Found this page useful?
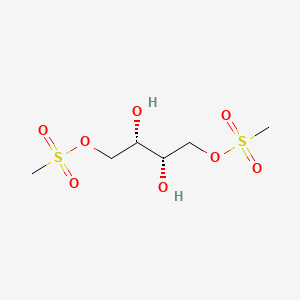
Treosulfan
 Web Resources: Treosulfan
Web Resources: Treosulfan Recent Research Publications
Recent Research PublicationsWeb Resources: Treosulfan (5 links)
Cancer Research UK
Irish Cancer Society
Macmillan Cancer Support
NHS Evidence
 Treosulfan - Substance Summary
Treosulfan - Substance Summary
PubChem
Recent Research Publications
Fein JA, Shimoni A, Labopin M, et al.
The impact of individual comorbidities on non-relapse mortality following allogeneic hematopoietic stem cell transplantation.
Leukemia. 2018; 32(8):1787-1794 [PubMed] Related Publications
The impact of individual comorbidities on non-relapse mortality following allogeneic hematopoietic stem cell transplantation.
Leukemia. 2018; 32(8):1787-1794 [PubMed] Related Publications
Comorbidity burden is a well-established risk factor for non-relapse mortality (NRM) following allogeneic stem cell transplantation (allo-SCT). We evaluated whether individual comorbidities could better characterize NRM risk. Furthermore, given differing toxicity profiles of conditioning agents, we hypothesized that the hazard of comorbidities is exerted in a regimen-specific manner. This retrospective study included 875 adults treated with an allo-SCT. Six conditioning regimens were considered. Across the entire cohort and within each regimen, the hazard ratio (HR) for NRM associated with individual comorbidities was assessed using multivariable Cox regressions. In the overall population, renal dysfunction, hypoalbuminemia, and severe hepatic disease were associated with the highest risk of NRM (HR 2.1, HR 1.9, HR 1.7, respectively). The risk associated with specific comorbidities was modified by the conditioning regimen and was not correlated with intensity. In patients conditioned with fludarabine/busulfan (Flu/Bu4), NRM risk was increased with cardiac disease (HR 5.54). Severe pulmonary disease and a pre-existing infection were associated with increased NRM risk in patients receiving fludarabine/melphalan (HR 4.9) and fludarabine/treosulfan (HR 3.6), respectively. Comorbidities may exert effects unique to particular conditioning regimens, suggesting that regimen selection should be driven in part by specific comorbidities.
Nemecek ER, Hilger RA, Adams A, et al.
Treosulfan, Fludarabine, and Low-Dose Total Body Irradiation for Children and Young Adults with Acute Myeloid Leukemia or Myelodysplastic Syndrome Undergoing Allogeneic Hematopoietic Cell Transplantation: Prospective Phase II Trial of the Pediatric Blood and Marrow Transplant Consortium.
Biol Blood Marrow Transplant. 2018; 24(8):1651-1656 [PubMed] Free Access to Full Article Related Publications
Treosulfan, Fludarabine, and Low-Dose Total Body Irradiation for Children and Young Adults with Acute Myeloid Leukemia or Myelodysplastic Syndrome Undergoing Allogeneic Hematopoietic Cell Transplantation: Prospective Phase II Trial of the Pediatric Blood and Marrow Transplant Consortium.
Biol Blood Marrow Transplant. 2018; 24(8):1651-1656 [PubMed] Free Access to Full Article Related Publications
This multicenter study evaluated a treosulfan-based regimen in children and young adults with acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS) undergoing allogeneic hematopoietic cell transplant (HCT). Forty patients with median age 11 years (range, 1 to 19) underwent allogeneic HCT for AML in first (n = 18), second (n = 11), and third or greater remission (n = 3) or MDS (n = 8) using bone marrow (n = 25), peripheral blood stem cells (n = 5), or cord blood (n = 9). The regimen consisted of body surface area (BSA)-based treosulfan 10 g/m
Steckel NK, Groth C, Mikesch JH, et al.
High-dose melphalan-based sequential conditioning chemotherapy followed by allogeneic haematopoietic stem cell transplantation in adult patients with relapsed or refractory acute myeloid leukaemia.
Br J Haematol. 2018; 180(6):840-853 [PubMed] Related Publications
High-dose melphalan-based sequential conditioning chemotherapy followed by allogeneic haematopoietic stem cell transplantation in adult patients with relapsed or refractory acute myeloid leukaemia.
Br J Haematol. 2018; 180(6):840-853 [PubMed] Related Publications
Considering the unsatisfactory results of salvage therapies for patients with relapsed/refractory acute myeloid leukaemia (R/R-AML), their value before allogeneic haematopoietic stem cell transplantation (HSCT) remains questionable. However, direct allogeneic HSCT following established conditioning regimens applied in patients with R/R-AML during active disease has been equally disappointing. In this retrospective observational study, high-dose melphalan, as part of a sequential preparative regimen, followed by a total body irradiation (4 × 2 Gy)-based or a treosulfan-based dose-adapted conditioning therapy for allogeneic HSCT was administered to 292 adult patients (median age 56 years, range 17-74) with primary refractory (144 patients), secondary refractory (97 patients) or relapsed AML (51 patients). Overall survival rates at 3 years were 34%, 29% and 41%, respectively. Risk factors associated with an inferior survival were higher age, transplantation from a human leucocyte antigen-mismatched donor and high disease burden. Patients transplanted with blast infiltration <20% showed a notable survival rate of 51% at 3 years. In particular, patients with primary refractory AML showed a more favourable outcome when transplanted early during their disease course. Thus, high-dose melphalan-based sequential conditioning chemotherapy followed by an allogeneic HSCT is feasible and enables long-term remission to be achieved in a substantial proportion of patients with active R/R-AML.
Deeg HJ, Stevens EA, Salit RB, et al.
Transplant Conditioning with Treosulfan/Fludarabine with or without Total Body Irradiation: A Randomized Phase II Trial in Patients with Myelodysplastic Syndrome and Acute Myeloid Leukemia.
Biol Blood Marrow Transplant. 2018; 24(5):956-963 [PubMed] Related Publications
Transplant Conditioning with Treosulfan/Fludarabine with or without Total Body Irradiation: A Randomized Phase II Trial in Patients with Myelodysplastic Syndrome and Acute Myeloid Leukemia.
Biol Blood Marrow Transplant. 2018; 24(5):956-963 [PubMed] Related Publications
In this prospective, randomized, phase II "pick the winner" trial we assessed the efficacy of transplant conditioning with treosulfan/fludarabine ± 2 Gy total body irradiation (TBI) in reducing post-transplant relapse in 100 patients, aged 2 to 70 years (median, 57), with myelodysplastic syndrome (MDS)/chronic myelomonocytic leukemia (n = 51) or acute myeloid leukemia (AML; n = 49). Patients received i.v. treosulfan, 14 g/m
Shimoni A, Labopin M, Savani B, et al.
Intravenous Busulfan Compared with Treosulfan-Based Conditioning for Allogeneic Stem Cell Transplantation in Acute Myeloid Leukemia: A Study on Behalf of the Acute Leukemia Working Party of European Society for Blood and Marrow Transplantation.
Biol Blood Marrow Transplant. 2018; 24(4):751-757 [PubMed] Related Publications
Intravenous Busulfan Compared with Treosulfan-Based Conditioning for Allogeneic Stem Cell Transplantation in Acute Myeloid Leukemia: A Study on Behalf of the Acute Leukemia Working Party of European Society for Blood and Marrow Transplantation.
Biol Blood Marrow Transplant. 2018; 24(4):751-757 [PubMed] Related Publications
Dose intensity of the conditioning regimen has significant impact on the outcomes after stem cell transplantation (SCT) for acute myeloid leukemia. Most studies have shown more relapse, less nonrelapse mortality (NRM), and similar overall survival after reduced-intensity and myeloablative conditioning. There are limited data on the dose equivalence and expected outcomes of treosulfan-based compared with busulfan-based conditioning. We compared SCT outcomes after fludarabine with either intravenous busulfan at a myeloablative dose (FB4, 12.8 mg/kg, n = 1265) or a reduced dose (FB2, 6.4 mg/kg, n = 1456) or treosulfan at 42 g/m
Shimoni A, Vago L, Bernardi M, et al.
Missing HLA C group 1 ligand in patients with AML and MDS is associated with reduced risk of relapse and better survival after allogeneic stem cell transplantation with fludarabine and treosulfan reduced toxicity conditioning.
Am J Hematol. 2017; 92(10):1011-1019 [PubMed] Related Publications
Missing HLA C group 1 ligand in patients with AML and MDS is associated with reduced risk of relapse and better survival after allogeneic stem cell transplantation with fludarabine and treosulfan reduced toxicity conditioning.
