, will be included. Prior to UCB-NK cell infusion, a laparoscopy is performed to place a catheter in the peritoneal cavity. The first cohort of three patients will receive a single intraperitoneal infusion of 1.5-3×10 UCB-NK cells, generated ex vivo from CD34+ hematopoietic progenitor cells obtained from an allogeneic UCB unit, without a preparative chemotherapy regimen. The second group of three patients will be treated with a similar dose of UCB-NK cells following a preparative four days non-myeloablative immunosuppressive conditioning regimen with cyclophosphamide and fludarabine (Cy/Flu). If no severe toxicity is seen in these 6 patients, an extension cohort of 6 patients will be included to answer the secondary objectives.
DISCUSSION: This study investigates the safety of a promising new cellular therapy in a group of patients with a poor prognosis. Demonstration of safety and in vivo expansion capacity of allogeneic UCB-NK cells in the absence of Cy/Flu pretreatment will provide rationale for UCB-NK cell infusion after regular second-line chemotherapy.
Sipilä JOT, Soilu-Hänninen M, Rautava P, Kytö V
Progressive multifocal leukoencephalopathy in Finland: a cross-sectional registry study.
J Neurol. 2019; 266(2):515-521 [PubMed] Free Access to Full Article Related Publications
Progressive multifocal leukoencephalopathy in Finland: a cross-sectional registry study.
J Neurol. 2019; 266(2):515-521 [PubMed] Free Access to Full Article Related Publications
OBJECTIVE: To investigate if progressive multifocal leucoencephalopathy (PML) incidence has increased in Finland like in the neighbouring Sweden.
METHODS: National administrative registries were searched for all PML admissions aged 16 years or more in 2004-2014 on all neurological and internal medicine wards in Finland. The mortality data of the patients was extracted from the national causes of death registry. National level data on annual predisposing drug use was obtained from the national pharmaceutical authority.
RESULTS: We identified 35 PML cases (57% male) with a peak in 2010-2011 that amounted to 49% of all cases. The annual incidence for the entire study period was 0.072/100,000 person-years (95% CI 0.050-0.10) with no temporal trend (p = 0.18). Mean age was 57 years (22-88 years) with no sex difference (p = 0.42). Neoplasms (60%), HIV infection (17%) and systemic connective tissue disorders (CTD, 14%) were the most common predisposing conditions. MS was recorded in three cases (9%). The national level use of drugs that predispose to PML increased during the study period, with the exceptions of alemtuzumab and fludarabine. Overall survival was 85% at 90 days, 79% at 1 year, and 66% at 5 years. Survival was worst in patients with malignancy and best in patients with CTD.
CONCLUSIONS: PML most often occurs in patients with malignancies and patients with HIV or CTD cover a third. PML incidence in Finland is lower than in Sweden and shows no temporal trend despite increasing use of predisposing drugs. Mortality after PML varies according to the predisposing condition.
METHODS: National administrative registries were searched for all PML admissions aged 16 years or more in 2004-2014 on all neurological and internal medicine wards in Finland. The mortality data of the patients was extracted from the national causes of death registry. National level data on annual predisposing drug use was obtained from the national pharmaceutical authority.
RESULTS: We identified 35 PML cases (57% male) with a peak in 2010-2011 that amounted to 49% of all cases. The annual incidence for the entire study period was 0.072/100,000 person-years (95% CI 0.050-0.10) with no temporal trend (p = 0.18). Mean age was 57 years (22-88 years) with no sex difference (p = 0.42). Neoplasms (60%), HIV infection (17%) and systemic connective tissue disorders (CTD, 14%) were the most common predisposing conditions. MS was recorded in three cases (9%). The national level use of drugs that predispose to PML increased during the study period, with the exceptions of alemtuzumab and fludarabine. Overall survival was 85% at 90 days, 79% at 1 year, and 66% at 5 years. Survival was worst in patients with malignancy and best in patients with CTD.
CONCLUSIONS: PML most often occurs in patients with malignancies and patients with HIV or CTD cover a third. PML incidence in Finland is lower than in Sweden and shows no temporal trend despite increasing use of predisposing drugs. Mortality after PML varies according to the predisposing condition.
Jain N
Selecting Frontline Therapy for CLL in 2018.
Hematology Am Soc Hematol Educ Program. 2018; 2018(1):242-247 [PubMed] Article available free on PMC after 30/11/2019 Related Publications
Selecting Frontline Therapy for CLL in 2018.
Hematology Am Soc Hematol Educ Program. 2018; 2018(1):242-247 [PubMed] Article available free on PMC after 30/11/2019 Related Publications
The treatment landscape of chronic lymphocytic leukemia (CLL) has changed dramatically in the last few years. The role of chemoimmunotherapy has declined significantly for patients with CLL. Fludarabine, cyclophosphamide, rituximab chemotherapy remains the standard frontline therapy for young fit patients with CLL, especially if
Al-Sawaf O, Bahlo J, Robrecht S, et al.
Outcome of patients aged 80 years or older treated for chronic lymphocytic leukaemia.
Br J Haematol. 2018; 183(5):727-735 [PubMed] Related Publications
Outcome of patients aged 80 years or older treated for chronic lymphocytic leukaemia.
