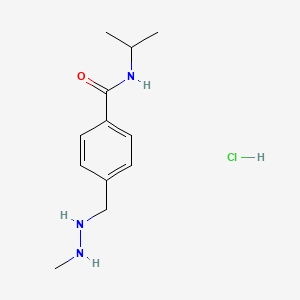
Procarbazine
"An antineoplastic agent used primarily in combination with mechlorethamine, vincristine, and prednisone (the MOPP protocol) in the treatment of Hodgkin's disease." (MeSH 2013)
Found this page useful?
 Web Resources: Procarbazine
Web Resources: Procarbazine Latest Research Publications
Latest Research PublicationsWeb Resources: Procarbazine (6 links)
Cancer Research UK
Irish Cancer Society
Macmillan Cancer Support
MedlinePlus
NHS Evidence
 Procarbazine - Substance Summary
Procarbazine - Substance Summary
PubChem
Latest Research Publications
This list of publications is regularly updated (Source: PubMed).
Teepen JC, de Vroom SL, van Leeuwen FE, et al.
Risk of subsequent gastrointestinal cancer among childhood cancer survivors: A systematic review.
Cancer Treat Rev. 2016; 43:92-103 [PubMed] Related Publications
Risk of subsequent gastrointestinal cancer among childhood cancer survivors: A systematic review.
Cancer Treat Rev. 2016; 43:92-103 [PubMed] Related Publications
BACKGROUND: Childhood cancer survivors (CCS) are at increased risk of developing subsequent malignant neoplasms, including gastrointestinal (GI) cancer. We performed a systematic review to summarize all available literature on the risk of, risk factors for, and outcome after subsequent GI cancer among CCS.
METHODS: A systematic search of the literature databases Medline/PubMed (1945-2014) and Embase (1947-2014) was performed to identify studies that consisted of ⩾1000 CCS and assessed incidence of or mortality from subsequent GI cancer as an outcome.
RESULTS: A total of 45 studies were included. Studies that reported risk measures for subsequent GI cancer compared to the general population showed a 3.2 to 9.7-fold elevated risk in cohort studies including all childhood cancer types. Abdominal radiotherapy was associated with an increased risk of subsequent GI cancer in all four studies that assessed this risk. Survivors who had received procarbazine and platinum agents were also suggested to be at increased risk.
CONCLUSION: Abdominal radiotherapy is a risk factor for developing a subsequent GI cancer. Few studies examined detailed treatment-related risk factors and most studies had small number of GI cancer cases. Therefore, no conclusions could be drawn on the effect of time since childhood cancer on GI cancer risk and on outcome after a subsequent GI cancer. Additional research is necessary to further explore risk factors for and outcome after a subsequent GI cancer, and to systematically evaluate the harms and benefits of GI screening among high-risk survivors in order to give sound screening recommendations.
METHODS: A systematic search of the literature databases Medline/PubMed (1945-2014) and Embase (1947-2014) was performed to identify studies that consisted of ⩾1000 CCS and assessed incidence of or mortality from subsequent GI cancer as an outcome.
RESULTS: A total of 45 studies were included. Studies that reported risk measures for subsequent GI cancer compared to the general population showed a 3.2 to 9.7-fold elevated risk in cohort studies including all childhood cancer types. Abdominal radiotherapy was associated with an increased risk of subsequent GI cancer in all four studies that assessed this risk. Survivors who had received procarbazine and platinum agents were also suggested to be at increased risk.
CONCLUSION: Abdominal radiotherapy is a risk factor for developing a subsequent GI cancer. Few studies examined detailed treatment-related risk factors and most studies had small number of GI cancer cases. Therefore, no conclusions could be drawn on the effect of time since childhood cancer on GI cancer risk and on outcome after a subsequent GI cancer. Additional research is necessary to further explore risk factors for and outcome after a subsequent GI cancer, and to systematically evaluate the harms and benefits of GI screening among high-risk survivors in order to give sound screening recommendations.
Webre C, Shonka N, Smith L, et al.
PC or PCV, That Is the Question: Primary Anaplastic Oligodendroglial Tumors Treated with Procarbazine and CCNU With and Without Vincristine.
Anticancer Res. 2015; 35(10):5467-72 [PubMed] Related Publications
PC or PCV, That Is the Question: Primary Anaplastic Oligodendroglial Tumors Treated with Procarbazine and CCNU With and Without Vincristine.
