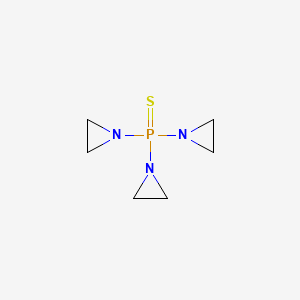
Thiotepa
"A very toxic alkylating antineoplastic agent also used as an insect sterilant. It causes skin, gastrointestinal, CNS, and bone marrow damage. According to the Fourth Annual Report on Carcinogens (NTP 85-002, 1985), thiotepa may reasonably be anticipated to be a carcinogen (Merck Index, 11th ed)." (MeSH 2013)
Found this page useful?
 Web Resources: Thiotepa
Web Resources: Thiotepa Latest Research Publications
Latest Research PublicationsWeb Resources: Thiotepa (6 links)
Cancer Research UK
Macmillan Cancer Support
NHS Evidence
PubChem
Irish Cancer Society
MedlinePlus
Latest Research Publications
This list of publications is regularly updated (Source: PubMed).
Yen HJ, Yu TY, Lee CY, et al.
The impact on outcomes by using thiotepa in tandem transplant for pediatric high-risk embryonal brain tumors.
J Chin Med Assoc. 2019; 82(2):148-154 [PubMed] Related Publications
The impact on outcomes by using thiotepa in tandem transplant for pediatric high-risk embryonal brain tumors.
J Chin Med Assoc. 2019; 82(2):148-154 [PubMed] Related Publications
BACKGROUND: Despite aggressive treatment including surgery, radiotherapy, and adjuvant chemotherapy, the outcome of pediatric high-risk embryonal brain tumors remains poor; especially in young children, in whom early radiotherapy inevitably brings significant long-term morbidities. Single or tandem autologous stem cell transplant has been reported to improve outcomes; but optimal use is not well defined.
METHODS: Pediatric patients with high-risk embryonal brain tumors who underwent tandem transplant as consolidation from August 2011 to December 2017 were included. We performed a retrospective chart review and analyzed the outcomes to identify possible prognostic factors.
RESULTS: Eleven pediatric patients with high-risk embryonal brain tumors were enrolled. They received double or triple autologous transplant at complete response in 5 patients and at partial response in 6 for a total of 24 transplants. There were five atypical teratoid rhabdoid tumors, four medulloblastoma, one primitive neuroectodermal tumors, and one pineoblastoma. Median age at diagnosis was 1.8 years (range, 0.6-11.2 years) and at transplant was 2.2 years (range, 1.2-11.9 years). Thiotepa-based regimens were used in 13 cycles of conditioning. All patients achieved successful engraftment. No transplant-related mortality was identified. With a median follow-up of 21.2 months (range, 6.9-51.8 months), seven patients had disease progression. Disease entity and the use of one or more cycles of thiotepa-based regimen during tandem transplant had statistically significant impact on both progression-free survival and overall survival.
CONCLUSION: With successful engraftment and manageable toxicity, tandem transplant in pediatric patients with high-risk embryonal brain tumor is feasible and safe. Patients receiving tandem transplant with one or more cycles of thiotepa-based regimen might have better outcome than those without. In combination with salvage radiotherapy, a favorable 2-year overall survival could be achieved in the majority of patients.
METHODS: Pediatric patients with high-risk embryonal brain tumors who underwent tandem transplant as consolidation from August 2011 to December 2017 were included. We performed a retrospective chart review and analyzed the outcomes to identify possible prognostic factors.
RESULTS: Eleven pediatric patients with high-risk embryonal brain tumors were enrolled. They received double or triple autologous transplant at complete response in 5 patients and at partial response in 6 for a total of 24 transplants. There were five atypical teratoid rhabdoid tumors, four medulloblastoma, one primitive neuroectodermal tumors, and one pineoblastoma. Median age at diagnosis was 1.8 years (range, 0.6-11.2 years) and at transplant was 2.2 years (range, 1.2-11.9 years). Thiotepa-based regimens were used in 13 cycles of conditioning. All patients achieved successful engraftment. No transplant-related mortality was identified. With a median follow-up of 21.2 months (range, 6.9-51.8 months), seven patients had disease progression. Disease entity and the use of one or more cycles of thiotepa-based regimen during tandem transplant had statistically significant impact on both progression-free survival and overall survival.
CONCLUSION: With successful engraftment and manageable toxicity, tandem transplant in pediatric patients with high-risk embryonal brain tumor is feasible and safe. Patients receiving tandem transplant with one or more cycles of thiotepa-based regimen might have better outcome than those without. In combination with salvage radiotherapy, a favorable 2-year overall survival could be achieved in the majority of patients.
Van Schandevyl G, Bauters T
Thiotepa-induced cutaneous toxicity in pediatric patients: Case report and implementation of preventive care guidelines.
J Oncol Pharm Pract. 2019; 25(3):689-693 [PubMed] Related Publications
Thiotepa-induced cutaneous toxicity in pediatric patients: Case report and implementation of preventive care guidelines.
J Oncol Pharm Pract. 2019; 25(3):689-693 [PubMed] Related Publications
Thiotepa, a highly lipophilic, alkylating agent, and/or its active metabolites may be excreted in part via skin in patients receiving high-dose therapy. We present a case of cutaneous toxicity observed in a 4.5-year-old girl patient with medulloblastoma treated with a high-dose thiotepa conditioning regimen before autologous stem cell transplantation. Skin lesions, as well as their pattern and locations, were evocative of thiotepa toxidermia. After the case herein described, preventive care guidelines were implemented in our unit as from 2014. A retrospective follow-up of 26 pediatric patients receiving thiotepa prior to stem cell transplantation was performed until March 2018. In this series of patients, only one patient experienced cutaneous toxicity as reported herein. Thereafter, only mild cutaneous toxicity was observed, even with double or triple transplantation protocols with high-dose thiotepa. Clear preventive care instructions should be detailed in the Summary of Product Characteristics in order to minimize the cutaneous toxicity of thiotepa.
Saraceni F, Beohou E, Labopin M, et al.
Thiotepa, busulfan and fludarabine compared to busulfan and cyclophosphamide as conditioning regimen for allogeneic stem cell transplant from matched siblings and unrelated donors for acute myeloid leukemia.
Am J Hematol. 2018; 93(10):1211-1219 [PubMed] Related Publications
Thiotepa, busulfan and fludarabine compared to busulfan and cyclophosphamide as conditioning regimen for allogeneic stem cell transplant from matched siblings and unrelated donors for acute myeloid leukemia.
Am J Hematol. 2018; 93(10):1211-1219 [PubMed] Related Publications
Busulfan plus cyclophosphamide (BuCy) is the traditional conditioning regimen for allogeneic stem cell transplant (allo-SCT) for young, fit patients with acute myeloid leukemia (AML). The thiotepa-busulfan-fludarabine (TBF) protocol has recently demonstrated promising outcome in cord blood and haploidentical SCT; however, there is limited evidence about this regimen in transplant from matched siblings (MSD) and unrelated donors (UD). We retrospectively compared outcomes of 2523 patients aged 18-50 with AML in remission, undergoing transplant from MSD or UD prepared with either TBF or BuCy conditioning. A 1:3 pair-matched analysis was performed: 146 patients receiving TBF were compared with 438 patients receiving BuCy. Relapse risk was significantly lower in the TBF when compared with BuCy group (HR 0.6, P = .02), while NRM did not differ. No significant difference was observed in LFS and OS between the two regimens. TBF was associated with a trend towards higher risk of grades III-IV aGVHD (HR 1.8, P = .06) and inferior cGVHD (HR 0.7, P = .04) when compared with BuCy. In patients undergoing transplant in first remission, the advantage for TBF in terms of relapse was more evident (HR 0.4, P = .02), leading to a trend for better LFS in favor of TBF (HR 0.7, P = .10), while OS did not differ between the two cohorts. In conclusion, TBF represents a valid myeloablative conditioning regimen providing significantly lower relapse and similar survival when compared with BuCy. Patients in first remission appear to gain the most from this protocol, as in this subgroup a tendency for better LFS was observed when compared with BuCy.
Sharma P, Pollyea DA, Smith CA, et al.
Thiotepa-Based Intensified Reduced-Intensity Conditioning Adult Double-Unit Cord Blood Hematopoietic Stem Cell Transplantation Results in Decreased Relapse Rate and Improved Survival Compared with Transplantation Following Standard Reduced-Intensity Conditioning: A Retrospective Cohort Comparison.
