Found this page useful?
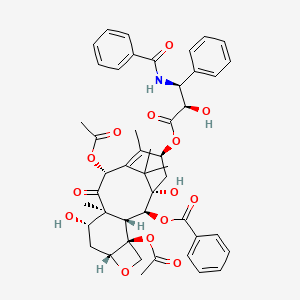
Abraxane
 Web Resources: Abraxane
Web Resources: Abraxane Recent Research Publications
Recent Research PublicationsWeb Resources: Abraxane (4 links)
Cancer Research UK
Macmillan Cancer Support
NHS Evidence
PubChem
Recent Research Publications
Xie F, De Clercq K, Vervaet C, et al.
Model-based analysis of treatment effects of paclitaxel microspheres in a microscopic peritoneal carcinomatosis model in mice.
Pharm Res. 2019; 36(9):127 [PubMed] Related Publications
Model-based analysis of treatment effects of paclitaxel microspheres in a microscopic peritoneal carcinomatosis model in mice.
Pharm Res. 2019; 36(9):127 [PubMed] Related Publications
PURPOSE: Paclitaxel (PTX)-loaded genipin-crosslinked gelatin microspheres (GP-MS) are a prolonged IP delivery system under development for the treatment of peritoneal minimal residual disease (pMRD). Here, we show the use of a pharmacokinetic-pharmacodynamic (PKPD) modelling approach to inform the formulation development of PTX-GP-MS in a mice pMRD model.
METHODS: PTX blood concentrations and survival data were obtained in Balb/c Nu mice receiving different single IP doses (7.5 and/or 35 mg/kg) of PTX-ethanolic loaded GP-MS (PTX
RESULTS: A PKPD model was developed that simultaneously describes the competing effects of treatment efficacy (driven by peritoneal concentration) and toxicity (driven by blood concentration) of PTX on survival. Clear survival advantages of PTX
CONCLUSIONS: The model predicts that the dose range of 7.5-15 mg/kg of PTX
METHODS: PTX blood concentrations and survival data were obtained in Balb/c Nu mice receiving different single IP doses (7.5 and/or 35 mg/kg) of PTX-ethanolic loaded GP-MS (PTX
RESULTS: A PKPD model was developed that simultaneously describes the competing effects of treatment efficacy (driven by peritoneal concentration) and toxicity (driven by blood concentration) of PTX on survival. Clear survival advantages of PTX
CONCLUSIONS: The model predicts that the dose range of 7.5-15 mg/kg of PTX
Tokunaga S, Takashima T, Kashiwagi S, et al.
Neoadjuvant Chemotherapy With Nab-paclitaxel Plus Trastuzumab Followed by 5-Fluorouracil/Epirubicin/Cyclophosphamide for HER2-positive Operable Breast Cancer: A Multicenter Phase II Trial.
Anticancer Res. 2019; 39(4):2053-2059 [PubMed] Related Publications
Neoadjuvant Chemotherapy With Nab-paclitaxel Plus Trastuzumab Followed by 5-Fluorouracil/Epirubicin/Cyclophosphamide for HER2-positive Operable Breast Cancer: A Multicenter Phase II Trial.
Anticancer Res. 2019; 39(4):2053-2059 [PubMed] Related Publications
AIM: This study was conducted in order to evaluate the efficacy and safety of nanoparticle albumin-bound paclitaxel (nab-paclitaxel) plus trastuzumab followed by 5-fluorouracil/ epirubicin/cyclophosphamide (FEC) in a neoadjuvant chemotherapy (NAC) setting for patients with human epidermal growth factor receptor 2 (HER2)-positive operable breast cancer.
PATIENTS AND METHODS: Each patient received four cycles of 260 mg/m
RESULTS: Twenty-nine patients were analyzed for the efficacy and safety of this treatment. All patients completed four cycles of nab-paclitaxel and trastuzumab, and 28 patients completed four cycles of FEC. Twenty-seven patients subsequently underwent surgery. The pCR rate was 74.0%. The most frequent toxicity was sensory neuropathy (96.6%), but grade 3 neuropathy rate was 3.4%.
CONCLUSION: Nab-paclitaxel plus trastuzumab followed by FEC in patients with HER2-positive operable breast cancer is considerably effective and well tolerated.
PATIENTS AND METHODS: Each patient received four cycles of 260 mg/m
RESULTS: Twenty-nine patients were analyzed for the efficacy and safety of this treatment. All patients completed four cycles of nab-paclitaxel and trastuzumab, and 28 patients completed four cycles of FEC. Twenty-seven patients subsequently underwent surgery. The pCR rate was 74.0%. The most frequent toxicity was sensory neuropathy (96.6%), but grade 3 neuropathy rate was 3.4%.
CONCLUSION: Nab-paclitaxel plus trastuzumab followed by FEC in patients with HER2-positive operable breast cancer is considerably effective and well tolerated.
Gao S, Zhu X, Shi X, et al.
Comparisons of different neoadjuvant chemotherapy regimens with or without stereotactic body radiation therapy for borderline resectable pancreatic cancer: study protocol of a prospective, randomized phase II trial (BRPCNCC-1).
Radiat Oncol. 2019; 14(1):52 [PubMed] Free Access to Full Article Related Publications
Comparisons of different neoadjuvant chemotherapy regimens with or without stereotactic body radiation therapy for borderline resectable pancreatic cancer: study protocol of a prospective, randomized phase II trial (BRPCNCC-1).
Radiat Oncol. 2019; 14(1):52 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Few patients with pancreatic cancer may be candidates for immediate surgical resection at the initial diagnosis. Even if patients with borderline resectable pancreatic cancer (BRPC), micrometastases may occur before surgery. Therefore, neoadjuvant therapy is vital for improved survival, which has been confirmed in previous studies that neoadjuvant chemotherapy with or without radiotherapy provides superior overall compared with upfront surgery. However, question of whether the addition of radiotherapy to neoadjuvant chemotherapy can improve prognosis compared with chemotherapy alone is a challenging matter. Moreover, most of previous studies only adopted conventional radiotherapy as the neoadjuvant modality though stereotactic body radiation therapy (SBRT) has been proven effective and commonly employed in pancreatic cancer. Also, no studies have evaluated the efficacy of S-1 as the neoadjuvant chemotherapy regimen for BRPC albeit similar prognosis has been found between S-1 and gemcitabine in advanced pancreatic cancer. Hence, the aim of this study is to investigate whether neoadjuvant chemotherapy plus SBRT results in better outcomes compared with neoadjuvant chemotherapy alone and also compare the efficacy of gemcitabine plus nab-paclitaxel with SBRT and S-1 plus nab-paclitaxel with SBRT.
METHODS: Patients with biopsy and radiographically confirmed BRPC, no prior treatment and severe morbidities are enrolled. They will be randomly allocated into three groups: neoadjuvant gemcitabine plus nab-paclitaxel, neoadjuvant gemcitabine plus nab-paclitaxel with SBRT and neoadjuvant S-1 plus nab-paclitaxel with SBRT. Standard doses of gemcitabine and nab-paclitaxel are used. The radiation dose of SBRT is 7.5-8Gy/f for 5 fractions. Surgical resection will be performed 3 weeks after SBRT. Artery first approach pancreaticoduodenectomy or radical antegrade modular pancreatosplenectomy will be used for the tumor in the head or body and tail of the pancreas, respectively. The primary endpoint is overall survival. The secondary outcomes are disease free survival, pathological complete response rate, R0 resection rate and incidence of adverse effects.
DISCUSSION: If results show the survival benefits of neoadjuvant chemotherapy plus SBRT and similar outcomes between S-1 and gemcitabine, it may provide evidence of clinical practice of this modality for BRPC.
TRIAL REGISTRATION: The study has been registered in ClinicalTrial.gov ( NCT03777462 ).
METHODS: Patients with biopsy and radiographically confirmed BRPC, no prior treatment and severe morbidities are enrolled. They will be randomly allocated into three groups: neoadjuvant gemcitabine plus nab-paclitaxel, neoadjuvant gemcitabine plus nab-paclitaxel with SBRT and neoadjuvant S-1 plus nab-paclitaxel with SBRT. Standard doses of gemcitabine and nab-paclitaxel are used. The radiation dose of SBRT is 7.5-8Gy/f for 5 fractions. Surgical resection will be performed 3 weeks after SBRT. Artery first approach pancreaticoduodenectomy or radical antegrade modular pancreatosplenectomy will be used for the tumor in the head or body and tail of the pancreas, respectively. The primary endpoint is overall survival. The secondary outcomes are disease free survival, pathological complete response rate, R0 resection rate and incidence of adverse effects.
DISCUSSION: If results show the survival benefits of neoadjuvant chemotherapy plus SBRT and similar outcomes between S-1 and gemcitabine, it may provide evidence of clinical practice of this modality for BRPC.
TRIAL REGISTRATION: The study has been registered in ClinicalTrial.gov ( NCT03777462 ).
Miyasaka Y, Ohtsuka T, Kimura R, et al.
Neoadjuvant Chemotherapy with Gemcitabine Plus Nab-Paclitaxel for Borderline Resectable Pancreatic Cancer Potentially Improves Survival and Facilitates Surgery.
Ann Surg Oncol. 2019; 26(5):1528-1534 [PubMed] Related Publications
Neoadjuvant Chemotherapy with Gemcitabine Plus Nab-Paclitaxel for Borderline Resectable Pancreatic Cancer Potentially Improves Survival and Facilitates Surgery.
Ann Surg Oncol. 2019; 26(5):1528-1534 [PubMed] Related Publications
BACKGROUND: Accumulation of evidence suggests that neoadjuvant chemotherapy improves the outcomes of borderline resectable pancreatic cancer (BRPC). Gemcitabine plus nab-paclitaxel (GnP) has been widely accepted as systemic chemotherapy for unresectable pancreatic cancer and reportedly results in remarkable tumor shrinkage. This study was performed to evaluate the safety and efficacy of neoadjuvant chemotherapy using neoadjuvant GnP for BRPC.