Anticancer Res. 2015; 35(10):5467-72 [PubMed] Related Publications
BACKGROUND: While procarbazine with 1-(2-chloroethyl)-3-cyclohexyl-1-nitrosourea (PC) added to vincristine (PCV) was proven beneficial in the treatment of co-deleted anaplastic oligodendroglioma (AO), the question of whether PC alone is sufficient is important, as vincristine adds toxicity with uncertain benefit. This retrospective study provides a comparison of PC and PCV.
PATIENTS AND METHODS: Patients diagnosed with AO treated at the M.D. Anderson Cancer Center from June 1, 1993 to October 13, 2009 were selected from the database and were eligible if diagnosed with a primary AO and treated with either PC or PCV at some point. Ninety-seven patients were treated with such chemotherapy before first progression.
RESULTS: Initial treatment included radiation and chemotherapy (81.4%) or chemotherapy alone (18.6%). Twenty-one patients (21.6%) received PC during primary treatment, while 76 patients (78.4%) received PCV. Eleven patients reported neurotoxicity in the PCV arm vs. none in the PC arm. Out of the 97 patients, 45 were alive at last contact, with a median follow-up of 9.9 years. The median overall survival was 6.5 years (95% confidence interval=4.8-16.7 years), while the median progression-free survival was 2.9 years (95% confidence interval=2.0-6.3 years); these differences were not significant (p=0.61 and p=0.28, respectively).
CONCLUSION: Initial therapy with PC achieved comparable results to those of PCV with a median follow-up of 9.9 years. Neurotoxicity was more frequent with vincristine. Although selecting only for patients with AO, rather than those with mixed histology, increased the likelihood of selecting for patients with tumors with co-deletions, further studies with correlative co-deletion status are required.
PATIENTS AND METHODS: Patients diagnosed with AO treated at the M.D. Anderson Cancer Center from June 1, 1993 to October 13, 2009 were selected from the database and were eligible if diagnosed with a primary AO and treated with either PC or PCV at some point. Ninety-seven patients were treated with such chemotherapy before first progression.
RESULTS: Initial treatment included radiation and chemotherapy (81.4%) or chemotherapy alone (18.6%). Twenty-one patients (21.6%) received PC during primary treatment, while 76 patients (78.4%) received PCV. Eleven patients reported neurotoxicity in the PCV arm vs. none in the PC arm. Out of the 97 patients, 45 were alive at last contact, with a median follow-up of 9.9 years. The median overall survival was 6.5 years (95% confidence interval=4.8-16.7 years), while the median progression-free survival was 2.9 years (95% confidence interval=2.0-6.3 years); these differences were not significant (p=0.61 and p=0.28, respectively).
CONCLUSION: Initial therapy with PC achieved comparable results to those of PCV with a median follow-up of 9.9 years. Neurotoxicity was more frequent with vincristine. Although selecting only for patients with AO, rather than those with mixed histology, increased the likelihood of selecting for patients with tumors with co-deletions, further studies with correlative co-deletion status are required.
Thomas-Teinturier C, Allodji RS, Svetlova E, et al.
Ovarian reserve after treatment with alkylating agents during childhood.
Hum Reprod. 2015; 30(6):1437-46 [PubMed] Related Publications
Ovarian reserve after treatment with alkylating agents during childhood.
Hum Reprod. 2015; 30(6):1437-46 [PubMed] Related Publications
STUDY QUESTION: What is the effect of different alkylating agents used without pelvic radiation to treat childhood cancer in girls on the ovarian reserve in survivors?
SUMMARY ANSWER: Ovarian reserve seems to be particularly reduced in survivors who received procarbazine (in most cases for Hodgkin lymphoma) or high-dose chemotherapy; procarbazine but not cyclophosphamide dose is associated with diminished ovarian reserve.
WHAT IS KNOWN ALREADY: A few studies have demonstrated diminished ovarian reserve in survivors after various combination therapies, but the individual role of each treatment is difficult to assess.
STUDY DESIGN: Prospective cross-sectional study, involving 105 survivors and 20 controls.
PARTICIPANTS/MATERIALS, SETTING, METHODS: One hundred and five survivors aged 17-40 years and 20 controls investigated on Days 2-5 of a menstrual cycle or Day 7 of an oral contraceptive pill-free interval.
MAIN OUTCOME MEASURES: ovarian surface area (OS), total number of antral follicles (AFC), serum levels of follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol and anti-Müllerian hormone (AMH).