Biol Blood Marrow Transplant. 2018; 24(8):1671-1677 [PubMed] Related Publications
Thiotepa-Based Intensified Reduced-Intensity Conditioning Adult Double-Unit Cord Blood Hematopoietic Stem Cell Transplantation Results in Decreased Relapse Rate and Improved Survival Compared with Transplantation Following Standard Reduced-Intensity Conditioning: A Retrospective Cohort Comparison.
Biol Blood Marrow Transplant. 2018; 24(8):1671-1677 [PubMed] Related Publications
The "Minnesota" reduced-intensity conditioning (RIC) cord blood transplantation (CBT) regimen (standard RIC) of fludarabine (Flu) (200 mg/m
Scordo M, Morjaria SM, Littmann ER, et al.
Distinctive Infectious Complications in Patients with Central Nervous System Lymphoma Undergoing Thiotepa, Busulfan, and Cyclophosphamide-conditioned Autologous Stem Cell Transplantation.
Biol Blood Marrow Transplant. 2018; 24(9):1914-1919 [PubMed] Free Access to Full Article Related Publications
Distinctive Infectious Complications in Patients with Central Nervous System Lymphoma Undergoing Thiotepa, Busulfan, and Cyclophosphamide-conditioned Autologous Stem Cell Transplantation.
Biol Blood Marrow Transplant. 2018; 24(9):1914-1919 [PubMed] Free Access to Full Article Related Publications
We investigated the incidence of viral, fungal, bacterial, and parasitic infections observed in 57 patients with central nervous system lymphoma after thiotepa, busulfan, and cyclophosphamide-conditioned autologous stem cell transplantation (TBC-ASCT) and 79 patients with systemic non-Hodgkin lymphoma after traditional carmustine, etoposide, cytarabine, and melphalan-conditioned ASCT (BEAM-ASCT). Twenty of 57 (35%) TBC-ASCT patients had detectable viremia with human herpesvirus 6, cytomegalovirus, adenovirus, or BK virus, versus 9 of 79 (11%) BEAM-ASCT patients. Eight TBC-ASCT patients had clinically relevant viral infections (4 human herpesvirus 6, 2 cytomegalovirus, 1 adenovirus, 2 BK virus), versus 0 in the BEAM-ASCT group. Four TBC-ASCT patients suffered infections from either a fungal or parasitic pathogen versus 1 BEAM-ASCT patient. TBC was associated with greater risk of viral reactivation compared with BEAM, independent of other factors (hazard ratio, 4.42; 95% confidence interval, 1.9 to 11.3; P < .001). Prolonged lymphopenia and steroid use in the peri- and post-ASCT period did not explain these observed differences. The pathogenesis of these unusual infections in TBC-ASCT patients remains incompletely understood, and may involve more potent immune suppression with TBC conditioning. Clinicians should be aware of these differences in infection risk in TBC-ASCT patients, which more closely parallel those seen in allogenic hematopoietic cell transplantation recipients. New prophylactic approaches to help minimize these infections should be considered in this population.
El-Cheikh J, Massoud R, Moukalled N, et al.
Thiotepa 10 mg/kg Treatment Regimen Is Superior to Thiotepa 5 mg/kg in TBF Conditioning in Patients Undergoing Allogeneic Stem-Cell Transplantation.
Clin Lymphoma Myeloma Leuk. 2018; 18(5):368-374 [PubMed] Related Publications
Thiotepa 10 mg/kg Treatment Regimen Is Superior to Thiotepa 5 mg/kg in TBF Conditioning in Patients Undergoing Allogeneic Stem-Cell Transplantation.
Clin Lymphoma Myeloma Leuk. 2018; 18(5):368-374 [PubMed] Related Publications
INTRODUCTION: The optimal intensity of myeloablation with a reduced-toxicity conditioning regimen to decrease relapse rate after allogeneic stem-cell transplantation without increasing transplant-related mortality (TRM) has not been well established.
MATERIALS AND METHODS: We compared outcomes between 5 mg/kg (T5) and 10 mg/kg (T10) thiotepa-based conditioning regimens in 29 adults who underwent allogeneic stem-cell transplantation for hematologic malignancies.
RESULTS: After a median follow-up of 11 months, TRM was 0% and 14% at 100 days and 1 year, respectively, with TRM observed only in the T5 group (P = .016). The relapse incidence at 1 year was 20%. No patient had disease in first complete remission at the time of transplantation. At 1 year, progression-free and overall survival were 30% versus 87% (P = .012) and 46% versus 87% (P = .008) in the T5 and T10 groups, respectively. In univariate and multivariate analysis, only age at transplantation and total dose of thiotepa had a significant impact on TRM, overall, and progression-free survival.
CONCLUSION: Patients deemed fit to receive T10-based conditioning for allogeneic stem-cell transplantation to treat high-risk hematologic malignancies had better overall and progression-free survival than those who received T5 with no additional toxicities. Patients should be stratified before conditioning, and those judged fit should receive T10, while the others should consider alternative reduced-intensity conditioning regimens.
MATERIALS AND METHODS: We compared outcomes between 5 mg/kg (T5) and 10 mg/kg (T10) thiotepa-based conditioning regimens in 29 adults who underwent allogeneic stem-cell transplantation for hematologic malignancies.
RESULTS: After a median follow-up of 11 months, TRM was 0% and 14% at 100 days and 1 year, respectively, with TRM observed only in the T5 group (P = .016). The relapse incidence at 1 year was 20%. No patient had disease in first complete remission at the time of transplantation. At 1 year, progression-free and overall survival were 30% versus 87% (P = .012) and 46% versus 87% (P = .008) in the T5 and T10 groups, respectively. In univariate and multivariate analysis, only age at transplantation and total dose of thiotepa had a significant impact on TRM, overall, and progression-free survival.
CONCLUSION: Patients deemed fit to receive T10-based conditioning for allogeneic stem-cell transplantation to treat high-risk hematologic malignancies had better overall and progression-free survival than those who received T5 with no additional toxicities. Patients should be stratified before conditioning, and those judged fit should receive T10, while the others should consider alternative reduced-intensity conditioning regimens.
Maritaz C, Lemare F, Laplanche A, et al.
High-dose thiotepa-related neurotoxicity and the role of tramadol in children.
BMC Cancer. 2018; 18(1):177 [PubMed] Free Access to Full Article Related Publications
High-dose thiotepa-related neurotoxicity and the role of tramadol in children.
BMC Cancer. 2018; 18(1):177 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Serious neurological adverse events (NAE) have occurred during treatment with high-dose thiotepa regimens of children with high-risk solid tumours. The objective was to assess the incidence of NAE related to high-dose thiotepa and to identify potential contributing factors that could exacerbate the occurrence of this neurotoxicity.
METHODS: From May 1987 to March 2011, children with solid tumours treated with high-dose thiotepa were retrospectively identified. Each NAE detected led to an independent case analysis. Potential contributing factors were pre-specified and univariate/multivariable analyses were performed.
RESULTS: Three hundred seven courses of thiotepa (251 patients) were identified. The total dose per treatment ranged from 600 to 900 mg/m
CONCLUSIONS: The incidence of neurotoxicity was 18.3%. Brain tumours and tramadol treatment are risk factors to consider when using high-dose thiotepa. The outcome of patients was favourable without sequelae in all cases and rechallenge with thiotepa was possible.
METHODS: From May 1987 to March 2011, children with solid tumours treated with high-dose thiotepa were retrospectively identified. Each NAE detected led to an independent case analysis. Potential contributing factors were pre-specified and univariate/multivariable analyses were performed.
RESULTS: Three hundred seven courses of thiotepa (251 patients) were identified. The total dose per treatment ranged from 600 to 900 mg/m
CONCLUSIONS: The incidence of neurotoxicity was 18.3%. Brain tumours and tramadol treatment are risk factors to consider when using high-dose thiotepa. The outcome of patients was favourable without sequelae in all cases and rechallenge with thiotepa was possible.
Duléry R, Ménard AL, Chantepie S, et al.
Sequential Conditioning with Thiotepa in T Cell- Replete Hematopoietic Stem Cell Transplantation for the Treatment of Refractory Hematologic Malignancies: Comparison with Matched Related, Haplo-Mismatched, and Unrelated Donors.
Biol Blood Marrow Transplant. 2018; 24(5):1013-1021 [PubMed] Related Publications
Sequential Conditioning with Thiotepa in T Cell- Replete Hematopoietic Stem Cell Transplantation for the Treatment of Refractory Hematologic Malignancies: Comparison with Matched Related, Haplo-Mismatched, and Unrelated Donors.