METHODS: The medical records of 57 patients who underwent treatment of BRPC from 2010 to 2017 were retrospectively reviewed. The patient characteristics and short- and intermediate-term outcomes were compared between the GnP and upfront surgery (UFS) groups.
RESULTS: The GnP group comprised 31 patients and the UFS group comprised 26 patients. The patient characteristics were comparable with the exception of a higher prevalence of arterial involvement in the GnP group. Twenty-seven of the 31 patients (87%) in the GnP group and all 26 patients in the UFS group underwent resection. The GnP group showed a significantly shorter operation time (429 vs. 509.5 min, p = 0.0068), less blood loss (760 vs. 1324 ml, p = 0.0115), and a higher R0 resection rate (100% vs. 77%, p = 0.0100) than the UFS group. Postoperative complications and hospital stay were comparable between the two groups, and no treatment-related mortality occurred in either group. Both the disease-free survival and overall survival times were significantly longer in the GnP group (p = 0.0018 and p = 0.0024, respectively).
CONCLUSIONS: Neoadjuvant GnP is a safe and effective treatment strategy for BRPC. It potentially improves patients' prognosis and facilitates surgical procedures.
METHODS: The medical records of 57 patients who underwent treatment of BRPC from 2010 to 2017 were retrospectively reviewed. The patient characteristics and short- and intermediate-term outcomes were compared between the GnP and upfront surgery (UFS) groups.
RESULTS: The GnP group comprised 31 patients and the UFS group comprised 26 patients. The patient characteristics were comparable with the exception of a higher prevalence of arterial involvement in the GnP group. Twenty-seven of the 31 patients (87%) in the GnP group and all 26 patients in the UFS group underwent resection. The GnP group showed a significantly shorter operation time (429 vs. 509.5 min, p = 0.0068), less blood loss (760 vs. 1324 ml, p = 0.0115), and a higher R0 resection rate (100% vs. 77%, p = 0.0100) than the UFS group. Postoperative complications and hospital stay were comparable between the two groups, and no treatment-related mortality occurred in either group. Both the disease-free survival and overall survival times were significantly longer in the GnP group (p = 0.0018 and p = 0.0024, respectively).
CONCLUSIONS: Neoadjuvant GnP is a safe and effective treatment strategy for BRPC. It potentially improves patients' prognosis and facilitates surgical procedures.
Nakashima K, Akamatsu H, Murakami H, et al.
Carboplatin Plus Nab-paclitaxel in Performance Status 2 Patients With Advanced Non-small-cell Lung Cancer.
Anticancer Res. 2019; 39(3):1463-1468 [PubMed] Related Publications
Carboplatin Plus Nab-paclitaxel in Performance Status 2 Patients With Advanced Non-small-cell Lung Cancer.
Anticancer Res. 2019; 39(3):1463-1468 [PubMed] Related Publications
BACKGROUND/AIM: This phase I/II study aimed at assessing the efficacy of combination therapy with carboplatin (CBDCA) on day 1 and nab-paclitaxel (Nab-PTX) on days 1 and 8 of a 21-day cycle in performance status (PS) 2 patients with non-small-cell lung cancer (NSCLC).
PATIENTS AND METHODS: PS 2 patients with NSCLC were enrolled into a phase I study using a 3 + 3 design. Once the recommended phase II dose (RP2D) was established, the patients were enrolled into phase II.
RESULTS: Based on the phase I findings, the RP2D was determined as CBDCA area under the curve 6 mg/ml/min and Nab-PTX 100 mg/m
CONCLUSION: CBDCA plus Nab-PTX therapy is a promising treatment strategy for PS 2 patients with NSCLC.
PATIENTS AND METHODS: PS 2 patients with NSCLC were enrolled into a phase I study using a 3 + 3 design. Once the recommended phase II dose (RP2D) was established, the patients were enrolled into phase II.
RESULTS: Based on the phase I findings, the RP2D was determined as CBDCA area under the curve 6 mg/ml/min and Nab-PTX 100 mg/m
CONCLUSION: CBDCA plus Nab-PTX therapy is a promising treatment strategy for PS 2 patients with NSCLC.
Sugiyama K, Kogure Y, Torii A, et al.
Solvent-based paclitaxel or nab-paclitaxel for heavily treated relapsed/refractory small cell lung cancer: Retrospective single-institution observational study.
Medicine (Baltimore). 2019; 98(9):e14758 [PubMed] Related Publications
Solvent-based paclitaxel or nab-paclitaxel for heavily treated relapsed/refractory small cell lung cancer: Retrospective single-institution observational study.
Medicine (Baltimore). 2019; 98(9):e14758 [PubMed] Related Publications
Treatment options for patients with relapsed/refractory small cell lung cancer (R/R SCLC) are limited, and the efficacy of salvage therapies for heavily treated patients should be assessed. Here, we evaluated the efficacy of paclitaxel (PTX) in R/R SCLC patients.A single-institute retrospective chart review was conducted. The primary endpoint was overall survival (OS), whereas the secondary endpoints were progression-free survival (PFS), overall response rate, disease control rate (DCR), and safety.Thirty-one patients (median age, 69 [range, 56-80] years) were analyzed. The median follow-up period was 122 (range, 28-1121) days. The median OS and PFS were 4.4 and 2.2 months, respectively. Adverse events of grade 3 or higher, other than hematological toxicity, were febrile neutropenia and neuropathy. Multivariate analyses identified the following independent predictors of poor OS: performance status and lactate dehydrogenase at the upper limit of normal.PTX monotherapy showed moderate efficacy with acceptable toxicity in heavily treated patients with R/R SCLC patients.
Sonbol MB, Ahn DH, Goldstein D, et al.
CanStem111P trial: a Phase III study of napabucasin plus nab-paclitaxel with gemcitabine.
Future Oncol. 2019; 15(12):1295-1302 [PubMed] Related Publications
CanStem111P trial: a Phase III study of napabucasin plus nab-paclitaxel with gemcitabine.
Future Oncol. 2019; 15(12):1295-1302 [PubMed] Related Publications
Napabucasin (also known as BBI-608 or BBI608) is an investigational, oral agent hypothesized to inhibit multiple oncogenic pathways. In this article, we describe the design and rationale for the CanStem111P clinical trial, a multicenter, randomized, open-label, Phase III study designed to determine the efficacy and safety of combining napabucasin with nab-paclitaxel and gemcitabine for first-line treatment of patients with metastatic pancreatic adenocarcinoma (NCT02993731). Patients were randomized in a 1:1 fashion to receive weekly gemcitabine and nab-paclitaxel with or without napabucasin. The results of this study will help define the role of this novel agent in the management of advanced pancreatic cancer.
Alavi M, Hamidi M
Passive and active targeting in cancer therapy by liposomes and lipid nanoparticles.
Drug Metab Pers Ther. 2019; 34(1) [PubMed] Related Publications
Passive and active targeting in cancer therapy by liposomes and lipid nanoparticles.
Drug Metab Pers Ther. 2019; 34(1) [PubMed] Related Publications
Considerable development in the application of injectable drug delivery systems for cancer therapy has occurred in the last few decades. These improvements include liposomes, lipid nanoparticles (LNPs), and other nanoparticles with or without macromolecular conjugates. For example, liposomal doxorubicin modified by poly(ethylene glycol) (Doxil) was the first liposome with anti-cancer effects which was approved by the US Food and Drug Administration, whereas Abraxane (modified albumin nanoparticles loaded by paclitaxel) was recently confirmed for the treatment of breast cancer. Recently, drug delivery systems by LNPs are an emerging technology with numerous advantages over conventional liposomes and chemotherapy using free drug treatment of cancer. These properties are biocompatibility, controlled and sustained release of anti-tumor drugs, and lower toxicity. Valuable experiments on these drug delivery systems offer better treatment of multidrug-resistant cancers and lower cardiotoxicity. LNPs have been presented with high functionality in chemotherapeutic targeting of breast and prostate cancer. The basis for this targeting behavior has been shown to be both passive and active targeting. The main objective of this review was an overview of the current position of the liposome-based drug delivery systems in targeted anticancer chemotherapy.
Specenier P
Efficacy of nab-paclitaxel in treating metastatic melanoma.
Expert Opin Pharmacother. 2019; 20(5):495-500 [PubMed] Related Publications
Efficacy of nab-paclitaxel in treating metastatic melanoma.
Expert Opin Pharmacother. 2019; 20(5):495-500 [PubMed] Related Publications
INTRODUCTION: Systemic treatment of metastatic melanoma has been revolutionized by the advent of checkpoint inhibitors and targeted agents which are widely accepted as standard front-line therapies. However, despite these major advances, a substantial portion of patients still fail checkpoint inhibitors and/or targeted agents and are not candidates for clinical trials. Commonly used cytotoxics in these patients include paclitaxel, dacarbazine, platins, and temozolomide. The overall response rates of these agents are usually disappointing and short-lived. Areas covered: Herein, the author provides a literature review of the role of nab-paclitaxel in metastatic melanoma including coverage of its pharmacokinetics, pharmacodynamics and efficacy. Expert opinion: The role of chemotherapy in the treatment of metastatic melanoma is limited to patients who failed checkpoint inhibitors and, when applicable, targeted agents, and those not appropriate for clinical trials. nab-Paclitaxel has single agent activity in chemotherapy-naïve untreated metastatic melanoma which compares favorably to the activity of weekly paclitaxel or single agent dacarbazine. However, the activity in chemotherapy-pretreated patients is modest. Data on nab-paclitaxel in patients pretreated with targeted agents or check point inhibitors are lacking. Further advances are expected from new checkpoint inhibitors and targeted agents for the treatment of metastatic melanoma in addition to the optimal combination and sequencing of these agents.
Raufi AG, Manji GA, Chabot JA, Bates SE
Neoadjuvant Treatment for Pancreatic Cancer.
Semin Oncol. 2019; 46(1):19-27 [PubMed] Related Publications
Neoadjuvant Treatment for Pancreatic Cancer.