MAIN RESULTS AND THE ROLE OF CHANCE: Survivors had a lower OS than controls: 3.5 versus 4.4 cm(2) per ovary (P = 0.0004), and lower AMH levels: 10.7 versus 22 pmol/l (P = 0.003). Ovarian markers (OS, AMH, AFC) were worse in patients who received high-dose compared with conventional-dose alkylating agents (P = 0.01 for OS, P = 0.002 for AMH, P < 0.0001 for AFC). Hodgkin lymphoma survivors seemed to have a greater reduction in ovarian reserve than survivors of leukaemia (P = 0.04 for AMH, P = 0.01 for AFC), sarcoma (P = 0.04 for AMH, P = 0.04 for AFC) and other lymphomas (P = 0.04 for AFC). A multiple linear regression analysis showed that procarbazine but not cyclophosphamide nor ifosfamide dose was associated with reduced OS (P = 0.0003), AFC (P = 0.0007), AMH (P < 0.0001) and higher FSH levels (P < 0.0001).
LIMITATIONS, REASONS FOR CAUTION: The small percentage of participating survivors (28%) from the total cohort does not allow conclusion on fertility issues because of possible response bias. The association between procarbazine and HL makes it impossible to dissociate their individual impacts on ovarian reserve. The number of controls is small, but ovarian volume and AMH levels in survivors were compared with published normal values and results were unchanged.
WIDER IMPLICATIONS OF THE FINDINGS: Early detection and follow-up of compromised ovarian function after cancer therapy should help physicians to counsel young survivors about their fertility window. However, longitudinal follow-up is required to determine the rate of progression from low ovarian reserve to premature ovarian failure.
STUDY FUNDING/COMPETING INTERESTS: La Ligue contre le Cancer (grant no., PRAYN7497). The authors have no competing interests to disclose.
SUMMARY ANSWER: Ovarian reserve seems to be particularly reduced in survivors who received procarbazine (in most cases for Hodgkin lymphoma) or high-dose chemotherapy; procarbazine but not cyclophosphamide dose is associated with diminished ovarian reserve.
WHAT IS KNOWN ALREADY: A few studies have demonstrated diminished ovarian reserve in survivors after various combination therapies, but the individual role of each treatment is difficult to assess.
STUDY DESIGN: Prospective cross-sectional study, involving 105 survivors and 20 controls.
PARTICIPANTS/MATERIALS, SETTING, METHODS: One hundred and five survivors aged 17-40 years and 20 controls investigated on Days 2-5 of a menstrual cycle or Day 7 of an oral contraceptive pill-free interval.
MAIN OUTCOME MEASURES: ovarian surface area (OS), total number of antral follicles (AFC), serum levels of follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol and anti-Müllerian hormone (AMH).
MAIN RESULTS AND THE ROLE OF CHANCE: Survivors had a lower OS than controls: 3.5 versus 4.4 cm(2) per ovary (P = 0.0004), and lower AMH levels: 10.7 versus 22 pmol/l (P = 0.003). Ovarian markers (OS, AMH, AFC) were worse in patients who received high-dose compared with conventional-dose alkylating agents (P = 0.01 for OS, P = 0.002 for AMH, P < 0.0001 for AFC). Hodgkin lymphoma survivors seemed to have a greater reduction in ovarian reserve than survivors of leukaemia (P = 0.04 for AMH, P = 0.01 for AFC), sarcoma (P = 0.04 for AMH, P = 0.04 for AFC) and other lymphomas (P = 0.04 for AFC). A multiple linear regression analysis showed that procarbazine but not cyclophosphamide nor ifosfamide dose was associated with reduced OS (P = 0.0003), AFC (P = 0.0007), AMH (P < 0.0001) and higher FSH levels (P < 0.0001).
LIMITATIONS, REASONS FOR CAUTION: The small percentage of participating survivors (28%) from the total cohort does not allow conclusion on fertility issues because of possible response bias. The association between procarbazine and HL makes it impossible to dissociate their individual impacts on ovarian reserve. The number of controls is small, but ovarian volume and AMH levels in survivors were compared with published normal values and results were unchanged.
WIDER IMPLICATIONS OF THE FINDINGS: Early detection and follow-up of compromised ovarian function after cancer therapy should help physicians to counsel young survivors about their fertility window. However, longitudinal follow-up is required to determine the rate of progression from low ovarian reserve to premature ovarian failure.