Biol Blood Marrow Transplant. 2018; 24(5):1013-1021 [PubMed] Related Publications
The results of conventional allogeneic stem cell transplantation (SCT) in refractory hematologic malignancies are poor. Sequential strategies have shown promising results in refractory acute myelogenous leukemia (AML), but have not been validated in a haploidentical (Haplo) transplant setting. We have developed a new sequential approach combining chemotherapy with broad antitumor activity (thiotepa 10 mg/kg, etoposide 400 mg/m
Joffe E, Rosenberg D, Rozovski U, et al.
Replacing carmustine by thiotepa and cyclophosphamide for autologous stem cell transplantation in Hodgkin's and non-Hodgkin's B-cell lymphoma.
Bone Marrow Transplant. 2018; 53(1):29-33 [PubMed] Related Publications
Replacing carmustine by thiotepa and cyclophosphamide for autologous stem cell transplantation in Hodgkin's and non-Hodgkin's B-cell lymphoma.
Bone Marrow Transplant. 2018; 53(1):29-33 [PubMed] Related Publications
This study aimed to compare the real-life results of TECAM, a thiotepa-based conditioning regimen consisting of thiotepa (40 mg/m
Osorio DS, Dunkel IJ, Cervone KA, et al.
Tandem thiotepa with autologous hematopoietic cell rescue in patients with recurrent, refractory, or poor prognosis solid tumor malignancies.
Pediatr Blood Cancer. 2018; 65(1) [PubMed] Related Publications
Tandem thiotepa with autologous hematopoietic cell rescue in patients with recurrent, refractory, or poor prognosis solid tumor malignancies.
Pediatr Blood Cancer. 2018; 65(1) [PubMed] Related Publications
BACKGROUND: The purpose of this study was to determine the feasibility and tolerability of tandem courses of high-dose thiotepa with autologous hematopoietic cell rescue (AHCR) in patients with recurrent, refractory solid tumors who were ineligible for a single course of high-dose therapy due to greater than minimal residual disease. Patients with decreased hearing or poor renal function were eligible.
PROCEDURE: Thiotepa was administered intravenously at a dose of 200 mg/m
RESULTS: Fifty-eight patients received 96 courses. Thirty-eight (65%) patients received two courses of therapy. Twenty-seven courses (28%) were administered completely in the outpatient setting. A toxic mortality rate of 3.4% was observed. Five of 26 patients with medulloblastoma were alive at a median of 35 months, whereas 21 patients died at a median of 11.7 months. Four of five patients with central nervous system germ cell tumors (CNS GCT) were alive 68-103 months following AHCR.
CONCLUSIONS: Two cycles of high-dose thiotepa with AHCR were well tolerated even in these heavily pretreated patients. This therapy may provide prolonged survival in patients with recurrent malignant brain tumors, particularly medulloblastoma and CNS GCT.
PROCEDURE: Thiotepa was administered intravenously at a dose of 200 mg/m
RESULTS: Fifty-eight patients received 96 courses. Thirty-eight (65%) patients received two courses of therapy. Twenty-seven courses (28%) were administered completely in the outpatient setting. A toxic mortality rate of 3.4% was observed. Five of 26 patients with medulloblastoma were alive at a median of 35 months, whereas 21 patients died at a median of 11.7 months. Four of five patients with central nervous system germ cell tumors (CNS GCT) were alive 68-103 months following AHCR.
CONCLUSIONS: Two cycles of high-dose thiotepa with AHCR were well tolerated even in these heavily pretreated patients. This therapy may provide prolonged survival in patients with recurrent malignant brain tumors, particularly medulloblastoma and CNS GCT.
Eder S, Canaani J, Beohou E, et al.
Thiotepa-based conditioning versus total body irradiation as myeloablative conditioning prior to allogeneic stem cell transplantation for acute lymphoblastic leukemia: A matched-pair analysis from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation.
Am J Hematol. 2017; 92(10):997-1003 [PubMed] Related Publications
Thiotepa-based conditioning versus total body irradiation as myeloablative conditioning prior to allogeneic stem cell transplantation for acute lymphoblastic leukemia: A matched-pair analysis from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation.
Am J Hematol. 2017; 92(10):997-1003 [PubMed] Related Publications
The optimal conditioning regimen to employ before hematopoietic stem cell transplantation in acute lymphoblastic leukemia (ALL) is still undecided, and while cyclophosphamide/total body irradiation (Cy/TBI) is the most commonly used myeloablative regimen, there are concerns regarding long-term toxicity for patients conditioned with this regimen. Thiotepa-based conditioning is an emerging radiation-free regimen with recent publications indicative of comparable clinical outcomes to TBI-based conditioning. In this analysis of the acute leukemia working party of the EBMT, we performed a retrospective matched-pair analysis, evaluating the outcome of adult patients with ALL who received thiotepa-based conditioning (n = 180) with those receiving Cy/TBI conditioning (n = 540). The 2-year leukemia-free survival and overall survival (OS) rates of both conditioning regimens were comparable, 33% for thiotepa [95% confidence interval (CI): 26.4-42.8] versus 39% for Cy/TBI (95% CI: 34.8-44.5] (P = .33) and 46.5% [95% CI: 38.6-56.1] versus 48.8% [95% CI: 44.2-54] (P = .9), respectively. There was no significant difference between the two regimens in the incidence of either acute graft versus host disease (GVHD) or chronic GVHD. Multivariate analysis demonstrated increased relapse incidence for thiotepa conditioning compared to Cy/TBI (HR = 1.78, 95% CI, 1.07-2.95; P = .03) which did not affect OS. Our results indicate that thiotepa-based conditioning may not be inferior to Cy/TBI for adult patients with ALL.
Schorb E, Fox CP, Fritsch K, et al.
High-dose thiotepa-based chemotherapy with autologous stem cell support in elderly patients with primary central nervous system lymphoma: a European retrospective study.
Bone Marrow Transplant. 2017; 52(8):1113-1119 [PubMed] Related Publications
High-dose thiotepa-based chemotherapy with autologous stem cell support in elderly patients with primary central nervous system lymphoma: a European retrospective study.
Bone Marrow Transplant. 2017; 52(8):1113-1119 [PubMed] Related Publications
In this retrospective multicentre study, we investigated the outcomes of elderly primary central nervous system lymphoma (PCNSL) patients (⩾65 years) who underwent high-dose chemotherapy followed by autologous stem cell transplantation (HDT-ASCT) at 11 centres between 2003 and 2016. End points included remission, progression-free survival (PFS), overall survival (OS) and treatment-related mortality. We identified 52 patients (median age 68.5 years, median Karnofsky Performance Status before HDT-ASCT 80%) who all underwent thiotepa-based HDT-ASCT. Fifteen patients (28.8%) received HDT-ASCT as first-line treatment and 37 (71.2%) received it as second or subsequent line. Remission status before HDT-ASCT was: CR 34.6%, PR 51.9%, stable disease 3.8% and progressive disease 9.6%. Following completion of HDT-ASCT, 36 patients (69.2%) achieved CR (21.2% first-line setting and 48.1% second or subsequent line setting) and 9 (17.3%) PR (5.8% first-line setting and 11.5% second or subsequent line setting). With a median follow-up of 22 months after HDT-ASCT, median PFS and OS were reached after 51.1 and 122.3 months, respectively. The 2-year PFS and OS rates were 62.0% and 70.8%, respectively. We observed two HDT-ASCT-associated deaths (3.8%). In selected elderly PCNSL patients, HDT-ASCT, using thiotepa-based conditioning regimes, is feasible and effective. Further prospective and comparative studies are warranted to further evaluate the role of HDT-ASCT in elderly PCNSL patients.
Eder S, Beohou E, Labopin M, et al.
Thiotepa-based conditioning for allogeneic stem cell transplantation in acute lymphoblastic leukemia-A survey from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation.
Am J Hematol. 2017; 92(1):18-22 [PubMed] Related Publications
Thiotepa-based conditioning for allogeneic stem cell transplantation in acute lymphoblastic leukemia-A survey from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation.