Semin Oncol. 2019; 46(1):19-27 [PubMed] Related Publications
Pancreatic ductal adenocarcinoma (PDAC) is an aggressive malignancy with limited effective therapeutic options and exceedingly high mortality rates. Currently, cure can only be achieved through resection, however the vast majority of patients present with advanced disease for which upfront surgery is not an option. In an effort to improve surgical candidacy, neoadjuvant chemotherapy, with or without radiation therapy, is often used in an effort to downstage borderline resectable and locally advanced tumors, and some argue for its use even in patients with resectable tumors. Underlying this thinking is the recognition that pancreatic cancer is simultaneously both a locally invasive and systemic disease, even in patients without evidence of metastasis on imaging. Current evidence to date is largely retrospective, but suggests that neoadjuvant therapy can increase R0 (pathologically negative margin) resection rates and improve overall survival. The standard approach to neoadjuvant treatment involves choosing between the two most active combination regimens for metastatic disease, namely modified FOLFIRNOX and gemcitabine/nab-paclitaxel. Nonrandomized data indicate that these regimens can yield resection rates up to 68% and 36%, in borderline resectable and locally advanced PDAC, respectively. Furthermore, randomized data in patients with resectable PDAC treated with gemcitabine-based neoadjuvant therapy suggests that despite an approximate 10% drop in resection rates, there is a significant improvement in median overall survival. Herein, we will discuss the rationale for neoadjuvant therapy, current and former treatment regimens, common issues faced by clinicians when using these combinations, and several ongoing clinical trials.
Péron J, Giai J, Maucort-Boulch D, Buyse M
The Benefit-Risk Balance of Nab-Paclitaxel in Metastatic Pancreatic Adenocarcinoma.
Pancreas. 2019; 48(2):275-280 [PubMed] Related Publications
The Benefit-Risk Balance of Nab-Paclitaxel in Metastatic Pancreatic Adenocarcinoma.
Pancreas. 2019; 48(2):275-280 [PubMed] Related Publications
OBJECTIVES: The benefit-risk balance of 5-fluorouracil, oxaliplatin, irinotecan, and leucovorin versus gemcitabine assessed using generalized pairwise comparison was strongly positive. We sought to assess the benefit-risk balance of nab-paclitaxel plus gemcitabine using the data of the MPACT trial, as it is an alternative to 5-fluorouracil, oxaliplatin, irinotecan, and leucovorin.
METHODS: This statistical method allows for the simultaneous analysis of several prioritized outcomes. The first priority outcome was survival time (overall survival). The second priority outcome was toxicity. The overall treatment effect was quantified using the overall net benefit. Multiple sensitivity analyses were performed to assess the consistency of the results according to possible patients' preferences.
RESULTS: In this trial, 861 patients received nab-paclitaxel plus gemcitabine or gemcitabine alone. The overall net benefit favored strongly and significantly the combination group. When only large survival differences were considered clinically relevant, the net benefit was not in favor of the combination group.
CONCLUSIONS: The overall net benefit is a clinically intuitive way of comparing patients with respect to all important efficacy and toxicity outcomes. The nab-paclitaxel plus gemcitabine combination has a positive benefit-risk balance, but it might not be suitable for patients who would consider losing several months of survival to avoid a significant toxic event.
METHODS: This statistical method allows for the simultaneous analysis of several prioritized outcomes. The first priority outcome was survival time (overall survival). The second priority outcome was toxicity. The overall treatment effect was quantified using the overall net benefit. Multiple sensitivity analyses were performed to assess the consistency of the results according to possible patients' preferences.
RESULTS: In this trial, 861 patients received nab-paclitaxel plus gemcitabine or gemcitabine alone. The overall net benefit favored strongly and significantly the combination group. When only large survival differences were considered clinically relevant, the net benefit was not in favor of the combination group.
CONCLUSIONS: The overall net benefit is a clinically intuitive way of comparing patients with respect to all important efficacy and toxicity outcomes. The nab-paclitaxel plus gemcitabine combination has a positive benefit-risk balance, but it might not be suitable for patients who would consider losing several months of survival to avoid a significant toxic event.
Kono M, Sakurai T, Okamoto K, et al.
Efficacy and Safety of Chemotherapy Following Anti-PD-1 Antibody Therapy for Gastric Cancer: A Case of Sclerosing Cholangitis.
Intern Med. 2019; 58(9):1263-1266 [PubMed] Free Access to Full Article Related Publications
Efficacy and Safety of Chemotherapy Following Anti-PD-1 Antibody Therapy for Gastric Cancer: A Case of Sclerosing Cholangitis.
Intern Med. 2019; 58(9):1263-1266 [PubMed] Free Access to Full Article Related Publications
Immunotherapy targeting programmed cell death-1 (PD-1) signaling is becoming the standard of care for advanced gastric cancer. We herein report a patient with gastric adenocarcinoma with peritoneal dissemination who was treated with nab-paclitaxel and ramucirumab following nivolumab and developed sclerosing cholangitis. Endoscopic retrograde cholangiography showed irregular narrowing and widening of the entire intrahepatic biliary system. Intriguingly, the patient receiving second-line chemotherapy with nab-paclitaxel plus ramucirumab prior to being administered nivolumab, however, he had experienced progressive disease. Thereafter, the administration of fourth-line chemotherapy with nab-paclitaxel and ramucirumab following nivolumab resulted in a clinical response. Nivolumab may enhance the efficacy of the subsequent chemotherapy regimens but also induce sclerosing cholangitis.
Vogl UM, Andalibi H, Klaus A, et al.
Nab-paclitaxel and gemcitabine or FOLFIRINOX as first-line treatment in patients with unresectable adenocarcinoma of the pancreas: does sequence matter?
BMC Cancer. 2019; 19(1):28 [PubMed] Free Access to Full Article Related Publications
Nab-paclitaxel and gemcitabine or FOLFIRINOX as first-line treatment in patients with unresectable adenocarcinoma of the pancreas: does sequence matter?
BMC Cancer. 2019; 19(1):28 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Locally advanced or metastatic adenocarcinoma of the pancreas remains - despite the implementation of new chemotherapy protocols - a disease with short overall survival (OS).
METHODS: Eighty-three patients were treated with locally advanced or metastatic adenocarcinoma of the pancreas with either FOLFIRINOX or nab-Paclitxel and Gemcitabine (nabPGem) as first- or second line therapy. We analysed the outcome for OS and progression-free survival (PFS) in terms of treatment regimen and sequence.
RESULTS: The majority of patients presented in good performance status (PS) with a median age of 68 years. Fourty-two patients received FOLFIRINOX as first-line therapy, 41 patients were treated with nabPGem as first line therapy. Forty-eight patients received both treatments. The OS of all 83 patients was 12.6 months (95% CI: 10.7-14.6), resulting in a 1-year OS of 54%. Forty-eight patients received FOLFIRINOX followed by nabPGem or vice versa. There was no significant difference in OS or PFS for either of the two sequences (p = 0.9). The OS for FOLFIRINOX followed by nabPGem or nabPGem followed by FOLFIRINOX was 13.7 months (95% CI: 12.6-14.7) and 13.8 months (95% CI: 8.6-19), respectively.
CONCLUSIONS: The sequence FOLFIRINOX followed by nab-Paclitaxel and Gemcitabine or vice versa lead to an equal OS outcome.
METHODS: Eighty-three patients were treated with locally advanced or metastatic adenocarcinoma of the pancreas with either FOLFIRINOX or nab-Paclitxel and Gemcitabine (nabPGem) as first- or second line therapy. We analysed the outcome for OS and progression-free survival (PFS) in terms of treatment regimen and sequence.
RESULTS: The majority of patients presented in good performance status (PS) with a median age of 68 years. Fourty-two patients received FOLFIRINOX as first-line therapy, 41 patients were treated with nabPGem as first line therapy. Forty-eight patients received both treatments. The OS of all 83 patients was 12.6 months (95% CI: 10.7-14.6), resulting in a 1-year OS of 54%. Forty-eight patients received FOLFIRINOX followed by nabPGem or vice versa. There was no significant difference in OS or PFS for either of the two sequences (p = 0.9). The OS for FOLFIRINOX followed by nabPGem or nabPGem followed by FOLFIRINOX was 13.7 months (95% CI: 12.6-14.7) and 13.8 months (95% CI: 8.6-19), respectively.
CONCLUSIONS: The sequence FOLFIRINOX followed by nab-Paclitaxel and Gemcitabine or vice versa lead to an equal OS outcome.
Blomstrand H, Scheibling U, Bratthäll C, et al.
Real world evidence on gemcitabine and nab-paclitaxel combination chemotherapy in advanced pancreatic cancer.
BMC Cancer. 2019; 19(1):40 [PubMed] Free Access to Full Article Related Publications
Real world evidence on gemcitabine and nab-paclitaxel combination chemotherapy in advanced pancreatic cancer.
BMC Cancer. 2019; 19(1):40 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: In the recent phase III trial MPACT the combination of gemcitabine and nab-paclitaxel (Gem/NabP) showed increased overall survival compared to gemcitabine alone in the treatment of advanced pancreatic ductal adenocarcinoma (aPDA). Until now there has been limited information on the clinical benefit and toxicity of the combination regimen in a real world setting. In addition the value for patients with locally advanced rather than metastatic aPDA has been unclear, since the former category of patients was not included in the MPACT trial.
METHODS: A multicentre retrospective observational study in the South Eastern Region of Sweden was performed, with the first 75 consecutive patients diagnosed with aPDA (both locally advanced and metastatic disease) who received first-line treatment with Gem/NabP.
RESULTS: In the overall population median progression free survival (PFS) and overall survival (OS) were 5.2 (3.4-7.0 95% CI) and 10.9 (7.8-14.0 95% CI) months, respectively. Patients with metastatic disease displayed a median OS of 9.4 (4.9-13.9) and a median PFS of 4.5 (3.3-5.7) months whereas the same parameters in the locally advanced subgroup were 17.1 (7.6-26.6) and 6.8 (5.2-8.4) months, respectively. Grade 3-4 hematologic toxicity was recorded: Neutropenia, leukopenia, thrombocytopenia, and anaemia were observed in 23, 20, 5, and 4% of patients, respectively. Dose reductions were performed in 80% of the patients.