STUDY FUNDING/COMPETING INTERESTS: La Ligue contre le Cancer (grant no., PRAYN7497). The authors have no competing interests to disclose.
van den Bent MJ
Practice changing mature results of RTOG study 9802: another positive PCV trial makes adjuvant chemotherapy part of standard of care in low-grade glioma.
Neuro Oncol. 2014; 16(12):1570-4 [PubMed] Free Access to Full Article Related Publications
Practice changing mature results of RTOG study 9802: another positive PCV trial makes adjuvant chemotherapy part of standard of care in low-grade glioma.
Neuro Oncol. 2014; 16(12):1570-4 [PubMed] Free Access to Full Article Related Publications
The long-term follow-up of the RTOG 9802 trial that compared 54 Gy of radiotherapy (RT) with the same RT followed by adjuvant procarbazine, CCNU, and vincristine (PCV) chemotherapy in high-risk low-grade glioma shows a major increase in survival after adjuvant PCV chemotherapy. Median overall survival increased from 7.8 years to 13.3 years, with a hazard ratio of death of 0.59 (log rank: P = .002). This increase in survival was observed despite the fact that 77% of patients who progressed after RT alone received salvage chemotherapy. With this outcome, RT + PCV is now to be considered standard of care for low-grade glioma requiring postsurgical adjuvant treatment. Unfortunately, studies on molecular correlates associated with response are still lacking. This is now the third trial showing benefit from the addition of PCV to RT in grade II or III diffuse glioma. The optimal parameter for selecting patients for adjuvant PCV has not yet been fully elucidated, but several candidate markers have so far emerged. It is still unclear whether temozolomide can replace PCV and whether initial management with chemotherapy only is a safe initial treatment. Potentially, that may adversely affect overall survival, but concerns for delayed RT-induced neurotoxicity may limit acceptance of early RT in patients with expected long term survival. The current evidence supports that in future trials, grades II and III tumors with similar molecular backgrounds should be combined, and trials should focus on molecular glial subtype regardless of grade.
Taal W, van der Rijt CC, Dinjens WN, et al.
Treatment of large low-grade oligodendroglial tumors with upfront procarbazine, lomustine, and vincristine chemotherapy with long follow-up: a retrospective cohort study with growth kinetics.
J Neurooncol. 2015; 121(2):365-72 [PubMed] Related Publications
Treatment of large low-grade oligodendroglial tumors with upfront procarbazine, lomustine, and vincristine chemotherapy with long follow-up: a retrospective cohort study with growth kinetics.
J Neurooncol. 2015; 121(2):365-72 [PubMed] Related Publications
We treated patients with newly diagnosed and large low-grade oligodendroglial tumors with upfront procarbazine, CCNU and vincristine (PCV) in order to delay radiotherapy. Patients were treated with PCV for a maximum of 6 cycles. The response to treatment was defined according to the RANO criteria; in addition change over time of mean tumor diameters (growth kinetics) was calculated. Thirty-two patients were treated between 1998 and 2006, 18 of which were diagnosed with 1p/19q co-deleted tumors. Median follow-up duration was 8 years (range 0.5-13 years). The median overall survival (mOS) was 120 months and the median progression-free survival (mPFS) was 46 months. Growth kinetics showed an ongoing decrease of the mean tumor diameter after completion of chemotherapy, during a median time of 35 months, but an increase of the mean tumor diameter did not herald progression as detected by RANO criteria. 1p/19q co-deletion was associated with a significant increase in OS (mOS 83 months versus not reached for codeleted tumors; p = 0.003)) and PFS (mPFS 35 months versus 67 months for codeleted tumors; p = 0.024). Patients with combined 1p/19q loss had a 10 year PFS of 34 % and the radiotherapy in these patients was postponed for a median period of more than 6 years. This long-term follow-up study indicates that upfront PCV chemotherapy is associated with long PFS and OS and delays radiotherapy for a considerable period of time in patients with low-grade oligodendroglial tumors, in particular with combined 1p/19q loss.
Kraft SL, Baker NM, Carpenter J, Bostwick JR
Procarbazine and antidepressants: a retrospective review of the risk of serotonin toxicity.
Psychooncology. 2014; 23(1):108-13 [PubMed] Related Publications
Procarbazine and antidepressants: a retrospective review of the risk of serotonin toxicity.