Am J Hematol. 2017; 92(1):18-22 [PubMed] Related Publications
In this study, we analyzed a thiotepa-based conditioning regimen for allogeneic stem cell transplantation in adults with acute lymphoblastic leukemia, using the EBMT database. A total of 323 patients were identified. The median age was 43 years. Disease status at transplant was first complete remission (CR1) in 48.9%, CR2 in 21.7%, CR3 in 6.2%, while 23.2% of the patients had an active disease at the time of transplant. This was performed from a HLA-matched sibling (49.8%) or a matched-unrelated donor (51.2%). The incidence of acute graft-vs.-host disease (GvHD) (grade > II) was 26.6%, while chronic GvHD occurred in 35.9% of the patients at 1 year (24.6% with extensive disease). With a median follow-up of 16.8 months, the nonrelapse mortality was 12.4 and 25.3% at 100 days and 1 year, respectively. The relapse incidence at 1 year was 33.3% with no difference for patients in CR1 (27%). The one-year leukemia-free survival (LFS) and overall survival (OS) were 57 and 66%, respectively for the entire cohort and 50 and 66%, respectively in patients in CR1. Thiotepa/busulfan ± melphalan (n = 213) in comparison to thiotepa/other (n = 110) conditioning regimen resulted in higher relapse incidence at 1 year (34.9 vs. 30.3%, P = 0.016) and lower LFS (38.8 vs. 45.9%, P = 0.0203), while nonrelapse mortality (23.8 vs. 26.3%, n.s.) and OS (59.6 vs. 51.1%, P = 0.109) did not differ. This large study suggests that a thiotepa-based conditioning for allogeneic transplantation in acute lymphoblastic leukemia is feasible and effective, with the main outcomes being comparable to those achieved with other regimens. Am. J. Hematol. 92:18-22, 2017. © 2016 Wiley Periodicals, Inc.
Eder S, Labopin M, Finke J, et al.
Safety and efficacy of thiotepa-based conditioning for allogeneic transplantation in AML: a survey from the ALWP of the EBMT.
Bone Marrow Transplant. 2017; 52(2):238-244 [PubMed] Related Publications
Safety and efficacy of thiotepa-based conditioning for allogeneic transplantation in AML: a survey from the ALWP of the EBMT.
Bone Marrow Transplant. 2017; 52(2):238-244 [PubMed] Related Publications
This study evaluated the safety and efficacy of thiotepa-based regimens before allogeneic stem cell transplantation in 310 adult patients with AML. Disease status at the time of transplantation was CR1 in 50%, CR2+ in 23.5% and advanced disease in 26.5%. Transplantation was performed from haploidentical (35%), matched sibling (27%), unrelated (20%) or cord blood (18%) donors. As for safety: mucositis occurred in 46.8% of the patients and the cumulative incidence (CI) of sinusoidal obstruction syndrome was 4.0%. With a median follow-up of 37 months, the CI of acute GvHD grade>II was 26.5%, whereas CI of chronic GvHD was 28.1% at 3 years. CI for non-relapse mortality at 3 years was 38.4%, 49.7% and 45.4% for patients in CR1, CR2+ and advanced disease, respectively (P=0.10). Relapse incidence at 3 years was 20.2, 30.7 and 40.6% in these three respective groups (P=0.002). CI for 3-year leukemia-free survival and overall survival were 41.4% and 45.6% (CR1), 19.6% and 27.7% (CR2+), and 13.9% and 13.6% (advanced disease), respectively (P<10
Ferreri AJ, Cwynarski K, Pulczynski E, et al.
Chemoimmunotherapy with methotrexate, cytarabine, thiotepa, and rituximab (MATRix regimen) in patients with primary CNS lymphoma: results of the first randomisation of the International Extranodal Lymphoma Study Group-32 (IELSG32) phase 2 trial.
Lancet Haematol. 2016; 3(5):e217-27 [PubMed] Related Publications
Chemoimmunotherapy with methotrexate, cytarabine, thiotepa, and rituximab (MATRix regimen) in patients with primary CNS lymphoma: results of the first randomisation of the International Extranodal Lymphoma Study Group-32 (IELSG32) phase 2 trial.
Lancet Haematol. 2016; 3(5):e217-27 [PubMed] Related Publications
BACKGROUND: Standard treatment for patients with primary CNS lymphoma remains to be defined. Active therapies are often associated with increased risk of haematological or neurological toxicity. In this trial, we addressed the tolerability and efficacy of adding rituximab with or without thiotepa to methotrexate-cytarabine combination therapy (the MATRix regimen), followed by a second randomisation comparing consolidation with whole-brain radiotherapy or autologous stem cell transplantation in patients with primary CNS lymphoma. We report the results of the first randomisation in this Article.
METHODS: For the international randomised phase 2 International Extranodal Lymphoma Study Group-32 (IELSG32) trial, HIV-negative patients (aged 18-70 years) with newly diagnosed primary CNS lymphoma and measurable disease were enrolled from 53 cancer centres in five European countries (Denmark, Germany, Italy, Switzerland, and the UK) and randomly assigned (1:1:1) to receive four courses of methotrexate 3·5 g/m(2) on day 1 plus cytarabine 2 g/m(2) twice daily on days 2 and 3 (group A); or the same combination plus two doses of rituximab 375 mg/m(2) on days -5 and 0 (group B); or the same methotrexate-cytarabine-rituximab combination plus thiotepa 30 mg/m(2) on day 4 (group C), with the three groups repeating treatment every 3 weeks. Patients with responsive or stable disease after the first stage were then randomly allocated between whole-brain radiotherapy and autologous stem cell transplantation. A permuted blocks randomised design (block size four) was used for both randomisations, and a computer-generated randomisation list was used within each stratum to preserve allocation concealment. Randomisation was stratified by IELSG risk score (low vs intermediate vs high). No masking after assignment to intervention was used. The primary endpoint of the first randomisation was the complete remission rate, analysed by modified intention to treat. This study is registered with ClinicalTrials.gov, number NCT01011920.
FINDINGS: Between Feb 19, 2010, and Aug 27, 2014, 227 eligible patients were recruited. 219 of these 227 enrolled patients were assessable. At median follow-up of 30 months (IQR 22-38), patients treated with rituximab and thiotepa had a complete remission rate of 49% (95% CI 38-60), compared with 23% (14-31) of those treated with methotrexate-cytarabine alone (hazard ratio 0·46, 95% CI 0·28-0·74) and 30% (21-42) of those treated with methotrexate-cytarabine plus rituximab (0·61, 0·40-0·94). Grade 4 haematological toxicity was more frequent in patients treated with methotrexate-cytarabine plus rituximab and thiotepa, but infective complications were similar in the three groups. The most common grade 3-4 adverse events in all three groups were neutropenia, thrombocytopenia, anaemia, and febrile neutropenia or infections. 13 (6%) patients died of toxicity.
INTERPRETATION: With the limitations of a randomised phase 2 study design, the IELSG32 trial provides a high level of evidence supporting the use of MATRix combination as the new standard chemoimmunotherapy for patients aged up to 70 years with newly diagnosed primary CNS lymphoma and as the control group for future randomised trials.
FUNDING: Associazione Italiana del Farmaco, Cancer Research UK, Oncosuisse, and Swiss National Foundation.
METHODS: For the international randomised phase 2 International Extranodal Lymphoma Study Group-32 (IELSG32) trial, HIV-negative patients (aged 18-70 years) with newly diagnosed primary CNS lymphoma and measurable disease were enrolled from 53 cancer centres in five European countries (Denmark, Germany, Italy, Switzerland, and the UK) and randomly assigned (1:1:1) to receive four courses of methotrexate 3·5 g/m(2) on day 1 plus cytarabine 2 g/m(2) twice daily on days 2 and 3 (group A); or the same combination plus two doses of rituximab 375 mg/m(2) on days -5 and 0 (group B); or the same methotrexate-cytarabine-rituximab combination plus thiotepa 30 mg/m(2) on day 4 (group C), with the three groups repeating treatment every 3 weeks. Patients with responsive or stable disease after the first stage were then randomly allocated between whole-brain radiotherapy and autologous stem cell transplantation. A permuted blocks randomised design (block size four) was used for both randomisations, and a computer-generated randomisation list was used within each stratum to preserve allocation concealment. Randomisation was stratified by IELSG risk score (low vs intermediate vs high). No masking after assignment to intervention was used. The primary endpoint of the first randomisation was the complete remission rate, analysed by modified intention to treat. This study is registered with ClinicalTrials.gov, number NCT01011920.
