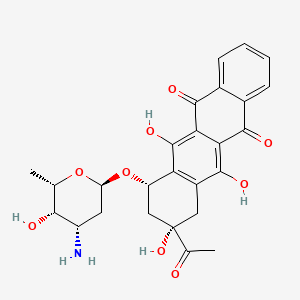
Idarubicin
"An orally administered anthracycline antineoplastic. The compound has shown activity against breast cancer, lymphomas and leukemias, together with the potential for reduced cardiac toxicity." (MeSH 2013)
Found this page useful?
 Web Resources: Idarubicin
Web Resources: Idarubicin Latest Research Publications
Latest Research PublicationsWeb Resources: Idarubicin (6 links)
Cancer Research UK
Macmillan Cancer Support
MedlinePlus
NHS Evidence
 Idarubicin - Substance Summary
Idarubicin - Substance Summary
PubChem
Irish Cancer Society
Latest Research Publications
This list of publications is regularly updated (Source: PubMed).
El-Kawy OA, Talaat HM
Preparation, characterization and evaluation of (186) Re-idarubicin: a novel agent for diagnosis and treatment of hepatocellular carcinoma.
J Labelled Comp Radiopharm. 2016; 59(2):72-7 [PubMed] Related Publications
Preparation, characterization and evaluation of (186) Re-idarubicin: a novel agent for diagnosis and treatment of hepatocellular carcinoma.
J Labelled Comp Radiopharm. 2016; 59(2):72-7 [PubMed] Related Publications
Hepatocellular carcinoma is a widely prevalent cancer, and hence, the development of radiopharmaceuticals for its management is an important issue. In the current investigation, the complexation of idarubicin with (186) Re was studied. Optimum labelling conditions were found to be 4 mg idarubicin, 1.5 mg stannous chloride dihydrate and ~70 MBq Re-186 at pH 7. The complex showed ~97.6% RCY value at 20 min and remained stable up to 24 h in the presence of 2.5 mg ascorbic acid. Molecular docking was performed to evaluate the complex binding to its target DNA-human topoisomerase II complex. Result of the in vivo evaluation showed that the complex tends to preferentially localize in cancerous tissues. The in vitro cell growth inhibition assay showed that the effect of the (186) Re-idarubicin was stronger than the effect of cold idarubicin, which strongly suggested that its cytotoxicity was mainly because of radiotoxicity rather than chemotherapeutic activity.
Lu T, Lokerse WJ, Seynhaeve AL, et al.
Formulation and optimization of idarubicin thermosensitive liposomes provides ultrafast triggered release at mild hyperthermia and improves tumor response.
J Control Release. 2015; 220(Pt A):425-37 [PubMed] Related Publications
Formulation and optimization of idarubicin thermosensitive liposomes provides ultrafast triggered release at mild hyperthermia and improves tumor response.
J Control Release. 2015; 220(Pt A):425-37 [PubMed] Related Publications
Drug delivery through thermosensitive liposomes (TSL) in combination with hyperthermia (HT) has shown great potential. HT can be applied locally forcing TSL to release their content in the heated tumor resulting in high peak concentrations. To perform optimally the drug is ideally released fast (seconds) and taken up rapidly by tumor cells. The aim of this study was to develop a novel thermosensitive liposome formulation of the anthracycline idarubicin (IDA-TSL). The hydrophobicity of idarubicin may improve its release from liposomes and subsequently rapid cellular uptake when combined mild hyperthermia. Here, we investigated a series of parameters to optimize IDA-TSL formulation. The results show that the optimal formulation for IDA-TSL is DPPC/DSPC/DSPE-PEG (6/3.5/0.5 mol%), with ammonium EDTA of 6.5 pH as loading buffer and a size of ~85 nm. In vitro studies demonstrated minimal leakage of ~20% in FCS at 37 °C for 1h, while an ultrafast and complete triggered release of IDA was observed at 42 °C. On tumor cells IDA-TSL showed comparable cytotoxicity to free IDA at 42 °C, but low cytotoxicity at 37 °C. Intravital microscopy imaging demonstrated an efficient in vivo intravascular triggered drug release of IDA-TSL under mild hyperthermia, and a subsequent massive IDA uptake by tumor cells. In animal efficacy studies, IDA-TSL plus mild HT demonstrated prominent tumor growth inhibition and superior survival rate over free IDA with HT or a clinically used Doxil treatment. These results suggest beneficial potential of IDA-TSL combined with local mild HT.
Shen Y, Chen J, Liu Y, Wu D
Addition of Cladribine to Idarubicin and Cytarabine during Induction Increases the Overall Efficacy Rate in Adult Patients with Acute Myeloid Leukemia: A Matched-Pair Retrospective Comparison.
Chemotherapy. 2014; 60(5-6):368-74 [PubMed] Related Publications
Addition of Cladribine to Idarubicin and Cytarabine during Induction Increases the Overall Efficacy Rate in Adult Patients with Acute Myeloid Leukemia: A Matched-Pair Retrospective Comparison.
Chemotherapy. 2014; 60(5-6):368-74 [PubMed] Related Publications
OBJECTIVES: The aims of this study were to evaluate a novel induction regimen composed of idarubicin (IDA), cytarabine (Ara-C) and cladribine (IAC regimen) for acute myeloid leukemia (AML) patients, and to identify the prognostic factors affecting treatment outcomes.
METHODS: The clinical data of 27 untreated AML patients who received the IAC regimen as primary induction therapy in our hospital between April and November 2014 were analyzed retrospectively. The treatment outcomes of the IAC regimen were compared with two IA (IDA + Ara-C) regimens (IDA 10 mg/m² and IDA 12 mg/m²) in a pair-matched analysis.
RESULTS: The complete remission (CR) rate in the IAC arm was higher compared to the IA(L) arm (p = 0.002) as was the overall efficacy rate (p = 0.017). There was no significant difference in outcomes between the IAC and IA(H) (Ara-C with high-dose IDA) arms. The IAC arm contained significantly higher CR rates than the IA(L) (Ara-C with low-dose IDA) arm in both the intermediate group (p = 0.050) and the unfavorable group (p = 0.013). Toxicity did not differ between the IAC group and the other two arms. High WBC at diagnosis (p = 0.022) and an unfavorable karyotype (p = 0.026) were related to a poorer response. The IAC regimen (p = 0.013) had greater superiority over the IAL regimen on efficacy than over the IA(H) regimen (p = 0.041).
CONCLUSIONS: The IAC regimen achieved a more significant advantage over the IA(L) regimen without increasing the risk of adverse events. The efficacy of induction therapy is associated with WBC at diagnosis, karyotype and induction regimen.
METHODS: The clinical data of 27 untreated AML patients who received the IAC regimen as primary induction therapy in our hospital between April and November 2014 were analyzed retrospectively. The treatment outcomes of the IAC regimen were compared with two IA (IDA + Ara-C) regimens (IDA 10 mg/m² and IDA 12 mg/m²) in a pair-matched analysis.
RESULTS: The complete remission (CR) rate in the IAC arm was higher compared to the IA(L) arm (p = 0.002) as was the overall efficacy rate (p = 0.017). There was no significant difference in outcomes between the IAC and IA(H) (Ara-C with high-dose IDA) arms. The IAC arm contained significantly higher CR rates than the IA(L) (Ara-C with low-dose IDA) arm in both the intermediate group (p = 0.050) and the unfavorable group (p = 0.013). Toxicity did not differ between the IAC group and the other two arms. High WBC at diagnosis (p = 0.022) and an unfavorable karyotype (p = 0.026) were related to a poorer response. The IAC regimen (p = 0.013) had greater superiority over the IAL regimen on efficacy than over the IA(H) regimen (p = 0.041).
CONCLUSIONS: The IAC regimen achieved a more significant advantage over the IA(L) regimen without increasing the risk of adverse events. The efficacy of induction therapy is associated with WBC at diagnosis, karyotype and induction regimen.
Burnett AK, Russell NH, Hills RK, et al.
Arsenic trioxide and all-trans retinoic acid treatment for acute promyelocytic leukaemia in all risk groups (AML17): results of a randomised, controlled, phase 3 trial.
Lancet Oncol. 2015; 16(13):1295-305 [PubMed] Related Publications
Arsenic trioxide and all-trans retinoic acid treatment for acute promyelocytic leukaemia in all risk groups (AML17): results of a randomised, controlled, phase 3 trial.
Lancet Oncol. 2015; 16(13):1295-305 [PubMed] Related Publications
BACKGROUND: Acute promyelocytic leukaemia is a chemotherapy-sensitive subgroup of acute myeloid leukaemia characterised by the presence of the PML-RARA fusion transcript. The present standard of care, chemotherapy and all-trans retinoic acid (ATRA), results in a high proportion of patients being cured. In this study, we compare a chemotherapy-free ATRA and arsenic trioxide treatment regimen with the standard chemotherapy-based regimen (ATRA and idarubicin) in both high-risk and low-risk patients with acute promyelocytic leukaemia.
METHODS: In the randomised, controlled, multicentre, AML17 trial, eligible patients (aged ≥16 years) with acute promyelocytic leukaemia, confirmed by the presence of the PML-RARA transcript and without significant cardiac or pulmonary comorbidities or active malignancy, and who were not pregnant or breastfeeding, were enrolled from 81 UK hospitals and randomised 1:1 to receive treatment with ATRA and arsenic trioxide or ATRA and idarubicin. ATRA was given to participants in both groups in a daily divided oral dose of 45 mg/m(2) until remission, or until day 60, and then in a 2 weeks on-2 weeks off schedule. In the ATRA and idarubicin group, idarubicin was given intravenously at 12 mg/m(2) on days 2, 4, 6, and 8 of course 1, and then at 5 mg/m(2) on days 1-4 of course 2; mitoxantrone at 10 mg/m(2) on days 1-4 of course 3, and idarubicin at 12 mg/m(2) on day 1 of the final (fourth) course. In the ATRA and arsenic trioxide group, arsenic trioxide was given intravenously at 0·3 mg/kg on days 1-5 of each course, and at 0·25 mg/kg twice weekly in weeks 2-8 of course 1 and weeks 2-4 of courses 2-5. High-risk patients (those presenting with a white blood cell count >10 × 10(9) cells per L) could receive an initial dose of the immunoconjugate gemtuzumab ozogamicin (6 mg/m(2) intravenously). Neither maintenance treatment nor CNS prophylaxis was given to patients in either group. All patients were monitored by real-time quantitative PCR. Allocation was by central computer minimisation, stratified by age, performance status, and de-novo versus secondary disease. The primary endpoint was quality of life on the European Organisation for Research and Treatment of Cancer (EORTC) QLQ-C30 global health status. All analyses are by intention to treat. This trial is registered with the ISRCTN registry, number ISRCTN55675535.