Psychooncology. 2014; 23(1):108-13 [PubMed] Related Publications
BACKGROUND: Procarbazine is an anticancer agent that also inhibits monoamine oxidase, an enzyme responsible for the metabolism of various catecholamines, including serotonin.
METHODS: A retrospective chart review of lymphoma patients who were treated with both procarbazine and an antidepressant, as well as procarbazine alone, was performed to determine if signs and symptoms of serotonin toxicity were present.
RESULTS: A total of 65 patients received procarbazine between 2004 and 2010 and were eligible to be included in the study. Twenty-six of these patients received an antidepressant in combination with procarbazine, with selective serotonin reuptake inhibitors being the most common type of antidepressant. No patients in the study were diagnosed with serotonin toxicity, nor did any meet Hunter's diagnostic criteria for serotonin toxicity. Diarrhea, tremor, and shivering were the symptoms from Sternbach's criteria that were further analyzed, with diarrhea occurring 8.54% of the time, tremor occurring 5.53% of the time, and shivering occurring 2.51% of the time in patients who received an antidepressant with their procarbazine. Despite these symptoms, the diagnosis of serotonin toxicity according to Sternbach's criteria was determined to be unlikely.
CONCLUSIONS: In this small sample of patients treated with procarbazine plus an antidepressant (most typically SSRIs), there were no reports of serotonin toxicity, nor did any patients demonstrate symptoms consistent with serotonin toxicity. The authors urge clinicians to ensure depression is adequately managed in cancer patients who are undergoing procarbazine therapy, starting with typical first-line antidepressant agents.
METHODS: A retrospective chart review of lymphoma patients who were treated with both procarbazine and an antidepressant, as well as procarbazine alone, was performed to determine if signs and symptoms of serotonin toxicity were present.
RESULTS: A total of 65 patients received procarbazine between 2004 and 2010 and were eligible to be included in the study. Twenty-six of these patients received an antidepressant in combination with procarbazine, with selective serotonin reuptake inhibitors being the most common type of antidepressant. No patients in the study were diagnosed with serotonin toxicity, nor did any meet Hunter's diagnostic criteria for serotonin toxicity. Diarrhea, tremor, and shivering were the symptoms from Sternbach's criteria that were further analyzed, with diarrhea occurring 8.54% of the time, tremor occurring 5.53% of the time, and shivering occurring 2.51% of the time in patients who received an antidepressant with their procarbazine. Despite these symptoms, the diagnosis of serotonin toxicity according to Sternbach's criteria was determined to be unlikely.
CONCLUSIONS: In this small sample of patients treated with procarbazine plus an antidepressant (most typically SSRIs), there were no reports of serotonin toxicity, nor did any patients demonstrate symptoms consistent with serotonin toxicity. The authors urge clinicians to ensure depression is adequately managed in cancer patients who are undergoing procarbazine therapy, starting with typical first-line antidepressant agents.
Pizer B, Salehzadeh A, Brodbelt A, Mallucci C
Prolonged survival associated with the use of intraoperative carmustine (Gliadel) in a paediatric patient with recurrent grade III astrocytoma.
Br J Neurosurg. 2013; 27(4):516-8 [PubMed] Related Publications
Prolonged survival associated with the use of intraoperative carmustine (Gliadel) in a paediatric patient with recurrent grade III astrocytoma.
Br J Neurosurg. 2013; 27(4):516-8 [PubMed] Related Publications
A 15-year-old female presented with a middle cranial fossa anaplastic astrocytoma that was completely excised. She received local radiotherapy (54 Gy) and oral temozolomide. Five months after therapy, MRI showed local relapse. She underwent resection of the tumour with implantation of seven carmustine-impregnated wafers (Gliadel). She then received six cycles of procarbazine and lomustine therapy. Three years later, she is well and disease free. This case supports the further investigation of Gliadel in children and young people with relapsed high-grade glioma, particularly in the setting of a second complete resection.
Shibui S, Narita Y, Mizusawa J, et al.
Randomized trial of chemoradiotherapy and adjuvant chemotherapy with nimustine (ACNU) versus nimustine plus procarbazine for newly diagnosed anaplastic astrocytoma and glioblastoma (JCOG0305).
Cancer Chemother Pharmacol. 2013; 71(2):511-21 [PubMed] Related Publications
Randomized trial of chemoradiotherapy and adjuvant chemotherapy with nimustine (ACNU) versus nimustine plus procarbazine for newly diagnosed anaplastic astrocytoma and glioblastoma (JCOG0305).