FINDINGS: Between Feb 19, 2010, and Aug 27, 2014, 227 eligible patients were recruited. 219 of these 227 enrolled patients were assessable. At median follow-up of 30 months (IQR 22-38), patients treated with rituximab and thiotepa had a complete remission rate of 49% (95% CI 38-60), compared with 23% (14-31) of those treated with methotrexate-cytarabine alone (hazard ratio 0·46, 95% CI 0·28-0·74) and 30% (21-42) of those treated with methotrexate-cytarabine plus rituximab (0·61, 0·40-0·94). Grade 4 haematological toxicity was more frequent in patients treated with methotrexate-cytarabine plus rituximab and thiotepa, but infective complications were similar in the three groups. The most common grade 3-4 adverse events in all three groups were neutropenia, thrombocytopenia, anaemia, and febrile neutropenia or infections. 13 (6%) patients died of toxicity.
INTERPRETATION: With the limitations of a randomised phase 2 study design, the IELSG32 trial provides a high level of evidence supporting the use of MATRix combination as the new standard chemoimmunotherapy for patients aged up to 70 years with newly diagnosed primary CNS lymphoma and as the control group for future randomised trials.
FUNDING: Associazione Italiana del Farmaco, Cancer Research UK, Oncosuisse, and Swiss National Foundation.
Song Q, Zhou X, Yu J, et al.
The prognostic values of CYP2B6 genetic polymorphisms and metastatic sites for advanced breast cancer patients treated with docetaxel and thiotepa.
Sci Rep. 2015; 5:16775 [PubMed] Free Access to Full Article Related Publications
The prognostic values of CYP2B6 genetic polymorphisms and metastatic sites for advanced breast cancer patients treated with docetaxel and thiotepa.
Sci Rep. 2015; 5:16775 [PubMed] Free Access to Full Article Related Publications
This study investigated interactive effects of CYP2B6 genotypes and liver metastasis on the prognosis of metastatic breast cancer patients who received combined chemotherapy of docetaxel and thiotepa. Totally 153 patients were retrospectively genotyped rs8192719 (c.1294 + 53C > T) and rs2279343 (c.785A > G). Kaplan-Meier method and Cox Proportional Hazard Regression model were used to estimate the survival. Patients with liver metastasis had worsen prognosis, conferring a 2.26-fold high risk of progression and 1.93-fold high risk of death (p < 0.05). Both CT/TT genotype of rs8192719 (c.1294 + 3C > T) and AG genotype of rs2279343 (c.785A > G) prolonged survival (p < 0.05). Furthermore, among liver metastatic patients, AG genotype of rs2279343 (c.785A > G) was associated with a 47% reduced risk of death and a 6-month-longer overall survival (p < 0.05). Among non-liver metastatic patients, hazard ratios of CT/TT genotype of rs8192719 (c.1294 + 53C > T) were 0.45 for progression and 0.40 for death; and the corresponding survival was improved by 6 months and 16 months, respectively (p < 0.05). Genotypes of CYP2B6 had an interaction with clinical efficacy of docetaxel and thiotepa on metastatic breast cancer patients; and metastatic sites also affected clinical responses. Further therapies should take into account of chemotherapy regimen, genotypes of metabolizing enzymes and metastatic sites for the particular subpopulation.
Sellner L, Boumendil A, Finel H, et al.
Thiotepa-based high-dose therapy for autologous stem cell transplantation in lymphoma: a retrospective study from the EBMT.
Bone Marrow Transplant. 2016; 51(2):212-8 [PubMed] Related Publications
Thiotepa-based high-dose therapy for autologous stem cell transplantation in lymphoma: a retrospective study from the EBMT.
Bone Marrow Transplant. 2016; 51(2):212-8 [PubMed] Related Publications
Clinical information about thiotepa-based autologous stem cell transplantation (auto-SCT) outside the primary central nervous system lymphoma (PCNSL) field is sparse. In this registry-based retrospective study, we evaluated potential risks and benefits of thiotepa-based preparative regimens compared with BEAM (carmustine, etoposide, cytarabine, melphalan) in auto-SCT for diffuse large B-cell lymphoma (DLBCL, excluding PCNSL), follicular lymphoma (FL) or Hodgkin lymphoma (HL). A total of 14 544 patients (589 thiotepa and 13 955 BEAM) met the eligibility criteria, and 535 thiotepa- and 1031 BEAM-treated patients were matched in a 1:2 ratio for final comparison. No significant differences between thiotepa and BEAM groups for any survival end point were identified in the whole sample or disease entity subsets. For a more detailed analysis, 47 TEAM (thiotepa, etoposide, cytarabine, melphalan)-treated patients were compared with 75 matched BEAM patients with additional collection of toxicity data. Again, there were no significant differences between the two groups for any survival end point. In addition, the frequency of common infectious and non-infectious complications including secondary malignancies was comparable between TEAM and BEAM. These results indicate that thiotepa-based high-dose therapy might be a valuable alternative to BEAM in DLBCL, HL and FL. Further evaluation by prospective clinical trials is warranted.
Cho KM, Kim YJ, Kim SH, et al.
Salvage Treatment with Intracerebrospinal Fluid Thiotepa in Patients with Leptomeningeal Metastasis After Failure of Methotrexate-based Treatment.
Anticancer Res. 2015; 35(10):5631-8 [PubMed] Related Publications
Salvage Treatment with Intracerebrospinal Fluid Thiotepa in Patients with Leptomeningeal Metastasis After Failure of Methotrexate-based Treatment.
Anticancer Res. 2015; 35(10):5631-8 [PubMed] Related Publications
AIM: To evaluate the efficacy of intracerebrospinal fluid (intra-CSF) thiotepa in patients with leptomeningeal metastasis (LM) after failure of a methotrexate-based treatment.
PATIENTS AND METHODS: We retrospectively reviewed the medical records of patients with LM who received 10 mg of intra-CSF thiotepa twice a week.
RESULTS: Out of 40 patients, 25 were females (63%), and 31 (78%) had an Eastern Cooperative Oncology Group performance status (ECOG PS) ≥2. Fourteen out of the 30 evaluable patients (47%) had a cytological response to intra-CSF thiotepa. The median overall survival (OS) after treatment with thiotepa was 19.4 weeks (95% confidence interval (CI)=15.3-23.5). Grade 3 toxicities were thrombocytopenia (N=2), bacterial meningitis (N=2), and pneumonia (N=1). According to a multivariate analysis, an ECOG PS ≥2 (hazard ratio (HR)=5.11, 95% CI=1.39-18.80, p=0.014), clinical improvement (HR=0.09, 95% CI=0.03-0.29, p<0.001), and radiation for LM after intra-CSF thiotepa (HR=0.33, 95% CI=0.11-0.97, p=0.043) were independently associated with survival.
CONCLUSION: Intra-CSF thiotepa seems to be a meaningful salvage treatment for patients with LM whose disease progresses after a methotrexate-based treatment.
PATIENTS AND METHODS: We retrospectively reviewed the medical records of patients with LM who received 10 mg of intra-CSF thiotepa twice a week.
RESULTS: Out of 40 patients, 25 were females (63%), and 31 (78%) had an Eastern Cooperative Oncology Group performance status (ECOG PS) ≥2. Fourteen out of the 30 evaluable patients (47%) had a cytological response to intra-CSF thiotepa. The median overall survival (OS) after treatment with thiotepa was 19.4 weeks (95% confidence interval (CI)=15.3-23.5). Grade 3 toxicities were thrombocytopenia (N=2), bacterial meningitis (N=2), and pneumonia (N=1). According to a multivariate analysis, an ECOG PS ≥2 (hazard ratio (HR)=5.11, 95% CI=1.39-18.80, p=0.014), clinical improvement (HR=0.09, 95% CI=0.03-0.29, p<0.001), and radiation for LM after intra-CSF thiotepa (HR=0.33, 95% CI=0.11-0.97, p=0.043) were independently associated with survival.
CONCLUSION: Intra-CSF thiotepa seems to be a meaningful salvage treatment for patients with LM whose disease progresses after a methotrexate-based treatment.
Zhou X, Wang X, Song Q, et al.
Transformation of alkylating regimen of thiotepa into tepa determines the disease progression through GSTP1 gene polymorphism for metastatic breast cancer patients receiving thiotepa containing salvage chemotherapy.
Int J Clin Pharmacol Ther. 2015; 53(11):914-22 [PubMed] Related Publications
Transformation of alkylating regimen of thiotepa into tepa determines the disease progression through GSTP1 gene polymorphism for metastatic breast cancer patients receiving thiotepa containing salvage chemotherapy.