FINDINGS: Between May 8, 2009, and Oct 3, 2013, 235 patients were enrolled and randomly assigned to ATRA and idarubicin (n=119) or ATRA and arsenic trioxide (n=116). Participants had a median age of 47 years (range 16-77; IQR 33-58) and included 57 high-risk patients. Quality of life did not differ significantly between the treatment groups (EORTC QLQ-C30 global functioning effect size 2·17 [95% CI -2·79 to 7·12; p=0·39]). Overall, 57 patients in the ATRA and idarubicin group and 40 patients in the ATRA and arsenic trioxide group reported grade 3-4 toxicities. After course 1 of treatment, grade 3-4 alopecia was reported in 23 (23%) of 98 patients in the ATRA and idarubicin group versus 5 (5%) of 95 in the ATRA and arsenic trioxide group, raised liver alanine transaminase in 11 (10%) of 108 versus 27 (25%) of 109, oral toxicity in 22 (19%) of 115 versus one (1%) of 109. After course 2 of treatment, grade 3-4 alopecia was reported in 25 (28%) of 89 patients in the ATRA and idarubicin group versus 2 (3%) of 77 in the ATRA and arsenic trioxide group; no other toxicities reached the 10% level. Patients in the ATRA and arsenic trioxide group had significantly less requirement for most aspects of supportive care than did those in the ATRA and idarubicin group.
INTERPRETATION: ATRA and arsenic trioxide is a feasible treatment in low-risk and high-risk patients with acute promyelocytic leukaemia, with a high cure rate and less relapse than, and survival not different to, ATRA and idarubicin, with a low incidence of liver toxicity. However, no improvement in quality of life was seen.
METHODS: In the randomised, controlled, multicentre, AML17 trial, eligible patients (aged ≥16 years) with acute promyelocytic leukaemia, confirmed by the presence of the PML-RARA transcript and without significant cardiac or pulmonary comorbidities or active malignancy, and who were not pregnant or breastfeeding, were enrolled from 81 UK hospitals and randomised 1:1 to receive treatment with ATRA and arsenic trioxide or ATRA and idarubicin. ATRA was given to participants in both groups in a daily divided oral dose of 45 mg/m(2) until remission, or until day 60, and then in a 2 weeks on-2 weeks off schedule. In the ATRA and idarubicin group, idarubicin was given intravenously at 12 mg/m(2) on days 2, 4, 6, and 8 of course 1, and then at 5 mg/m(2) on days 1-4 of course 2; mitoxantrone at 10 mg/m(2) on days 1-4 of course 3, and idarubicin at 12 mg/m(2) on day 1 of the final (fourth) course. In the ATRA and arsenic trioxide group, arsenic trioxide was given intravenously at 0·3 mg/kg on days 1-5 of each course, and at 0·25 mg/kg twice weekly in weeks 2-8 of course 1 and weeks 2-4 of courses 2-5. High-risk patients (those presenting with a white blood cell count >10 × 10(9) cells per L) could receive an initial dose of the immunoconjugate gemtuzumab ozogamicin (6 mg/m(2) intravenously). Neither maintenance treatment nor CNS prophylaxis was given to patients in either group. All patients were monitored by real-time quantitative PCR. Allocation was by central computer minimisation, stratified by age, performance status, and de-novo versus secondary disease. The primary endpoint was quality of life on the European Organisation for Research and Treatment of Cancer (EORTC) QLQ-C30 global health status. All analyses are by intention to treat. This trial is registered with the ISRCTN registry, number ISRCTN55675535.
FINDINGS: Between May 8, 2009, and Oct 3, 2013, 235 patients were enrolled and randomly assigned to ATRA and idarubicin (n=119) or ATRA and arsenic trioxide (n=116). Participants had a median age of 47 years (range 16-77; IQR 33-58) and included 57 high-risk patients. Quality of life did not differ significantly between the treatment groups (EORTC QLQ-C30 global functioning effect size 2·17 [95% CI -2·79 to 7·12; p=0·39]). Overall, 57 patients in the ATRA and idarubicin group and 40 patients in the ATRA and arsenic trioxide group reported grade 3-4 toxicities. After course 1 of treatment, grade 3-4 alopecia was reported in 23 (23%) of 98 patients in the ATRA and idarubicin group versus 5 (5%) of 95 in the ATRA and arsenic trioxide group, raised liver alanine transaminase in 11 (10%) of 108 versus 27 (25%) of 109, oral toxicity in 22 (19%) of 115 versus one (1%) of 109. After course 2 of treatment, grade 3-4 alopecia was reported in 25 (28%) of 89 patients in the ATRA and idarubicin group versus 2 (3%) of 77 in the ATRA and arsenic trioxide group; no other toxicities reached the 10% level. Patients in the ATRA and arsenic trioxide group had significantly less requirement for most aspects of supportive care than did those in the ATRA and idarubicin group.
INTERPRETATION: ATRA and arsenic trioxide is a feasible treatment in low-risk and high-risk patients with acute promyelocytic leukaemia, with a high cure rate and less relapse than, and survival not different to, ATRA and idarubicin, with a low incidence of liver toxicity. However, no improvement in quality of life was seen.
Boulin M, Schmitt A, Delhom E, et al.
Improved stability of lipiodol-drug emulsion for transarterial chemoembolisation of hepatocellular carcinoma results in improved pharmacokinetic profile: Proof of concept using idarubicin.
Eur Radiol. 2016; 26(2):601-9 [PubMed] Related Publications
Improved stability of lipiodol-drug emulsion for transarterial chemoembolisation of hepatocellular carcinoma results in improved pharmacokinetic profile: Proof of concept using idarubicin.
Eur Radiol. 2016; 26(2):601-9 [PubMed] Related Publications
OBJECTIVES: To investigate the relationship between the improved stability of an anticancer drug-lipiodol emulsion and pharmacokinetic (PK) profile for transarterial chemoembolisation (TACE) of hepatocellular carcinoma (HCC).
METHODS: The stability of four doxorubicin- or idarubicin-lipiodol emulsions was evaluated over 7 days. PK and clinical data were recorded after TACE with the most stable emulsion in eight unresectable HCC patients, after institutional review board approval.
RESULTS: The most stable emulsion was the one that combined idarubicin and lipiodol (1:2 v:v). At 7 days, the percentages of aqueous, persisting emulsion and oily phases were 50-0-50, 33-0-67, 31-39-30, and 10-90-0 for the doxorubicin-lipiodol (1:1 v:v), doxorubicin-lipiodol (1:2 v:v), idarubicin-lipiodol (1:1 v:v), and the idarubicin-lipiodol (1:2 v:v) emulsion, respectively. After TACE, mean idarubicin Cmax and AUC0-24h were 12.5 ± 9.4 ng/mL and 52 ± 16 ng/mL*h. Within 24 h after injection, 40% of the idarubicin was in the liver, either in vessels, tumours, or hepatocytes. During the 2 months after TACE, no clinical grade >3 adverse events occurred. One complete response, five partial responses, one stabilisation, and one progression were observed at 2 months.
CONCLUSION: This study showed a promising and favourable PK and safety profile for the idarubicin-lipiodol (1:2 v:v) emulsion for TACE.
KEY POINTS: • Transarterial chemoembolisation (TACE) regimens that improve survival in hepatocellular carcinoma are needed. • Improved emulsion stability for TACE resulted in a favourable pharmacokinetic profile. • Preliminary safety and efficacy data for the idarubicin-lipiodol emulsion for TACE were encouraging.
METHODS: The stability of four doxorubicin- or idarubicin-lipiodol emulsions was evaluated over 7 days. PK and clinical data were recorded after TACE with the most stable emulsion in eight unresectable HCC patients, after institutional review board approval.
RESULTS: The most stable emulsion was the one that combined idarubicin and lipiodol (1:2 v:v). At 7 days, the percentages of aqueous, persisting emulsion and oily phases were 50-0-50, 33-0-67, 31-39-30, and 10-90-0 for the doxorubicin-lipiodol (1:1 v:v), doxorubicin-lipiodol (1:2 v:v), idarubicin-lipiodol (1:1 v:v), and the idarubicin-lipiodol (1:2 v:v) emulsion, respectively. After TACE, mean idarubicin Cmax and AUC0-24h were 12.5 ± 9.4 ng/mL and 52 ± 16 ng/mL*h. Within 24 h after injection, 40% of the idarubicin was in the liver, either in vessels, tumours, or hepatocytes. During the 2 months after TACE, no clinical grade >3 adverse events occurred. One complete response, five partial responses, one stabilisation, and one progression were observed at 2 months.
CONCLUSION: This study showed a promising and favourable PK and safety profile for the idarubicin-lipiodol (1:2 v:v) emulsion for TACE.
KEY POINTS: • Transarterial chemoembolisation (TACE) regimens that improve survival in hepatocellular carcinoma are needed. • Improved emulsion stability for TACE resulted in a favourable pharmacokinetic profile. • Preliminary safety and efficacy data for the idarubicin-lipiodol emulsion for TACE were encouraging.
Li X, Xu S, Tan Y, Chen J
The effects of idarubicin versus other anthracyclines for induction therapy of patients with newly diagnosed leukaemia.
Cochrane Database Syst Rev. 2015; (6):CD010432 [PubMed] Related Publications
The effects of idarubicin versus other anthracyclines for induction therapy of patients with newly diagnosed leukaemia.
Cochrane Database Syst Rev. 2015; (6):CD010432 [PubMed] Related Publications
BACKGROUND: Anthracycline combined with cytarabine has been the standard for induction therapy of newly diagnosed acute myeloid leukaemia (AML) for several decades. Due to theoretical advantages, idarubicin (IDA) might be the most effective and tolerable anthracycline. However, there is no evidence that would definitively prove the superiority of IDA over other anthracyclines.
OBJECTIVES: To assess the efficacy and safety of IDA versus other anthracyclines in induction therapy of newly diagnosed AML.
SEARCH METHODS: We identified relevant randomised controlled trials (RCTs) by searching the Cochrane Central Register of Controlled Trials (The Cochrane Library 2014, Issue 8), MEDLINE (from 1946 to 3 August 2014), EMBASE (from 1974 to 3 August 2014), Chinese BioMedical Literature Database (1978 to 3 August 2014), relevant conference proceedings and databases of ongoing trials.
SELECTION CRITERIA: RCTs that compared IDA with other anthracyclines in induction therapy of newly diagnosed AML.