CONCLUSION: This study confirms the effectiveness and safety of first-line Gem/NabP in both locally advanced and metastatic PDA in a real world setting.
METHODS: A multicentre retrospective observational study in the South Eastern Region of Sweden was performed, with the first 75 consecutive patients diagnosed with aPDA (both locally advanced and metastatic disease) who received first-line treatment with Gem/NabP.
RESULTS: In the overall population median progression free survival (PFS) and overall survival (OS) were 5.2 (3.4-7.0 95% CI) and 10.9 (7.8-14.0 95% CI) months, respectively. Patients with metastatic disease displayed a median OS of 9.4 (4.9-13.9) and a median PFS of 4.5 (3.3-5.7) months whereas the same parameters in the locally advanced subgroup were 17.1 (7.6-26.6) and 6.8 (5.2-8.4) months, respectively. Grade 3-4 hematologic toxicity was recorded: Neutropenia, leukopenia, thrombocytopenia, and anaemia were observed in 23, 20, 5, and 4% of patients, respectively. Dose reductions were performed in 80% of the patients.
CONCLUSION: This study confirms the effectiveness and safety of first-line Gem/NabP in both locally advanced and metastatic PDA in a real world setting.
Higuchi T, Kawaguchi K, Miyake K, et al.
The combination of gemcitabine and nab-paclitaxel as a novel effective treatment strategy for undifferentiated soft-tissue sarcoma in a patient-derived orthotopic xenograft (PDOX) nude-mouse model.
Biomed Pharmacother. 2019; 111:835-840 [PubMed] Related Publications
The combination of gemcitabine and nab-paclitaxel as a novel effective treatment strategy for undifferentiated soft-tissue sarcoma in a patient-derived orthotopic xenograft (PDOX) nude-mouse model.
Biomed Pharmacother. 2019; 111:835-840 [PubMed] Related Publications
Undifferentiated/unclassified soft-tissue sarcomas (USTS) is recalcitrant neoplasms that is usually treated with doxorubicin (DOX)-containing regimens as first-line therapy. Nanoparticle albumin-bound paclitaxel (nab-PTX) is a nanotechnology-based drug and is widely used in pancreatic cancer in combination with gemcitabine (GEM). The major goal of the present study was to determine the efficacy of nab-PTX in combination with GEM, compared to conventional drugs such as docetaxel (DOC), GEM combined with DOC, or first-line drug DOX on a USTS not-otherwise specified (USTS/NOS) from a striated muscle implanted in the right biceps femoris muscle of nude mice to establish a patient-derived orthotopic xenograft (PDOX) model. USTS PDOX models were randomized into six groups: untreated control; DOX; DOC; nab-PTX; GEM combined with DOC; and GEM combined with nab-PTX. Tumor size and body weight were measured. Tumor growth was inhibited to the greatest extent by GEM combined with nab-PTX. Tumors treated with GEM combined with nab-PTX had the most necrosis. Body weight of the treated mice was not significantly different from the untreated controls. The present study demonstrates the power of the PDOX model to identify a novel effective treatment strategy of the combination of GEM and nab-PTX for recalcitrant soft-tissue sarcomas. These results suggest that combination of GEM and nab-PTX could be a promising therapeutic strategy for USTS.
Shi S, Yu X
Selecting chemotherapy for pancreatic cancer: Far away or so close?
Semin Oncol. 2019; 46(1):39-47 [PubMed] Related Publications
Selecting chemotherapy for pancreatic cancer: Far away or so close?
Semin Oncol. 2019; 46(1):39-47 [PubMed] Related Publications
Pancreatic cancer is a lethal disease with a very poor prognosis. In contrast to treatments for many other tumor types, cytotoxic agents are still the first-line drugs for pancreatic cancer in both the palliative and adjuvant settings. Some progress has been made in recent years, but most large phase 3 studies have not shown significant improvements in survival. Because the available drugs and regimens are limited in both type and effect, the selection of chemotherapy based on clinicopathologic characteristics may be consequential for pancreatic cancer. In the present report, we focused on 7 landmark clinical trials for pancreatic cancer. We observed that FOLFIRINOX (oxaliplatin, irinotecan, fluorouracil, and leucovorin) and NG (nab-paclitaxel and gemcitabine), 2 first-line regimens, exerted opposite effects on metastatic pancreatic cancer patients with different baseline carbohydrate antigen 19-9 (CA19-9) levels. This suggested that not only the performance status but possibly also CA19-9 levels should be considered when making a therapeutic choice for patients with advanced pancreatic cancer. Moreover, we found that patients with a diagnosis of pancreatic cancer who have undergone a surgical resection with a negative margin (R0) may benefit more from fluorouracil and/or oral prodrugs of fluorouracil-based adjuvant therapy than from gemcitabine. Conversely, gemcitabine or gemcitabine-based regimens may be more effective for patients with a positive resection margin (R1). Based on these findings, we propose flowcharts for selecting chemotherapy for both advanced and resected pancreatic cancer. Furthermore, we present possible mechanisms and interpretations underlying the selection of chemotherapy for pancreatic cancer and propose the tumor burden as a key variable in this process. Regardless of the possible bias and exact treatment selection process, this study offers an opportunity to improve patient outcomes by using agents currently used in the therapy of pancreatic cancer. Although these conclusions are based on indirect evidence, we provide insights and possibilities to drive the selection of chemotherapy for pancreatic cancer.
Tan H, Hu J, Liu S
Efficacy and safety of nanoparticle albumin-bound paclitaxel in non-small cell lung cancer: a systematic review and meta-analysis.
Artif Cells Nanomed Biotechnol. 2019; 47(1):268-277 [PubMed] Related Publications
Efficacy and safety of nanoparticle albumin-bound paclitaxel in non-small cell lung cancer: a systematic review and meta-analysis.
Artif Cells Nanomed Biotechnol. 2019; 47(1):268-277 [PubMed] Related Publications
Nanoparticle albumin-bound paclitaxel (Nab-paclitaxel) offer more efficient paclitaxel delivery into tumor cells with fewer side effects than conventional chemotherapies. However, whether the efficacy of Nab-paclitaxel for non-small cell lung cancer (NSCLC) patients is age-related remains unknown. We performed this meta-analysis to evaluate the anticancer efficacy and safety of Nab-paclitaxel in NSCLC. Hazard ratios (HRs) or rate ratios (RRs) with corresponding 95% confidence intervals (CIs) for outcomes were retrieved. Thirteen high-quality studies with 4613 patients were included, of which five were comparative trials comparing nab-paclitaxel plus carboplatin (nab-P/C) with solvent-based paclitaxel plus carboplatin (sb-P/C), and the others were non-comparative trials investigating the nab-paclitaxel efficacy. Pooled comparative trial estimates showed that nab-P/C significantly improved overall response rates ([RR]: 1.31) and prolonged progression-free survival (PFS) (HR: 0.89) and overall survival (OS) (HR: 0.93) compared with the control. However, meta-analysis of the younger subgroup indicated that PFS (HR: 93) and OS (HR: 96) were similar between the two arms. Regarding safety, nab-paclitaxel significantly increased risk for grade ≥3 anaemia. For non-hematological adverse events, grade ≥3 sensory neuropathy and arthralgia occurred more frequently in the control arm than in the experimental arm. In conclusion: Nab-paclitaxel is effective and safe for NSCLC patients, especially the elderly.
Ettrich TJ, Berger AW, Perkhofer L, et al.
Neoadjuvant plus adjuvant or only adjuvant nab-paclitaxel plus gemcitabine for resectable pancreatic cancer - the NEONAX trial (AIO-PAK-0313), a prospective, randomized, controlled, phase II study of the AIO pancreatic cancer group.
BMC Cancer. 2018; 18(1):1298 [PubMed] Free Access to Full Article Related Publications
Neoadjuvant plus adjuvant or only adjuvant nab-paclitaxel plus gemcitabine for resectable pancreatic cancer - the NEONAX trial (AIO-PAK-0313), a prospective, randomized, controlled, phase II study of the AIO pancreatic cancer group.
BMC Cancer. 2018; 18(1):1298 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Even clearly resectable pancreatic cancer still has an unfavorable prognosis. Neoadjuvant or perioperative therapies might improve the prognosis of these patients. Thus, evaluation of perioperative chemotherapy in resectable pancreatic cancer in a prospective, randomized trial is warranted. A substantial improvement in overall survival of patients with metastatic pancreatic cancer with FOLFIRINOX and nab-paclitaxel/gemcitabine vs standard gemcitabine has been demonstrated in phase III-trials. Indeed nab-paclitaxel/gemcitabine has a more favorable toxicity profile compared to the FOLFIRINOX protocol and appears applicable in a perioperative setting.
METHODS: NEONAX is an interventional, prospective, randomized, controlled, open label, two sided phase II study with an unconnected analysis of the results in both experimental arms against a fixed survival probability (38% at 18 months with adjuvant gemcitabine), NCT02047513. NEONAX will enroll 166 patients with resectable pancreatic ductal adenocarcinoma (≤ cT3, N0 or N1, cM0) in two arms: Arm A (perioperative arm): 2 cycles nab-paclitaxel (125 mg/m2)/gemcitabine (1000 mg/m2, d1, 8 and 15 of an 28 day-cycle) followed by tumor surgery followed by 4 cycles nab-paclitaxel/gemcitabine, Arm B (adjuvant arm): tumor surgery followed by 6 cycles nab-paclitaxel/gemcitabine. The randomization (1:1) is eminent to avoid allocation bias between the groups. Randomization is stratified for tumor stage (ct1/2 vs. cT3) and lymph node status (cN0 vs. cN1). Primary objective is disease free survival (DFS) at 18 months after randomization. Key secondary objectives are 3-year overall survival (OS) rate and DFS rate, progression during neoadjuvant therapy, R0 and R1 resection rate, quality of life and correlation of DFS, OS and tumor regression with pharmacogenomic markers, tumor biomarkers and molecular analyses (ctDNA, transcriptome, miRNA-arrays). In addition, circulating tumor-DNA will be analyzed in patients with the best and the worst responses to the neoadjuvant treatment. The study was initiated in March 2015 in 26 centers for pancreatic surgery in Germany.