Int J Clin Pharmacol Ther. 2015; 53(11):914-22 [PubMed] Related Publications
BACKGROUND: The shifts to second-line chemotherapy for metastatic breast cancer (MBC) were widely required based on pharmaceutical molecular profiles to reach out precision medicine. The emerging precise treatment of cancer requires the implementation of clarified pharmacogenetic profiles which are capable of elucidating the predictive responses to cancer chemotherapy. Therefore we were interested in the analysis of the roles of single nucleotide polymorphism (SNP) of GSTP1 (glutathione S-transferase pi 1 gene) alleles to identify pharmacological links with predictors of clinical responses and toxicities.
METHODS: 93 MBC patients receiving thiotepa plus docetaxel chemotherapy were enrolled in this study. Optimized CYP3A5, CYP2B6, and GSTP1 were predominantly selected as candidate genes and their three SNPs (CYP2B6 G516T, CYP3A5 A6986G, and GSTP1 A313G) were genotyped by matrix-assisted laser desorption ionization/time of flight (MALDI-TOF) mass spectrometry. Progression-free survival (PFS), disease control rate, and chemo-related toxicities were recorded.
RESULTS: GSTP1 A313G (rs1695) was identified to be related with disease progression. In particular, patients harboring AG/GG genotype demonstrated a statistically longer PFS than those with AA. Multivariate analysis confirmed that AG/GG genotype was associated with both clinical responses and liver-localized metastatic lesions. No correlation was found between these three SNPs and chemotherapy-induced toxicity.
CONCLUSIONS: These results suggest that the GSTP1 polymorphism is a novel prognostic marker for clinical response to thiotepa-containing chemotherapy regimens. Such evidence could provide insight into the role of pharmacogenetics to deprive of biases in shifting regimens solely by empirical choices.
METHODS: 93 MBC patients receiving thiotepa plus docetaxel chemotherapy were enrolled in this study. Optimized CYP3A5, CYP2B6, and GSTP1 were predominantly selected as candidate genes and their three SNPs (CYP2B6 G516T, CYP3A5 A6986G, and GSTP1 A313G) were genotyped by matrix-assisted laser desorption ionization/time of flight (MALDI-TOF) mass spectrometry. Progression-free survival (PFS), disease control rate, and chemo-related toxicities were recorded.
RESULTS: GSTP1 A313G (rs1695) was identified to be related with disease progression. In particular, patients harboring AG/GG genotype demonstrated a statistically longer PFS than those with AA. Multivariate analysis confirmed that AG/GG genotype was associated with both clinical responses and liver-localized metastatic lesions. No correlation was found between these three SNPs and chemotherapy-induced toxicity.
CONCLUSIONS: These results suggest that the GSTP1 polymorphism is a novel prognostic marker for clinical response to thiotepa-containing chemotherapy regimens. Such evidence could provide insight into the role of pharmacogenetics to deprive of biases in shifting regimens solely by empirical choices.
Jahnukainen K, Kallio P, Koivusalo A, Saarinen-Pihkala UM
High-dose Thiotepa as Consolidation Therapy With Autologous Hematopoietic Stem Cell Transplantation for High-risk Ewing Family Tumors: Single-institution Experience.
J Pediatr Hematol Oncol. 2015; 37(7):536-42 [PubMed] Related Publications
High-dose Thiotepa as Consolidation Therapy With Autologous Hematopoietic Stem Cell Transplantation for High-risk Ewing Family Tumors: Single-institution Experience.
J Pediatr Hematol Oncol. 2015; 37(7):536-42 [PubMed] Related Publications
High-dose therapy (HDTx) with autologous stem cell rescue has been widely applied in very-poor-risk pediatric solid tumors. Promising data have become available with the use of high-dose busulfan, whereas high-dose (HD) thiotepa is less commonly used. We report retrospectively our single-institution experience from 1986 to 2012 of single and tandem HDTx with special emphasis on HD-thiotepa as the backbone of HD regimen in Ewing family tumors, including all 24 patients in the Helsinki University Hospital referral area in population-based fashion (Ewing sarcoma 9, Askin tumor 9, peripheral neuroectodermal tumor 6). The 10-year overall survival for the entire cohort was 0.73±0.01. Thirteen out of the 24 underwent HDTx (10 single, 3 tandem). The HDTx regimen consisted of HD-thiotepa (900 mg/m), VP16, and carboplatin. Additional HD-melphalan and total body irradiation were used in the tandem regimens. There was no toxic mortality. The 5-year event-free survival was 0.73±0.16 for high-risk cases transplanted in 1CR. In the relapse group, 1 out of the 3 survived. Radiotherapy to axial sites was given safely in combination with HD-thiotepa in all 3 patients. Thiotepa-based HDTx approach resulted in an encouraging outcome without toxic mortality for high-risk patients. HD-thiotepa merits further studies in larger controlled series.
Musso M, Messina G, Marcacci G, et al.
High-Dose Melphalan Plus Thiotepa as Conditioning Regimen before Second Autologous Stem Cell Transplantation for "De Novo" Multiple Myeloma Patients: A Phase II Study.
Biol Blood Marrow Transplant. 2015; 21(11):1932-8 [PubMed] Related Publications
High-Dose Melphalan Plus Thiotepa as Conditioning Regimen before Second Autologous Stem Cell Transplantation for "De Novo" Multiple Myeloma Patients: A Phase II Study.
Biol Blood Marrow Transplant. 2015; 21(11):1932-8 [PubMed] Related Publications
High-dose melphalan (MEL) is the standard therapy for autologous stem cell transplantation (ASCT) in multiple myeloma (MM), although the optimal conditioning regimen remains yet to be identified. Thiotepa (THIO) appears to be a potentially effective option, with broad-spectrum antitumor efficacy that can be added to myeloablative multiagent regimens for ASCT in hematopoietic tumors. We conducted a phase II trial, adding THIO (275 mg/m(2)) to high-dose MEL (140 mg/m(2)) before a second ASCT, in a tandem ASCT strategy, in 64 patients with "de novo" MM. Overall, there was no transplant-related mortality. The incidence of neutropenic fever and mucositis (grades 3 to 4) was 39% and 9%, respectively. Median number of days to neutrophil and platelet engraftment were 11 and 12, respectively. After the second transplantation, the complete response improved to 43.8%. Overall response rate was 86%. After a median follow-up of 18.1 months, 13 patients had progressed and 3 died from MM. Median progression-free survival was not reached, and actuarial 2-year rates of progression-free and overall survival were 71% and 88.9%, respectively. Our results suggest that THIO/MEL is a feasible and safe conditioning regimen for ASCT in MM and should be explored for efficacy in a phase III study.
Chahal J, Stopeck A, Clarke K, et al.
Intravenous thiotepa for treatment of breast cancer-related leptomeningeal carcinomatosis: case series.
Neurol Sci. 2015; 36(9):1691-3 [PubMed] Related Publications
Intravenous thiotepa for treatment of breast cancer-related leptomeningeal carcinomatosis: case series.
Neurol Sci. 2015; 36(9):1691-3 [PubMed] Related Publications
Leptomeningeal carcinomatosis (LMC) secondary to metastatic breast cancer (MBC) has increased in incidence with improved systemic disease control. Current treatment options include radiation therapy (to symptomatic sites) and systemic treatment [intrathecal (IT) or intravenous (IV) chemotherapy]. Methotrexate (MTX), thiotepa and cytarabine are the most commonly used IT agents, while high-dose MTX is the most common IV regimen. While IT treatments are generally well tolerated, complications like chemical meningitis, leukoencephalopathy, etc. occur. LMC may cause a breakdown in the blood-brain barrier and thus allow systemic agents to penetrate; however, efficacy is reported only for agents administered at high doses (MTX). We report our institution's experience in using IV thiotepa as treatment for LMC secondary to MBC. We conducted a retrospective chart review of 13 patients with MBC who developed LMC and treated with IV thiotepa at our institution. It was administered at 40 mg/m(2) every 21 days; median number of thiotepa cycles administered was 5 with the major dose-limiting toxicity being myelosuppression. Four had partial response, 3 had stable disease and 6 had progressive disease. The 6-month survival rate was 69 % and 1-year survival rate was 31 %. Despite retrospective nature of our case series, we found the use of IV thiotepa as sole treatment for LMC in patients with MBC to be well tolerated, easily administered in the ambulatory setting, and with efficacy comparable to the other chemotherapeutic agents commonly used in the treatment of LMC. This regimen warrants further investigation in prospective studies.
Eder S, Labopin M, Arcese W, et al.
Thiotepa-based versus total body irradiation-based myeloablative conditioning prior to allogeneic stem cell transplantation for acute myeloid leukaemia in first complete remission: a retrospective analysis from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation.