Br J Haematol. 2018; 183(5):727-735 [PubMed] Related Publications
Clinical management of chronic lymphocytic leukaemia (CLL) in patients aged ≥80 years is based on limited evidence due to the lack of published information. Therefore, we analysed CLL patients aged ≥80 years using data from seven phase III clinical trials of the German CLL Study Group. Among 3552 participants, 152 were ≥80 years old at initiation of first-line study treatment. Median age was 82 years (range 80-90). Concomitant diseases were present in 99% of the patients, with a median cumulative illness rating scale score of 8 (0-18). Chemoimmunotherapy with chlorambucil-obinutuzumab (CLB-OB) or chlorambucil-rituximab (CLB-R) was administered to 61 (40%) and 56 (37%) patients. The remaining patients received CLB (n = 19) or fludarabine (F, n = 10), F/cyclophosphamide (FC, n = 1), FC/rituximab (FCR, n = 2) or bendamustine/rituximab (BR, n = 3). Rates of grade 3 or 4 neutropenia and infections were 35% and 13%. Overall response rate was 77% with 13% complete remissions. Median progression-free survival and treatment-free survival were 17·2 and 32·3 months, respectively. Median overall survival was 48·3 months; adverse events (22%) and progressive CLL (16·4%) were the most frequent causes of death. These findings suggest that anti-leukaemic treatment including chemoimmunotherapy is feasible and efficacious in ≥80-year-old CLL patients. However, this group of patients lives for a shorter time than age-matched controls of the general population.
Ueda T, Maeda T, Kusakabe S, et al.
Addition of melphalan to fludarabine/busulfan (FLU/BU4/MEL) provides survival benefit for patients with myeloid malignancy following allogeneic bone-marrow transplantation/peripheral blood stem-cell transplantation.
Int J Hematol. 2019; 109(2):197-205 [PubMed] Related Publications
Addition of melphalan to fludarabine/busulfan (FLU/BU4/MEL) provides survival benefit for patients with myeloid malignancy following allogeneic bone-marrow transplantation/peripheral blood stem-cell transplantation.
Int J Hematol. 2019; 109(2):197-205 [PubMed] Related Publications
A conditioning regimen with fludarabine and myeloablative dose of busulfan (FLU/BU4) has been commonly used in allogeneic hematopoietic cell transplantation (allo-HCT). However, there are two major problems with this regimen: insufficient anti-leukemic effect, especially in advanced cases, and slow time to complete donor-type chimerism, especially T-cell chimerism. To overcome these issues, we designed a combination regimen with FLU (150 mg/m
Fu C, Shi X, Gong Y, et al.
Constitutively Photomorphogenic 1 Reduces the Sensitivity of Chronic Lymphocytic Leukemia Cells to Fludarabine Through Promotion of Ubiquitin-Mediated P53 Degradation.
Cell Physiol Biochem. 2018; 50(6):2314-2328 [PubMed] Related Publications
Constitutively Photomorphogenic 1 Reduces the Sensitivity of Chronic Lymphocytic Leukemia Cells to Fludarabine Through Promotion of Ubiquitin-Mediated P53 Degradation.
Cell Physiol Biochem. 2018; 50(6):2314-2328 [PubMed] Related Publications
BACKGROUND/AIMS: Chronic Lymphocytic leukemia (CLL) is characterized by accumulation of cells in the G0/G1 phase of the cell cycle and resistance to apoptosis due to gene mutation or abnormal gene expression. In our previous study, constitutively photomorphogenic 1 (COP1) was shown to be upregulated in Binet C-phase CLL patients. Based on the negative regulation of COP1 in the repair of DNA damage, we further studied the function of COP1 in CLL cell apoptosis induced by fludarabine in vitro and in vivo.
METHODS: We analyzed the sensitivity of primary CLL cells to the fludarabine by CCK-8, and detected the expression of p53 in cells after drug treatment by western blot. Next, we constructed COP1 overexrpessing CLL cell line HG3, and analyzed the effect of COP1 overexpression on the HG3 cell's apoptosis, and HG3 transplant mice survival with drug treatment.
RESULTS: Here, we found that primary CLL cells with high expression of COP1 showed low sensitivity to the drug and presented delayed enrichment of p53 protein than cells with low COP1 expressed. COP1 overexpression reduced HG3 cell sensitivity to the fludarabine treatment and inhibited cell apoptosis, and also retarded itself via autoubiquitination. The further study showed that COP1 promoted ubiquitin-dependent p53 degradation, which further disrupts the formation of the p53-Brn-3a complex and activation of Bcl-2 transcription. Moreover, mice engrafted with cells overexpressing COP1 showed a shortened survival, increased tumor cells burden in spleen and bone marrow (BM), and reduced tumor cell apoptosis even when fludarabine combined cyclophosphamide (F+C) therapy was administered.
CONCLUSION: This study demonstrates that COP1 contributes to drug resistance of CLL cells to the fludarabine treatment in vitro and in vivo.
METHODS: We analyzed the sensitivity of primary CLL cells to the fludarabine by CCK-8, and detected the expression of p53 in cells after drug treatment by western blot. Next, we constructed COP1 overexrpessing CLL cell line HG3, and analyzed the effect of COP1 overexpression on the HG3 cell's apoptosis, and HG3 transplant mice survival with drug treatment.
RESULTS: Here, we found that primary CLL cells with high expression of COP1 showed low sensitivity to the drug and presented delayed enrichment of p53 protein than cells with low COP1 expressed. COP1 overexpression reduced HG3 cell sensitivity to the fludarabine treatment and inhibited cell apoptosis, and also retarded itself via autoubiquitination. The further study showed that COP1 promoted ubiquitin-dependent p53 degradation, which further disrupts the formation of the p53-Brn-3a complex and activation of Bcl-2 transcription. Moreover, mice engrafted with cells overexpressing COP1 showed a shortened survival, increased tumor cells burden in spleen and bone marrow (BM), and reduced tumor cell apoptosis even when fludarabine combined cyclophosphamide (F+C) therapy was administered.