DATA COLLECTION AND ANALYSIS: Two review authors independently extracted data and assessed the quality of studies according to methodological standards of the Cochrane Collaboration. We estimated hazard ratios (HRs) for time-to-event data outcomes using the inverse variance method, and risk ratios (RRs) for dichotomous data outcomes using the Mantel-Haenszel method. We adopted a fixed-effect model and repeated the main meta-analysis by a random-effects model in a sensitivity analysis.
MAIN RESULTS: We identified 2017 references. Ultimately, 27 RCTs (including 22 two-armed RCTs and five three-armed RCTs) involving 9549 patients were eligible. The consolidation treatments adopted in the studies were comparable and had no impact on the results. Overall, the risk of bias of the studies was unclear to high.Eighteen RCTs (N = 6755) assessed IDA versus daunorubicin (DNR). The main meta-analyses showed that IDA compared with DNR prolonged overall survival (OS) (12 studies, 5976 patients; HR 0.90, 95% confidence interval (CI) 0.84 to 0.96, P = 0.0008; high quality of evidence) and disease-free survival (DFS) (eight studies, 3070 patients; HR 0.88, 95% CI 0.81 to 0.96, P = 0.004; moderate quality of evidence), increased complete remission (CR) rate (18 studies, 6692 patients; RR 1.04, 95% CI 1.01 to 1.07, P = 0.009; moderate quality of evidence), and reduced relapse rate (four studies, 1091 patients; RR 0.88, 95% CI 0.80 to 0.98, P = 0.02; moderate quality of evidence), although increased the risks of death on induction therapy (14 studies, 6349 patients; RR 1.18, 95% CI 1.01 to 1.36, P = 0.03; moderate quality of evidence) and grade 3/4 mucositis (five studies, 2000 patients; RR 1.22, 95% CI 1.04 to 1.44, P = 0.02; moderate quality of evidence). There was no evidence for difference in the risks of grade 3/4 cardiac toxicity (six studies, 2795 patients; RR 0.98, 95% CI 0.70 to 1.37, P = 0.91; moderate quality of evidence) and other grade 3/4 adverse events (AEs). None of the studies reported on quality of life (QoL).Eight RCTs (N = 2419) evaluated IDA versus mitoxantrone (MIT). The main meta-analyses showed that there was no evidence for difference between arms in OS (six studies, 2171 patients; HR 0.98, 95% CI 0.89 to 1.08, P = 0.69; high quality of evidence), DFS (four studies, 249 patients; HR 0.88, 95% CI 0.70 to 1.10, P = 0.26; low quality of evidence), CR rate (eight studies, 2411 patients; RR 0.97, 95% CI 0.92 to 1.03, P = 0.32;moderate quality of evidence), the risks of death on induction therapy (five studies, 2055 patients; RR 1.10, 95% CI 0.88 to 1.38, P = 0.39; moderate quality of evidence) and relapse (three studies, 328 patients; RR 0.99, 95% CI 0.80 to 1.22, P = 0.89; moderate quality of evidence). There was no evidence for difference in the risks of grade 3/4 cardiac toxicity (one study, 160 patients; RR 0.67, 95% CI 0.11 to 3.88, P = 0.65; low quality of evidence) and other grade 3/4 AEs. None of the studies reported on QoL.Two RCTs (N = 211) compared IDA with doxorubicin (DOX). Neither study assessed OS. One study showed that there was no evidence for difference in DFS (63 patients; HR 0.62, 95% CI 0.34 to 1.14, P = 0.12; low quality of evidence). The main meta-analysis for CR rate showed an improved CR rate with IDA (two studies, 187 patients; RR 1.28, 95% CI 1.03 to 1.59, P = 0.02; low quality of evidence). Neither study provided data for the risks of death on induction therapy and relapse. One trial showed that there was no evidence for difference in the risk of grade 3/4 cardiac toxicity (one study, 100 patients; RR 0.31, 95% CI 0.01 to 7.39, P = 0.47; very low quality of evidence). Neither study reported on QoL.Two RCTs (N = 1037) evaluated IDA versus zorubicin (ZRB). Neither study assessed OS. One trial showed that there was no evidence for difference in DFS (one study, 155 patients; HR 1.25, 95% CI 0.83 to 1.88, P = 0.29; low quality of evidence). The main meta-analyses for CR and death on induction therapy both showed that there was no evidence for difference (CR rate: two studies, 964 patients; RR 1.04, 95% CI 0.96 to 1.13, P = 0.31; low quality of evidence. risk of death on induction therapy: two studies, 964 patients; RR 0.75, 95% CI 0.50 to 1.13, P = 0.17; moderate quality of evidence). Neither study reported the risks of relapse and grade 3/4 cardiotoxicity. One trial showed that IDA reduced the risk of grade 3/4 mucositis. Neither study reported on QoL.
AUTHORS' CONCLUSIONS: Compared with DNR in induction therapy of newly diagnosed AML, IDA prolongs OS and DFS, increases CR rate and reduces relapse rate, although increases the risks of death on induction therapy and grade 3/4 mucositis. The currently available evidence does not show any difference between IDA and MIT used in induction therapy of newly diagnosed AML. There is insufficient evidence regarding IDA versus DOX and IDA versus ZRB to make final conclusions. Additionally, there is no evidence for difference on the effect of IDA compared with DNR, MIT, DOX or ZRB on QoL.
OBJECTIVES: To assess the efficacy and safety of IDA versus other anthracyclines in induction therapy of newly diagnosed AML.
SEARCH METHODS: We identified relevant randomised controlled trials (RCTs) by searching the Cochrane Central Register of Controlled Trials (The Cochrane Library 2014, Issue 8), MEDLINE (from 1946 to 3 August 2014), EMBASE (from 1974 to 3 August 2014), Chinese BioMedical Literature Database (1978 to 3 August 2014), relevant conference proceedings and databases of ongoing trials.
SELECTION CRITERIA: RCTs that compared IDA with other anthracyclines in induction therapy of newly diagnosed AML.
DATA COLLECTION AND ANALYSIS: Two review authors independently extracted data and assessed the quality of studies according to methodological standards of the Cochrane Collaboration. We estimated hazard ratios (HRs) for time-to-event data outcomes using the inverse variance method, and risk ratios (RRs) for dichotomous data outcomes using the Mantel-Haenszel method. We adopted a fixed-effect model and repeated the main meta-analysis by a random-effects model in a sensitivity analysis.
MAIN RESULTS: We identified 2017 references. Ultimately, 27 RCTs (including 22 two-armed RCTs and five three-armed RCTs) involving 9549 patients were eligible. The consolidation treatments adopted in the studies were comparable and had no impact on the results. Overall, the risk of bias of the studies was unclear to high.Eighteen RCTs (N = 6755) assessed IDA versus daunorubicin (DNR). The main meta-analyses showed that IDA compared with DNR prolonged overall survival (OS) (12 studies, 5976 patients; HR 0.90, 95% confidence interval (CI) 0.84 to 0.96, P = 0.0008; high quality of evidence) and disease-free survival (DFS) (eight studies, 3070 patients; HR 0.88, 95% CI 0.81 to 0.96, P = 0.004; moderate quality of evidence), increased complete remission (CR) rate (18 studies, 6692 patients; RR 1.04, 95% CI 1.01 to 1.07, P = 0.009; moderate quality of evidence), and reduced relapse rate (four studies, 1091 patients; RR 0.88, 95% CI 0.80 to 0.98, P = 0.02; moderate quality of evidence), although increased the risks of death on induction therapy (14 studies, 6349 patients; RR 1.18, 95% CI 1.01 to 1.36, P = 0.03; moderate quality of evidence) and grade 3/4 mucositis (five studies, 2000 patients; RR 1.22, 95% CI 1.04 to 1.44, P = 0.02; moderate quality of evidence). There was no evidence for difference in the risks of grade 3/4 cardiac toxicity (six studies, 2795 patients; RR 0.98, 95% CI 0.70 to 1.37, P = 0.91; moderate quality of evidence) and other grade 3/4 adverse events (AEs). None of the studies reported on quality of life (QoL).Eight RCTs (N = 2419) evaluated IDA versus mitoxantrone (MIT). The main meta-analyses showed that there was no evidence for difference between arms in OS (six studies, 2171 patients; HR 0.98, 95% CI 0.89 to 1.08, P = 0.69; high quality of evidence), DFS (four studies, 249 patients; HR 0.88, 95% CI 0.70 to 1.10, P = 0.26; low quality of evidence), CR rate (eight studies, 2411 patients; RR 0.97, 95% CI 0.92 to 1.03, P = 0.32;moderate quality of evidence), the risks of death on induction therapy (five studies, 2055 patients; RR 1.10, 95% CI 0.88 to 1.38, P = 0.39; moderate quality of evidence) and relapse (three studies, 328 patients; RR 0.99, 95% CI 0.80 to 1.22, P = 0.89; moderate quality of evidence). There was no evidence for difference in the risks of grade 3/4 cardiac toxicity (one study, 160 patients; RR 0.67, 95% CI 0.11 to 3.88, P = 0.65; low quality of evidence) and other grade 3/4 AEs. None of the studies reported on QoL.Two RCTs (N = 211) compared IDA with doxorubicin (DOX). Neither study assessed OS. One study showed that there was no evidence for difference in DFS (63 patients; HR 0.62, 95% CI 0.34 to 1.14, P = 0.12; low quality of evidence). The main meta-analysis for CR rate showed an improved CR rate with IDA (two studies, 187 patients; RR 1.28, 95% CI 1.03 to 1.59, P = 0.02; low quality of evidence). Neither study provided data for the risks of death on induction therapy and relapse. One trial showed that there was no evidence for difference in the risk of grade 3/4 cardiac toxicity (one study, 100 patients; RR 0.31, 95% CI 0.01 to 7.39, P = 0.47; very low quality of evidence). Neither study reported on QoL.Two RCTs (N = 1037) evaluated IDA versus zorubicin (ZRB). Neither study assessed OS. One trial showed that there was no evidence for difference in DFS (one study, 155 patients; HR 1.25, 95% CI 0.83 to 1.88, P = 0.29; low quality of evidence). The main meta-analyses for CR and death on induction therapy both showed that there was no evidence for difference (CR rate: two studies, 964 patients; RR 1.04, 95% CI 0.96 to 1.13, P = 0.31; low quality of evidence. risk of death on induction therapy: two studies, 964 patients; RR 0.75, 95% CI 0.50 to 1.13, P = 0.17; moderate quality of evidence). Neither study reported the risks of relapse and grade 3/4 cardiotoxicity. One trial showed that IDA reduced the risk of grade 3/4 mucositis. Neither study reported on QoL.