Eur J Haematol. 2016; 96(1):90-7 [PubMed] Related Publications
Thiotepa-based versus total body irradiation-based myeloablative conditioning prior to allogeneic stem cell transplantation for acute myeloid leukaemia in first complete remission: a retrospective analysis from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation.
Eur J Haematol. 2016; 96(1):90-7 [PubMed] Related Publications
Thiotepa is an alkylating compound with an antineoplastic and myeloablative activity and can mimic the effect of radiation. However, it is unknown whether this new regimen could safely replace the long-established ones. This retrospective matched-pair analysis evaluated the outcome of adults with acute myeloid leukaemia in first complete remission who received myeloablative conditioning either with a thiotepa-based (n = 121) or a cyclophosphamide/total body irradiation-based (TBI; n = 358) regimen for allogeneic hematopoietic stem cell transplantation from an HLA-matched sibling or an unrelated donor. With a median follow-up of 44 months, the outcome was similar in both groups. Acute graft-versus-host disease grade II-IV was observed in 25% after thiotepa-containing regimen versus 35% after TBI (P = 0.06). The 2-yr cumulative incidence of chronic graft-versus-host disease was 40.5% for thiotepa and 41% for TBI (P = 0.98). At 2 yrs, the cumulative incidences of non-relapse mortality and relapse incidence were 23.9% (thiotepa) vs. 22.4% (TBI; P = 0.66) and 17.2% (thiotepa) vs. 23.3% (TBI; P = 0.77), respectively. The probabilities of leukaemia-free and overall survival at 2 yrs were not significantly different between the thiotepa and TBI groups, at 58.9% vs. 54.2% (P = 0.95) and 61.4% vs. 58% (P = 0.72), respectively. Myeloablative regimens using combinations including thiotepa can provide satisfactory outcomes, but the optimal conditioning remains unclear for the individual patient in this setting.
Baronciani D, Depau C, Targhetta C, et al.
Treosulfan-fludarabine-thiotepa conditioning before allogeneic haemopoietic stem cell transplantation for patients with advanced lympho-proliferative disease. A single centre study.
Hematol Oncol. 2016; 34(1):17-21 [PubMed] Related Publications
Treosulfan-fludarabine-thiotepa conditioning before allogeneic haemopoietic stem cell transplantation for patients with advanced lympho-proliferative disease. A single centre study.
Hematol Oncol. 2016; 34(1):17-21 [PubMed] Related Publications
In recent years, with the aim of reducing transplant-related mortality, new conditioning regimens have been explored in patients not eligible for conventional haemopoietic stem cell transplantation. In this setting, we investigated safety and feasibility of the treosulfan-fludarabine-thiotepa combination prior to allogeneic haemopoietic stem cell transplantation in patients with advanced lympho-proliferative diseases and at high transplant risk. Twenty-seven consecutive patients, median age 43 years (range 19-60), entered this study. All of them were affected by lympho-proliferative disease in advanced phase and have been heavily pre-treated. The median haemopoietic stem cell transplant co-morbidity index was 1 (range 0-3). Twenty-five patients had regular engraftment, while the remaining two patients were not evaluable for early deaths. Non-haematological toxicity was limited. No patient developed veno-occlusive disease. The estimated probability of overall survival and progression-free survival with a median follow-up of 40 months was 52% (95% confidence interval 33-73) and 50% (95% confidence interval 30-70) respectively. Six patients have relapsed; all of them were not in remission before transplantation. The treosulfan-fludarabine-thiotepa combination is a reduced toxicity but myeloablative regimen that can be proposed to patients not fitting criteria for conventional myeloablative transplant regimens. Longer follow-up and prospective randomized studies are necessary to evaluate this regimen.
Thust SC, Blanco E, Michalski AJ, et al.
MRI abnormalities in children following sequential chemotherapy, hyperfractionated accelerated radiotherapy and high-dose thiotepa for high-risk primitive neuroectodermal tumours of the central nervous system.
J Med Imaging Radiat Oncol. 2014; 58(6):683-90 [PubMed] Related Publications
MRI abnormalities in children following sequential chemotherapy, hyperfractionated accelerated radiotherapy and high-dose thiotepa for high-risk primitive neuroectodermal tumours of the central nervous system.
J Med Imaging Radiat Oncol. 2014; 58(6):683-90 [PubMed] Related Publications
INTRODUCTION: Intensive postsurgical therapies have improved survival in children with primitive neuroectodermal tumour, but there is concern that the combination of chemotherapy and radiotherapy may result in a compound injury to normal brain. The purposes of this analysis were to characterise what types of imaging abnormalities occur, identify risk factors and explore how treatment-related changes may be distinguished from tumour.
METHOD: One hundred fifty-three MRI studies in 14 children treated with sequential chemotherapy, hyperfractionated accelerated radiotherapy and high-dose thiotepa were retrospectively analysed at a paediatric national referral centre.
RESULTS: We observed 11 episodes of new focal enhancing lesions, 5 of which were transient and judged to be treatment related. In addition, 7/14 (50%) of children demonstrated moderate to severe brain volume loss featuring a leukodystrophy pattern.
CONCLUSION: Treatment-related brain MRI abnormalities occurred frequently in this series with a risk of misdiagnosis as tumour. A proportion of patients suffer generalised white matter injury, which has not been appreciated as a side effect of this particular therapy.
METHOD: One hundred fifty-three MRI studies in 14 children treated with sequential chemotherapy, hyperfractionated accelerated radiotherapy and high-dose thiotepa were retrospectively analysed at a paediatric national referral centre.
RESULTS: We observed 11 episodes of new focal enhancing lesions, 5 of which were transient and judged to be treatment related. In addition, 7/14 (50%) of children demonstrated moderate to severe brain volume loss featuring a leukodystrophy pattern.
CONCLUSION: Treatment-related brain MRI abnormalities occurred frequently in this series with a risk of misdiagnosis as tumour. A proportion of patients suffer generalised white matter injury, which has not been appreciated as a side effect of this particular therapy.
Kokolo MB, Fergusson D, O'Neill J, et al.
Effectiveness and safety of thiotepa as conditioning treatment prior to stem cell transplant in patients with central nervous system lymphoma.
Leuk Lymphoma. 2014; 55(12):2712-20 [PubMed] Related Publications
Effectiveness and safety of thiotepa as conditioning treatment prior to stem cell transplant in patients with central nervous system lymphoma.
Leuk Lymphoma. 2014; 55(12):2712-20 [PubMed] Related Publications
BACKGROUND: Thiothepa is a cytostatic agent used in managing solid malignancies, and also as conditioning treatment before hematopoietic stem cell transplantation [HSCT]. This systematic review summarizes evidence on its effectiveness and safety, in patients with central nervous system [CNS] lymphoma.
METHODS: We searched 3 databases for clinical studies. When feasible, we performed meta-analyses.
RESULTS: We identified 13 eligible studies, none of which with a priori controls. So data synthesis focused on the 226 patients who received thiotepa. Based on pooled estimates, 75.9% of thiotepa-treated patients achieved a complete remission (95% confidence interval [CI] = 67.5-82.8), and 61.7% had a progression-free survival for up to 125 months post-treatment (95% CI = 49.4-72.7). However, 25.5% relapsed, 24.6% experienced infection, and 13.2% experienced neurotoxicity.
DISCUSSION: Thiotepa-based conditioning followed by HSCT may be effective in most CNS lymphoma patients, with a manageable toxicity profile. But adequately powered randomized trials are needed to better evaluate and isolate the effects of thiotepa.
METHODS: We searched 3 databases for clinical studies. When feasible, we performed meta-analyses.
RESULTS: We identified 13 eligible studies, none of which with a priori controls. So data synthesis focused on the 226 patients who received thiotepa. Based on pooled estimates, 75.9% of thiotepa-treated patients achieved a complete remission (95% confidence interval [CI] = 67.5-82.8), and 61.7% had a progression-free survival for up to 125 months post-treatment (95% CI = 49.4-72.7). However, 25.5% relapsed, 24.6% experienced infection, and 13.2% experienced neurotoxicity.
DISCUSSION: Thiotepa-based conditioning followed by HSCT may be effective in most CNS lymphoma patients, with a manageable toxicity profile. But adequately powered randomized trials are needed to better evaluate and isolate the effects of thiotepa.
Comte A, Jdid W, Guilhaume MN, et al.
Survival of breast cancer patients with meningeal carcinomatosis treated by intrathecal thiotepa.
J Neurooncol. 2013; 115(3):445-52 [PubMed] Related Publications
Survival of breast cancer patients with meningeal carcinomatosis treated by intrathecal thiotepa.