CONCLUSION: This study demonstrates that COP1 contributes to drug resistance of CLL cells to the fludarabine treatment in vitro and in vivo.
Popat UR, Mehta RS, Bassett R, et al.
Fludarabine with a higher versus lower dose of myeloablative timed-sequential busulfan in older patients and patients with comorbidities: an open-label, non-stratified, randomised phase 2 trial.
Lancet Haematol. 2018; 5(11):e532-e542 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
Fludarabine with a higher versus lower dose of myeloablative timed-sequential busulfan in older patients and patients with comorbidities: an open-label, non-stratified, randomised phase 2 trial.
Lancet Haematol. 2018; 5(11):e532-e542 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
BACKGROUND: Haemopoietic stem-cell transplantation (HCT) conditioning regimens that can reduce risk of relapse without increasing non-relapse mortality are needed. We aimed to test the safety of timed-sequential delivery of low-dose versus high-dose myeloablative busulfan in older patients and patients with comorbidities.
METHODS: This non-stratified, open-label, randomised phase 2 trial was done at The University of Texas MD Anderson Cancer Center (Houston, TX, USA). Patients with haematological cancers aged between 5 and 75 years were eligible to participate in the study. Patients who had HIV or uncontrollable infections were excluded. Eligible patients were randomly assigned (1:1 by a computer-generated programme in block sizes of four) to receive a total intravenous busulfan dose to achieve an area under the curve of 16 000 μmol/min (16K group) or 20 000 μmol/min (20K group) on the basis of pharmacokinetic analysis, plus intravenous fludarabine 40 mg/m
FINDINGS: Between April 18, 2012, and Dec 9, 2015, 98 patients were enrolled. 49 patients were randomly assigned to the 16K group and 49 to the 20K group, one of which was removed from the study before starting the intervention. Median age was 60 years (IQR 54-67). 50 (52%) patients had an HCT-specific comorbidity index score of 3 or more, and 41 (42%) had a high or very high Disease Risk Index score. Day 100 non-relapse mortality was 4% (95% CI 0-10) in the 16K group and 6% (0-13) in the 20K group (p=0·65). Infection was the most common grade 3-5 toxicity in both the 20K group (25 [52%] of 48 patients) and the 16K group (24 [49%] of 49 participants). Mucositis (nine [19%] of 48 patients vs three [6%] of 49 patients), idiopathic pneumonia syndrome (nine [19%] of 48 patients vs two [4%] of 49 patients), and culture-negative neutropenic fever (16 [33%] of 48 patients vs eight [16%] of 49 patients) were more common in the 20K group than in the 16K group.
INTERPRETATION: Myeloablative doses of busulfan administered in a timed-sequential manner with fludarabine is associated with low non-relapse mortality in older patients and patients with comorbidities. Additional studies are required to show whether this approach can reduce the risk of relapse.
FUNDING: Cancer Center Support Grant (US National Cancer Institute, National Institutes of Health).
METHODS: This non-stratified, open-label, randomised phase 2 trial was done at The University of Texas MD Anderson Cancer Center (Houston, TX, USA). Patients with haematological cancers aged between 5 and 75 years were eligible to participate in the study. Patients who had HIV or uncontrollable infections were excluded. Eligible patients were randomly assigned (1:1 by a computer-generated programme in block sizes of four) to receive a total intravenous busulfan dose to achieve an area under the curve of 16 000 μmol/min (16K group) or 20 000 μmol/min (20K group) on the basis of pharmacokinetic analysis, plus intravenous fludarabine 40 mg/m
FINDINGS: Between April 18, 2012, and Dec 9, 2015, 98 patients were enrolled. 49 patients were randomly assigned to the 16K group and 49 to the 20K group, one of which was removed from the study before starting the intervention. Median age was 60 years (IQR 54-67). 50 (52%) patients had an HCT-specific comorbidity index score of 3 or more, and 41 (42%) had a high or very high Disease Risk Index score. Day 100 non-relapse mortality was 4% (95% CI 0-10) in the 16K group and 6% (0-13) in the 20K group (p=0·65). Infection was the most common grade 3-5 toxicity in both the 20K group (25 [52%] of 48 patients) and the 16K group (24 [49%] of 49 participants). Mucositis (nine [19%] of 48 patients vs three [6%] of 49 patients), idiopathic pneumonia syndrome (nine [19%] of 48 patients vs two [4%] of 49 patients), and culture-negative neutropenic fever (16 [33%] of 48 patients vs eight [16%] of 49 patients) were more common in the 20K group than in the 16K group.
INTERPRETATION: Myeloablative doses of busulfan administered in a timed-sequential manner with fludarabine is associated with low non-relapse mortality in older patients and patients with comorbidities. Additional studies are required to show whether this approach can reduce the risk of relapse.
FUNDING: Cancer Center Support Grant (US National Cancer Institute, National Institutes of Health).
Poręba M, Gać P, Usnarska-Zubkiewicz L, et al.
Evaluation of the impact of treatment with hematopoietic stem cells transplantation (HSCT) on biochemical markers of heart function and novel electrocardiographic markers of repolarization in patients with hematological malignancies.
Med Oncol. 2018; 35(12):162 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
Evaluation of the impact of treatment with hematopoietic stem cells transplantation (HSCT) on biochemical markers of heart function and novel electrocardiographic markers of repolarization in patients with hematological malignancies.