Cancer Chemother Pharmacol. 2013; 71(2):511-21 [PubMed] Related Publications
PURPOSE: Glioblastoma (GBM) is one of the worst cancers in terms of prognosis. Standard therapy consists of resection with concomitant chemoradiotherapy. Resistance to nimustine hydrochloride (ACNU), an alkylating agent, has been linked to methylguanine DNA methyltransferase (MGMT). Daily administration of procarbazine (PCZ) has been reported to decrease MGMT activity. This study investigated the efficacy of ACNU + PCZ compared to ACNU alone for GBM and anaplastic astrocytoma (AA).
METHODS: Patients (20-69 years) who had newly diagnosed AA and GBM were randomly assigned to receive radiotherapy with ACNU alone or with ACNU + PCZ. The primary endpoint was overall survival (OS). This was designed as a phase II/III trial with a total sample size of 310 patients and was registered as UMIN-CTR C000000108.
RESULTS: After 111 patients from 19 centers in Japan were enrolled, this study was terminated early because temozolomide was newly approved in Japan. The median OS and median progression-free survival (PFS) with ACNU alone (n = 55) or ACNU + PCZ (n = 56) in the intention-to-treat population were 27.4 and 22.4 months (p = 0.75), and 8.6 and 6.9 months, respectively. The median OS and median PFS of the GBM subgroup treated with ACNU alone (n = 40) or ACNU + PCZ (n = 41) were 19.0 and 19.5 months, and 6.2 and 6.3 months, respectively. Grade 3/4 hematologic adverse events occurred in more than 40 % of patients in both arms, and 27 % of patients discontinued treatment because of adverse events.
CONCLUSIONS: The addition of PCZ to ACNU was not beneficial, in comparison with ACNU alone, for patients with newly diagnosed AA and GBM.
METHODS: Patients (20-69 years) who had newly diagnosed AA and GBM were randomly assigned to receive radiotherapy with ACNU alone or with ACNU + PCZ. The primary endpoint was overall survival (OS). This was designed as a phase II/III trial with a total sample size of 310 patients and was registered as UMIN-CTR C000000108.
RESULTS: After 111 patients from 19 centers in Japan were enrolled, this study was terminated early because temozolomide was newly approved in Japan. The median OS and median progression-free survival (PFS) with ACNU alone (n = 55) or ACNU + PCZ (n = 56) in the intention-to-treat population were 27.4 and 22.4 months (p = 0.75), and 8.6 and 6.9 months, respectively. The median OS and median PFS of the GBM subgroup treated with ACNU alone (n = 40) or ACNU + PCZ (n = 41) were 19.0 and 19.5 months, and 6.2 and 6.3 months, respectively. Grade 3/4 hematologic adverse events occurred in more than 40 % of patients in both arms, and 27 % of patients discontinued treatment because of adverse events.
CONCLUSIONS: The addition of PCZ to ACNU was not beneficial, in comparison with ACNU alone, for patients with newly diagnosed AA and GBM.
Coleman M, Ruan G, Elstrom RL, et al.
Metronomic therapy for refractory/relapsed lymphoma: the PEP-C low-dose oral combination chemotherapy regimen.
Hematology. 2012; 17 Suppl 1:S90-2 [PubMed] Related Publications
Metronomic therapy for refractory/relapsed lymphoma: the PEP-C low-dose oral combination chemotherapy regimen.
Hematology. 2012; 17 Suppl 1:S90-2 [PubMed] Related Publications
BACKGROUND: Metronomic therapy is the application of continuous, low dose chemotherapy. The doses of chemotherapy are usually not sufficient to destroy neoplastic cells, but impact the milieu, particularly angiogenesis.
OBJECTIVE: To determine if the oral PEP-C regimen, consisting of prednisone 20 mgm, etoposide 50 mgm, procarbazine 50 mgm, and cyclophosphamide 50 mgm given in either a daily, alternate day, or fractionated basis, is effective in a variety of lymphomas.
METHODS: One hundred twenty two patients were studied although the majority had low grade or mantle cell lymphoma. All had received at least two or more prior therapies.
RESULTS: Overall, 75% achieved an objective response (OR) with 38% complete responses (CRs) or CRs unconfirmed, and 37% partial responses. ORs were achieved in mantle cell (85%), follicular (88%), marginal zone (71%), and small lymphocytic (67%) lymphomas. Chemosensitive disease was more responsive. Toxicity was minimal.