AUTHORS' CONCLUSIONS: Compared with DNR in induction therapy of newly diagnosed AML, IDA prolongs OS and DFS, increases CR rate and reduces relapse rate, although increases the risks of death on induction therapy and grade 3/4 mucositis. The currently available evidence does not show any difference between IDA and MIT used in induction therapy of newly diagnosed AML. There is insufficient evidence regarding IDA versus DOX and IDA versus ZRB to make final conclusions. Additionally, there is no evidence for difference on the effect of IDA compared with DNR, MIT, DOX or ZRB on QoL.
Kim H, Lee JH, Joo YD, et al.
A prospective, multicenter phase II study of continuous infusion of FLAG for patients older than 60 yr with resistant acute myeloid leukemia: a comparison with intensive younger patients' trial.
Eur J Haematol. 2016; 96(2):188-97 [PubMed] Related Publications
A prospective, multicenter phase II study of continuous infusion of FLAG for patients older than 60 yr with resistant acute myeloid leukemia: a comparison with intensive younger patients' trial.
Eur J Haematol. 2016; 96(2):188-97 [PubMed] Related Publications
Relapsed or refractory acute myeloid leukemia (R/R AML) in elderly (≥60 yr old) patients were eligible. Induction chemotherapy consisted fludarabine and cytarabine (ARAC) as a 24-hr CI without idarubicin (C-FLAG), which was compared with the results of C-FLAG with idarubicin (CI-FLAG2) in younger patients' trial. A total of 33 and 68 patients were enrolled in C-FLAG and CI-FLAG2, respectively. CR, CRp, and CRi were achieved in 10 (30.3%), 3 (9.1%), and 2 (6.1%), respectively. When comparing outcomes between C-FLAG and CI-FLAG2, there were no difference in terms of CR rate (P = 0.572) and objective response rate (ORR; P = 0.899). Favorable predictors on ORR in C-FLAG were PB WBC ≤ 20K/uL at salvage (P = 0.024) and early evaluation peripheral BLAST = 0% (P = 0.013) on multivariate analysis. The overall survival of patients who achieve CR/CRp/CRi showed significantly prolonged survival compared with patients who did not in C-FLAG (P < 0.001) and was a favorable predictor of longer survival by multivariate analysis (P = 0.009). Median overall survival was 3.19 (95% CI, 2.05-4.33) months and similar with that of CI-FLAG2 (P = 0.841). Attenuated salvage regimen C-FLGA in elderly patients was as effective as more intensive younger patients' regimen CI-FLAG2 in terms of response and survival although elderly patients had more unfavorable clinical characteristics.
Nafee N, Hirosue M, Loretz B, et al.
Cyclodextrin-based star polymers as a versatile platform for nanochemotherapeutics: Enhanced entrapment and uptake of idarubicin.
Colloids Surf B Biointerfaces. 2015; 129:30-8 [PubMed] Related Publications
Cyclodextrin-based star polymers as a versatile platform for nanochemotherapeutics: Enhanced entrapment and uptake of idarubicin.
Colloids Surf B Biointerfaces. 2015; 129:30-8 [PubMed] Related Publications
A series of cyclodextrin-based star polymers were synthesized using β-cyclodextrin (CD) as hydrophilic core, methyl methacrylate (MMA) and tert-butyl acrylate (tBA) as hydrophobic arms. Star polymers, either homopolymers or random/block copolymers, showed narrow molecular weight distributions. Grafting hydrophobic arms created CD-based nanoparticles (CD-NPs) in the size range (130-200nm) with narrow PdI <0.15 and slightly negative ζ-potential. Particle surface could be modified with chitosan to impart a positive surface charge. Colloidal stability of CD-NPs was a function of pH as revealed by the pH-titration curves. CD-NPs were used as carrier for the chemotherapeutic drug idarubicin (encapsulation efficiency, EE ∼40%) ensuring prolonged release profile (∼80% after 48h). For cell-based studies, coumarin-6 was encapsulated as a fluorescent marker (EE ∼75%). Uptake studies carried out on A549 and Caco-2 cell lines proved the uptake of coumarin-loaded NPs as a function of time and preferential localization in the cytoplasm. Uptake kinetics revealed no saturation or plateau over 6h. Chitosan-modified NPs showed significantly improved, concentration-dependent cellular uptake. Meanwhile, CD-NPs were non-cytotoxic on both cell lines over the concentration range (0.25-3mg/ml) as studied by MTT and LDH assays. In conclusion, CD star polymers can be considered a versatile platform for a new class of biocompatible nanochemotherapy.
Röllig C, Schäfer-Eckardt K, Hänel M, et al.
Two cycles of risk-adapted consolidation therapy in patients with acute promyelocytic leukemia. Results from the SAL-AIDA2000 trial.
Ann Hematol. 2015; 94(4):557-63 [PubMed] Related Publications
Two cycles of risk-adapted consolidation therapy in patients with acute promyelocytic leukemia. Results from the SAL-AIDA2000 trial.
Ann Hematol. 2015; 94(4):557-63 [PubMed] Related Publications
The combination of all-trans retinoic acid (ATRA) and idarubicin (AIDA) for induction therapy followed by three cycles of risk-adapted consolidation cycles is considered standard of care for patients with acute promyelocytic leukemia (APL). We report the outcome of 141 patients (median age 51 years; range, 19-82, 31 % ≥60 years) enrolled into the prospective Study Alliance Leukemia (SAL)-AIDA2000 trial, which comprised AIDA-based induction followed by only two courses of risk-adapted consolidation (daunorubicin or mitoxantrone ± cytarabine) followed by 2-year maintenance treatment. The early death rate was 7 % (median age 66 years), and additional 9 % stopped further treatment after induction. The estimated 6-year disease-free survival (DFS) was 80 % in all patients, 84 % in patients ≤60 and 72 % in patients >60 years (p = 0.140). No significant survival differences were observed between the high-risk and the non-high-risk patients (6-year OS 78 vs. 81 %, p = 0.625). Our results confirm the efficacy of a risk-adapted approach in APL patients. Furthermore, long-term outcomes are comparable to the results obtained with three cycles of consolidation. A modification of the number and intensity of conventional consolidation treatment may be a less toxic but equally effective approach and should be considered for further evaluation in randomized clinical trials in APL.
Sekine L, Morais VD, Lima KM, et al.
Conventional and high-dose daunorubicin and idarubicin in acute myeloid leukaemia remission induction treatment: a mixed treatment comparison meta-analysis of 7258 patients.
Hematol Oncol. 2015; 33(4):212-9 [PubMed] Related Publications
Conventional and high-dose daunorubicin and idarubicin in acute myeloid leukaemia remission induction treatment: a mixed treatment comparison meta-analysis of 7258 patients.
Hematol Oncol. 2015; 33(4):212-9 [PubMed] Related Publications
Previous meta-analyses suggested that acute myeloid leukaemia induction regimens containing idarubicin (IDA) or high-dose daunorubicin (HDD) induce higher rates of complete remission (CR) than conventional-dose daunorubicin (CDD), with a possible benefit in overall survival. However, robust comparisons between these regimens are still lacking. We conducted a mixed treatment comparison meta-analysis regarding these three regimens. Mixed treatment comparison is a statistical method of data summarization that aggregates data from both direct and indirect effect estimates. Literature search strategy included MEDLINE, EMBASE, Cochrane, Scielo and LILACS, from inception until August 2013 and resulted in the inclusion of 17 trials enrolling 7258 adult patients. HDD [relative risk (RR) 1.13; 95% credible interval (CrI) 1.02-1.26] and IDA (RR 1.13; 95% CrI 1.05-1.23) showed higher CR rates than CDD. IDA also led to lower long-term overall mortality rates when compared with CDD (RR 0.93, 95% CrI 0.86-0.99), whereas HDD and CDD were no different (RR 0.94, 95% CrI 0.85-1.02). HDD and IDA comparison did not reach statistically significant differences in CR (RR 1.00; 95% CrI 0.89-1.11) and in long-term mortality (RR 1.01, 95% CrI 0.91-1.11). IDA and HDD are consistently superior to CDD in inducing CR, and IDA was associated with lower long-term mortality. On the basis of these findings, we recommend incorporation of IDA and HDD instead of the traditional CDD as standard treatments for acute myeloid leukaemia induction. The lack of HDD benefit on mortality, when compared with CDD in this study, should be cautiously addressed, because it may have been susceptible to underestimation because of statistical power limitations.
Guiu B, Schmitt A, Reinhardt S, et al.
Idarubicin-loaded ONCOZENE drug-eluting embolic agents for chemoembolization of hepatocellular carcinoma: in vitro loading and release and in vivo pharmacokinetics.
J Vasc Interv Radiol. 2015; 26(2):262-70 [PubMed] Related Publications
Idarubicin-loaded ONCOZENE drug-eluting embolic agents for chemoembolization of hepatocellular carcinoma: in vitro loading and release and in vivo pharmacokinetics.
J Vasc Interv Radiol. 2015; 26(2):262-70 [PubMed] Related Publications
PURPOSE: To present in vitro loading and release characteristics of idarubicin with ONCOZENE (CeloNova BioSciences, Inc, San Antonio, Texas) drug-eluting embolic (DEE) agents and in vivo pharmacokinetics data after transarterial chemoembolization with idarubicin-loaded ONCOZENE DEE agents in patients with hepatocellular carcinoma.
MATERIALS AND METHODS: Loading efficacy of idarubicin with ONCOZENE DEE agents 100 µm and DC Bead (Biocompatibles UK Ltd, Farnham, United Kingdom) DEE agents 100-300 µm was monitored at 10, 20, and 30 minutes loading time by high-pressure liquid chromatography. A T-apparatus was used to monitor the release of idarubicin from the two types of DEE agents over 12 hours. Clinical and 24-hour pharmacokinetics data were recorded after transarterial chemoembolization with idarubicin-loaded ONCOZENE DEE agents in four patients with unresectable hepatocellular carcinoma.
RESULTS: Idarubicin loading in ONCOZENE DEE agents was > 99% at 10 minutes. Time to reach 75% of the release plateau level was 37 minutes ± 6 for DC Bead DEE agents and 170 minutes ± 19 for ONCOZENE DEE agents both loaded with idarubicin 10 mg/mL. After transarterial chemoembolization with idarubicin-loaded ONCOZENE DEE agents, three partial responses and one complete response were observed with only two asymptomatic grade 3 biologic adverse events. Median time to maximum concentration for idarubicin in patients was 10 minutes, and mean maximum concentration was 4.9 µg/L ± 1.7. Mean area under the concentration-time curve from 0-24 hours was equal to 29.5 µg.h/L ± 20.5.