Med Oncol. 2018; 35(12):162 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
High-dose chemotherapy (HDC) followed by stem cell transplantation (HSCT) is a well-established method in patients with hematological malignancies, and for last few years, many efforts have been made to estimate short- and long-term efficacy of this method, as well as early and late complications. The present study concentrates on cardiotoxic effects, mainly early changes using biochemical markers such as N-terminal natriuretic peptide type B (NT-proBNP) and cardiac troponins (cTn). Simultaneously, the analysis of 12-lead ECG was done before and after the procedure in which the novel repolarization markers: T
Luo W, Yu H, Zou X, et al.
Long non-coding RNA taurine-upregulated gene 1 correlates with unfavorable prognosis in patients with refractory or relapsed acute myeloid leukemia treated by purine analogue based chemotherapy regimens.
Cancer Biomark. 2018; 23(4):485-494 [PubMed] Related Publications
Long non-coding RNA taurine-upregulated gene 1 correlates with unfavorable prognosis in patients with refractory or relapsed acute myeloid leukemia treated by purine analogue based chemotherapy regimens.
Cancer Biomark. 2018; 23(4):485-494 [PubMed] Related Publications
OBJECTIVE: This study aimed to explore the correlation of long non-coding RNA taurine-upregulated gene 1 (lncRNA TUG1) expression with clinicopathological features and its predictive value for treatment response and survival profiles in refractory or relapsed acute myeloid leukemia (R/R AML) patients.
METHODS: Seventy three R/R AML patients who received cladribine combined with cytarabine and granulocyte colony-stimulating factor (G-CSF) (CLAG) or fludarabine combined with cytarabine and G-CSF (FLAG) based chemotherapy and 37 non-malignant controls were recruited. LncRNA TUG1 expression was detected in bone marrow sample obtained before treatment. Complete response (CR), partial response (PR), overall response rate (ORR) and overall survival (OS) were evaluated.
RESULTS: LncRNA TUG1 expression was upregulated in R/R AML patients compared to controls. It was also elevated in R/R AML patients with age ⩾ 60 years (vs. age < 60 years, P= 0.030) and in patients with secondary AML (vs. primary AML, P= 0.035). R/R AML patients with lncRNA TUG1 high expression achieved numerically lower CR (P= 0.053), decreased ORR (P= 0.028) and shorter OS (P< 0.001) than patients with lncRNA TUG1 low expression. Univariate logistic regression and COX's regression disclosed that lncRNA TUG1 high expression correlated with declined ORR, numerically decreased CR, and reduced OS. Furthermore, multivariate analyses verified that lncRNA TUG1 high expression was an independent predictive factor for decreased ORR and worse OS.
CONCLUSIONS: In conclusion, lncRNA TUG1 expression was elevated in R/R AML patients, and it might serve as a potential biomarker for poor prognosis in R/R AML patients treated with CLAG or FLAG based chemotherapy.
METHODS: Seventy three R/R AML patients who received cladribine combined with cytarabine and granulocyte colony-stimulating factor (G-CSF) (CLAG) or fludarabine combined with cytarabine and G-CSF (FLAG) based chemotherapy and 37 non-malignant controls were recruited. LncRNA TUG1 expression was detected in bone marrow sample obtained before treatment. Complete response (CR), partial response (PR), overall response rate (ORR) and overall survival (OS) were evaluated.
RESULTS: LncRNA TUG1 expression was upregulated in R/R AML patients compared to controls. It was also elevated in R/R AML patients with age ⩾ 60 years (vs. age < 60 years, P= 0.030) and in patients with secondary AML (vs. primary AML, P= 0.035). R/R AML patients with lncRNA TUG1 high expression achieved numerically lower CR (P= 0.053), decreased ORR (P= 0.028) and shorter OS (P< 0.001) than patients with lncRNA TUG1 low expression. Univariate logistic regression and COX's regression disclosed that lncRNA TUG1 high expression correlated with declined ORR, numerically decreased CR, and reduced OS. Furthermore, multivariate analyses verified that lncRNA TUG1 high expression was an independent predictive factor for decreased ORR and worse OS.
CONCLUSIONS: In conclusion, lncRNA TUG1 expression was elevated in R/R AML patients, and it might serve as a potential biomarker for poor prognosis in R/R AML patients treated with CLAG or FLAG based chemotherapy.
Knecht KM, Buzovetsky O, Schneider C, et al.
The structural basis for cancer drug interactions with the catalytic and allosteric sites of SAMHD1.
Proc Natl Acad Sci U S A. 2018; 115(43):E10022-E10031 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
The structural basis for cancer drug interactions with the catalytic and allosteric sites of SAMHD1.
Proc Natl Acad Sci U S A. 2018; 115(43):E10022-E10031 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
SAMHD1 is a deoxynucleoside triphosphate triphosphohydrolase (dNTPase) that depletes cellular dNTPs in noncycling cells to promote genome stability and to inhibit retroviral and herpes viral replication. In addition to being substrates, cellular nucleotides also allosterically regulate SAMHD1 activity. Recently, it was shown that high expression levels of SAMHD1 are also correlated with significantly worse patient responses to nucleotide analog drugs important for treating a variety of cancers, including acute myeloid leukemia (AML). In this study, we used biochemical, structural, and cellular methods to examine the interactions of various cancer drugs with SAMHD1. We found that both the catalytic and the allosteric sites of SAMHD1 are sensitive to sugar modifications of the nucleotide analogs, with the allosteric site being significantly more restrictive. We crystallized cladribine-TP, clofarabine-TP, fludarabine-TP, vidarabine-TP, cytarabine-TP, and gemcitabine-TP in the catalytic pocket of SAMHD1. We found that all of these drugs are substrates of SAMHD1 and that the efficacy of most of these drugs is affected by SAMHD1 activity. Of the nucleotide analogs tested, only cladribine-TP with a deoxyribose sugar efficiently induced the catalytically active SAMHD1 tetramer. Together, these results establish a detailed framework for understanding the substrate specificity and allosteric activation of SAMHD1 with regard to nucleotide analogs, which can be used to improve current cancer and antiviral therapies.