DISCUSSION: The NEONAX trial is an innovative study on resectable pancreatic cancer and currently one of the largest trials in this field of research. It addresses the question of the role of intensified perioperative treatment with nab-paclitaxel plus gemcitabine in resectable pancreatic cancers to improve disease-free survival and offers a unique potential for translational research.
TRIAL REGISTRATION: ClinicalTrials.gov : NCT02047513, 08/13/2014.
METHODS: NEONAX is an interventional, prospective, randomized, controlled, open label, two sided phase II study with an unconnected analysis of the results in both experimental arms against a fixed survival probability (38% at 18 months with adjuvant gemcitabine), NCT02047513. NEONAX will enroll 166 patients with resectable pancreatic ductal adenocarcinoma (≤ cT3, N0 or N1, cM0) in two arms: Arm A (perioperative arm): 2 cycles nab-paclitaxel (125 mg/m2)/gemcitabine (1000 mg/m2, d1, 8 and 15 of an 28 day-cycle) followed by tumor surgery followed by 4 cycles nab-paclitaxel/gemcitabine, Arm B (adjuvant arm): tumor surgery followed by 6 cycles nab-paclitaxel/gemcitabine. The randomization (1:1) is eminent to avoid allocation bias between the groups. Randomization is stratified for tumor stage (ct1/2 vs. cT3) and lymph node status (cN0 vs. cN1). Primary objective is disease free survival (DFS) at 18 months after randomization. Key secondary objectives are 3-year overall survival (OS) rate and DFS rate, progression during neoadjuvant therapy, R0 and R1 resection rate, quality of life and correlation of DFS, OS and tumor regression with pharmacogenomic markers, tumor biomarkers and molecular analyses (ctDNA, transcriptome, miRNA-arrays). In addition, circulating tumor-DNA will be analyzed in patients with the best and the worst responses to the neoadjuvant treatment. The study was initiated in March 2015 in 26 centers for pancreatic surgery in Germany.
DISCUSSION: The NEONAX trial is an innovative study on resectable pancreatic cancer and currently one of the largest trials in this field of research. It addresses the question of the role of intensified perioperative treatment with nab-paclitaxel plus gemcitabine in resectable pancreatic cancers to improve disease-free survival and offers a unique potential for translational research.
TRIAL REGISTRATION: ClinicalTrials.gov : NCT02047513, 08/13/2014.
Sasaki T, Kanata R, Yamada I, et al.
Improvement of Treatment Outcomes for Metastatic Pancreatic Cancer: A Real-world Data Analysis.
In Vivo. 2019 Jan-Feb; 33(1):271-276 [PubMed] Free Access to Full Article Related Publications
Improvement of Treatment Outcomes for Metastatic Pancreatic Cancer: A Real-world Data Analysis.
In Vivo. 2019 Jan-Feb; 33(1):271-276 [PubMed] Free Access to Full Article Related Publications
BACKGROUND/AIM: FOLFIRINOX (5-fluorouracil, leucovorin, irinotecan, oxaliplatin) and gemcitabine plus nab-paclitaxel therapy have recently been introduced for the treatment of metastatic pancreatic cancer. Herein, overall treatment outcomes of metastatic pancreatic cancer after introduction of FOLFIRINOX and gemcitabine plus nab-paclitaxel therapy were evaluated, in daily practice.
PATIENTS AND METHODS: Metastatic pancreatic cancer patients (n=321) who started systemic chemotherapy between January 2011 and December 2016 were included and were divided into two groups: group A (2011-2013) and group B (2014-2016). Treatment outcomes were evaluated retrospectively.
RESULTS: Patient characteristics were similar between the two groups except for the rates of distant lymph node metastasis and peritoneal metastasis. The preferred regimens in groups A and B were gemcitabine monotherapy and gemcitabine plus nab-paclitaxel therapy, respectively. The response rates, median progression-free survival, and median overall survival of groups A and B were 7.8% and 28.4% (p<0.01), 3.1 months and 5.4 months (p<0.01), and 6.7 months and 10.2 months (p<0.01), respectively.
CONCLUSION: Overall treatment outcomes for metastatic pancreatic cancer were significantly improved after introduction of FOLFIRINOX and gemcitabine plus nab-paclitaxel combination therapy in daily practice.
PATIENTS AND METHODS: Metastatic pancreatic cancer patients (n=321) who started systemic chemotherapy between January 2011 and December 2016 were included and were divided into two groups: group A (2011-2013) and group B (2014-2016). Treatment outcomes were evaluated retrospectively.
RESULTS: Patient characteristics were similar between the two groups except for the rates of distant lymph node metastasis and peritoneal metastasis. The preferred regimens in groups A and B were gemcitabine monotherapy and gemcitabine plus nab-paclitaxel therapy, respectively. The response rates, median progression-free survival, and median overall survival of groups A and B were 7.8% and 28.4% (p<0.01), 3.1 months and 5.4 months (p<0.01), and 6.7 months and 10.2 months (p<0.01), respectively.
CONCLUSION: Overall treatment outcomes for metastatic pancreatic cancer were significantly improved after introduction of FOLFIRINOX and gemcitabine plus nab-paclitaxel combination therapy in daily practice.
Kashiwada T, Saito Y, Terasaki Y, et al.
Interstitial lung disease associated with nanoparticle albumin-bound paclitaxel treatment in patients with lung cancer.
Jpn J Clin Oncol. 2019; 49(2):165-173 [PubMed] Related Publications
Interstitial lung disease associated with nanoparticle albumin-bound paclitaxel treatment in patients with lung cancer.
Jpn J Clin Oncol. 2019; 49(2):165-173 [PubMed] Related Publications
Background: Nanoparticle albumin-bound paclitaxel is indicated for the treatment of patients with lung cancer. It can induce interstitial lung disease, but the incidence of nanoparticle albumin-bound paclitaxel-associated interstitial lung disease in clinical practice has not been determined. We investigated the incidence of interstitial lung disease in patients with lung cancer who had received nanoparticle albumin-bound paclitaxel therapy at our institution.
Methods: We reviewed clinical data for patients with advanced lung cancer who received nanoparticle albumin-bound paclitaxel with or without carboplatin or bevacizumab therapy at the Nippon Medical School Main Hospital between April 2013 and September 2017. Interstitial lung disease was diagnosed based on clinical symptoms, radiographic findings and exclusion of other diseases.
Results: A total of 110 advanced lung cancer patients received nanoparticle albumin-bound paclitaxel, and nine of them (8.2%) developed interstitial lung disease. Of those who developed interstitial lung disease, eight were treated with corticosteroids and three received cyclophosphamide pulse therapy. High-resolution computed tomography images demonstrated diffuse alveolar damage pattern pneumonitis in seven patients and organized pneumonia pattern pneumonitis in two patients. Six of the patients with diffuse alveolar damage pattern pneumonitis died from respiratory failure. The two patients with organized pneumonia pattern pneumonitis recovered. The incidence of interstitial lung disease was 19.0% (8/42) among patients with preexisting interstitial pneumonia and 1.5% (1/68) among those without preexisting interstitial pneumonia. Six patients with preexisting interstitial pneumonia met the criteria for acute exacerbation of interstitial pneumonia (14.3%).
Conclusion: Nanoparticle albumin-bound paclitaxel-associated interstitial lung disease was a severe and potentially fatal adverse event. We found it demonstrated diffuse alveolar damage or organized pneumonia pattern pneumonitis, and preexisting interstitial pneumonia was associated with higher rate of nanoparticle albumin-bound paclitaxel-associated interstitial lung disease.
Methods: We reviewed clinical data for patients with advanced lung cancer who received nanoparticle albumin-bound paclitaxel with or without carboplatin or bevacizumab therapy at the Nippon Medical School Main Hospital between April 2013 and September 2017. Interstitial lung disease was diagnosed based on clinical symptoms, radiographic findings and exclusion of other diseases.
Results: A total of 110 advanced lung cancer patients received nanoparticle albumin-bound paclitaxel, and nine of them (8.2%) developed interstitial lung disease. Of those who developed interstitial lung disease, eight were treated with corticosteroids and three received cyclophosphamide pulse therapy. High-resolution computed tomography images demonstrated diffuse alveolar damage pattern pneumonitis in seven patients and organized pneumonia pattern pneumonitis in two patients. Six of the patients with diffuse alveolar damage pattern pneumonitis died from respiratory failure. The two patients with organized pneumonia pattern pneumonitis recovered. The incidence of interstitial lung disease was 19.0% (8/42) among patients with preexisting interstitial pneumonia and 1.5% (1/68) among those without preexisting interstitial pneumonia. Six patients with preexisting interstitial pneumonia met the criteria for acute exacerbation of interstitial pneumonia (14.3%).
Conclusion: Nanoparticle albumin-bound paclitaxel-associated interstitial lung disease was a severe and potentially fatal adverse event. We found it demonstrated diffuse alveolar damage or organized pneumonia pattern pneumonitis, and preexisting interstitial pneumonia was associated with higher rate of nanoparticle albumin-bound paclitaxel-associated interstitial lung disease.
Sato S, Kunisaki C, Tanaka Y, et al.
A Phase II Study of Tri-weekly Low-dose Nab-paclitaxel Chemotherapy for Patients with Advanced Gastric Cancer.
Anticancer Res. 2018; 38(12):6911-6917 [PubMed] Related Publications
A Phase II Study of Tri-weekly Low-dose Nab-paclitaxel Chemotherapy for Patients with Advanced Gastric Cancer.