Am J Hematol. 2017; 92(10):1011-1019 [PubMed] Related Publications
Reduced-toxicity conditioning with fludarabine and treosulfan is a dose-intensive regimen with enhanced anti-leukemia effect and acceptable toxicity in AML/MDS. HLA-C regulates natural-killer (NK) cell function by inhibiting Killer immunoglobulin-like receptors (KIR) and is divided into C1 and C2 epitopes. The missing-ligand theory suggests that missing recipient KIR ligands drives NK-alloreactivity after SCT, in the absence of HLA-mismatch by activating unlicensed donor NK cells. We analyzed SCT outcomes in 203 patients with AML/MDS, median age 58 years, given SCT from matched-siblings (n = 97) or matched-unrelated donors (n = 106), using two treosulfan doses (total 36 or 42 g/m
Nagler A, Labopin M, Beelen D, et al.
Long-term outcome after a treosulfan-based conditioning regimen for patients with acute myeloid leukemia: A report from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation.
Cancer. 2017; 123(14):2671-2679 [PubMed] Related Publications
Long-term outcome after a treosulfan-based conditioning regimen for patients with acute myeloid leukemia: A report from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation.
Cancer. 2017; 123(14):2671-2679 [PubMed] Related Publications
BACKGROUND: Allogeneic hematopoietic cell transplantation (HCT) is a curative therapy for patients with acute myeloid leukemia (AML). However, post-HCT relapse and regimen-related toxicity remain significant barriers to long-term survival. In recent years, new conditioning regimens have been explored to improve transplantation outcomes in patients with AML. Treosulfan combines a potent immunosuppressive and antileukemic effect with a low toxicity profile.
METHODS: To investigate the role of treosulfan-based conditioning, the European Society for Blood and Marrow Transplantation Acute Leukemia Working Party performed a registry analysis of 520 adult patients with AML who received treosulfan-based conditioning and underwent HCT between 2000 and 2012, including 225 patients in first complete remission, 107 in second or later complete remission, and 188 with active/advanced disease 188 (88 with primary refractory disease). The median patient age was 57 years (range, 20-73 years). Donors were human leukocyte antigen-identical siblings (n = 187), unrelated donors (n = 235), or mismatched related donors (n = 98). Conditioning regimens included treosulfan (42 g/m
RESULTS: At a median follow-up of 61 months, the 5-year overall survival, leukemia-free survival, relapse incidence, and nonrelapse mortality rates were 38%, 33%, 42%, and 25%, respectively. The incidence of grade II-IV acute and chronic graft-versus-host disease was 24% (grade III-V, 11%) and 38%, respectively. Only 11 patients (2%) developed veno-occlusive disease, with two deaths (0.4%) from veno-occlusive disease.
CONCLUSIONS: Treosulfan-based conditioning regimens provide an acceptable long-term survival with favorable nonrelapse mortality and a very low risk of veno-occlusive disease. Further studies are needed to optimize the treosulfan-based conditioning regimen for patients with AML. Cancer 2017;123:2671-79. © 2017 American Cancer Society.
METHODS: To investigate the role of treosulfan-based conditioning, the European Society for Blood and Marrow Transplantation Acute Leukemia Working Party performed a registry analysis of 520 adult patients with AML who received treosulfan-based conditioning and underwent HCT between 2000 and 2012, including 225 patients in first complete remission, 107 in second or later complete remission, and 188 with active/advanced disease 188 (88 with primary refractory disease). The median patient age was 57 years (range, 20-73 years). Donors were human leukocyte antigen-identical siblings (n = 187), unrelated donors (n = 235), or mismatched related donors (n = 98). Conditioning regimens included treosulfan (42 g/m
RESULTS: At a median follow-up of 61 months, the 5-year overall survival, leukemia-free survival, relapse incidence, and nonrelapse mortality rates were 38%, 33%, 42%, and 25%, respectively. The incidence of grade II-IV acute and chronic graft-versus-host disease was 24% (grade III-V, 11%) and 38%, respectively. Only 11 patients (2%) developed veno-occlusive disease, with two deaths (0.4%) from veno-occlusive disease.
CONCLUSIONS: Treosulfan-based conditioning regimens provide an acceptable long-term survival with favorable nonrelapse mortality and a very low risk of veno-occlusive disease. Further studies are needed to optimize the treosulfan-based conditioning regimen for patients with AML. Cancer 2017;123:2671-79. © 2017 American Cancer Society.
Bresters D, Wanders DCM, Louwerens M, et al.
Permanent diffuse alopecia after haematopoietic stem cell transplantation in childhood.
Bone Marrow Transplant. 2017; 52(7):984-988 [PubMed] Related Publications
Permanent diffuse alopecia after haematopoietic stem cell transplantation in childhood.
Bone Marrow Transplant. 2017; 52(7):984-988 [PubMed] Related Publications
Permanent alopecia after haematopoietic stem cell transplantation (HSCT) is distressing and few studies have investigated this late effect. The aim of the study was to assess the percentage of patients with alopecia and investigate risk factors for alopecia. Patients who underwent allogeneic HSCT before age 19 years, from January 1990 to January 2013, who were at least 2 years after transplant and in follow-up in our clinic were included. Alopecia was defined as clinically apparent decreased hair density. Possible risk factors considered for alopecia after HSCT included: gender, age, diagnosis, donor type, conditioning regimen: cranial irradiation (TBI/cranial radiotherapy) and/or chemotherapy, which chemotherapeutic agents were used and acute/chronic GvHD. The percentage of permanent alopecia in our cohort was 15.6% (41/263 patients). All patients had diffuse alopecia except for one with alopecia totalis. In multivariate analysis, a conditioning regimen with busulphan and busulphan plus fludarabine (odds ratio (OR) 5.7 (confidence interval (CI): 2.5-12.7) and OR 7.4 (CI: 3.3-16.2), respectively, was the main risk factor and associated with alopecia independent of acute/chronic GvHD. Neither TBI nor other alkylating chemotherapy, including treosulfan, was associated with alopecia. In conclusion, permanent alopecia after HSCT is associated with busulphan and GvHD and occurs in 16% of patients.
Terjung A, Altgassen C, Friedrich M
Treosulfan for advanced breast cancer in a heavily pre-treated patient - a case report.
Eur J Gynaecol Oncol. 2017; 38(1):115-117 [PubMed] Related Publications
Treosulfan for advanced breast cancer in a heavily pre-treated patient - a case report.
Eur J Gynaecol Oncol. 2017; 38(1):115-117 [PubMed] Related Publications
BACKGROUND: Treatment of metastatic breast cancer experienced significant improvement in the past decades by introduction of highly effective therapies, but survival still remains poor. Nonetheless, in some patients, long-term survival can be achieved by sequent endocrine and chemotherapy treatment, although toxicity and resistance eventually occur, until no further suitable and approved therapies remain. If further therapy is needed, therapist may be forced to consider treatients which are promising but not approved, such as the alkylating agent treosulfan, which is approved for the treatment of ovarian cancer only. Thus, relevant clinical data on its use in human breast cancer are lacking.
CASE REPORT: The authors report the case of a 49-yeAr-old woman with heavily pre-treated, metastatic breast cancer, who experienced complete remission of pulmonary and soft tissue metastases while under treatment with treosulfan. Treatment was generally well-tolerated.
CONCLUSION: Treosulfan might be an effective and well-tolerated treatment even in heavily pre-treated patients with metastatic breast cancer.
CASE REPORT: The authors report the case of a 49-yeAr-old woman with heavily pre-treated, metastatic breast cancer, who experienced complete remission of pulmonary and soft tissue metastases while under treatment with treosulfan. Treatment was generally well-tolerated.
CONCLUSION: Treosulfan might be an effective and well-tolerated treatment even in heavily pre-treated patients with metastatic breast cancer.
Sakellari I, Mallouri D, Gavriilaki E, et al.
Survival Advantage and Comparable Toxicity in Reduced-Toxicity Treosulfan-Based versus Reduced-Intensity Busulfan-Based Conditioning Regimen in Myelodysplastic Syndrome and Acute Myeloid Leukemia Patients after Allogeneic Hematopoietic Cell Transplantation.
Biol Blood Marrow Transplant. 2017; 23(3):445-451 [PubMed] Related Publications
Survival Advantage and Comparable Toxicity in Reduced-Toxicity Treosulfan-Based versus Reduced-Intensity Busulfan-Based Conditioning Regimen in Myelodysplastic Syndrome and Acute Myeloid Leukemia Patients after Allogeneic Hematopoietic Cell Transplantation.
Biol Blood Marrow Transplant. 2017; 23(3):445-451 [PubMed] Related Publications
Treosulfan has been incorporated in conditioning regimens for sustained remission without substantial toxicity and treatment-related mortality (TRM). We aimed to analyze the safety and efficacy of a fludarabine 150 mg/m
Holtick U, Herling M, Pflug N, et al.
Similar outcome after allogeneic stem cell transplantation with a modified FLAMSA conditioning protocol substituting 4 Gy TBI with treosulfan in an elderly population with high-risk AML.
Ann Hematol. 2017; 96(3):479-487 [PubMed] Related Publications
Similar outcome after allogeneic stem cell transplantation with a modified FLAMSA conditioning protocol substituting 4 Gy TBI with treosulfan in an elderly population with high-risk AML.