CONCLUSIONS: ONCOZENE DEE agents show promising results with very fast loading ability, a favorable in vivo pharmacokinetics profile with a sustained release of idarubicin during the first 24 hours, and encouraging safety and responses. Histopathologic and clinical studies are needed to evaluate idarubicin release around the DEE agents in tumor tissue and to confirm safety and efficacy.
MATERIALS AND METHODS: Loading efficacy of idarubicin with ONCOZENE DEE agents 100 µm and DC Bead (Biocompatibles UK Ltd, Farnham, United Kingdom) DEE agents 100-300 µm was monitored at 10, 20, and 30 minutes loading time by high-pressure liquid chromatography. A T-apparatus was used to monitor the release of idarubicin from the two types of DEE agents over 12 hours. Clinical and 24-hour pharmacokinetics data were recorded after transarterial chemoembolization with idarubicin-loaded ONCOZENE DEE agents in four patients with unresectable hepatocellular carcinoma.
RESULTS: Idarubicin loading in ONCOZENE DEE agents was > 99% at 10 minutes. Time to reach 75% of the release plateau level was 37 minutes ± 6 for DC Bead DEE agents and 170 minutes ± 19 for ONCOZENE DEE agents both loaded with idarubicin 10 mg/mL. After transarterial chemoembolization with idarubicin-loaded ONCOZENE DEE agents, three partial responses and one complete response were observed with only two asymptomatic grade 3 biologic adverse events. Median time to maximum concentration for idarubicin in patients was 10 minutes, and mean maximum concentration was 4.9 µg/L ± 1.7. Mean area under the concentration-time curve from 0-24 hours was equal to 29.5 µg.h/L ± 20.5.
CONCLUSIONS: ONCOZENE DEE agents show promising results with very fast loading ability, a favorable in vivo pharmacokinetics profile with a sustained release of idarubicin during the first 24 hours, and encouraging safety and responses. Histopathologic and clinical studies are needed to evaluate idarubicin release around the DEE agents in tumor tissue and to confirm safety and efficacy.
Gunduz U, Keskin T, Tansık G, et al.
Idarubicin-loaded folic acid conjugated magnetic nanoparticles as a targetable drug delivery system for breast cancer.
Biomed Pharmacother. 2014; 68(6):729-36 [PubMed] Related Publications
Idarubicin-loaded folic acid conjugated magnetic nanoparticles as a targetable drug delivery system for breast cancer.
Biomed Pharmacother. 2014; 68(6):729-36 [PubMed] Related Publications
Conventional cancer chemotherapies cannot differentiate between healthy and cancer cells, and lead to severe side effects and systemic toxicity. Another major problem is the drug resistance development before or during the treatment. In the last decades, different kinds of controlled drug delivery systems have been developed to overcome these shortcomings. The studies aim targeted drug delivery to tumor site. Magnetic nanoparticles (MNP) are potentially important in cancer treatment since they can be targeted to tumor site by an externally applied magnetic field. In this study, MNPs were synthesized, covered with biocompatible polyethylene glycol (PEG) and conjugated with folic acid. Then, anti-cancer drug idarubicin was loaded onto the nanoparticles. Shape, size, crystal and chemical structures, and magnetic properties of synthesized nanoparticles were characterized. The characterization of synthesized nanoparticles was performed by dynamic light scattering (DLS), Fourier transform-infrared spectroscopy (FT-IR), transmission electron microscopy (TEM), scanning electron microscopy (SEM) analyses. Internalization and accumulation of MNPs in MCF-7 cells were illustrated by light and confocal microscopy. Empty MNPs did not have any toxicity in the concentration ranges of 0-500μg/mL on MCF-7 cells, while drug-loaded nanoparticles led to significant toxicity in a concentration-dependent manner. Besides, idarubicin-loaded MNPs exhibited higher toxicity compared to free idarubicin. The results are promising for improvement in cancer chemotherapy.
Ristic B, Bosnjak M, Arsikin K, et al.
Idarubicin induces mTOR-dependent cytotoxic autophagy in leukemic cells.
Exp Cell Res. 2014; 326(1):90-102 [PubMed] Related Publications
Idarubicin induces mTOR-dependent cytotoxic autophagy in leukemic cells.
Exp Cell Res. 2014; 326(1):90-102 [PubMed] Related Publications
We investigated if the antileukemic drug idarubicin induces autophagy, a process of programmed cellular self-digestion, in leukemic cell lines and primary leukemic cells. Transmission electron microscopy and acridine orange staining demonstrated the presence of autophagic vesicles and intracellular acidification, respectively, in idarubicin-treated REH leukemic cell line. Idarubicin increased punctuation/aggregation of microtubule-associated light chain 3B (LC3B), enhanced the conversion of LC3B-I to autophagosome-associated LC3B-II in the presence of proteolysis inhibitors, and promoted the degradation of the selective autophagic target p62, thus indicating the increase in autophagic flux. Idarubicin inhibited the phosphorylation of the main autophagy repressor mammalian target of rapamycin (mTOR) and its downstream target p70S6 kinase. The treatment with the mTOR activator leucine prevented idarubicin-mediated autophagy induction. Idarubicin-induced mTOR repression was associated with the activation of the mTOR inhibitor AMP-activated protein kinase and down-regulation of the mTOR activator Akt. The suppression of autophagy by pharmacological inhibitors or LC3B and beclin-1 genetic knockdown rescued REH cells from idarubicin-mediated oxidative stress, mitochondrial depolarization, caspase activation and apoptotic DNA fragmentation. Idarubicin also caused mTOR inhibition and cytotoxic autophagy in K562 leukemic cell line and leukocytes from chronic myeloid leukemia patients, but not healthy controls. By demonstrating mTOR-dependent cytotoxic autophagy in idarubicin-treated leukemic cells, our results warrant caution when considering combining idarubicin with autophagy inhibitors in leukemia therapy.
Hong M, Miao KR, Zhang R, et al.
High-dose idarubicin plus busulfan as conditioning regimen to autologous stem cell transplantation: promising post-remission therapy for acute myeloid leukemia in first complete remission?
Med Oncol. 2014; 31(6):980 [PubMed] Related Publications
High-dose idarubicin plus busulfan as conditioning regimen to autologous stem cell transplantation: promising post-remission therapy for acute myeloid leukemia in first complete remission?
Med Oncol. 2014; 31(6):980 [PubMed] Related Publications
The optimal post-remission therapy (PRT) for acute myeloid leukemia (AML) remains uncertain. We reported 32 AML patients in first complete remission (CR1) undergoing autologous hematopoietic stem cell transplantation (ASCT) with a characteristic conditioning regimen, termed I-Bu, based on high-dose idarubicin plus busulfan, which considerably strengthened antileukemic activity. Most patients were in better or intermediate-risk group except that cytogenetic or molecular risk information was missing for 18.7 % of the patients. Unpurged peripheral blood stem cells were used in all the cases. The adverse effects were mild and reversible. Only one case of transplant-related mortality was observed. All the patients in this study acquired hematopoietic reconstitution after ASCT. After a median follow-up of 30 (6-119) months, 24 patients (75.0 %) were alive in which 20 (62.5 %) patients were in continuous CR. There were 11 (34.4 %) patients who relapsed after HSCT. Cumulative relapse probability was about 40 % after 24 months. Median OS and DFS have not been reached. Patients in the better and intermediate-risk group had different clinical outcomes, but the differences were not statistically significant. ASCT with I-Bu regimen is possibly promising PRT for better and intermediate-risk AML patients in CR1.
Boulin M, Hillon P, Cercueil JP, et al.
Idarubicin-loaded beads for chemoembolisation of hepatocellular carcinoma: results of the IDASPHERE phase I trial.
Aliment Pharmacol Ther. 2014; 39(11):1301-13 [PubMed] Related Publications
Idarubicin-loaded beads for chemoembolisation of hepatocellular carcinoma: results of the IDASPHERE phase I trial.
Aliment Pharmacol Ther. 2014; 39(11):1301-13 [PubMed] Related Publications
BACKGROUND: A phase I dose-escalation trial of transarterial chemoembolisation (TACE) with idarubicin-loaded beads was performed in cirrhotic patients with hepatocellular carcinoma (HCC).
AIM: To estimate the maximum-tolerated dose (MTD) and to assess safety, efficacy, pharmacokinetics and quality of life.
METHODS: Patients received a single TACE session with injection of 2 mL drug-eluting beads (DEBs; DC Bead 300-500 μm) loaded with idarubicin. The idarubicin dose was escalated according to a modified continuous reassessment method. MTD was defined as the dose level closest to that causing dose-limiting toxicity (DLT) in 20% of patients.
RESULTS: Twenty-one patients were enrolled, including nine patients at 5 mg, six patients at 10 mg, and six patients at 15 mg. One patient at each dose level experienced DLT (acute myocardial infarction, hyperbilirubinaemia and elevated aspartate aminotransferase (AST) at 5-, 10- and 15-mg, respectively). The calculated MTD of idarubicin was 10 mg. The most frequent grade ≥3 adverse events were pain, elevated AST, elevated γ-glutamyltranspeptidase and thrombocytopenia. At 2 months, the objective response rate was 52% (complete response, 28%, and partial response, 24%) by modified Response Evaluation Criteria in Solid Tumours. The median time to progression was 12.1 months (95% CI 7.4 months--not reached); the median overall survival was 24.5 months (95% CI 14.7 months--not reached). Pharmacokinetic analysis demonstrated the ability of DEBs to release idarubicin slowly.
CONCLUSIONS: Using drug-eluting beads, the maximum-tolerated dose of idarubicin was 10 mg per TACE session. Encouraging responses and median time to progression were observed. Further clinical investigations are warranted (NCT01040559).
AIM: To estimate the maximum-tolerated dose (MTD) and to assess safety, efficacy, pharmacokinetics and quality of life.
METHODS: Patients received a single TACE session with injection of 2 mL drug-eluting beads (DEBs; DC Bead 300-500 μm) loaded with idarubicin. The idarubicin dose was escalated according to a modified continuous reassessment method. MTD was defined as the dose level closest to that causing dose-limiting toxicity (DLT) in 20% of patients.
RESULTS: Twenty-one patients were enrolled, including nine patients at 5 mg, six patients at 10 mg, and six patients at 15 mg. One patient at each dose level experienced DLT (acute myocardial infarction, hyperbilirubinaemia and elevated aspartate aminotransferase (AST) at 5-, 10- and 15-mg, respectively). The calculated MTD of idarubicin was 10 mg. The most frequent grade ≥3 adverse events were pain, elevated AST, elevated γ-glutamyltranspeptidase and thrombocytopenia. At 2 months, the objective response rate was 52% (complete response, 28%, and partial response, 24%) by modified Response Evaluation Criteria in Solid Tumours. The median time to progression was 12.1 months (95% CI 7.4 months--not reached); the median overall survival was 24.5 months (95% CI 14.7 months--not reached). Pharmacokinetic analysis demonstrated the ability of DEBs to release idarubicin slowly.