Thebo U, Millett RL, Elkon J, Haroun F
Two distinct histological Richter's transformations 23 years apart in a patient with chronic lymphocytic leukaemia.
BMJ Case Rep. 2018; 2018 [PubMed] Related Publications
Two distinct histological Richter's transformations 23 years apart in a patient with chronic lymphocytic leukaemia.
BMJ Case Rep. 2018; 2018 [PubMed] Related Publications
A 53-year-old man with a 1-year history of chronic lymphocytic leukaemia (CLL) presented with a left bicep mass. Biopsy and staging workup revealed Richter's transformation (RT) Ann Arbor stage 1E diffuse large B-cell lymphoma in the bicep. The patient was treated with combination chemotherapy with cyclophosphamide, doxorubicin, Vincristine and prednisone followed by site radiation and did well thereafter. His CLL progressed and required treatment on two more occasions 11 and 18 years after his initial diagnosis with fludarabine, Cytoxan and Rituxan and then with bendamustine and rituximab. 23 years after initial presentation, he developed diffuse lymphadenopathy and B-symptoms. A biopsy of an enlarged cervical lymph node demonstrated only CLL for which he was started on ibrutinib. Treatment was shortly discontinued thereafter due to intolerance and worsening symptoms. A second biopsy was performed which revealed concurrent CLL and Hodgkin's lymphoma representing a second and histologically distinct RT.
Jamy O, Bae S, Costa LJ, et al.
Outcomes of fludarabine, high dose cytarabine and granulocyte-colony stimulating factor (FLAG) as re-induction for residual acute myeloid leukemia on day 14 bone marrow.
Leuk Res. 2018; 74:64-67 [PubMed] Related Publications
Outcomes of fludarabine, high dose cytarabine and granulocyte-colony stimulating factor (FLAG) as re-induction for residual acute myeloid leukemia on day 14 bone marrow.
Leuk Res. 2018; 74:64-67 [PubMed] Related Publications
BACKGROUND: Patients with acute myeloid leukemia (AML) treated with intensive chemotherapy may require re-induction based on the evaluation of day 14 bone marrow biopsy.
METHODS: A retrospective chart review was performed to evaluate adult patients with AML who received re-induction with fludarabine, high dose cytarabine and granulocyte colony stimulating factor (FLAG) regimen for residual disease (≥ 5% blasts by morphology) on day 14 bone marrow examination between September 2012 and July 2017 at our institution.
RESULTS: We identified 27 patients who received FLAG therapy for treatment of residual disease on day 14 marrow examination following initial induction. The median age at diagnosis was 61 years and the majority of patients had poor risk AML. The overall response rate was 78% and 15 patients proceeded to allogeneic hematopoietic stem cell transplantation.
CONCLUSION: The regimen was well tolerated and is a viable re-induction option for patients with residual disease on a day 14 bone marrow.
METHODS: A retrospective chart review was performed to evaluate adult patients with AML who received re-induction with fludarabine, high dose cytarabine and granulocyte colony stimulating factor (FLAG) regimen for residual disease (≥ 5% blasts by morphology) on day 14 bone marrow examination between September 2012 and July 2017 at our institution.
RESULTS: We identified 27 patients who received FLAG therapy for treatment of residual disease on day 14 marrow examination following initial induction. The median age at diagnosis was 61 years and the majority of patients had poor risk AML. The overall response rate was 78% and 15 patients proceeded to allogeneic hematopoietic stem cell transplantation.
CONCLUSION: The regimen was well tolerated and is a viable re-induction option for patients with residual disease on a day 14 bone marrow.
Xu J, Lv TT, Zhou XF, et al.
Efficacy of common salvage chemotherapy regimens in patients with refractory or relapsed acute myeloid leukemia: A retrospective cohort study.
Medicine (Baltimore). 2018; 97(39):e12102 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
Efficacy of common salvage chemotherapy regimens in patients with refractory or relapsed acute myeloid leukemia: A retrospective cohort study.
Medicine (Baltimore). 2018; 97(39):e12102 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
To assess treatment response and overall survival (OS) in refractory or relapsed acute myeloid leukemia (R/R AML) patients treated by different common salvage chemotherapy regimens.Medical records data from 142 R/R AML patients were reviewed in this retrospective study. Patients were treated with regimens based on the following drugs: cytarabine, granulocyte colony-stimulating factor (G-CSF), and fludarabine (FLAG) (n = 46); cytarabine and G-CSF in addition to aclarubicin or daunorubicin (CAG/DAG) (n = 30); cytarabine, G-CSF, and cladribine (CLAG) (n = 27); cytarabine, etoposide, and mitoxantrone (MEA) (n = 17); cytarabine plus idarubicin, daunorubicin, or mitoxantrone (IA/DA/MA) (n = 12); and homoharringtonine, cytarabine, and aclarubicin or daunorubicin (HAA/HAD) (n = 10).A total of 43 (35.2%) patients achieved complete remission (CR), 60 (49.2%) patients achieved overall remission rate (ORR), and 18 (14.8%) patients received allogeneic hematopoietic stem cell transplantation (allo-HSCT) after CR. Median OS was 8.0 (95% CI 6.6-9.4) months with a 1-year OS rate of (29.9 ± 3.9)% and 3-year OS rate of (11.1 ± 3.6)%. No difference of CR (P = .621), ORR (P = .385), and allo-HSCT (P = .537) achievement was observed among different chemotherapy regimens. Interestingly, we observed that the CLAG-based regimen did not affect CR (P = .165), while it achieved a numerically higher ORR (P = .093) and was an independent factor for prolonged OS (P = .016). No other regimens were determined to be correlated with CR, ORR, or OS.FLAG-, CAG/DAG-, CLAG-, MEA-, IA/DA/MA- and HAA/HAD-based regimens were found to achieve similar CR rates, while the CLAG-based regimen achieved numerically higher ORR rates and significant favorable OS. Therefore, CLAG-based regimens should be a prioritized treatment option for R/R AML patients.