CONCLUSION: The PEP-C regimen is an easily administered highly effective treatment for heavily pretreated mantle cell and low grade lymphomas.
OBJECTIVE: To determine if the oral PEP-C regimen, consisting of prednisone 20 mgm, etoposide 50 mgm, procarbazine 50 mgm, and cyclophosphamide 50 mgm given in either a daily, alternate day, or fractionated basis, is effective in a variety of lymphomas.
METHODS: One hundred twenty two patients were studied although the majority had low grade or mantle cell lymphoma. All had received at least two or more prior therapies.
RESULTS: Overall, 75% achieved an objective response (OR) with 38% complete responses (CRs) or CRs unconfirmed, and 37% partial responses. ORs were achieved in mantle cell (85%), follicular (88%), marginal zone (71%), and small lymphocytic (67%) lymphomas. Chemosensitive disease was more responsive. Toxicity was minimal.
CONCLUSION: The PEP-C regimen is an easily administered highly effective treatment for heavily pretreated mantle cell and low grade lymphomas.
Iwadate Y, Matsutani T, Shinozaki N, Saeki N
Anaplastic oligodendroglial tumors harboring 1p/19q deletion can be successfully treated without radiotherapy.
Anticancer Res. 2011; 31(12):4475-9 [PubMed] Related Publications
Anaplastic oligodendroglial tumors harboring 1p/19q deletion can be successfully treated without radiotherapy.
Anticancer Res. 2011; 31(12):4475-9 [PubMed] Related Publications
Although anaplastic oligodendroglial tumors are known to be chemosensitive, patients under this diagnosis have been traditionally treated with radiotherapy. To avoid possible neurotoxicity, we prospectively treated patients with anaplastic oligodendroglial tumors harboring 1p/19q deletion, with exclusive procarbazine, ACNU, and vincristine chemotherapy without radiotherapy. Twenty-five patients were enrolled in the study (12 with 1p/19q co-deletion, 2 with 1p mono-deletion, 2 with 19q mono-deletion, and 9 without 1p/19q deletion). The median progression-free survival (PFS) was 50 months for all the patients, and those with tumors harboring 1p/19q deletion were progression free for a significantly longer period than those without the deletion (p=0.0391). The median overall survival (OS) time was not reached in both patient groups with and without 1p/19q deletion (p=0.230), and the 5-year OS rate was 62.2% for all patients. The excellent treatment results warrant a large-scale clinical study to confirm the efficacy of upfront chemotherapy omitting radiotherapy as initial therapy for anaplastic oligodendroglial tumors with 1p/19q deletion.
Ruiz J, Case D, Enevold G, et al.
A phase II trial of thalidomide and procarbazine in adult patients with recurrent or progressive malignant gliomas.
J Neurooncol. 2012; 106(3):611-7 [PubMed] Free Access to Full Article Related Publications
A phase II trial of thalidomide and procarbazine in adult patients with recurrent or progressive malignant gliomas.
J Neurooncol. 2012; 106(3):611-7 [PubMed] Free Access to Full Article Related Publications
Thalidomide and procarbazine have demonstrated single agent activity against malignant gliomas (MG). We evaluated the combination of thalidomide and procarbazine with a single arm phase II trial in adults with recurrent or progressive MG. Procarbazine was given at a dose of 250 mg/m(2)/d × 5day q 28 days. Thalidomide was administered at a dose of 200 mg/day continuously. Intrapatient dose escalation of thalidomide was attempted (increase by 100 mg/day weekly as tolerated) to a maximum of 800 mg/day. The primary outcome was tumor response, assessed by MRI and CT. Secondary outcomes were progression free survival (PFS), overall survival (OS) and toxicity. In addition, quality of life questionnaires were performed at baseline and prior to each odd cycle in all treated patients. Eighteen patients (median age of 50) were accrued and received a total of 36 cycles (median 2) of therapy. The median maximum thalidomide dose achieved was 400 mg (range 0-800). No complete or partial responses were seen. One patient (6%) experienced stable disease, fourteen (78%) progressed as best response and three (17%) were not evaluable for response. Median time to progression was 2.1 months (95% CI, 1.5-2.5). Seventeen patients have died (one patient lost to follow-up after progression); median survival from enrollment was 7.6 months (95% CI, 3.5-9.4). Grade 3/4 drug related toxicity was minimal. Quality of life diminished over time. The combination of thalidomide and procarbazine demonstrated no efficacy in this trial.