Anticancer Res. 2018; 38(12):6911-6917 [PubMed] Related Publications
BACKGROUND/AIM: Nanoparticle albumin-bound (nab)-paclitaxel has demonstrated antitumor activity against advanced gastric cancer. However, gastric cancer patients can be difficult to treat with the recommended dose because of the high incidence of adverse toxicities. The aim of this study was to evaluate the safety and effectiveness of low-dose nab-paclitaxel in a multicenter, single-arm, phase II study.
PATIENTS AND METHODS: Treatment included low doses of 180 mg/m
RESULTS: The ORR was 5.9%. The median PFS and OS were 2.4 months and 9.2 months, respectively. The most common grade 3/4 toxicities were anemia (8.8%), neutropenia (5.9%), appetite loss (5.9%) and peripheral sensory neuropathy (5.9%). No treatment-related deaths occurred.
CONCLUSION: The tri-weekly low dose of nab-paclitaxel therapy is effective towards advanced gastric cancer patients with good tolerability and an acceptable margin of safety.
PATIENTS AND METHODS: Treatment included low doses of 180 mg/m
RESULTS: The ORR was 5.9%. The median PFS and OS were 2.4 months and 9.2 months, respectively. The most common grade 3/4 toxicities were anemia (8.8%), neutropenia (5.9%), appetite loss (5.9%) and peripheral sensory neuropathy (5.9%). No treatment-related deaths occurred.
CONCLUSION: The tri-weekly low dose of nab-paclitaxel therapy is effective towards advanced gastric cancer patients with good tolerability and an acceptable margin of safety.
Fernández A, Salgado M, García A, et al.
Prognostic factors for survival with nab-paclitaxel plus gemcitabine in metastatic pancreatic cancer in real-life practice: the ANICE-PaC study.
BMC Cancer. 2018; 18(1):1185 [PubMed] Free Access to Full Article Related Publications
Prognostic factors for survival with nab-paclitaxel plus gemcitabine in metastatic pancreatic cancer in real-life practice: the ANICE-PaC study.
BMC Cancer. 2018; 18(1):1185 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Treatment with nab-paclitaxel plus gemcitabine increases survival in patients with metastatic pancreatic cancer. However, the assessment of treatment efficacy and safety in non-selected patients in a real-life setting may provide useful information to support decision-making processes in routine practice.
METHODS: Retrospective, multicenter study including patients with metastatic pancreatic cancer, who started first-line treatment with nab-paclitaxel plus gemcitabine between December 2013 and June 2015 according to routine clinical practice. In addition to describing the treatment pattern, overall survival (OS) and progression-free survival (PFS) were assessed for the total sample and the exploratory subgroups based on the treatment and patients' clinical characteristics.
RESULTS: All 210 eligible patients had a median age of 65.0 years (range 37-81). Metastatic pancreatic adenocarcinoma was recurrent in 46 (21.9%) patients and de novo in 164 (78.1%); 38 (18%) patients had a biliary stent. At baseline, 33 (18.1%) patients had an ECOG performance status ≥2. Patients received a median of four cycles of treatment (range 1-21), with a median duration of 3.5 months; 137 (65.2%) patients had a dose reduction of nab-paclitaxel and/or gemcitabine during treatment, and 33 (17.2%) discontinued treatment due to toxicity. Relative dose intensity (RDI) for nab-paclitaxel, gemcitabine, and the combined treatment was 66.7%. Median OS was 7.2 months (95% CI 6.0-8.5), and median PFS was 5.0 months (95% CI 4.3-5.9); 50 patients achieved either a partial or complete response (ORR 24.6%). OS was influenced by baseline ECOG PS, NLR and CA 19.9, but not by age ≥ 70 years and/or the presence of hepatobiliary stent or RDI < 85%. All included variables, computed as dichotomous, showed a significant contribution to the Cox regression model to build a nomogram for predicting survival in these patients: baseline ECOG 0-1 vs. 2-3 (p = 0.030), baseline NLR > 3 vs. ≤ 3 (p = 0.043), and baseline CA 19.9 > 37 U/mL vs. ≤37 U/mL (p = 0.004).
CONCLUSIONS: Nab-Paclitaxel plus gemcitabine remain effective in a real-life setting, despite the high burden of dose reductions and poorer performance of these patients. A nomogram to predict survival using baseline ECOG performance status, NLR and CA 19.9 is proposed.
METHODS: Retrospective, multicenter study including patients with metastatic pancreatic cancer, who started first-line treatment with nab-paclitaxel plus gemcitabine between December 2013 and June 2015 according to routine clinical practice. In addition to describing the treatment pattern, overall survival (OS) and progression-free survival (PFS) were assessed for the total sample and the exploratory subgroups based on the treatment and patients' clinical characteristics.
RESULTS: All 210 eligible patients had a median age of 65.0 years (range 37-81). Metastatic pancreatic adenocarcinoma was recurrent in 46 (21.9%) patients and de novo in 164 (78.1%); 38 (18%) patients had a biliary stent. At baseline, 33 (18.1%) patients had an ECOG performance status ≥2. Patients received a median of four cycles of treatment (range 1-21), with a median duration of 3.5 months; 137 (65.2%) patients had a dose reduction of nab-paclitaxel and/or gemcitabine during treatment, and 33 (17.2%) discontinued treatment due to toxicity. Relative dose intensity (RDI) for nab-paclitaxel, gemcitabine, and the combined treatment was 66.7%. Median OS was 7.2 months (95% CI 6.0-8.5), and median PFS was 5.0 months (95% CI 4.3-5.9); 50 patients achieved either a partial or complete response (ORR 24.6%). OS was influenced by baseline ECOG PS, NLR and CA 19.9, but not by age ≥ 70 years and/or the presence of hepatobiliary stent or RDI < 85%. All included variables, computed as dichotomous, showed a significant contribution to the Cox regression model to build a nomogram for predicting survival in these patients: baseline ECOG 0-1 vs. 2-3 (p = 0.030), baseline NLR > 3 vs. ≤ 3 (p = 0.043), and baseline CA 19.9 > 37 U/mL vs. ≤37 U/mL (p = 0.004).
CONCLUSIONS: Nab-Paclitaxel plus gemcitabine remain effective in a real-life setting, despite the high burden of dose reductions and poorer performance of these patients. A nomogram to predict survival using baseline ECOG performance status, NLR and CA 19.9 is proposed.
Adrianzen Herrera D, Ashai N, Perez-Soler R, Cheng H
Nanoparticle albumin bound-paclitaxel for treatment of advanced non-small cell lung cancer: an evaluation of the clinical evidence.
Expert Opin Pharmacother. 2019; 20(1):95-102 [PubMed] Related Publications
Nanoparticle albumin bound-paclitaxel for treatment of advanced non-small cell lung cancer: an evaluation of the clinical evidence.
Expert Opin Pharmacother. 2019; 20(1):95-102 [PubMed] Related Publications
INTRODUCTION: Nanoparticle albumin-bound paclitaxel (nab-paclitaxel), a microtubule inhibitor, has demonstrated clinical efficacy in the treatment of advanced non-small cell lung cancer (NSCLC) either as monotherapy or in combination. Nab-paclitaxel was developed to reduce the toxicities associated with solvent-bound paclitaxel (sb-paclitaxel). Areas covered: This review first focuses on the clinical trials evaluating the efficacy and tolerability of nab-paclitaxel in NSCLC at different settings. The approval of nab-paclitaxel in combination with carboplatin at the front-line setting for advanced NSCLC was based on the key phase III study, which showed that nab-paclitaxel/carboplatin was associated with superior overall response rate and favorable toxicity profile compared to sb-paclitaxel/carboplatin. The review also addresses the nab-paclitaxel pharmacology, other combinations (e.g. immunotherapy with PD-1/PD-L1 inhibitors), potential biomarkers (e.g. caveolin-1), and special subgroups (e.g. the elderly, squamous histology). Expert opinion: Existing data has established the role of nab-paclitaxel in the management of advanced NSCLC. Emerging evidence, such as preliminary results from Keynote-407 and IMpower 131 studies, indicates that novel combinations of nab-paclitaxel/carboplatin and PD-1/PD-L1 inhibitors could further improve clinical benefits with manageable toxicity. Nevertheless, in order to better position nab-paclitaxel and to improve patient selection, future studies are warranted to further understand its mechanism of action, predictive biomarkers, and potential synergism with other agents.
Ostwal V, Sahu A, Zanwar S, et al.
Experience with non-cremophor-based paclitaxel-gemcitabine regimen in advanced pancreatic cancer: Results from a single tertiary cancer centre.
Indian J Med Res. 2018; 148(3):284-290 [PubMed] Free Access to Full Article Related Publications
Experience with non-cremophor-based paclitaxel-gemcitabine regimen in advanced pancreatic cancer: Results from a single tertiary cancer centre.
Indian J Med Res. 2018; 148(3):284-290 [PubMed] Free Access to Full Article Related Publications
Background & objectives: Gemcitabine combined with non-cremophor-based paclitaxel is one of the standards of care in advanced inoperable pancreatic cancer. This study was undertaken to retrospectively evaluate real world non-trial outcomes with this combination.
Methods: Patients with histologically proven advanced inoperable pancreatic adenocarcinoma (PDAC), treated with non-cremophor-based paclitaxel-gemcitabine combination (PG) (gemcitabine-nanoxel or gemcitabine-abraxane) between January 2012 and June 2015, were retrospectively analyzed. Response assessment was done every 8-12 wk with computed tomography scan and responses were measured as per the Response Evaluation Criteria in Solid Tumours 1.1 criteria where feasible. Toxicity was recorded as per the Common Terminology Criteria for Adverse Events (CTCAE) v4 criteria. Progression-free survival (PFS) and overall survival (OS) were calculated using the Kaplan-Meier method.
Results: A total of 78 patients with PDAC were treated with the combination. Of these, 83.3 per cent of patients had metastatic disease. The median number of chemotherapy cycles administered was three. The objective response rate for the whole group was 30.8 per cent. Grade III/IV toxicities were seen in 35.9 per cent of patients. Median PFS was 5.6 months and median OS was 11.6 months.