J Neurooncol. 2013; 115(3):445-52 [PubMed] Related Publications
Treatment of breast cancer meningeal carcinomatosis (MC) relies on intrathecal chemotherapy. Thiotepa is one of the few drugs approved in this setting, although no large cohort has been reported. The aim of our retrospective study is to describe survival and prognostic factors of breast cancer patients treated by intrathecal thiotepa. A search in the electronic database of the Institut Curie was performed and retrieved the patients diagnosed with breast cancer MC from 2000 to 2012 and who received at least one intrathecal injection of thiotepa. The standard regimen was intrathecal thiotepa (10 mg) and methylprednisolone (40 mg), repeated every other week. Clinical data were retrieved from the computerized medical file of each patient. Sixty-six patients have been treated with intrathecal thiotepa either as first line or second line of treatment for breast cancer MC. The median overall survival was 4.5 months (range 0.1-50). There was no significant survival difference between patients treated as first or second line. In multivariate analysis, main adverse prognostic factors at diagnosis were performance status >2 (p = 0.001, RR = 3.4, 95 % CI 1.6-7.2) and history of more than 3 previous systemic chemotherapy lines (p = 0.002, RR = 2.90, 95 % CI 1.50-5.65). After start of the treatment, high primary tumor grade, elevated Cyfra 21-1 levels in the cerebrospinal fluid, and lack of clinical improvement were also independent adverse prognostic factors in multivariate analysis. This is the largest retrospective cohort of breast cancer MC treated by intrathecal thiotepa ever reported. The median overall survival was short but some patients clearly benefited from this treatment, even used as second line.
Le Rhun E, Taillibert S, Devos P, et al.
Salvage intracerebrospinal fluid thiotepa in breast cancer-related leptomeningeal metastases: a retrospective case series.
Anticancer Drugs. 2013; 24(10):1093-7 [PubMed] Related Publications
Salvage intracerebrospinal fluid thiotepa in breast cancer-related leptomeningeal metastases: a retrospective case series.
Anticancer Drugs. 2013; 24(10):1093-7 [PubMed] Related Publications
There is currently a paucity of data on salvage intracerebrospinal fluid (intra-CSF) chemotherapy in leptomeningeal metastases (LM). This report is a single-institution experience with salvage treatment in patients with breast cancer (BC) and LM. This retrospective cohort describes 24 consecutive patients with BC selected for a second-line of treatment for LM. The first line of LM treatment consisted of intra-CSF liposomal cytarabine in all patients combined with systemic therapy in 18 cases and radiotherapy in four cases. Second-line (salvage) treatment utilized intra-CSF thiotepa in all and systemic chemotherapy in nine patients. No patient received CNS-directed radiotherapy. The median Eastern Cooperative Oncology Group performance status at initiation of intra-CSF thiotepa treatment was 3 (range 1-4). The median progression-free survival and median survival following intra-CSF thiotepa was 3.1 months (range 3 days-2 years) and 4.0 months (range 6 days-2.5 years), respectively. The median overall survival from LM diagnosis was 9.5 months (range 1.3 months-2.7 years). No grade 3 or higher toxicity was observed. Recognizing the limits of a retrospective study, intra-CSF thiotepa has an acceptable toxicity profile and appears to be a reasonable option for selected BC patients.
Christopoulos P, Schmoor C, Waterhouse M, et al.
Reduced-intensity conditioning with fludarabine and thiotepa for second allogeneic transplantation of relapsed patients with AML.
Bone Marrow Transplant. 2013; 48(7):901-7 [PubMed] Related Publications
Reduced-intensity conditioning with fludarabine and thiotepa for second allogeneic transplantation of relapsed patients with AML.
Bone Marrow Transplant. 2013; 48(7):901-7 [PubMed] Related Publications
A second allograft was offered to 58 relapsed AML patients after conditioning with fludarabine 90-150 mg/m(2) and thiotepa 15 mg/kg, in most cases with active disease. Median age was 53 years (range 23-69), median time to relapse after the first allo-SCT was 326 (47-2189) days and median follow-up was 6.7 years. GVHD prophylaxis consisted mainly of CsA and alemtuzumab. Response rates at 1 month were CR in 50 and persistent disease in 3/53 evaluable patients. At 3 years, the relapse incidence (95% confidence interval) was 56 (45-71)%, the TRM 31 (21-46)%, the OS rate was 18 (9-29)% and the EFS rate was 13 (5-23)%. OS improved with younger patient age, longer relapse-free interval after the first allo-SCT and the development of chronic GVHD. Patients ≥ 65 years old who relapsed >12 months after the first allograft (n=20) had a 3-year OS rate of 41 (19-62)%. Conventional cytogenetics and FLT3 mutation status did not affect outcome. Our regimen is feasible and provides at least for a subgroup of patients with AML recurrence after allo-SCT a reasonable therapeutic option in an otherwise fatal situation. Further modifications and a better understanding of the underlying biology could help lower the risk of relapse.
Saarinen-Pihkala UM, Hovi L, Koivusalo A, et al.
Thiotepa and melphalan based single, tandem, and triple high dose therapy and autologous stem cell transplantation for high risk neuroblastoma.
Pediatr Blood Cancer. 2012; 59(7):1190-7 [PubMed] Related Publications
Thiotepa and melphalan based single, tandem, and triple high dose therapy and autologous stem cell transplantation for high risk neuroblastoma.
Pediatr Blood Cancer. 2012; 59(7):1190-7 [PubMed] Related Publications
BACKGROUND: Outcome of high risk neuroblastoma (NBL) remains unsatisfactory in spite of intensive treatment efforts. Consolidation with high-dose (HD) chemotherapy and autologous stem cell transplantation (ASCT) has been intensified with tandem and triple cycles with promising results. Our purpose was to improve the outcome with two or three HD-consolidations.
METHODS: Thirty six children with high risk NBL, diagnosed 1995-2010, had intensive induction and surgery, and were stratified to single, tandem or triple HD-therapy and ASCT, followed by local irradiation and cis-retinoic acid. In inoperable patients surgery was facilitated by preoperative HD-melphalan. Long-term outcome of our old cohort from 1987-1994 was updated.
RESULTS: Ten year event-free survival (EFS) from diagnosis was 0.44+/-0.10 of the old and 0.43+/-0.085 of the new cohort. EFS from the last ASCT was 0.53 +/-0.12 and 0.48+/-0.091, respectively. Preoperative HD-melphalan rendered 73% of bulky primaries operable in the new cohort. The 5-yr EFS from ASCT was 0.46+/-0.15 for single and 0.73+/-0.15 for tandem ASCT (P = 0.19). All triple ASCT patients, selected by poor/slow response, relapsed or died.
CONCLUSIONS: Thiotepa- and melphalan based HD regimens, with or without total body irradiation (TBI), appeared to give an outcome comparable to major NBL study groups with acceptable toxicity. Tandem HD therapy gave a 5-year EFS of 73%, whereas a third HD consolidation did not offer any additional advantage for ultra high risk patients with slow response. Pediatr Blood Cancer 2012; 59: 1190-1197. © 2012 Wiley Periodicals, Inc.
METHODS: Thirty six children with high risk NBL, diagnosed 1995-2010, had intensive induction and surgery, and were stratified to single, tandem or triple HD-therapy and ASCT, followed by local irradiation and cis-retinoic acid. In inoperable patients surgery was facilitated by preoperative HD-melphalan. Long-term outcome of our old cohort from 1987-1994 was updated.
RESULTS: Ten year event-free survival (EFS) from diagnosis was 0.44+/-0.10 of the old and 0.43+/-0.085 of the new cohort. EFS from the last ASCT was 0.53 +/-0.12 and 0.48+/-0.091, respectively. Preoperative HD-melphalan rendered 73% of bulky primaries operable in the new cohort. The 5-yr EFS from ASCT was 0.46+/-0.15 for single and 0.73+/-0.15 for tandem ASCT (P = 0.19). All triple ASCT patients, selected by poor/slow response, relapsed or died.
CONCLUSIONS: Thiotepa- and melphalan based HD regimens, with or without total body irradiation (TBI), appeared to give an outcome comparable to major NBL study groups with acceptable toxicity. Tandem HD therapy gave a 5-year EFS of 73%, whereas a third HD consolidation did not offer any additional advantage for ultra high risk patients with slow response. Pediatr Blood Cancer 2012; 59: 1190-1197. © 2012 Wiley Periodicals, Inc.



 Childhood Brain Tumours
Childhood Brain Tumours