Ann Hematol. 2017; 96(3):479-487 [PubMed] Related Publications
The fludarabine, amsacrine, and cytarabine (FLAMSA)-reduced-intensity conditioning (RIC) protocol has been described to be effective in patients with high-risk and refractory acute myeloic leukemia (AML) undergoing allogeneic hematopoietic stem cell transplantation (aSCT). To increase safety and tolerability of the conditioning, we previously reported the feasibility to substitute the TBI component by treosulfan in elderly AML patients. We now present long-term follow-up data on patients treated with FLAMSA/treosulfan compared to the original FLAMSA/4Gy TBI protocol. We retrospectively analyzed 130 consecutive patients with high-risk or relapsed AML after aSCT following FLAMSA conditioning at our center. Fifty-eight patients were treated with FLAMSA/treosulfan due to age and/or comorbidities. Seventy-two patients were treated with FLAMSA/TBI. Median age of patients treated with FLAMSA/treosulfan was 60 years compared to 46 years in those treated with FLAMSA/TBI. The cumulative incidence of a non-relapse mortality at 4 years was 28% in FLAMSA/treosulfan patients as compared to 13% in FLAMSA/TBI. Cumulative incidence of relapse was higher in patients treated with FLAMSA/TBI (46 vs. 32%). This difference was even more prominent for patients treated in blast persistence prior to transplant (relapse incidence 70% for TBI vs. 35% for treosulfan). The overall and relapse-free survival rates at 4 years were 47 and 41%, respectively, for patients treated with FLAMSA/TBI as compared to 43 and 40% in patients treated with FLAMSA/treosulfan. These data indicate an anti-leukemic activity by FLAMSA/treosulfan especially in patients with a blast persistence prior to transplant. Older age was an independent factor for a higher non-relapse mortality. Translating FLAMSA/treosulfan to younger patients, a lower non-relapse mortality, and an improved anti-leukemic activity might add up to improved overall survival. Randomized studies are required to demonstrate an improved efficacy of treosulfan- versus TBI-based FLAMSA conditioning.
Sehouli J, Tomè O, Dimitrova D, et al.
A phase III, open label, randomized multicenter controlled trial of oral versus intravenous treosulfan in heavily pretreated recurrent ovarian cancer: a study of the North-Eastern German Society of Gynecological Oncology (NOGGO).
J Cancer Res Clin Oncol. 2017; 143(3):541-550 [PubMed] Free Access to Full Article Related Publications
A phase III, open label, randomized multicenter controlled trial of oral versus intravenous treosulfan in heavily pretreated recurrent ovarian cancer: a study of the North-Eastern German Society of Gynecological Oncology (NOGGO).
J Cancer Res Clin Oncol. 2017; 143(3):541-550 [PubMed] Free Access to Full Article Related Publications
OBJECTIVE: In recurrent ovarian cancer (ROC), there is a high demand on effective therapies with a mild toxicity profile. Treosulfan is an alkylating agent approved as oral (p.o.) and intravenous (i.v.) formulation for the treatment of recurrent ovarian cancer. Data on safety and efficacy for either formulation are rare. For the first time we conducted a randomized phase III study comparing both formulations in women with ROC.
METHODS: Patients having received at least two previous lines of chemotherapy were randomly assigned to one of two treatment arms: treosulfan i.v. 7000 mg/m
RESULTS: 250 patients were treated with treosulfan i.v. (128) or treosulfan p.o. (122). In general treosulfan therapy was well tolerated in both treatment arms. Leukopenia grade III/IV occurred significantly more frequently in the p.o. arm (3.9% i.v. arm, 14.8% p.o. arm, p = 0.002). Other toxicities were similar in both arms. CBR was comparable between arms (41.4% i.v. arm, 36.9% p.o. arm). No difference in TTP (3.7 months i.v. arm, 3.5 months p.o. arm) or OS (13.6 months i.v. arm, 10.4 months p.o. arm, p = 0.087) occurred.
CONCLUSIONS: Given the safety and efficacy results treosulfan is an acceptable option for heavily pretreated OC patients. Regarding the toxicity profile the i.v. application was better tolerated with less grade III and IV toxicities.
METHODS: Patients having received at least two previous lines of chemotherapy were randomly assigned to one of two treatment arms: treosulfan i.v. 7000 mg/m
RESULTS: 250 patients were treated with treosulfan i.v. (128) or treosulfan p.o. (122). In general treosulfan therapy was well tolerated in both treatment arms. Leukopenia grade III/IV occurred significantly more frequently in the p.o. arm (3.9% i.v. arm, 14.8% p.o. arm, p = 0.002). Other toxicities were similar in both arms. CBR was comparable between arms (41.4% i.v. arm, 36.9% p.o. arm). No difference in TTP (3.7 months i.v. arm, 3.5 months p.o. arm) or OS (13.6 months i.v. arm, 10.4 months p.o. arm, p = 0.087) occurred.
CONCLUSIONS: Given the safety and efficacy results treosulfan is an acceptable option for heavily pretreated OC patients. Regarding the toxicity profile the i.v. application was better tolerated with less grade III and IV toxicities.
Hilal Z, Schultheis B, Hartmann F, et al.
What Characterizes Long-term Survivors of Recurrent Ovarian Cancer? Case Report and Review of the Literature.
Anticancer Res. 2016; 36(10):5365-5371 [PubMed] Related Publications
What Characterizes Long-term Survivors of Recurrent Ovarian Cancer? Case Report and Review of the Literature.
Anticancer Res. 2016; 36(10):5365-5371 [PubMed] Related Publications
BACKGROUND: Women with recurrent ovarian cancer have a poor prognosis and short survival. However, some women are long-term survivors and it is unclear whether they share specific common characteristics.
CASE REPORT: We present the case of a 63-year-old woman with histologically-proven recurrent ovarian cancer and a survival time of 16 years after the diagnosis of recurrence. She underwent initial debulking surgery in 1994, followed by 6 cycles of adjuvant chemotherapy with cisplatin and paclitaxel. After recurrent disease was diagnosed by re-laparotomy in 2000, she underwent four lines of systemic chemotherapy from 2000 to 2009 (carboplatin/paclitaxel, topotecan, etoposide/treosulfan and liposomal doxorubicin) and four lines of endocrine therapy between 2002 and 2014 (tamoxifen, goserelin, tamoxifen and exemestane). In 2014, she underwent secondary debulking surgery and was tumor-free until 2015. Upon progression, she was then started on the fifth-line of endocrine therapy, fulvestrant, which was changed to the mTOR inhibitor everolimus in June 2016. In a PUBMED literature search, 360 cases of long-term survivors of recurrent ovarian cancer (LTSROC), defined as women with survival >5 years after the diagnosis of recurrence, were identified with a mean post-recurrence survival time of 7.5 years. Comparing the patient and therapy details of these women, we identified common characteristics of LTSROC, i.e. young age and optimal debulking at initial surgery, a long time span between first-line therapy and first recurrence and the combined use of optimal cytoreductive surgery and systemic chemotherapy.
CONCLUSION: LTSROC are rare, with 360 cases described in the literature. LTSROC are characterized by young age, low tumor stage, long recurrence-free interval and combined modality treatment with optimal cytoreductive surgery and systemic chemotherapy.
CASE REPORT: We present the case of a 63-year-old woman with histologically-proven recurrent ovarian cancer and a survival time of 16 years after the diagnosis of recurrence. She underwent initial debulking surgery in 1994, followed by 6 cycles of adjuvant chemotherapy with cisplatin and paclitaxel. After recurrent disease was diagnosed by re-laparotomy in 2000, she underwent four lines of systemic chemotherapy from 2000 to 2009 (carboplatin/paclitaxel, topotecan, etoposide/treosulfan and liposomal doxorubicin) and four lines of endocrine therapy between 2002 and 2014 (tamoxifen, goserelin, tamoxifen and exemestane). In 2014, she underwent secondary debulking surgery and was tumor-free until 2015. Upon progression, she was then started on the fifth-line of endocrine therapy, fulvestrant, which was changed to the mTOR inhibitor everolimus in June 2016. In a PUBMED literature search, 360 cases of long-term survivors of recurrent ovarian cancer (LTSROC), defined as women with survival >5 years after the diagnosis of recurrence, were identified with a mean post-recurrence survival time of 7.5 years. Comparing the patient and therapy details of these women, we identified common characteristics of LTSROC, i.e. young age and optimal debulking at initial surgery, a long time span between first-line therapy and first recurrence and the combined use of optimal cytoreductive surgery and systemic chemotherapy.
CONCLUSION: LTSROC are rare, with 360 cases described in the literature. LTSROC are characterized by young age, low tumor stage, long recurrence-free interval and combined modality treatment with optimal cytoreductive surgery and systemic chemotherapy.
Wuntakal R, Seshadri S, Montes A, Lane G
Luteinising hormone releasing hormone (LHRH) agonists for the treatment of relapsed epithelial ovarian cancer.
Cochrane Database Syst Rev. 2016; (6):CD011322 [PubMed] Free Access to Full Article Related Publications
Luteinising hormone releasing hormone (LHRH) agonists for the treatment of relapsed epithelial ovarian cancer.