CONCLUSIONS: Using drug-eluting beads, the maximum-tolerated dose of idarubicin was 10 mg per TACE session. Encouraging responses and median time to progression were observed. Further clinical investigations are warranted (NCT01040559).
Kim H, Lee JH, Joo YD, et al.
Prospective, multicenter, phase II study on reducing the dosage of idarubicin and FLAG for patients younger than 65 years with resistant acute myeloid leukemia: a comparison with a higher dosage trial.
Acta Haematol. 2014; 132(1):87-96 [PubMed] Related Publications
Prospective, multicenter, phase II study on reducing the dosage of idarubicin and FLAG for patients younger than 65 years with resistant acute myeloid leukemia: a comparison with a higher dosage trial.
Acta Haematol. 2014; 132(1):87-96 [PubMed] Related Publications
We previously assessed continuous infusion (CI) of fludarabine and cytarabine plus idarubicin (CI-FLAG1) for patients under 65 years of age with resistant acute myeloid leukemia. Induction chemotherapy consisted of idarubicin (IDA) plus fludarabine and cytarabine (ARAC) as a 24-hour CI. In response to induction, 31.6% of patients achieved complete remission (CR) and in 68.4% the treatment failed. We concluded that CI-FLAG1 carried a high risk of toxicity and reduced CI-FLAG doses were recommended. Therefore, we revised the protocol (CI-FLAG2) by reducing the dose of IDA and ARAC. In total, 38 and 68 patients were enrolled into CI-FLAG1 and CI-FLAG2, respectively. When comparing outcomes between CI-FLAG1 and CI-FLAG2, there were no differences in terms of the CR rate (p = 0.306) and the overall response rate (ORR; p = 0.206). The treatment failure patterns were different between CI-FLAG1 and CI-FLAG2. The median overall survival showed only a trend towards longer survival in CI-FLAG2 (p = 0.074). Among intermediate-risk patients, there were high response rates favoring CI-FLAG2 in terms of the CR rate (p = 0.108), the ORR (p = 0.031), and overall survival (p = 0.033). This represented a relatively improved response rate compared to our previous study. There was decreased aplasia with dose reductions at the expense of increased resistance. A reduced dose of CI-FLAG might be most beneficial for intermediate-risk groups.
Liu Y, Chen F, Wang S, et al.
Low-dose triptolide in combination with idarubicin induces apoptosis in AML leukemic stem-like KG1a cell line by modulation of the intrinsic and extrinsic factors.
Cell Death Dis. 2013; 4:e948 [PubMed] Free Access to Full Article Related Publications
Low-dose triptolide in combination with idarubicin induces apoptosis in AML leukemic stem-like KG1a cell line by modulation of the intrinsic and extrinsic factors.
Cell Death Dis. 2013; 4:e948 [PubMed] Free Access to Full Article Related Publications
Leukemia stem cells (LSCs) are considered to be the main reason for relapse and are also regarded as a major hurdle for the success of acute myeloid leukemia chemotherapy. Thus, new drugs targeting LSCs are urgently needed. Triptolide (TPL) is cytotoxic to LSCs. Low dose of TPL enhances the cytotoxicity of idarubicin (IDA) in LSCs. In this study, the ability of TPL to induce apoptosis in leukemic stem cell (LSC)-like cells derived from acute myeloid leukemia cell line KG1a was investigated. LSC-like cells sorted from KG1a were subjected to cell cycle analysis and different treatments, and then followed by in vitro methyl thiazole tetrazolium bromide cytotoxicity assay. The effects of different drug combinations on cell viability, intracellular reactive-oxygen species (ROS) activity, colony-forming ability and apoptotic status were also examined. Combination index-isobologram analysis indicates a synergistic effect between TPL and IDA, which inhibits the colony-forming ability of LSC-like cells and induces their apoptosis. We further investigated the expression of Nrf2, HIF-1α and their downstream target genes. LSC-like cells treated with both TPL and IDA have increased levels of ROS, decreased expression of Nrf2 and HIF-1α pathways. Our findings indicate that the synergistic cytotoxicity of TPL and IDA in LSCs-like cells may attribute to both induction of ROS and inhibition of the Nrf2 and HIF-1α pathways.
Rigolin GM, Martinelli S, Formigaro L, et al.
Delirium in acute promyelocytic leukemia patients: two case reports.
BMC Res Notes. 2013; 6:469 [PubMed] Free Access to Full Article Related Publications
Delirium in acute promyelocytic leukemia patients: two case reports.
BMC Res Notes. 2013; 6:469 [PubMed] Free Access to Full Article Related Publications
BACKGROUND: Delirium is a frequently misdiagnosed and inadequately treated neuropsychiatric complication most commonly observed in terminally ill cancer patients. To our knowledge this is the first report describing delirium in two patients aged less than 60 years and enrolled in an intensive chemotherapeutic protocol for acute promyelocytic leukemia.
CASE PRESENTATION: Two female Caucasian acute promyelocytic leukemia patients aged 46 and 56 years developed delirium during their induction treatment with all-trans retinoic acid and idarubicin. In both cases symptoms were initially attributed to all-trans retinoic acid that was therefore immediately suspended. In these two patients several situations may have contribute to the delirium: in patient 1 a previous psychiatric disorder, concomitant treatments with steroids and benzodiazepines, a severe infection and central nervous system bleeding while in patient 2 steroid treatment and isolation. In patient 1 delirium was treated with short-term low-doses of haloperidol while in patient 2 non-pharmacologic interventions had a beneficial role. When the diagnosis of delirium was clear, induction treatment was resumed and both patients completed their therapeutic program without any relapse of the psychiatric symptoms. Both patients are alive and in complete remission as far as their leukemia is concerned.
CONCLUSIONS: We suggest that patients with acute promyelocytic leukemia eligible to intensive chemotherapy should be carefully evaluated by a multisciplinary team including psychiatrists in order to early recognize symptoms of delirium and avoid inadequate treatments. In case of delirium, both pharmacologic and non-pharmacologic interventions may be considered.
CASE PRESENTATION: Two female Caucasian acute promyelocytic leukemia patients aged 46 and 56 years developed delirium during their induction treatment with all-trans retinoic acid and idarubicin. In both cases symptoms were initially attributed to all-trans retinoic acid that was therefore immediately suspended. In these two patients several situations may have contribute to the delirium: in patient 1 a previous psychiatric disorder, concomitant treatments with steroids and benzodiazepines, a severe infection and central nervous system bleeding while in patient 2 steroid treatment and isolation. In patient 1 delirium was treated with short-term low-doses of haloperidol while in patient 2 non-pharmacologic interventions had a beneficial role. When the diagnosis of delirium was clear, induction treatment was resumed and both patients completed their therapeutic program without any relapse of the psychiatric symptoms. Both patients are alive and in complete remission as far as their leukemia is concerned.
CONCLUSIONS: We suggest that patients with acute promyelocytic leukemia eligible to intensive chemotherapy should be carefully evaluated by a multisciplinary team including psychiatrists in order to early recognize symptoms of delirium and avoid inadequate treatments. In case of delirium, both pharmacologic and non-pharmacologic interventions may be considered.
Kobayashi T, Ichikawa M, Nannya Y, Kurokawa M
The effect of decreased-dose idarubicin for elderly patients with acute myeloid leukemia.
Jpn J Clin Oncol. 2013; 43(10):1047-51 [PubMed] Related Publications
The effect of decreased-dose idarubicin for elderly patients with acute myeloid leukemia.
Jpn J Clin Oncol. 2013; 43(10):1047-51 [PubMed] Related Publications
We evaluated whether reduced-dose chemotherapy with 2 days of idarubicin (12 mg/m(2)) and 5 days of cytarabine (100 mg/m(2)) (2 + 5) is effective for patients aged 65-74 by retrospectively comparing the results with those aged 55-64 treated with 3 + 7. In 1999-2009, we treated 20 patients aged 65-74 with 2 + 5, and 23 patients aged 55-64 with 3 + 7. The complete remission rates by the first induction were 50.0 and 69.6% for older and younger groups (P = 0.203). Two-year overall survival rates were 55.9 and 32.3% for older and younger groups; 2-year rates of relapse-free survival for all these patients were 15.7 and 36.5%. The differences in overall and relapse-free survival were statistically insignificant (P = 0.726 and 0.413, respectively). The treatment results of 2 + 5 for the older group were not significantly worse compared with those of 3 + 7 for the younger. Therefore, elderly patients who do not tolerate 3 + 7 should still benefit from 2 + 5.
Nazha A, Kantarjian H, Ravandi F, et al.
Clofarabine, idarubicin, and cytarabine (CIA) as frontline therapy for patients ≤60 years with newly diagnosed acute myeloid leukemia.
Am J Hematol. 2013; 88(11):961-6 [PubMed] Free Access to Full Article Related Publications
Clofarabine, idarubicin, and cytarabine (CIA) as frontline therapy for patients ≤60 years with newly diagnosed acute myeloid leukemia.
Am J Hematol. 2013; 88(11):961-6 [PubMed] Free Access to Full Article Related Publications
Clofarabine is a second generation nucleoside analogue with activity in adults with acute myeloid leukemia (AML). A phase I trial of clofarabine, idarubicin, and cytarabine (CIA) in relapsed and refractory AML had shown an overall response rate (ORR) of 48%. To explore this combination further, we conducted a phase II study of (CIA) in patients with newly diagnosed AML ≤60 years. Patients ≥18-60 years with AML and adequate organ function were enrolled. Induction therapy consisted of clofarabine (C) 20 mg m⁻² IV daily (days 1-5), idarubicin (I) 10 mg m⁻² IV daily (days 1-3), and cytarabine (A) 1 g m⁻² IV daily (days 1-5). Patients in remission received up to six consolidation cycles (C 15 mg m⁻² × 3, I 8 mg m⁻² × 2, and A 0.75 g m⁻² × 3). Fifty-seven patients were evaluable. ORR was 79%. With a median follow up of 10.9 months, the median overall survival (OS) was not reached, the median event-free survival (EFS) was 13.5 months. Most toxicities were ≤grade 2. Four week mortality was 2%. In subgroup analysis, patients ≤40 years had better OS (P = 0.04) and EFS (P = 0.04) compared to patients >40 years. Compared to historical patients treated with idarubicin and cyarabine (IA), the OS and EFS were significantly longer for CIA treated patients. In multivariate analysis, CIA retained its favorable impact on OS compared to IA. Thus, CIA is an effective and safe therapy for patients ≤60 years with newly diagnosed AML.