Gao RW, Weisdorf DJ, DeFor TE, et al.
Influence of Total Body Irradiation Dose Rate on Idiopathic Pneumonia Syndrome in Acute Leukemia Patients Undergoing Allogeneic Hematopoietic Cell Transplantation.
Int J Radiat Oncol Biol Phys. 2019; 103(1):180-189 [PubMed] Related Publications
Influence of Total Body Irradiation Dose Rate on Idiopathic Pneumonia Syndrome in Acute Leukemia Patients Undergoing Allogeneic Hematopoietic Cell Transplantation.
Int J Radiat Oncol Biol Phys. 2019; 103(1):180-189 [PubMed] Related Publications
PURPOSE: To determine the relationship between dose rate and other factors in the development of idiopathic pneumonia syndrome (IPS) in patients with acute lymphoblastic leukemia or acute myeloid leukemia who are undergoing total body irradiation (TBI)-based myeloablative conditioning for allogeneic hematopoietic cell transplantation (HCT).
METHODS AND MATERIALS: From 2006 to 2016, 202 patients with acute leukemia (111 acute lymphoblastic leukemia, 91 acute myeloid leukemia) ranging in age from 1 to 57 years (median, 25 years) underwent allogeneic HCT at University of Minnesota. Pretransplantation conditioning included cyclophosphamide (120 mg/kg) with (68%) or without fludarabine (75 mg/m
RESULTS: IPS developed in 42 patients (21%) between 4 and 73 days (median, 16 days) after transplantation. HDR TBI was associated with a higher rate of IPS compared with LDR TBI (29% vs 10%; P < .01). On multiple regression analysis, HDR remained a significant predictor of IPS (hazard ratio, 2.6; 95% confidence interval, 1.2-5.3; P = .01), and this led to inferior 1-year overall survival (60% vs 76%; P = .01) and increased 1-year nonrelapse mortality (28% vs 15%; P = .02).
CONCLUSIONS: TBI dose rates ≤15 cGy/min reduce the risk of posttransplantation IPS and improve overall survival. LDR TBI should be strongly considered as an easily implemented parameter to improve the safety of pretransplantation TBI-based conditioning.
METHODS AND MATERIALS: From 2006 to 2016, 202 patients with acute leukemia (111 acute lymphoblastic leukemia, 91 acute myeloid leukemia) ranging in age from 1 to 57 years (median, 25 years) underwent allogeneic HCT at University of Minnesota. Pretransplantation conditioning included cyclophosphamide (120 mg/kg) with (68%) or without fludarabine (75 mg/m
RESULTS: IPS developed in 42 patients (21%) between 4 and 73 days (median, 16 days) after transplantation. HDR TBI was associated with a higher rate of IPS compared with LDR TBI (29% vs 10%; P < .01). On multiple regression analysis, HDR remained a significant predictor of IPS (hazard ratio, 2.6; 95% confidence interval, 1.2-5.3; P = .01), and this led to inferior 1-year overall survival (60% vs 76%; P = .01) and increased 1-year nonrelapse mortality (28% vs 15%; P = .02).
CONCLUSIONS: TBI dose rates ≤15 cGy/min reduce the risk of posttransplantation IPS and improve overall survival. LDR TBI should be strongly considered as an easily implemented parameter to improve the safety of pretransplantation TBI-based conditioning.
Eapen M, Brazauskas R, Hemmer M, et al.
Hematopoietic cell transplant for acute myeloid leukemia and myelodysplastic syndrome: conditioning regimen intensity.
Blood Adv. 2018; 2(16):2095-2103 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
Hematopoietic cell transplant for acute myeloid leukemia and myelodysplastic syndrome: conditioning regimen intensity.
Blood Adv. 2018; 2(16):2095-2103 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
In this study, we sought to identify specific individual high-intensity or reduced-intensity conditioning regimens with the best relapse-free survival (RFS) rather than the global high- vs reduced-intensity regimen comparison. Patients (median age, 58 years) with acute myeloid leukemia (AML; n = 1258), who were in first or subsequent remission, or with MDS (n = 951) who had refractory anemia with unilineage or multilineage dysplasia, 5q- syndrome, or refractory anemia with excess blasts received nonirradiation-containing regimens and were transplanted between 2009 and 2014 in the United States. Three-year RFS with high-intensity busulfan/cyclophosphamide (Bu4/Cy; 44%) was comparable to conditioning with high-intensity fludarabine/busulfan (Flu/Bu4; 44%), reduced-intensity fludarabine/melphalan (Flu/Mel; 52%;
Robak T, Burger JA, Tedeschi A, et al.
Single-agent ibrutinib versus chemoimmunotherapy regimens for treatment-naïve patients with chronic lymphocytic leukemia: A cross-trial comparison of phase 3 studies.
Am J Hematol. 2018; 93(11):1402-1410 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
Single-agent ibrutinib versus chemoimmunotherapy regimens for treatment-naïve patients with chronic lymphocytic leukemia: A cross-trial comparison of phase 3 studies.