Cochrane Database Syst Rev. 2016; (6):CD011322 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Ovarian cancer is seventh most common cancer in women worldwide. Approximately 1.3% of women will be diagnosed with ovarian cancer at some point during their life time. The majority of tumours arise from surface of the ovary (epithelial). Two thirds of these women will present with advanced disease, requiring aggressive treatment, which includes debulking surgery (removal of as much disease as possible) and chemotherapy. However, most women (75%) with advanced epithelial ovarian cancer (EOC) will relapse following surgery and chemotherapy. Patients who relapse are treated with either platinum or non-platinum drugs and this is dependent on the platinum-sensitivity and platinum-free interval. These drug regimens are generally well-tolerated although there are potential severe side effects. New treatments that can be used to treat recurrence or prevent disease progression after first-line or subsequent chemotherapy are important, especially those with a low toxicity profile. Hormones such as luteinising hormone releasing hormone (LHRH) agonists have been used in the treatment of relapsed EOC. Some studies have shown objective remissions, while other studies have shown little or no benefit. Most small studies report a better side-effect profile for LHRH agonists when compared to standard chemotherapeutic agents used in EOC.
OBJECTIVES: To compare the effectiveness and safety of luteinising hormone releasing hormone (LHRH) agonists with chemotherapeutic agents or placebo in relapsed epithelial ovarian cancer (EOC).
SEARCH METHODS: We searched the Cochrane Gynaecological Cancer Group trials register, Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and Embase up to January 2016. We also searched registers of clinical trials and abstracts of scientific meetings.
SELECTION CRITERIA: Randomised controlled trials (RCTs) that compared LHRH agonists with chemotherapeutic agents or placebo in relapsed EOC.
DATA COLLECTION AND ANALYSIS: Two review authors independently assessed whether relevant studies met the inclusion criteria, retrieved data and assessed risk of bias.
MAIN RESULTS: Two studies, including 97 women, met our inclusion criteria: one assessed LHRH agonist (leuprorelin) use in relapsed (platinum-resistant and platinum-refractory) EOC in comparison with a chemotherapeutic agent (treosulfan) (Du Bois 2002); the other examined LHRH agonist (decapeptyl) versus a placebo (Currie 1994). Since both studies had different control groups, a meta-analysis was not possible.There may be little or no difference between treatment with leuprorelin or treosulfan in overall survival (OS) (hazard ratio (HR) 0.98, 95% confidence interval (CI) 0.58 to 1.67; very low-quality evidence) or progression-free survival (PFS) at six and 12 months (risk ratio (RR) 0.61, 95% CI 0.22 to 1.68, and RR 0.65, 95% CI 0.12 to 3.66; very low-quality evidence), respectively (Du Bois 2002). The duration of follow-up was 2.5 years and quality of life (QoL) was not reported in this study.Alopecia and fatigue were probably more common with treosulfan than leuprorelin (alopecia RR 0.32, 95% CI 0.12 to 0.91 (very low-quality evidence)). There may be little or no difference in other Grade 3/4 side effects: nausea and vomiting (RR 0.65, 95% CI 0.12 to 3.66 (very low-quality evidence)); neurotoxicity (RR 0.32, 95% CI 0.01 to 7.71 (very low-quality evidence)) and neutropenia (RR 0.97, 95% 0.06 to 14.97 (very low-quality evidence)),The Currie 1994 study, which compared decapeptyl treatment with placebo, reported mean PFS of 16 weeks verus 11.2 weeks, respectively. No relative effects measures or P value at a particular time point were reported. Overall survival (OS) and QoL outcomes were not reported. In addition, adverse events were only mentioned for the decapeptyl group.Adverse events were incompletely reported (no adverse events in decapeptyl group, but not reported for the placebo group).
AUTHORS' CONCLUSIONS: Based on this review of two small RCTs, there is not enough evidence to comment on the safety and effectiveness of LHRH agonists in the treatment of platinum-refractory and platinum-resistant (relapsed) EOC. Overall, the quality of evidence for all outcomes (including OS, PFS, QoL and adverse events) is very low.
OBJECTIVES: To compare the effectiveness and safety of luteinising hormone releasing hormone (LHRH) agonists with chemotherapeutic agents or placebo in relapsed epithelial ovarian cancer (EOC).
SEARCH METHODS: We searched the Cochrane Gynaecological Cancer Group trials register, Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and Embase up to January 2016. We also searched registers of clinical trials and abstracts of scientific meetings.
SELECTION CRITERIA: Randomised controlled trials (RCTs) that compared LHRH agonists with chemotherapeutic agents or placebo in relapsed EOC.
DATA COLLECTION AND ANALYSIS: Two review authors independently assessed whether relevant studies met the inclusion criteria, retrieved data and assessed risk of bias.
MAIN RESULTS: Two studies, including 97 women, met our inclusion criteria: one assessed LHRH agonist (leuprorelin) use in relapsed (platinum-resistant and platinum-refractory) EOC in comparison with a chemotherapeutic agent (treosulfan) (Du Bois 2002); the other examined LHRH agonist (decapeptyl) versus a placebo (Currie 1994). Since both studies had different control groups, a meta-analysis was not possible.There may be little or no difference between treatment with leuprorelin or treosulfan in overall survival (OS) (hazard ratio (HR) 0.98, 95% confidence interval (CI) 0.58 to 1.67; very low-quality evidence) or progression-free survival (PFS) at six and 12 months (risk ratio (RR) 0.61, 95% CI 0.22 to 1.68, and RR 0.65, 95% CI 0.12 to 3.66; very low-quality evidence), respectively (Du Bois 2002). The duration of follow-up was 2.5 years and quality of life (QoL) was not reported in this study.Alopecia and fatigue were probably more common with treosulfan than leuprorelin (alopecia RR 0.32, 95% CI 0.12 to 0.91 (very low-quality evidence)). There may be little or no difference in other Grade 3/4 side effects: nausea and vomiting (RR 0.65, 95% CI 0.12 to 3.66 (very low-quality evidence)); neurotoxicity (RR 0.32, 95% CI 0.01 to 7.71 (very low-quality evidence)) and neutropenia (RR 0.97, 95% 0.06 to 14.97 (very low-quality evidence)),The Currie 1994 study, which compared decapeptyl treatment with placebo, reported mean PFS of 16 weeks verus 11.2 weeks, respectively. No relative effects measures or P value at a particular time point were reported. Overall survival (OS) and QoL outcomes were not reported. In addition, adverse events were only mentioned for the decapeptyl group.Adverse events were incompletely reported (no adverse events in decapeptyl group, but not reported for the placebo group).
AUTHORS' CONCLUSIONS: Based on this review of two small RCTs, there is not enough evidence to comment on the safety and effectiveness of LHRH agonists in the treatment of platinum-refractory and platinum-resistant (relapsed) EOC. Overall, the quality of evidence for all outcomes (including OS, PFS, QoL and adverse events) is very low.
Maschan M, Shelikhova L, Ilushina M, et al.
TCR-alpha/beta and CD19 depletion and treosulfan-based conditioning regimen in unrelated and haploidentical transplantation in children with acute myeloid leukemia.
Bone Marrow Transplant. 2016; 51(5):668-74 [PubMed] Related Publications
TCR-alpha/beta and CD19 depletion and treosulfan-based conditioning regimen in unrelated and haploidentical transplantation in children with acute myeloid leukemia.
Bone Marrow Transplant. 2016; 51(5):668-74 [PubMed] Related Publications
We evaluated the depletion of TCR-alpha/beta cells from the graft of children with high-risk AML, who received transplantation from unrelated (n=20) and haploidentical donors (n=13). The preparative regimen included treosulfan, melphalan, fludarabine and anti-thymocyte globulin. Grafts were PBSC engineered by TCR-alpha/beta and CD19 depletion. The graft contained a median of 9 × 10(6)/kg of CD34+ and 20 × 10(3)/kg of αβ-T cells. Post-transplant immune suppression included tacrolimus till day +30 and Mtx in 21 patients, tacrolimus in 5, Mtx in 2 and no prophylaxis in 5 patients. Sixteen patients received native or TCR-alpha/beta-depleted donor lymphocytes at a median of 47 (40-204) days. Median follow-up is 1.76 years. Primary engraftment was achieved in 33 patients (100%). Cumulative incidence of acute GvHD (aGvHD) grade 2-3 was 39 (26-60)%, half of them had skin-only aGvHD. Cumulative incidence of chronic GvHD was 30(18-50)%. Transplant-related mortality is 10(4-26)%. Event-free survival (EFS) is 60(43-76)% and overall survival (OS) is 67(50-84)% at 2 years. In a subgroup of patients, who received transplantation in CR, EFS is 66(48-84)% and OS-72(53-90)% at 2 years. Our data suggest that TCR-alpha/beta and CD19 depletion is a robust method of graft manipulation, which can be used to engineer grafts for children with AML.
Chekerov R, Kaltenecker G, Reichert D, et al.