Wu KN, Zhao YM, He Y, et al.
Rapamycin interacts synergistically with idarubicin to induce T-leukemia cell apoptosis in vitro and in a mesenchymal stem cell simulated drug-resistant microenvironment via Akt/mammalian target of rapamycin and extracellular signal-related kinase signaling pathways.
Leuk Lymphoma. 2014; 55(3):668-76 [PubMed] Related Publications
Rapamycin interacts synergistically with idarubicin to induce T-leukemia cell apoptosis in vitro and in a mesenchymal stem cell simulated drug-resistant microenvironment via Akt/mammalian target of rapamycin and extracellular signal-related kinase signaling pathways.
Leuk Lymphoma. 2014; 55(3):668-76 [PubMed] Related Publications
T-cell acute lymphoblastic leukemias (T-ALLs) are clonal lymphoid malignancies with a poor prognosis, and still a lack of effective treatment. Here we examined the interactions between the mammalian target of rapamycin (mTOR) inhibitor rapamycin and idarubicin (IDA) in a series of human T-ALL cell lines Molt-4, Jurkat, CCRF-CEM and CEM/C1. Co-exposure of cells to rapamycin and IDA synergistically induced T-ALL cell growth inhibition and apoptosis mediated by caspase activation via the intrinsic mitochondrial pathway and extrinsic pathway. Combined treatment with rapamycin and IDA down-regulated Bcl-2 and Mcl-1, and inhibited the activation of phosphoinositide 3-kinase (PI3K)/mTOR and extracellular signal-related kinase (ERK). They also played synergistic pro-apoptotic roles in the drug-resistant microenvironment simulated by mesenchymal stem cells (MSCs) as a feeder layer. In addition, MSCs protected T-ALL cells from IDA cytotoxicity by up-regulating ERK phosphorylation, while rapamycin efficiently reversed this protective effect. Taken together, we confirm the synergistic antitumor effects of rapamycin and IDA, and provide an insight into the potential future clinical applications of combined rapamycin-IDA regimens for treating T-cell malignancies.
Trifilio S, Zhou Z, Mehta J, et al.
Idarubicin appears equivalent to dose-intense daunorubicin for remission induction in patients with acute myeloid leukemia.
Leuk Res. 2013; 37(8):868-71 [PubMed] Related Publications
Idarubicin appears equivalent to dose-intense daunorubicin for remission induction in patients with acute myeloid leukemia.
Leuk Res. 2013; 37(8):868-71 [PubMed] Related Publications
Daunorubicin has historically been considered the anthracycline of choice at many cancer centers for the treatment of acute myeloid leukemia (AML). Drug shortages have required the substitution of daunorubicin with idarubicin. Randomized studies have shown idarubicin (10-12mg/m(2)) to be comparable or superior to standard dose daunorubicin (45-60mg/m(2)) for achieving complete remission (CR). Whether these results can be extrapolated to dose-intense daunorubicin (90mg/m(2)), recently shown to improve CR rates when compared to standard daunorubicin doses remains uncertain. This observational study was conducted at Northwestern Memorial Hospital (NMH) to compare CR rates. The results suggest idarubicin is equivalent to daunorubicin, and for some subsets of patients, idarubicin may have superior CR rates.
Creutzig U, Zimmermann M, Bourquin JP, et al.
Randomized trial comparing liposomal daunorubicin with idarubicin as induction for pediatric acute myeloid leukemia: results from Study AML-BFM 2004.
Blood. 2013; 122(1):37-43 [PubMed] Related Publications
Randomized trial comparing liposomal daunorubicin with idarubicin as induction for pediatric acute myeloid leukemia: results from Study AML-BFM 2004.
Blood. 2013; 122(1):37-43 [PubMed] Related Publications
Outcomes of patients with acute myeloid leukemia (AML) improve significantly by intensification of induction. To further intensify anthracycline dosage without increasing cardiotoxicity, we compared potentially less cardiotoxic liposomal daunorubicin (L-DNR) to idarubicin at a higher-than-equivalent dose (80 vs 12 mg/m(2) per day for 3 days) during induction. In the multicenter therapy-optimization trial AML-BFM 2004, 521 of 611 pediatric patients (85%) were randomly assigned to L-DNR or idarubicin induction. Five-year results in both treatment arms were similar (overall survival 76% ± 3% [L-DNR] vs 75% ± 3% [idarubicin], Plogrank = .65; event-free survival [EFS] 59% ± 3% vs 53% ± 3%, Plogrank = .25; cumulative incidence of relapse 29% ± 3% vs 31% ± 3%, P(Gray) = .75), as were EFS results for standard (72% ± 5% vs 68% ± 5%, Plogrank = .47) and high-risk (51% ± 4% vs 46% ± 4%, Plogrank = .45) patients. L-DNR resulted in significantly better probability of EFS in patients with t(8;21). Overall, treatment-related mortality was lower with L-DNR than idarubicin (2/257 vs 10/264 patients, P = .04). Grade 3/4 cardiotoxicity was rare after induction (4 L-DNR vs 5 idarubicin). Only 1 L-DNR and 3 idarubicin patients presented with subclinical or mild cardiomyopathy during follow-up. In conclusion, at the given dose, L-DNR has overall antileukemic activity comparable to idarubicin, promises to be more active in subgroups, and causes less treatment-related mortality. This trial was registered at www.clinicaltrials.gov as #NCT00111345.
Clavio M, Cruciani F, Minetto P, et al.
De novo AML patients with favourable-intermediate karyotype may benefit from the addition of low-dose gemtuzumab ozogamicin (GO) to fludarabine, Ara-C and idarubicin (FLAI): a contribution to the reopened "GO question".
Ann Hematol. 2013; 92(10):1309-18 [PubMed] Related Publications
De novo AML patients with favourable-intermediate karyotype may benefit from the addition of low-dose gemtuzumab ozogamicin (GO) to fludarabine, Ara-C and idarubicin (FLAI): a contribution to the reopened "GO question".
Ann Hematol. 2013; 92(10):1309-18 [PubMed] Related Publications
We report the final results of a prospective trial testing the combination of fludarabine, Ara-C and idarubicin (FLAI) followed by low-dose gemtuzumab ozogamicin (FLAI-GO) in 85 patients aged 60 years or more with CD33+ acute myeloid leukaemia (AML). Median age was 68 years (60-82); karyotype was unfavourable in 21 patients (24%), intermediate in 63 (74%) and favourable in 1 (2%). There were five therapy-related deaths. Of the 80 evaluable patients, 47 achieved complete response (CR) (58%); CR rates were 65 and 32% in good-intermediate/poor karyotype patients, respectively. Median length of CR was 7 months (3-76). The cumulative incidence of relapse was 84% with an actuarial survival of 50.3% at 1 year and 14.4% at 2 years. The study control population is an unselected consecutive historic cohort of 104 patients treated with the FLAI regimen, who were matched for age and prognostic factors. CR rates after FLAI-GO and FLAI were comparable. However, patients with de novo AML and intermediate-favourable karyotype receiving GO had a significantly lower risk of relapse at 2 years as compared to patients not receiving GO (n = 77) (40 vs 80%, p = 0.01) and significantly better disease-free survival (p = 0.018) and overall survival (p = 0.022).
Teuffel O, Leibundgut K, Lehrnbecher T, et al.
Anthracyclines during induction therapy in acute myeloid leukaemia: a systematic review and meta-analysis.
Br J Haematol. 2013; 161(2):192-203 [PubMed] Related Publications
Anthracyclines during induction therapy in acute myeloid leukaemia: a systematic review and meta-analysis.
Br J Haematol. 2013; 161(2):192-203 [PubMed] Related Publications
This systematic review and meta-analysis compared the efficacy of different anthracyclines and anthracycline dosing schedules for induction therapy in acute myeloid leukaemia in children and adults younger than 60 years of age. Twenty-nine randomized controlled trials were eligible for inclusion in the review. Idarubicin (IDA), in comparison to daunorubicin (DNR), reduced remission failure rates (risk ratio (RR) 0·81; 95% confidence interval (CI), 0·66-0·99; P = 0·04), but did not alter rates of early death or overall mortality. Superiority of IDA for remission induction was limited to studies with a DNR/IDA dose ratio <5 (ratio <5: RR 0·65; 95% CI, 0·51-0·81; P < 0·001; ratio ≥5: RR 1·03; 95% CI, 0·91-1·16; P = 0·63). Higher-dose DNR, compared to lower-dose DNR, was associated with reduced rates for remission failure (RR 0·75; 95% CI, 0·60-0·94; P = 0·003) and overall mortality (RR 0·83; 95% CI, 0·75-0·93; P < 0·001), but not for early death. Comparisons of several other anthracycline derivates did not reveal significant differences in outcomes. Survival estimates in adults suggest that both high-dose DNR (90 mg/m(2) daily × 3 or 50 mg/m(2) daily × 5) and IDA (12 mg/m(2) daily × 3) can achieve 5-year survival rates of between 40 and 50 percent.
Erba HP, Sayar H, Juckett M, et al.
Safety and pharmacokinetics of the antisense oligonucleotide (ASO) LY2181308 as a single-agent or in combination with idarubicin and cytarabine in patients with refractory or relapsed acute myeloid leukemia (AML).
Invest New Drugs. 2013; 31(4):1023-34 [PubMed] Free Access to Full Article Related Publications
Safety and pharmacokinetics of the antisense oligonucleotide (ASO) LY2181308 as a single-agent or in combination with idarubicin and cytarabine in patients with refractory or relapsed acute myeloid leukemia (AML).
Invest New Drugs. 2013; 31(4):1023-34 [PubMed] Free Access to Full Article Related Publications
Survivin is expressed in tumor cells, including acute myeloid leukemia (AML), regulates mitosis, and prevents tumor cell death. The antisense oligonucleotide sodium LY2181308 (LY2181308) inhibits survivin expression and may cause cell cycle arrest and restore apoptosis in AML. In this study, the safety, pharmacokinetics, and pharmacodynamics/efficacy of LY2181308 was examined in AML patients, first in a cohort with monotherapy (n = 8) and then post-amendment in a cohort with the combination of cytarabine and idarubicin treatment (n = 16). LY2181308 was administered with a loading dosage of three consecutive daily infusions of 750 mg followed by weekly intravenous (IV) maintenance doses of 750 mg. Cytarabine 1.5 g/m(2) was administered as a 4-hour IV infusion on Days 3, 4, and 5 of Cycle 1, and idarubicin 12 mg/m(2) was administered as a 30-minute IV infusion on Days 3, 4, and 5 of Cycle 1. Cytarabine and idarubicin were administered on Days 1, 2, and 3 of each subsequent 28-day cycle. Reduction of survivin was evaluated in peripheral blasts and bone marrow. Single-agent LY2181308 was well tolerated and survivin was reduced only in patients with a high survivin expression. In combination with chemotherapy, 4/16 patients had complete responses, 1/16 patients had incomplete responses, and 4/16 patients had cytoreduction. Nine patients died on study: 6 (monotherapy), 3 (combination). LY2181308 alone is well tolerated in patients with AML. In combination with cytarabine and idarubicin, LY2181308 does not appear to cause additional toxicity, and has shown some clinical benefit needing confirmation in future clinical trials.