Interpretation & conclusions: Non-cremophor-based paclitaxel in combination with gemcitabine appeared efficacious for advanced pancreatic cancers in routine clinical practice. Within the confines of a single-centre retrospective analysis, gemcitabine-nanoxel and gemcitabine-abraxane appeared to have similar efficacy and toxicity in advanced pancreatic cancers.
Methods: Patients with histologically proven advanced inoperable pancreatic adenocarcinoma (PDAC), treated with non-cremophor-based paclitaxel-gemcitabine combination (PG) (gemcitabine-nanoxel or gemcitabine-abraxane) between January 2012 and June 2015, were retrospectively analyzed. Response assessment was done every 8-12 wk with computed tomography scan and responses were measured as per the Response Evaluation Criteria in Solid Tumours 1.1 criteria where feasible. Toxicity was recorded as per the Common Terminology Criteria for Adverse Events (CTCAE) v4 criteria. Progression-free survival (PFS) and overall survival (OS) were calculated using the Kaplan-Meier method.
Results: A total of 78 patients with PDAC were treated with the combination. Of these, 83.3 per cent of patients had metastatic disease. The median number of chemotherapy cycles administered was three. The objective response rate for the whole group was 30.8 per cent. Grade III/IV toxicities were seen in 35.9 per cent of patients. Median PFS was 5.6 months and median OS was 11.6 months.
Interpretation & conclusions: Non-cremophor-based paclitaxel in combination with gemcitabine appeared efficacious for advanced pancreatic cancers in routine clinical practice. Within the confines of a single-centre retrospective analysis, gemcitabine-nanoxel and gemcitabine-abraxane appeared to have similar efficacy and toxicity in advanced pancreatic cancers.
You MS, Ryu JK, Choi YH, et al.
Efficacy of Nab-Paclitaxel Plus Gemcitabine and Prognostic Value of Peripheral Neuropathy in Patients with Metastatic Pancreatic Cancer.
Gut Liver. 2018; 12(6):728-735 [PubMed] Free Access to Full Article Related Publications
Efficacy of Nab-Paclitaxel Plus Gemcitabine and Prognostic Value of Peripheral Neuropathy in Patients with Metastatic Pancreatic Cancer.
Gut Liver. 2018; 12(6):728-735 [PubMed] Free Access to Full Article Related Publications
Background/Aims: The combination of nab-paclitaxel and gemcitabine (nab-P/Gem) is widely used for treating metastatic pancreatic cancer (MPC). We aimed to evaluate the therapeutic outcomes and prognostic role of treatment-related peripheral neuropathy in patients with MPC treated with nab-P/Gem in clinical practice.
Methods: MPC patients treated with nab-P/Gem as the first-line chemotherapy were included. All 88 Korean patients underwent at least two cycles of nab-P/Gem combination chemotherapy (125 and 1,000 mg/m
Results: Patients underwent a mean of 6.7±4.2 cycles during 6.3±4.4 months. The median overall survival and progression-free survival rates were 14.2 months (95% confidence interval [CI], 11.8 to 20.3 months) and 8.4 months (95% CI, 7.1 to 13.2 months), respectively. The disease control rate was 84.1%; a partial response and stable disease were achieved in 30 (34.1%) and 44 (50.0%) patients, respectively. Treatment-related peripheral neuropathy developed in 52 patients (59.1%), and 13 (14.8%) and 16 (18.2%) patients experienced grades 2 and 3 neuropathy, respectively. In the landmark model, at 6 months, treatment-related peripheral neuropathy did not have a significant correlation with survival (p=0.089).
Conclusions: Nab-P/Gem is a reasonable choice for treating MPC, as it shows a considerable disease control rate while the treatment-related peripheral neuropathy was tolerable. The prognostic role of treatment-related neuropathy was limited.
Methods: MPC patients treated with nab-P/Gem as the first-line chemotherapy were included. All 88 Korean patients underwent at least two cycles of nab-P/Gem combination chemotherapy (125 and 1,000 mg/m
Results: Patients underwent a mean of 6.7±4.2 cycles during 6.3±4.4 months. The median overall survival and progression-free survival rates were 14.2 months (95% confidence interval [CI], 11.8 to 20.3 months) and 8.4 months (95% CI, 7.1 to 13.2 months), respectively. The disease control rate was 84.1%; a partial response and stable disease were achieved in 30 (34.1%) and 44 (50.0%) patients, respectively. Treatment-related peripheral neuropathy developed in 52 patients (59.1%), and 13 (14.8%) and 16 (18.2%) patients experienced grades 2 and 3 neuropathy, respectively. In the landmark model, at 6 months, treatment-related peripheral neuropathy did not have a significant correlation with survival (p=0.089).
Conclusions: Nab-P/Gem is a reasonable choice for treating MPC, as it shows a considerable disease control rate while the treatment-related peripheral neuropathy was tolerable. The prognostic role of treatment-related neuropathy was limited.
Kawaida H, Kono H, Amemiya H, et al.
Feasibility of Combination Therapy with Nab-paclitaxel Plus Gemcitabine in Patients with Recurrent Pancreatic Cancer.
Anticancer Res. 2018; 38(11):6537-6542 [PubMed] Related Publications
Feasibility of Combination Therapy with Nab-paclitaxel Plus Gemcitabine in Patients with Recurrent Pancreatic Cancer.
Anticancer Res. 2018; 38(11):6537-6542 [PubMed] Related Publications
BACKGROUND/AIM: Nab-paclitaxel plus gemcitabine (nab-P+Gem) is one of most reliable and effective regimens for borderline or unresectable pancreatic cancer (PC). However, the feasibility and clinical benefits of this regimen have never been evaluated for patients with recurrent PC after pancreatectomy. The aim of this study was to investigate the feasibility of combination therapy with nab-paclitaxel plus gemcitabine (nab-P+Gem) for patients with recurrent PC.
PATIENTS AND METHODS: Twenty-two patients with recurrent PC received an intravenous infusion of nab-P (125 mg/m
RESULTS: The treatment completion rate of the 4 cycles was 90.9%. The objective response rate was 13.6% and the disease control rate was 63.6%. The median progression-free survival was 7.2 months. The most common grade 3 or higher hematological toxicity was neutropenia (72.7%). There was no treatment-related death. Furthermore, the chemotherapeutic effects varied with the time of recurrence.
CONCLUSION: Combination nab-P+Gem therapy was well-tolerated and effective in patients with recurrent PC.
PATIENTS AND METHODS: Twenty-two patients with recurrent PC received an intravenous infusion of nab-P (125 mg/m
RESULTS: The treatment completion rate of the 4 cycles was 90.9%. The objective response rate was 13.6% and the disease control rate was 63.6%. The median progression-free survival was 7.2 months. The most common grade 3 or higher hematological toxicity was neutropenia (72.7%). There was no treatment-related death. Furthermore, the chemotherapeutic effects varied with the time of recurrence.
CONCLUSION: Combination nab-P+Gem therapy was well-tolerated and effective in patients with recurrent PC.
Rivera F, Benavides M, Gallego J, et al.
Tumor treating fields in combination with gemcitabine or gemcitabine plus nab-paclitaxel in pancreatic cancer: Results of the PANOVA phase 2 study.
Pancreatology. 2019; 19(1):64-72 [PubMed] Related Publications
Tumor treating fields in combination with gemcitabine or gemcitabine plus nab-paclitaxel in pancreatic cancer: Results of the PANOVA phase 2 study.
Pancreatology. 2019; 19(1):64-72 [PubMed] Related Publications
BACKGROUND: Tumor Treating Fields (TTFields), low intensity alternating electric fields with antimitotic activity, have demonstrated survival benefit in patients with glioblastoma. This phase 2 PANOVA study was conducted to examine the combination of TTFields plus chemotherapy in patients with pancreatic ductal adenocarcinoma (PDAC).
METHODS: Forty patients with newly-diagnosed, locally advanced or metastatic PDAC received continuous TTFields (150 KHz for ≥18 h/day) plus gemcitabine (1000 mg/m
RESULTS: Seventeen patients (85%) in each cohort reported Grade ≥3 adverse events (AEs). No increase in serious AEs (SAEs) was observed compared to that anticipated with systemic chemotherapy alone. Twenty-one patients reported TTFields-related skin toxicity, of which 7 were Grade 3; all resolved following temporary reduction of daily TTFields usage. No TTFields-related SAEs were reported. Compliance to TTFields was 68-78% of the recommended average daily use in both cohorts. Median PFS was 8.3 months (95% CI 4.3, 10.3) and median OS was 14.9 months (95% CI 6.2, NA) in the TTFields + gemcitabine cohort. In the TTFields + gemcitabine + nab-paclitaxel cohort, the median PFS was 12.7 months (95% CI 5.4, NA); median OS has not been reached.
CONCLUSION: The PANOVA trial demonstrated that the combination of TTFields and systemic chemotherapy is safe and tolerable in patients with advanced PDAC. Based on the safety and preliminary efficacy results of this phase 2 study, a randomized phase 3 study (PANOVA-3) is underway.
METHODS: Forty patients with newly-diagnosed, locally advanced or metastatic PDAC received continuous TTFields (150 KHz for ≥18 h/day) plus gemcitabine (1000 mg/m
RESULTS: Seventeen patients (85%) in each cohort reported Grade ≥3 adverse events (AEs). No increase in serious AEs (SAEs) was observed compared to that anticipated with systemic chemotherapy alone. Twenty-one patients reported TTFields-related skin toxicity, of which 7 were Grade 3; all resolved following temporary reduction of daily TTFields usage. No TTFields-related SAEs were reported. Compliance to TTFields was 68-78% of the recommended average daily use in both cohorts. Median PFS was 8.3 months (95% CI 4.3, 10.3) and median OS was 14.9 months (95% CI 6.2, NA) in the TTFields + gemcitabine cohort. In the TTFields + gemcitabine + nab-paclitaxel cohort, the median PFS was 12.7 months (95% CI 5.4, NA); median OS has not been reached.