Treosulfan in the Treatment of Advanced Ovarian Cancer - Results of a German Multicenter Non-interventional Study.
Anticancer Res. 2015; 35(12):6869-75 [PubMed] Related Publications
Treosulfan in the Treatment of Advanced Ovarian Cancer - Results of a German Multicenter Non-interventional Study.
Anticancer Res. 2015; 35(12):6869-75 [PubMed] Related Publications
BACKGROUND: Data on routine systemic treatment of patients with ovarian cancer are currently available only to a limited degree. The alkylating agent treosulfan is approved in oral (p.o.) and intravenous (i.v.) form for the treatment of ovarian carcinoma. The present non-interventional study analyzed the clinical use of treosulfan in Germany, evaluating the mode of application, toxicity, and response and survival rate.
PATIENTS AND METHODS: Two hundred and forty-eight ovarian cancer patients in 57 Centers, who received treosulfan mainly either i.v. (5,000-8,000 mg/m(2) d1, q21d or q28d) or p.o. (400-600 mg/m(2) d1-14 or 21, q28d) for at least one therapy cycle were evaluable and were included in the study.
RESULTS: With a median age of 70 years (range=36-92 years), predominantly elderly patients received treosulfan treatment. Most participants presented serous histology (131, 52.8%) and advanced-stage FIGO III (122, 49%) or IV (55, 22%) disease. Median ECOG status was 1 (range=0-2), whereas cardiac co-morbidity was common (31%). Treosulfan was usually administered as second- (26%), third- (21%) or fourth-line (17%) therapy. Two hundred and one patients received i.v. and 47 p.o.
TREATMENT: The most common reason for dose modifications was due to hematological toxicity (46%). The main reason for a therapy discontinuation was progressive disease (38.5%). Response was observed in 25.8% of participants, disease stabilization in 28.6 % and progress in 45.6%. The median progression-free and overall survival was 196 and 405 days, respectively.
CONCLUSION: In predominantly elderly and heavily pre-treated patients with recurrent ovarian cancer, treosulfan featured a clinical relevant efficacy and well-manageable, mostly hematological, toxicity, which resulted in a positive therapeutic index.
PATIENTS AND METHODS: Two hundred and forty-eight ovarian cancer patients in 57 Centers, who received treosulfan mainly either i.v. (5,000-8,000 mg/m(2) d1, q21d or q28d) or p.o. (400-600 mg/m(2) d1-14 or 21, q28d) for at least one therapy cycle were evaluable and were included in the study.
RESULTS: With a median age of 70 years (range=36-92 years), predominantly elderly patients received treosulfan treatment. Most participants presented serous histology (131, 52.8%) and advanced-stage FIGO III (122, 49%) or IV (55, 22%) disease. Median ECOG status was 1 (range=0-2), whereas cardiac co-morbidity was common (31%). Treosulfan was usually administered as second- (26%), third- (21%) or fourth-line (17%) therapy. Two hundred and one patients received i.v. and 47 p.o.
TREATMENT: The most common reason for dose modifications was due to hematological toxicity (46%). The main reason for a therapy discontinuation was progressive disease (38.5%). Response was observed in 25.8% of participants, disease stabilization in 28.6 % and progress in 45.6%. The median progression-free and overall survival was 196 and 405 days, respectively.
CONCLUSION: In predominantly elderly and heavily pre-treated patients with recurrent ovarian cancer, treosulfan featured a clinical relevant efficacy and well-manageable, mostly hematological, toxicity, which resulted in a positive therapeutic index.
Pogorzala M, Kubicka M, Rafinska B, et al.
Drug-resistance Profile in Multiple-relapsed Childhood Acute Lymphoblastic Leukemia.
Anticancer Res. 2015; 35(10):5667-70 [PubMed] Related Publications
Drug-resistance Profile in Multiple-relapsed Childhood Acute Lymphoblastic Leukemia.
Anticancer Res. 2015; 35(10):5667-70 [PubMed] Related Publications
AIM: To analyze the drug-resistance profile at first and subsequent relapse in children with acute lymphoblastic leukemia (ALL).
PATIENTS AND METHODS: A total of 154 pediatric ALL samples were tested for ex vivo chemosensitivity for up to 19 drugs. Their combined drug resistance profile (PVA score) was analyzed.
RESULTS: The median relative resistance scores between patients with multiple relapse and those with first relapse considering all drugs was 2.0. The median PVA score at subsequent relapses was 8 vs. 6 at first relapse (p=0.004). Samples from multiple-relapsed ALL were more drug resistant to: prednisolone (>1.9-fold), dexamethasone (>1.5-fold), vincristine (3.1-fold), L-asparaginase (5-fold), mitoxantrone (2.4-fold), cytarabine (4.3-fold), mercaptopurine (2.2-fold), thioguanine (4.8-fold), etoposide (2.6-fold) and melphalan (2.7-fold). Lymphoblasts at multiple relapse were comparably resistant to: daunorubicin, doxorubicin, cyclophosphamide, ifosfamide, busulfan, treosulfan, fludarabine, clofarabine and bortezomib.
CONCLUSION: In comparison to first relapse, subsequent relapsed childhood ALL is more ex vivo-resistant to most tested drugs.
PATIENTS AND METHODS: A total of 154 pediatric ALL samples were tested for ex vivo chemosensitivity for up to 19 drugs. Their combined drug resistance profile (PVA score) was analyzed.
RESULTS: The median relative resistance scores between patients with multiple relapse and those with first relapse considering all drugs was 2.0. The median PVA score at subsequent relapses was 8 vs. 6 at first relapse (p=0.004). Samples from multiple-relapsed ALL were more drug resistant to: prednisolone (>1.9-fold), dexamethasone (>1.5-fold), vincristine (3.1-fold), L-asparaginase (5-fold), mitoxantrone (2.4-fold), cytarabine (4.3-fold), mercaptopurine (2.2-fold), thioguanine (4.8-fold), etoposide (2.6-fold) and melphalan (2.7-fold). Lymphoblasts at multiple relapse were comparably resistant to: daunorubicin, doxorubicin, cyclophosphamide, ifosfamide, busulfan, treosulfan, fludarabine, clofarabine and bortezomib.
CONCLUSION: In comparison to first relapse, subsequent relapsed childhood ALL is more ex vivo-resistant to most tested drugs.
Boztug H, Sykora KW, Slatter M, et al.
European Society for Blood and Marrow Transplantation Analysis of Treosulfan Conditioning Before Hematopoietic Stem Cell Transplantation in Children and Adolescents With Hematological Malignancies.
Pediatr Blood Cancer. 2016; 63(1):139-48 [PubMed] Related Publications
European Society for Blood and Marrow Transplantation Analysis of Treosulfan Conditioning Before Hematopoietic Stem Cell Transplantation in Children and Adolescents With Hematological Malignancies.
Pediatr Blood Cancer. 2016; 63(1):139-48 [PubMed] Related Publications
BACKGROUND: Standard myeloablative conditioning regimens for children with hematological malignancies undergoing allogeneic HSCT are based mainly on total body irradiation or busulfan. Their serious short- and long-term side effects warranted the exploration of less toxic alternatives. Treosulfan is increasingly used for adults and children before HSCT due to its potent immunosuppressive and cytotoxic effects combined with low organ toxicity.
PROCEDURE: To further investigate the role of treosulfan conditioning in children, the EBMT Pediatric diseases working party performed a retrospective analysis of 193 children with hematological malignancies (ALL n = 71, AML n = 47, MDS/MPS n = 40, other leukemia/lymphoma n = 25) undergoing allogeneic HSCT following treosulfan between January 2005 and July 2010.
RESULTS: Early regimen-related toxicity was low and mainly gastrointestinal. Veno-occlusive disease and neurological toxicity were rare. There was no association of toxicity with type of disease or treosulfan dose. High-grade early toxicity was not higher in infants or patients undergoing second or later transplantation. Treatment related mortality was low at 14%. Three-year event-free survival was 45 ± 4% and not significantly influenced by number of transplants, however it appeared to be significantly better for infants (P = 0.022). When compared to treosulfan plus fludarabine, the combination of treosulfan, fludarabine and an alkylator (either thiotepa or melphalan) resulted in significantly better overall survival (OS, P = 0.048) and a trend toward better EFS.
CONCLUSIONS: Treosulfan based conditioning is a safe and effective approach for children with hematological malignancies, including and importantly for infants and those patients undergoing second or later transplantation.
PROCEDURE: To further investigate the role of treosulfan conditioning in children, the EBMT Pediatric diseases working party performed a retrospective analysis of 193 children with hematological malignancies (ALL n = 71, AML n = 47, MDS/MPS n = 40, other leukemia/lymphoma n = 25) undergoing allogeneic HSCT following treosulfan between January 2005 and July 2010.