Bertoli S, Bérard E, Huguet F, et al.
Time from diagnosis to intensive chemotherapy initiation does not adversely impact the outcome of patients with acute myeloid leukemia.
Blood. 2013; 121(14):2618-26 [PubMed] Related Publications
Time from diagnosis to intensive chemotherapy initiation does not adversely impact the outcome of patients with acute myeloid leukemia.
Blood. 2013; 121(14):2618-26 [PubMed] Related Publications
In acute myeloid leukemia (AML), new strategies assess the potential benefit of genetically targeted therapy at diagnosis. This implies waiting for laboratory tests and therefore a delay in initiation of chemotherapy. We studied the impact of time from diagnosis to treatment (TDT) on overall survival, early death, and response rate in a retrospective series of 599 newly diagnosed AML patients treated by induction chemotherapy between 2000 and 2009. The effect of TDT was assessed using multivariate analysis. TDT was analyzed as a continuous variable using a specific polynomial function to model the shape and form of the relationship. The median TDT was 8 days (interquartile range, 4-16) and was significantly longer in patients with a white blood cell count (WBC) <50 Giga per liter (G/L) (P < .0001) and in older patients (P = .0004). In multivariate analysis, TDT had no impact on overall survival (P = .4095) compared with age >60 years, secondary AML, WBC >50 G/L, European LeukemiaNet risk groups, and Eastern Cooperative Oncology Group performance status. Furthermore, TDT was not associated with response rate and early death. Thus, waiting a short period of time for laboratory tests to characterize leukemias better and design adapted therapeutic strategies at diagnosis seems possible.
Kim WS, Lee MJ, Kim DH, et al.
5'-OH-5-nitro-Indirubin oxime (AGM130), an Indirubin derivative, induces apoptosis of Imatinib-resistant chronic myeloid leukemia cells.
Leuk Res. 2013; 37(4):427-33 [PubMed] Related Publications
5'-OH-5-nitro-Indirubin oxime (AGM130), an Indirubin derivative, induces apoptosis of Imatinib-resistant chronic myeloid leukemia cells.
Leuk Res. 2013; 37(4):427-33 [PubMed] Related Publications
Imatinib is a highly effective drug for the treatment of chronic myeloid leukemia (CML) that targets the BCR-ABL kinase. However, a number of patients have CML that is resistant to Imatinib treatment. In this report, we developed AGM130 as a potential therapeutic drug for Imatinib-resistant CML treatment. The AGM130 compound is derived from Indirubin, which is an ingredient of Danggui Longhui Wan and known as a cyclin-dependent kinase (CDK) inhibitor. The water solubility of AGM130 is more enhanced than that of the original form of Indirubin, which has very poor water solubility. Our data showed that the AGM130 compound efficiently decreased the viability of CML-derived K562 cells. Moreover, this compound also efficiently decreased the viability of Imatinib-resistant K562 cells in in vitro and in vivo systems. In addition, like Indirubin, AGM130 also inhibited phosphorylation of retinoblastoma protein (Rb), which is a major substrate of CDK. Conclusively, our data suggest that AGM130 is a strong candidate for treating Imatinib-resistant CML.
Gardin C, Chevret S, Pautas C, et al.
Superior long-term outcome with idarubicin compared with high-dose daunorubicin in patients with acute myeloid leukemia age 50 years and older.
J Clin Oncol. 2013; 31(3):321-7 [PubMed] Related Publications
Superior long-term outcome with idarubicin compared with high-dose daunorubicin in patients with acute myeloid leukemia age 50 years and older.
J Clin Oncol. 2013; 31(3):321-7 [PubMed] Related Publications
PURPOSE: Although standard chemotherapy remains associated with a poor outcome in older patients with acute myeloid leukemia (AML), it is unclear which patients can survive long enough to be considered as cured. This study aimed to identify factors influencing the long-term outcome in these patients.
PATIENTS AND METHODS: The study included 727 older patients with AML (median age, 67 years) treated in two idarubicin (IDA) versus daunorubicin (DNR) Acute Leukemia French Association trials. Prognostic analysis was based on standard univariate and multivariate models and also included a cure fraction model to focus on long-term outcome.
RESULTS: Age, WBC count, secondary AML, Eastern Cooperative Oncology Group (ECOG) performance status (PS), and adverse-risk and favorable-risk AML subsets (European LeukemiaNet classification) all influenced complete remission (CR) rate and overall survival (OS). IDA random assignment was associated with higher CR rate, but not with longer OS (P = .13). The overall cure rate was 13.3%. Older age and ECOG-PS more than 1 negatively influenced cure rate, which was higher in patients with favorable-risk AML (39.1% v 8.0% in adverse-risk AML; P < .001) and those treated with IDA (16.6% v 9.8% with DNR; P = .018). The long-term impact of IDA was still observed in patients younger than age 65 years, although all of the younger patients in the DNR control arm received high DNR doses (cure rate, 27.4% for IDA v 15.9% for DNR; P = .049). In multivariate analysis, IDA random assignment remained associated with a higher cure rate (P = .04), together with younger age and favorable-risk AML, despite not influencing OS (P = .11).
CONCLUSION: In older patients with AML, younger age, favorable-risk AML, and IDA treatment predict a better long-term outcome.
PATIENTS AND METHODS: The study included 727 older patients with AML (median age, 67 years) treated in two idarubicin (IDA) versus daunorubicin (DNR) Acute Leukemia French Association trials. Prognostic analysis was based on standard univariate and multivariate models and also included a cure fraction model to focus on long-term outcome.
RESULTS: Age, WBC count, secondary AML, Eastern Cooperative Oncology Group (ECOG) performance status (PS), and adverse-risk and favorable-risk AML subsets (European LeukemiaNet classification) all influenced complete remission (CR) rate and overall survival (OS). IDA random assignment was associated with higher CR rate, but not with longer OS (P = .13). The overall cure rate was 13.3%. Older age and ECOG-PS more than 1 negatively influenced cure rate, which was higher in patients with favorable-risk AML (39.1% v 8.0% in adverse-risk AML; P < .001) and those treated with IDA (16.6% v 9.8% with DNR; P = .018). The long-term impact of IDA was still observed in patients younger than age 65 years, although all of the younger patients in the DNR control arm received high DNR doses (cure rate, 27.4% for IDA v 15.9% for DNR; P = .049). In multivariate analysis, IDA random assignment remained associated with a higher cure rate (P = .04), together with younger age and favorable-risk AML, despite not influencing OS (P = .11).
CONCLUSION: In older patients with AML, younger age, favorable-risk AML, and IDA treatment predict a better long-term outcome.
Favelier S, Boulin M, Hamza S, et al.
Lipiodol trans-arterial chemoembolization of hepatocellular carcinoma with idarubicin: first experience.
Cardiovasc Intervent Radiol. 2013; 36(4):1039-46 [PubMed] Related Publications
Lipiodol trans-arterial chemoembolization of hepatocellular carcinoma with idarubicin: first experience.
Cardiovasc Intervent Radiol. 2013; 36(4):1039-46 [PubMed] Related Publications
BACKGROUND: There is still no consensus about the best chemotherapeutic agent for transarterial chemoembolization (TACE). A recent in vitro study demonstrated that idarubicin, an anthracycline, was by far the most cytotoxic drug on human hepatocellular carcinoma (HCC) cell lines. Idarubicin is much more lipophilic than doxorubicin, leading to higher cell penetration through lipidic membranes and greater accumulation of the drug in the lipiodol. Furthermore, idarubicin has the ability to overcome multidrug resistance. Therefore, we designed this pilot human study to evaluate the safety and efficacy of lipiodol TACE using idarubicin.
METHODS: In 21 consecutive patients treated by lipiodol TACE with idarubicin (10 mg) for HCC, safety data, tumor response (Response Evaluation Criteria in Solid Tumors, mRECIST), time to treatment failure (TTTF), and overall survival were evaluated.
RESULTS: Postembolization syndrome was observed after 30.9% (17 of 55) of sessions. No patient died from a TACE-related complication. No hematological grade 3-5 adverse event was observed. At least one grade 3 or higher adverse event occurred in 19% (4 of 21) of patients. On imaging, no progression was encountered; four patients (24%) exhibited stable disease, 12 (57%) exhibited a partial response, and five (19%) exhibited a complete response. Median TTTF was 16.7 months (Kaplan-Meier analysis). At 6 months, 94.7% (95% confidence interval [CI] 68.1-99.2) of patients did not reach treatment failure, whereas treatment failure was not reached in 50.6% (95% CI 21.6-73.9) of patients at 1 year. Overall survival was 83.5% (95% CI 57-94.4) at 1 year.
CONCLUSION: Idarubicin seems safe and effective in lipiodol TACE of HCC. This warrants further study to determine the potential of this drug to replace doxorubicin for TACE.
METHODS: In 21 consecutive patients treated by lipiodol TACE with idarubicin (10 mg) for HCC, safety data, tumor response (Response Evaluation Criteria in Solid Tumors, mRECIST), time to treatment failure (TTTF), and overall survival were evaluated.
RESULTS: Postembolization syndrome was observed after 30.9% (17 of 55) of sessions. No patient died from a TACE-related complication. No hematological grade 3-5 adverse event was observed. At least one grade 3 or higher adverse event occurred in 19% (4 of 21) of patients. On imaging, no progression was encountered; four patients (24%) exhibited stable disease, 12 (57%) exhibited a partial response, and five (19%) exhibited a complete response. Median TTTF was 16.7 months (Kaplan-Meier analysis). At 6 months, 94.7% (95% confidence interval [CI] 68.1-99.2) of patients did not reach treatment failure, whereas treatment failure was not reached in 50.6% (95% CI 21.6-73.9) of patients at 1 year. Overall survival was 83.5% (95% CI 57-94.4) at 1 year.
CONCLUSION: Idarubicin seems safe and effective in lipiodol TACE of HCC. This warrants further study to determine the potential of this drug to replace doxorubicin for TACE.


 Liver Cancer
Liver Cancer