Am J Hematol. 2018; 93(11):1402-1410 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
Chemoimmunotherapy (CIT) and targeted therapy with single-agent ibrutinib are both recommended first-line treatments for chronic lymphocytic leukemia (CLL), although their outcomes have not been directly compared. Using ibrutinib data from the RESONATE-2 (PCYC-1115/1116) study conducted in patients ≥65 years without del(17p), we performed a cross-trial comparison with CIT data from published phase 3 studies in first-line treatment of CLL. Progression-free survival (PFS), overall survival (OS), and safety data for ibrutinib (median follow-up 35.7 months) were evaluated alongside available CIT data. CIT regimens included: fludarabine + cyclophosphamide + rituximab (CLL8, CLL10), bendamustine + rituximab (CLL10), obinutuzumab + chlorambucil and rituximab + chlorambucil (CLL11), and ofatumumab + chlorambucil (COMPLEMENT-1). Median age across studies was 61-74 years, with older populations receiving ibrutinib, obinutuzumab + chlorambucil, or rituximab + chlorambucil. Median follow-up varied across studies/regimens (range 14.5-37.4 months). Among all patients, PFS appeared longer with ibrutinib relative to CIT and OS appeared comparable. Relative to CIT studies that similarly excluded patients with del(17p) (CLL10) or enrolled older/less-fit patients (CLL11), PFS appeared favorable for ibrutinib in high-risk subgroups, including advanced disease, bulky lymph nodes, unmutated IGHV status, and presence of del(11q). Grade ≥ 3 infections ranged from 9% (ofatumumab + chlorambucil) to 40% (fludarabine + cyclophosphamide + rituximab), and was 25% with ibrutinib. Grade ≥ 3 neutropenia was 12% for ibrutinib and 26%-84% for CIT. Although definitive conclusions cannot be made due to inherent limitations of cross-trial comparisons, this report suggests that ibrutinib has a favorable benefit/risk profile and may potentially eliminate the need for chemotherapy in some patients. Randomized, comparative studies are needed to support these findings.
Franiak-Pietryga I, Ostrowska K, Maciejewski H, et al.
Affecting NF-κB cell signaling pathway in chronic lymphocytic leukemia by dendrimers-based nanoparticles.
Toxicol Appl Pharmacol. 2018; 357:33-38 [PubMed] Related Publications
Affecting NF-κB cell signaling pathway in chronic lymphocytic leukemia by dendrimers-based nanoparticles.
Toxicol Appl Pharmacol. 2018; 357:33-38 [PubMed] Related Publications
The complex genetic diversity of chronic lymphocytic leukemia (CLL) makes it difficult to determine the effective and durable therapy beneficial to patients. During the several past years' significant insights in the biology of the disease and its treatment have been made, allowing for the identification of promising novel therapeutic agents. The investigation of signaling pathways to understand the biological character of CLL together with the development of molecular profiling is key in personalized approach in therapy for this disease. As it was already proven, maltotriose (M3) modified fourth generation poly(propylene imine) dendrimers (PPI-G4) modulate BCR, TRAIL and WNT signaling pathway gene expression in CLL cells and strongly influence their survival by inducing apoptosis and inhibiting proliferation. The aim of this study was to evaluate the influence of PPI-G4-M3 dendrimers on NFκB pathway gene expression in CLL (MEC-1) cells with 60 K microarray, as it is one of the major factors in the pathogenesis of B-cell neoplasms. The findings were compared with those obtained with Fludarabine (FA) and the results indicate that PPI-G4-M3 dendrimers affect the expression of the examined genes and exert comparable effect on the CLL cells to FA. Dendrimers are one of the most potent groups of nanometer-sized macromolecules for closing the gap between the present ineffective treatment and the future effective personalized therapy due to their potential versatile biological properties.
Anderson E, Mehta P, Heywood J, et al.
CPX-351 exhibits hENT-independent uptake and can be potentiated by fludarabine in leukaemic cells lines and primary refractory AML.
Leuk Res. 2018; 74:121-129 [PubMed] Related Publications
CPX-351 exhibits hENT-independent uptake and can be potentiated by fludarabine in leukaemic cells lines and primary refractory AML.
Leuk Res. 2018; 74:121-129 [PubMed] Related Publications
CPX-351, a liposomal formulation co-encapsulating cytarabine and daunorubicin (DNR) in a synergistic 5:1 M ratio, has shown favourable response in newly diagnosed elderly high-risk AML. This study assessed intracellular ara-CTP levels following in vitro exposure of human immortalised leukaemic cell lines and primary AML blasts to CPX-351, and investigated fludarabine potentiation of intracellular ara-CTP formation from CPX-351. Comparison of intracellular handling of CPX-351 to cytarabine in HL-60 cells indicated slower conversion to ara-CTP for CPX-351, but equivalent cytotoxicity to cytarabine and combined DNR/cytarabine (DA) at 48 h, mostly likely reflecting the need for intracellular liposome processing to release encapsulated drugs. Further assessment demonstrated cytotoxicity of CPX-351 to be superior to DA at 48 and 72 h in cytarabine-resistant THP-1 cells (p < 0.001), and this effect could not be inhibited upon blockade of human equilibrative nucleoside transporter (hENT) function with dipyridamole. Assessment of Flu-CPX in primary blasts from presentation AML patients (n = 5) demonstrated a more rapid and pronounced potentiation of ara-CTP from CPX-351 than in immortalised cell lines, with 4/5 patients showing significant increases in ara-CTP, notably for those that went on to fail induction and relapse treatment in vivo (n = 3). This suggests a favourable impact on patient outcome from Flu-CPX.