RESULTS: Early regimen-related toxicity was low and mainly gastrointestinal. Veno-occlusive disease and neurological toxicity were rare. There was no association of toxicity with type of disease or treosulfan dose. High-grade early toxicity was not higher in infants or patients undergoing second or later transplantation. Treatment related mortality was low at 14%. Three-year event-free survival was 45 ± 4% and not significantly influenced by number of transplants, however it appeared to be significantly better for infants (P = 0.022). When compared to treosulfan plus fludarabine, the combination of treosulfan, fludarabine and an alkylator (either thiotepa or melphalan) resulted in significantly better overall survival (OS, P = 0.048) and a trend toward better EFS.
CONCLUSIONS: Treosulfan based conditioning is a safe and effective approach for children with hematological malignancies, including and importantly for infants and those patients undergoing second or later transplantation.
Kröger N, Bornhäuser M, Stelljes M, et al.
Allogeneic stem cell transplantation after conditioning with treosulfan, etoposide and cyclophosphamide for patients with ALL: a phase II-study on behalf of the German Cooperative Transplant Study Group and ALL Study Group (GMALL).
Bone Marrow Transplant. 2015; 50(12):1503-7 [PubMed] Related Publications
Allogeneic stem cell transplantation after conditioning with treosulfan, etoposide and cyclophosphamide for patients with ALL: a phase II-study on behalf of the German Cooperative Transplant Study Group and ALL Study Group (GMALL).
Bone Marrow Transplant. 2015; 50(12):1503-7 [PubMed] Related Publications
TBI-based preparative regimens are considered as standard conditioning therapy for allogeneic stem cell transplantation (AHSC) in patients with ALL. We investigated toxicity and efficacy of a non-TBI-based regimen consisting of treosulfan, etoposide and cyclophosphamide for ALL within a prospective study. Major inclusion criteria were CR and non-eligibility for TBI. Fifty patients with a median age of 46.5 years (range, 18-64) were included. Donors were HLA-identical sibling (n=8), matched (n=42) or mismatched (n=10) unrelated. The toxicity was moderate, resulting in a cumulative incidence of non-relapse mortality (NRM) at 1 year of 8% (90% confidence interval: 2-15%). Acute GvHD grade II-IV and grade III/IV was noted in 53% and 14%, respectively. Chronic GvHD at one year was seen in 41%. After a median follow-up of 24 months the cumulative incidence of relapse was 36% (90% confidence interval: 24-48) and 51% (90% confidence interval: 37-65) at 1 and 2 years, respectively. The estimated 2-year disease-free and overall survivals were 36 and 48%, respectively. Treosulfan, etoposide and cyclophosphamide followed by AHSC has a favorable toxicity profile with low NRM and therefore represents a potential alternative regimen for ALL in 1. CR (NCT00682305).
Yerushalmi R, Shem-Tov N, Danylesko I, et al.
Fludarabine and treosulfan compared with other reduced-intensity conditioning regimens for allogeneic stem cell transplantation in patients with lymphoid malignancies.
Bone Marrow Transplant. 2015; 50(12):1526-35 [PubMed] Related Publications
Fludarabine and treosulfan compared with other reduced-intensity conditioning regimens for allogeneic stem cell transplantation in patients with lymphoid malignancies.
Bone Marrow Transplant. 2015; 50(12):1526-35 [PubMed] Related Publications
Allogeneic stem-cell transplantation (SCT) is a potentially curative therapy for lymphoid malignancies. Myeloablative conditioning is associated with high non-relapse mortality (NRM). Reduced-intensity condition (RIC) reduces NRM but relapse rate is increased. Novel regimens with intensive anti-malignancy activity but limited toxicity are of benefit. We evaluated outcomes of 144 lymphoma patients given allogeneic SCT with RIC consisting of fludarabine and treosulfan (FT, n=50), intravenous-busulfan (FB2, n=38) or melphalan (FM, n=56). Sixty-nine patients (48%) had chemo-sensitive disease and 75 (52%) had chemo-refractory disease at SCT. The median follow-up is 39 months (4-149). Three-year survival was 67, 74 and 48% after FT, FB2 and FM, in chemo-sensitive disease (P=0.14) and 34, 11 and 17% in chemo-refractory disease, respectively (P=0.08). Three-year NRM was 24, 24 and 54% (P=0.002), whereas relapse mortality was 22, 34 and 18%, respectively (P=0.13). Multivariate analysis identified a high comorbidity-score, chemo-refractory disease and FM as associated with shortened survival. In conclusion, FB2 is associated with low NRM and good results in chemo-sensitive disease, but with higher relapse mortality rates. FM controls disease better, but with high NRM. FT probably balances these outcomes more optimally. It is as safe as FB2 and as cytoreductive as FM, resulting in improved outcome, mostly in advanced disease.
Baronciani D, Depau C, Targhetta C, et al.
Treosulfan-fludarabine-thiotepa conditioning before allogeneic haemopoietic stem cell transplantation for patients with advanced lympho-proliferative disease. A single centre study.
Hematol Oncol. 2016; 34(1):17-21 [PubMed] Related Publications
Treosulfan-fludarabine-thiotepa conditioning before allogeneic haemopoietic stem cell transplantation for patients with advanced lympho-proliferative disease. A single centre study.
Hematol Oncol. 2016; 34(1):17-21 [PubMed] Related Publications
In recent years, with the aim of reducing transplant-related mortality, new conditioning regimens have been explored in patients not eligible for conventional haemopoietic stem cell transplantation. In this setting, we investigated safety and feasibility of the treosulfan-fludarabine-thiotepa combination prior to allogeneic haemopoietic stem cell transplantation in patients with advanced lympho-proliferative diseases and at high transplant risk. Twenty-seven consecutive patients, median age 43 years (range 19-60), entered this study. All of them were affected by lympho-proliferative disease in advanced phase and have been heavily pre-treated. The median haemopoietic stem cell transplant co-morbidity index was 1 (range 0-3). Twenty-five patients had regular engraftment, while the remaining two patients were not evaluable for early deaths. Non-haematological toxicity was limited. No patient developed veno-occlusive disease. The estimated probability of overall survival and progression-free survival with a median follow-up of 40 months was 52% (95% confidence interval 33-73) and 50% (95% confidence interval 30-70) respectively. Six patients have relapsed; all of them were not in remission before transplantation. The treosulfan-fludarabine-thiotepa combination is a reduced toxicity but myeloablative regimen that can be proposed to patients not fitting criteria for conventional myeloablative transplant regimens. Longer follow-up and prospective randomized studies are necessary to evaluate this regimen.
Michelagnoli M, Whelan J, Forsyth S,
A phase II study to determine the efficacy and safety of oral treosulfan in patients with advanced pre-treated Ewing sarcoma ISRCTN11631773.
Pediatr Blood Cancer. 2015; 62(1):158-9 [PubMed] Related Publications
A phase II study to determine the efficacy and safety of oral treosulfan in patients with advanced pre-treated Ewing sarcoma ISRCTN11631773.
Pediatr Blood Cancer. 2015; 62(1):158-9 [PubMed] Related Publications
We report a prospective Phase II study of efficacy and toxicity for oral treosulfan in advanced Ewing sarcoma. Twenty patients, median age 19 years (range 7-39) from five UK sites, were treated with oral treosulfan 1 g/m(2) daily for 7 days in 28. Primary endpoint was objective response rate. Best response was stable disease in one patient. All patients died of progressive disease, after median 6.41 months. Median progression free survival was 1.8 months. Toxicity was minimal. No activity was demonstrated for treosulfan at this dose. Progression free survival data should be able to be used for comparison when planning future clinical trials.
Jahnke HG, Poenick S, Maschke J, et al.
Direct chemosensitivity monitoring ex vivo on undissociated melanoma tumor tissue by impedance spectroscopy.
Cancer Res. 2014; 74(22):6408-18 [PubMed] Related Publications
Direct chemosensitivity monitoring ex vivo on undissociated melanoma tumor tissue by impedance spectroscopy.
Cancer Res. 2014; 74(22):6408-18 [PubMed] Related Publications
Stage III/IV melanoma remains incurable in most cases due to chemotherapeutic resistance. Thus, predicting and monitoring chemotherapeutic responses in this setting offer great interest. To overcome limitations of existing assays in evaluating the chemosensitivity of dissociated tumor cells, we developed a label-free monitoring system to directly analyze the chemosensitivity of undissociated tumor tissue. Using a preparation of tumor micro-fragments (TMF) established from melanoma biopsies, we characterized the tissue organization and biomarker expression by immunocytochemistry. Robust generation of TMF was established successfully and demonstrated on a broad range of primary melanoma tumors and tumor metastases. Organization and biomarker expression within the TMF were highly comparable with tumor tissue, in contrast to dissociated, cultivated tumor cells. Using isolated TMF, sensitivity to six clinically relevant chemotherapeutic drugs (dacarbazine, doxorubicin, paclitaxel, cisplatin, gemcitabine, and treosulfan) was determined by impedance spectroscopy in combination with a unique microcavity array technology we developed. In parallel, comparative analyses were performed on monolayer tumor cell cultures. Lastly, we determined the efficacy of chemotherapeutic agents on TMF by impedance spectroscopy to obtain individual chemosensitivity patterns. Our results demonstrated nonpredictable differences in the reaction of tumor cells to chemotherapy in TMF by comparison with dissociated, cultivated tumor cells. Our direct impedimetric analysis of melanoma biopsies offers a direct ex vivo system to more reliably predict patient-specific chemosensitivity patterns and to monitor antitumor efficacy.