CONCLUSION: The PANOVA trial demonstrated that the combination of TTFields and systemic chemotherapy is safe and tolerable in patients with advanced PDAC. Based on the safety and preliminary efficacy results of this phase 2 study, a randomized phase 3 study (PANOVA-3) is underway.
Noguchi Y, Kawashima Y, Maruyama M, et al.
Risk Factors for Eye Disorders Caused by Paclitaxel: A Retrospective Study.
Biol Pharm Bull. 2018; 41(11):1694-1700 [PubMed] Related Publications
Risk Factors for Eye Disorders Caused by Paclitaxel: A Retrospective Study.
Biol Pharm Bull. 2018; 41(11):1694-1700 [PubMed] Related Publications
Paclitaxel and nanoparticle albumin-bound paclitaxel are known to cause adverse events of eye disorders, such as cystoid macular edema. However, at present, the risk factors remain unclear. Therefore, risk factors for eye disorders caused by paclitaxel and nanoparticle albumin-bound paclitaxel were studied. This retrospective study targeted patients who were newly administered paclitaxel or nanoparticle albumin-bound paclitaxel at Kyoto Okamoto Memorial Hospital between April 1, 2012, and March 31, 2017. Eye disorder occurrence was defined as an event in which the pharmacist confirmed the symptoms in a patient interview and the ophthalmologist diagnosed the disorder. To analyze the risk factors, logistic regression analysis using 41 factors was performed. Of 128 subjects, 13 (10.2%) had eye disorders with symptom degrees of Grades 1 and 2. The symptoms were conjunctivitis or subconjunctival hemorrhage (3.1%), visual acuity reduction (2.3%), blurred vision and eye pain (1.6% each), eye mucus, blepharitis, stye, watering eyes, photopsia, and muscae volitantes (0.8% each). In eight patients, the conditions patients improved with spontaneously or with medication use; no improvements were observed the cases of visual acuity reduction, blurred vision, or muscae volitantes. Multivariate logistic regression analysis revealed that a cumulative dose of ≥819 mg/m
Zhao Y, Lv F, Chen S, et al.
Caveolin-1 expression predicts efficacy of weekly nab-paclitaxel plus gemcitabine for metastatic breast cancer in the phase II clinical trial.
BMC Cancer. 2018; 18(1):1019 [PubMed] Free Access to Full Article Related Publications
Caveolin-1 expression predicts efficacy of weekly nab-paclitaxel plus gemcitabine for metastatic breast cancer in the phase II clinical trial.
BMC Cancer. 2018; 18(1):1019 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Nanoparticle albumin-bound (nab)-paclitaxel has better efficacy, safety profiles, and no need to use prophylactic steroids compared with solvent-based paclitaxel. We performed a single arm, phase II study to evaluate the efficacy and safety of weekly nab-paclitaxel and gemcitabine combination in patients with metastatic breast cancer (MBC) and explored role of tumor/stromal Caveolin-1 (Cav-1) as a predictive biomarker for the efficacy.
METHODS: Nab-paclitaxel (125 mg/m
RESULTS: Among 85 patients enrolled in the study, ORR was 52.4%. After a median follow-up of 17.2 months, median PFS was 7.9 months (95%CI, 6.6-9.2) and median OS was 25.8 months (95% CI, 20.4-31.1). The most common toxicities were neutropenia (75.0% for all grades; 45.2% for grade 3 or worse) and the most common non-hematologic toxicity was peripheral neuropathy (50.0% for all grades, 7.14% for grade 3 or worse). Higher tumor Cav-1 level and lower stromal Cav-1 level were significantly associated with longer PFS of nab-paclitaxel and gemcitabine.
CONCLUSIONS: The regimen had substantial antitumor activity and was well tolerated in MBC patients. Tumor/stromal Cav-1 level may be a good predictor for the efficacy of nab-paclitaxel and gemcitabine.
TRIAL REGISTRATION: NCT01550848 . Registered 12 March 2012.
METHODS: Nab-paclitaxel (125 mg/m
RESULTS: Among 85 patients enrolled in the study, ORR was 52.4%. After a median follow-up of 17.2 months, median PFS was 7.9 months (95%CI, 6.6-9.2) and median OS was 25.8 months (95% CI, 20.4-31.1). The most common toxicities were neutropenia (75.0% for all grades; 45.2% for grade 3 or worse) and the most common non-hematologic toxicity was peripheral neuropathy (50.0% for all grades, 7.14% for grade 3 or worse). Higher tumor Cav-1 level and lower stromal Cav-1 level were significantly associated with longer PFS of nab-paclitaxel and gemcitabine.
CONCLUSIONS: The regimen had substantial antitumor activity and was well tolerated in MBC patients. Tumor/stromal Cav-1 level may be a good predictor for the efficacy of nab-paclitaxel and gemcitabine.
TRIAL REGISTRATION: NCT01550848 . Registered 12 March 2012.
Schmid P, Adams S, Rugo HS, et al.
Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer.
N Engl J Med. 2018; 379(22):2108-2121 [PubMed] Related Publications
Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer.
N Engl J Med. 2018; 379(22):2108-2121 [PubMed] Related Publications
BACKGROUND: Unresectable locally advanced or metastatic triple-negative (hormone-receptor-negative and human epidermal growth factor receptor 2 [HER2]-negative) breast cancer is an aggressive disease with poor outcomes. Nanoparticle albumin-bound (nab)-paclitaxel may enhance the anticancer activity of atezolizumab.
METHODS: In this phase 3 trial, we randomly assigned (in a 1:1 ratio) patients with untreated metastatic triple-negative breast cancer to receive atezolizumab plus nab-paclitaxel or placebo plus nab-paclitaxel; patients continued the intervention until disease progression or an unacceptable level of toxic effects occurred. Stratification factors were the receipt or nonreceipt of neoadjuvant or adjuvant taxane therapy, the presence or absence of liver metastases at baseline, and programmed death ligand 1 (PD-L1) expression at baseline (positive vs. negative). The two primary end points were progression-free survival (in the intention-to-treat population and PD-L1-positive subgroup) and overall survival (tested in the intention-to-treat population; if the finding was significant, then it would be tested in the PD-L1-positive subgroup).
RESULTS: Each group included 451 patients (median follow-up, 12.9 months). In the intention-to-treat analysis, the median progression-free survival was 7.2 months with atezolizumab plus nab-paclitaxel, as compared with 5.5 months with placebo plus nab-paclitaxel (hazard ratio for progression or death, 0.80; 95% confidence interval [CI], 0.69 to 0.92; P=0.002); among patients with PD-L1-positive tumors, the median progression-free survival was 7.5 months and 5.0 months, respectively (hazard ratio, 0.62; 95% CI, 0.49 to 0.78; P<0.001). In the intention-to-treat analysis, the median overall survival was 21.3 months with atezolizumab plus nab-paclitaxel and 17.6 months with placebo plus nab-paclitaxel (hazard ratio for death, 0.84; 95% CI, 0.69 to 1.02; P=0.08); among patients with PD-L1-positive tumors, the median overall survival was 25.0 months and 15.5 months, respectively (hazard ratio, 0.62; 95% CI, 0.45 to 0.86). No new adverse effects were identified. Adverse events that led to the discontinuation of any agent occurred in 15.9% of the patients who received atezolizumab plus nab-paclitaxel and in 8.2% of those who received placebo plus nab-paclitaxel.
CONCLUSIONS: Atezolizumab plus nab-paclitaxel prolonged progression-free survival among patients with metastatic triple-negative breast cancer in both the intention-to-treat population and the PD-L1-positive subgroup. Adverse events were consistent with the known safety profiles of each agent. (Funded by F. Hoffmann-La Roche/Genentech; IMpassion130 ClinicalTrials.gov number, NCT02425891 .).
METHODS: In this phase 3 trial, we randomly assigned (in a 1:1 ratio) patients with untreated metastatic triple-negative breast cancer to receive atezolizumab plus nab-paclitaxel or placebo plus nab-paclitaxel; patients continued the intervention until disease progression or an unacceptable level of toxic effects occurred. Stratification factors were the receipt or nonreceipt of neoadjuvant or adjuvant taxane therapy, the presence or absence of liver metastases at baseline, and programmed death ligand 1 (PD-L1) expression at baseline (positive vs. negative). The two primary end points were progression-free survival (in the intention-to-treat population and PD-L1-positive subgroup) and overall survival (tested in the intention-to-treat population; if the finding was significant, then it would be tested in the PD-L1-positive subgroup).
RESULTS: Each group included 451 patients (median follow-up, 12.9 months). In the intention-to-treat analysis, the median progression-free survival was 7.2 months with atezolizumab plus nab-paclitaxel, as compared with 5.5 months with placebo plus nab-paclitaxel (hazard ratio for progression or death, 0.80; 95% confidence interval [CI], 0.69 to 0.92; P=0.002); among patients with PD-L1-positive tumors, the median progression-free survival was 7.5 months and 5.0 months, respectively (hazard ratio, 0.62; 95% CI, 0.49 to 0.78; P<0.001). In the intention-to-treat analysis, the median overall survival was 21.3 months with atezolizumab plus nab-paclitaxel and 17.6 months with placebo plus nab-paclitaxel (hazard ratio for death, 0.84; 95% CI, 0.69 to 1.02; P=0.08); among patients with PD-L1-positive tumors, the median overall survival was 25.0 months and 15.5 months, respectively (hazard ratio, 0.62; 95% CI, 0.45 to 0.86). No new adverse effects were identified. Adverse events that led to the discontinuation of any agent occurred in 15.9% of the patients who received atezolizumab plus nab-paclitaxel and in 8.2% of those who received placebo plus nab-paclitaxel.
CONCLUSIONS: Atezolizumab plus nab-paclitaxel prolonged progression-free survival among patients with metastatic triple-negative breast cancer in both the intention-to-treat population and the PD-L1-positive subgroup. Adverse events were consistent with the known safety profiles of each agent. (Funded by F. Hoffmann-La Roche/Genentech; IMpassion130 ClinicalTrials.gov number, NCT02425891 .).


 Abraxane
Abraxane