Cerna K, Oppelt J, Chochola V, et al.
MicroRNA miR-34a downregulates FOXP1 during DNA damage response to limit BCR signalling in chronic lymphocytic leukaemia B cells.
Leukemia. 2019; 33(2):403-414 [PubMed] Related Publications
MicroRNA miR-34a downregulates FOXP1 during DNA damage response to limit BCR signalling in chronic lymphocytic leukaemia B cells.
Leukemia. 2019; 33(2):403-414 [PubMed] Related Publications
The variable clinical course in chronic lymphocytic leukaemia (CLL) largely depends on p53 functionality and B-cell receptor (BCR) signalling propensity; however, it is unclear if there is any crosstalk between these pathways. We show that DNA damage response (DDR) activation leads to down-modulating the transcriptional factor FOXP1, which functions as a positive BCR signalling regulator and its high levels are associated with worse CLL prognosis. We identified microRNA (miRNA) miR-34a as the most prominently upregulated miRNA during DDR in CLL cells in vitro and in vivo during FCR therapy (fludarabine, cyclophosphamide, rituximab). MiR-34a induced by DDR activation and p53 stabilization potently represses FOXP1 expression by binding in its 3'-UTR. The low FOXP1 levels limit BCR signalling partially via derepressing BCR-inhibitory molecule CD22. We also show that low miR-34a levels can be used as a biomarker for worse response or shorter progression free survival in CLL patients treated with FCR chemoimmunotherapy, and shorter overall survival, irrespective of TP53 status. Additionally, we have developed a method for the absolute quantification of miR-34a copies and defined precise prognostic/predictive cutoffs. Overall, herein, we reveal for the first time that B cells limit their BCR signalling during DDR by down-modulating FOXP1 via DDR-p53/miR-34a axis.
Saraceni F, Beohou E, Labopin M, et al.
Thiotepa, busulfan and fludarabine compared to busulfan and cyclophosphamide as conditioning regimen for allogeneic stem cell transplant from matched siblings and unrelated donors for acute myeloid leukemia.
Am J Hematol. 2018; 93(10):1211-1219 [PubMed] Related Publications
Thiotepa, busulfan and fludarabine compared to busulfan and cyclophosphamide as conditioning regimen for allogeneic stem cell transplant from matched siblings and unrelated donors for acute myeloid leukemia.
Am J Hematol. 2018; 93(10):1211-1219 [PubMed] Related Publications
Busulfan plus cyclophosphamide (BuCy) is the traditional conditioning regimen for allogeneic stem cell transplant (allo-SCT) for young, fit patients with acute myeloid leukemia (AML). The thiotepa-busulfan-fludarabine (TBF) protocol has recently demonstrated promising outcome in cord blood and haploidentical SCT; however, there is limited evidence about this regimen in transplant from matched siblings (MSD) and unrelated donors (UD). We retrospectively compared outcomes of 2523 patients aged 18-50 with AML in remission, undergoing transplant from MSD or UD prepared with either TBF or BuCy conditioning. A 1:3 pair-matched analysis was performed: 146 patients receiving TBF were compared with 438 patients receiving BuCy. Relapse risk was significantly lower in the TBF when compared with BuCy group (HR 0.6, P = .02), while NRM did not differ. No significant difference was observed in LFS and OS between the two regimens. TBF was associated with a trend towards higher risk of grades III-IV aGVHD (HR 1.8, P = .06) and inferior cGVHD (HR 0.7, P = .04) when compared with BuCy. In patients undergoing transplant in first remission, the advantage for TBF in terms of relapse was more evident (HR 0.4, P = .02), leading to a trend for better LFS in favor of TBF (HR 0.7, P = .10), while OS did not differ between the two cohorts. In conclusion, TBF represents a valid myeloablative conditioning regimen providing significantly lower relapse and similar survival when compared with BuCy. Patients in first remission appear to gain the most from this protocol, as in this subgroup a tendency for better LFS was observed when compared with BuCy.
Byrd JC, Ruppert AS, Heerema NA, et al.
Lenalidomide consolidation benefits patients with CLL receiving chemoimmunotherapy: results for CALGB 10404 (Alliance).
Blood Adv. 2018; 2(14):1705-1718 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
Lenalidomide consolidation benefits patients with CLL receiving chemoimmunotherapy: results for CALGB 10404 (Alliance).
Blood Adv. 2018; 2(14):1705-1718 [PubMed] Article available free on PMC after 01/11/2019 Related Publications
Prior to novel targeted agents for chronic lymphocytic leukemia (CLL), the best chemoimmunotherapy regimen in patients with non-del(11q) disease was unclear. The role of lenalidomide was also not defined. This phase 2 study randomized 342 untreated patients with non-del(11q) CLL requiring therapy to fludarabine plus rituximab (FR; n = 123), FR plus lenalidomide consolidation (FR+L; n = 109), or FR plus cyclophosphamide (FCR; n = 110) and compared 2-year progression-free survival (PFS) rates of each to the historical control rate with FC (60%). Patients with del(11q) in at least 20% of pretreatment cells continued with FCR (n = 27) or were reassigned to FCR+L (n = 31) and excluded from the primary analysis. Among non-del(11q) patients, 2-year PFS rates were 64% (90% confidence interval [CI], 57-71; FR), 72% (90% CI, 65-79; FR+L), and 74% (90% CI, 66-80; FCR); FR+L and FCR had rates significantly greater than historical control. Median PFS was significantly shorter with FR compared with FR+L (


 Cyclophosphamide
Cyclophosphamide