Boztug H, Zecca M, Sykora KW, et al.
Treosulfan-based conditioning regimens for allogeneic HSCT in children with acute lymphoblastic leukaemia.
Ann Hematol. 2015; 94(2):297-306 [PubMed] Related Publications
Treosulfan-based conditioning regimens for allogeneic HSCT in children with acute lymphoblastic leukaemia.
Ann Hematol. 2015; 94(2):297-306 [PubMed] Related Publications
Standard myeloablative conditioning regimens for children with acute lymphoblastic leukaemia are based on total body irradiation (TBI). However, TBI causes profound short-term and long-term side effects, provoking the necessity for alternative regimens. Treosulfan combines a potent immunosuppressive and antileukaemic effect with myeloablative activity and low toxicity profile. We retrospectively studied toxicity and outcome of 71 paediatric patients with acute lymphoblastic leukaemia (ALL) undergoing haematopoietic stem cell transplantation (HSCT) following treosulfan-based conditioning aiming to identify risk factors for treatment failure and dose-depending outcome differences. Early regimen-related toxicity was low. No case of veno-occlusive disease was reported. There was no association of toxicity with age or number of HSCT. Event-free survival (EFS) of infants was significantly better compared to older children. Overall survival (OS) at 3 years was 51 % and not significantly influenced by number of HSCT (first HSCT 54 %, ≥second HSCT 44 %, p = 0.71). In multivariate analysis, OS and EFS were significantly worse for patients transplanted without complete remission (p = 0.04 and 0.004). Treatment-related mortality was low at 14 %. We conclude that treosulfan-based conditioning is a safe and efficacious approach for paediatric ALL.
Radujkovic A, Luft T, Dreger P, et al.
In vitro testing of drug combinations employing nilotinib and alkylating agents with regard to pretransplant conditioning treatment of advanced-phase chronic myeloid leukemia.
Cancer Chemother Pharmacol. 2014; 74(2):427-32 [PubMed] Related Publications
In vitro testing of drug combinations employing nilotinib and alkylating agents with regard to pretransplant conditioning treatment of advanced-phase chronic myeloid leukemia.
Cancer Chemother Pharmacol. 2014; 74(2):427-32 [PubMed] Related Publications
PURPOSE: The prognosis of patients with advanced-phase chronic myeloid leukemia (CML) remains dismal despite the availability of targeted therapies and allogeneic stem cell transplantation (allo-SCT). Increasing the antileukemic efficacy of the pretransplant conditioning regimen may be a strategy to increase remission rates and duration. We therefore investigated the antiproliferative effects of nilotinib in combination with drugs that are usually used for conditioning: the alkylating agents mafosfamide, treosulfan, and busulfan.
METHODS: Drug combinations were tested in vitro in different imatinib-sensitive and imatinib-resistant BCR-ABL-positive cell lines. A tetrazolium-based MTT assay was used for the assessment and quantification of growth inhibition after exposure to alkylating agents alone or to combinations with nilotinib. Drug interaction was analyzed using the median-effect method of Chou and Talalay, and combination index (CI) values were calculated according to the classic isobologram equation.
RESULTS: Treatment of imatinib-sensitive, BCR-ABL-positive K562 and LAMA84 cells with nilotinib in combination with mafosfamide, treosulfan, or busulfan resulted in synergistic (CI < 1), additive (CI ~ 1), and predominantly antagonistic (CI > 1) effects, respectively. In imatinib-resistant K562-R and LAMA84-R cells, all applied drug combinations were synergistic (CI < 1) at higher growth inhibition levels.
CONCLUSIONS: Our in vitro data warrant further investigation and may provide the basis for nilotinib-supplemented conditioning regimens for allo-SCT in advanced-phase CML.
METHODS: Drug combinations were tested in vitro in different imatinib-sensitive and imatinib-resistant BCR-ABL-positive cell lines. A tetrazolium-based MTT assay was used for the assessment and quantification of growth inhibition after exposure to alkylating agents alone or to combinations with nilotinib. Drug interaction was analyzed using the median-effect method of Chou and Talalay, and combination index (CI) values were calculated according to the classic isobologram equation.
RESULTS: Treatment of imatinib-sensitive, BCR-ABL-positive K562 and LAMA84 cells with nilotinib in combination with mafosfamide, treosulfan, or busulfan resulted in synergistic (CI < 1), additive (CI ~ 1), and predominantly antagonistic (CI > 1) effects, respectively. In imatinib-resistant K562-R and LAMA84-R cells, all applied drug combinations were synergistic (CI < 1) at higher growth inhibition levels.
CONCLUSIONS: Our in vitro data warrant further investigation and may provide the basis for nilotinib-supplemented conditioning regimens for allo-SCT in advanced-phase CML.
Rasper M, Jabar S, Ranft A, et al.
The value of high-dose chemotherapy in patients with first relapsed Ewing sarcoma.
Pediatr Blood Cancer. 2014; 61(8):1382-6 [PubMed] Related Publications
The value of high-dose chemotherapy in patients with first relapsed Ewing sarcoma.
Pediatr Blood Cancer. 2014; 61(8):1382-6 [PubMed] Related Publications
BACKGROUND: Prognosis of patients with relapsed Ewing sarcoma (ES) is poor. The 5-year overall survival (OS) is 13%. We analyzed high-dose chemotherapy (HDtx) versus conventional chemotherapy (CHtx) in patients with relapsed ES.
PROCEDURE: Data from 239 patients with first relapse, registered during 2000-2011 in the ES relapse registry of the Cooperative Ewing Sarcoma Study Group (CESS) were analyzed.
RESULTS: Of 239 patients, 200 received various non-HDtx second-line CHtx regimens. Seventy-three patients had additional HDtx followed by autologous stem cell rescue. The 2-year event-free survival (EFS) was 10% (SE = 0.02) in patients treated without HDtx and 45% (SE = 0.09) in patients treated with HDtx. In a second step, we focused on those patients who achieved complete remission (CR) or partial remission (PR) after four to six cycles of conventional second-line CHtx. Here, the 2-year EFS was 31% (SE = 0.08) without additional HDtx and 44% (SE = 0.09) with additional HDtx. In addition, multivariate regression analysis indicates absence of HDtx treatment, with a Hazard ratio (HR) of 2.90 (95% CI 1.41-6.0), and early relapse, with a HR of 4.76 (95% CI 2.31-9.78), as independent prognostic factors for EFS.
CONCLUSION: Additional HDtx may contribute to further reduce the risk of further events in patients who respond to conventional second-line CHtx.
PROCEDURE: Data from 239 patients with first relapse, registered during 2000-2011 in the ES relapse registry of the Cooperative Ewing Sarcoma Study Group (CESS) were analyzed.
RESULTS: Of 239 patients, 200 received various non-HDtx second-line CHtx regimens. Seventy-three patients had additional HDtx followed by autologous stem cell rescue. The 2-year event-free survival (EFS) was 10% (SE = 0.02) in patients treated without HDtx and 45% (SE = 0.09) in patients treated with HDtx. In a second step, we focused on those patients who achieved complete remission (CR) or partial remission (PR) after four to six cycles of conventional second-line CHtx. Here, the 2-year EFS was 31% (SE = 0.08) without additional HDtx and 44% (SE = 0.09) with additional HDtx. In addition, multivariate regression analysis indicates absence of HDtx treatment, with a Hazard ratio (HR) of 2.90 (95% CI 1.41-6.0), and early relapse, with a HR of 4.76 (95% CI 2.31-9.78), as independent prognostic factors for EFS.
CONCLUSION: Additional HDtx may contribute to further reduce the risk of further events in patients who respond to conventional second-line CHtx.
Nitsch E, Mina S, Brammer I, et al.
Synergistic cytotoxic activity of treosulfan and gemcitabine in pancreatic cancer cell lines.
Anticancer Res. 2014; 34(4):1779-84 [PubMed] Related Publications
Synergistic cytotoxic activity of treosulfan and gemcitabine in pancreatic cancer cell lines.
Anticancer Res. 2014; 34(4):1779-84 [PubMed] Related Publications
BACKGROUND: Treatment for advanced pancreatic cancer is still very unsatisfactory. Treosulfan is an alkylating agent used for conventional, as well as high-dose chemotherapy regimens, whereby plasma concentrations over 500 μg/ml can be achieved. We investigated the effects of treosulfan on pancreatic cancer cell lines.
MATERIALS AND METHODS: Using Panc-1, MIA PaCa-2 and Capan-2 cell lines, we investigated the in vitro cytotoxicity of treosulfan-alone and in combination with gemcitabine, 5-fluorouracil or irradiation.
RESULTS: Treosulfan was potently cytotoxic against all pancreatic cancer cell lines at all concentrations (1-100 μg/ml). Combination of treosulfan and gemcitabine revealed strong synergistic effects independent of the sequence of drug administration. Similarly, synergism was observed with irradiation. Combination of treosulfan and 5-fluorouracil revealed antagonism.
CONCLUSION: Treosulfan effectively kills pancreatic carcinoma cells in vitro and has synergistic activity in combination with gemcitabine and irradiation. These results warrant further investigation of treosulfan in the treatment of pancreatic cancer.
MATERIALS AND METHODS: Using Panc-1, MIA PaCa-2 and Capan-2 cell lines, we investigated the in vitro cytotoxicity of treosulfan-alone and in combination with gemcitabine, 5-fluorouracil or irradiation.
RESULTS: Treosulfan was potently cytotoxic against all pancreatic cancer cell lines at all concentrations (1-100 μg/ml). Combination of treosulfan and gemcitabine revealed strong synergistic effects independent of the sequence of drug administration. Similarly, synergism was observed with irradiation. Combination of treosulfan and 5-fluorouracil revealed antagonism.
CONCLUSION: Treosulfan effectively kills pancreatic carcinoma cells in vitro and has synergistic activity in combination with gemcitabine and irradiation. These results warrant further investigation of treosulfan in the treatment of pancreatic cancer.
Legert KG, Remberger M, Ringdén O, et al.
Reduced intensity conditioning and oral care measures prevent oral mucositis and reduces days of hospitalization in allogeneic stem cell transplantation recipients.
Support Care Cancer. 2014; 22(8):2133-40 [PubMed] Related Publications
Reduced intensity conditioning and oral care measures prevent oral mucositis and reduces days of hospitalization in allogeneic stem cell transplantation recipients.
Support Care Cancer. 2014; 22(8):2133-40 [PubMed] Related Publications
PURPOSE: Oral mucositis (OM) is a side effect of intensive chemotherapy and radiation and has been reported to affect 75-100% of hematopoietic stem cell transplantation (HSCT) recipients. The purpose of this study was to compare the incidence of OM in patients conditioned with myeloablative conditioning (MAC) to reduced-intensity conditioning (RIC) and to determine the effect of a new oral care protocol.
METHODS: The study involved 171 HSCT recipients, with hematological malignancies transplanted between 2007 and 2011. Median age of the patients was 50 years (range 12-71). Ninety-nine (58%) received RIC and 72 received MAC. Clinical features of OM were recorded from day -3 before to day +25 after HSCT using the World Health Organization (WHO) scoring system and the oral mucositis assessment score (OMAS).
RESULTS: Overall, 87% of the patients developed OM of any severity, which peaked on days 10-11. The mean WHO score was 1.7. In multivariate analysis, the severity of OM was associated with MAC (relative hazard (RH) 1.57, 95% confidence interval (CI) 1.37-1.80, p < 0.001), all donor-recipient gender combinations except female-to-male (RH = 1.26, 95% CI 1.10-1.4, p = 0.001), and early year of HSCT (RH = 0.84, 95%CI 0.7-0.96, p = 0.013). There was a correlation between long hospitalization and OM (day 15, r = 0.31, p < 0.001). There was a good correlation between the WHO and OMAS scoring systems for OM (r = 0.74, p < 0.001).
CONCLUSIONS: Oral mucositis was reduced in patients treated with RIC and in patients treated during recent years, when oral care was intensified. Increased scores of OM prolonged hospitalization.
METHODS: The study involved 171 HSCT recipients, with hematological malignancies transplanted between 2007 and 2011. Median age of the patients was 50 years (range 12-71). Ninety-nine (58%) received RIC and 72 received MAC. Clinical features of OM were recorded from day -3 before to day +25 after HSCT using the World Health Organization (WHO) scoring system and the oral mucositis assessment score (OMAS).
RESULTS: Overall, 87% of the patients developed OM of any severity, which peaked on days 10-11. The mean WHO score was 1.7. In multivariate analysis, the severity of OM was associated with MAC (relative hazard (RH) 1.57, 95% confidence interval (CI) 1.37-1.80, p < 0.001), all donor-recipient gender combinations except female-to-male (RH = 1.26, 95% CI 1.10-1.4, p = 0.001), and early year of HSCT (RH = 0.84, 95%CI 0.7-0.96, p = 0.013). There was a correlation between long hospitalization and OM (day 15, r = 0.31, p < 0.001). There was a good correlation between the WHO and OMAS scoring systems for OM (r = 0.74, p < 0.001).
CONCLUSIONS: Oral mucositis was reduced in patients treated with RIC and in patients treated during recent years, when oral care was intensified. Increased scores of OM prolonged hospitalization.
Gyurkocza B, Gutman J, Nemecek ER, et al.
Treosulfan, fludarabine, and 2-Gy total body irradiation followed by allogeneic hematopoietic cell transplantation in patients with myelodysplastic syndrome and acute myeloid leukemia.
Biol Blood Marrow Transplant. 2014; 20(4):549-55 [PubMed] Free Access to Full Article Related Publications
Treosulfan, fludarabine, and 2-Gy total body irradiation followed by allogeneic hematopoietic cell transplantation in patients with myelodysplastic syndrome and acute myeloid leukemia.
Biol Blood Marrow Transplant. 2014; 20(4):549-55 [PubMed] Free Access to Full Article Related Publications
Allogeneic hematopoietic cell transplantation (HCT) offers curative therapy for many patients with myelodysplastic syndrome (MDS) or acute myeloid leukemia (AML). However, post-HCT relapse remains a major problem, particularly in patients with high-risk cytogenetics. In this prospective phase II trial, we assessed the efficacy and toxicity of treosulfan, fludarabine, and 2 Gy total body irradiation (TBI) as conditioning for allogeneic HCT in patients with MDS or AML. Ninety-six patients with MDS (n = 36: 15 refractory cytopenia with multilineage dysplasia, 10 refractory anemia with excess blasts type 1, 10 refractory anemia with excess blasts type 2, 1 chronic myelomonocytic leukemia type 1) or AML (n = 60: 35 first complete remission [CR], 18 second CR, 3 advanced CR, 4 refractory relapse) were enrolled; median age was 51 (range, 1 to 60) years. Twelve patients had undergone a prior HCT with high-intensity conditioning. Patients received 14 g/m(2)/day treosulfan i.v. on days -6 to -4, 30 mg/m(2)/day fludarabine i.v. on days -6 to -2, and 2 Gy TBI on day 0, followed by infusion of hematopoietic cells from related (n = 27) or unrelated (n = 69) donors. Graft-versus-host disease prophylaxis consisted of tacrolimus and methotrexate. With a median follow-up of 30 months, the 2-year overall survival (OS), relapse incidence, and nonrelapse mortality were 73%, 27%, and 8%, respectively. The incidences of grades II to IV (III to IV) acute and chronic graft-versus-host disease were 59% (10%) and 47%, respectively. Two-year OS was not significantly different between MDS patients with poor-risk and good/intermediate-risk cytogenetics (69% and 85%, respectively) or between AML patients with unfavorable and favorable/intermediate-risk cytogenetics (64% and 76%, respectively). In AML patients, minimal residual disease (MRD; n = 10) at the time of HCT predicted higher relapse incidence (70% versus 18%) and lower OS (41% versus 79%) at 2 years, when compared with patients without MRD. In conclusion, treosulfan, fludarabine, and low-dose TBI provided effective conditioning for allogeneic HCT in patients with MDS or AML and resulted in low relapse incidence, regardless of cytogenetic risk. In patients with AML, MRD at the time of HCT remained a risk factor for post-HCT relapse.
Linz U, Ulus B, Neuloh G, et al.
Can in-vitro chemoresponse assays help find new treatment regimens for malignant gliomas?
Anticancer Drugs. 2014; 25(4):375-84 [PubMed] Related Publications
Can in-vitro chemoresponse assays help find new treatment regimens for malignant gliomas?
Anticancer Drugs. 2014; 25(4):375-84 [PubMed] Related Publications
Various in-vitro chemosensitivity and resistance assays (CSRAs) have been demonstrated to be helpful decision aids for non-neurological tumors. Here, we evaluated the performance characteristics of two CSRAs for glioblastoma (GB) cells. The chemoresponse of fresh GB cells from 30 patients was studied in vitro using the ATP tumor chemoresponse assay and the chemotherapy resistance assay (CTR-Test). Both assay platforms provided comparable results. Of seven different chemotherapeutic drugs and drug combinations tested in vitro, treosulfan plus cytarabine (TARA) was the most effective, followed by nimustine (ACNU) plus teniposide (VM26) and temozolomide (TMZ). Whereas ACNU/VM26 and TMZ have proven their clinical value for malignant gliomas in large randomized studies, TARA has not been successful in newly diagnosed gliomas. This seeming discrepancy between in vitro and clinical result might be explained by the pharmacological behavior of treosulfan. Our results show reasonable agreement between two cell-based CSRAs. They appear to confirm the clinical effectiveness of drugs used in GB treatment as long as pharmacological preconditions such as overcoming the blood-brain barrier are properly considered.


 Acute Myeloid Leukemia (AML)
Acute Myeloid Leukemia (AML)