Sung KH, Lee EH, Kim YZ
Factors influencing the response to high dose methotrexate-based vincristine and procarbazine combination chemotherapy for primary central nervous system lymphoma.
J Korean Med Sci. 2011; 26(4):551-60 [PubMed] Free Access to Full Article Related Publications
Factors influencing the response to high dose methotrexate-based vincristine and procarbazine combination chemotherapy for primary central nervous system lymphoma.
J Korean Med Sci. 2011; 26(4):551-60 [PubMed] Free Access to Full Article Related Publications
The authors investigated objective response rate to high dose methotrexate (HDMTX)-based combination chemotherapy in primary central nervous system lymphoma (PCNSL), and sought to identify factors that influence response to HDMTX-based combination therapy. Prospective observational analysis was performed on 52 PCNSL patients. All patients received HDMTX (3.5 g/m(2)) and vincristine (1.4 mg/m(2)/day) for one day during weeks 1, 3, 5, 7, and 9, and procarbazine (100 mg/m(2)/day) for one week during weeks 1, 5, and 9. Forty-one patients (78.8%) achieved complete or partial remission. Higher objective response rates were observed for patients with: 1) age < 60 yr; 2) Eastern Cooperative Oncology Group (ECOG) performance score of < 2; 3) low risk status as defined by the International Extranodal Lymphoma Study Group; 4) p53 positivity; 5) XBP-1 negativity; 6) MUM-1 negativity; and 7) homogenous gadolinium enhancement in MR images. Multivariate analysis showed that ECOG performance score of < 2, low risk, negativity for XBP-1, homogenous gadolinium enhancement by MRI, and response to chemotherapy were associated with longer overall survival. In particular, it is interesting to note that patients with a PCNSL that is homogeneously enhanced by gadolinium have a higher objective response rate, and a longer progression-free survival and overall survival.
Fesler MJ, Becker-Koepke S, Di Bisceglie AM, Petruska PJ
Procarbazine-induced hepatotoxicity: case report and review of the literature.
Pharmacotherapy. 2010; 30(5):540 [PubMed] Related Publications
Procarbazine-induced hepatotoxicity: case report and review of the literature.
Pharmacotherapy. 2010; 30(5):540 [PubMed] Related Publications
Procarbazine hydrochloride is an oral alkylating agent primarily used as a component of chemotherapy regimens for Hodgkin's lymphoma, as well as in regimens for primary central nervous system lymphoma and high-grade gliomas. Although the prescribing information for procarbazine lists hepatic dysfunction as a potential adverse reaction, we found only one published report with a probable link between procarbazine and liver injury. We describe a 65-year-old man who developed liver injury due to procarbazine during salvage chemotherapy for non-Hodgkin's lymphoma. The patient had no preexisting liver disease, his lymphoma was without hepatic involvement, and no liver injury developed after initial chemotherapy with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone). Due to relapse of his non-Hodgkin's lymphoma, salvage chemotherapy with C-MOPP-R (cyclophosphamide, vincristine, procarbazine, prednisone, and rituximab) was administered, and the patient developed fever and aminotransferase level elevation during the second cycle. After discontinuation of all drug therapy, exclusion of other potential etiologies, and resolution of hepatic injury, the patient was rechallenged with procarbazine and again experienced fever with aminotransferase level elevation. His aminotransferase levels promptly returned to normal after discontinuation of procarbazine, and he experienced no further evidence of liver disease. Use of validated scoring systems of drug-induced liver injury indicated a definitive association between the patient's hepatic injury and procarbazine. Based on our experience with this patient, periodic assessment of hepatic function, as suggested in the package insert, is recommended in patients receiving procarbazine.
Al-Tonbary Y, Sarhan MM, El-Ashry RA, et al.
Comparative study of two mechlorethamine, vincristine, procarbazine, and prednisone derived chemotherapeutic protocols for the management of pediatric Hodgkin lymphoma (HL): single-center 5-year experience.
Leuk Lymphoma. 2010; 51(4):656-63 [PubMed] Related Publications
Comparative study of two mechlorethamine, vincristine, procarbazine, and prednisone derived chemotherapeutic protocols for the management of pediatric Hodgkin lymphoma (HL): single-center 5-year experience.
Leuk Lymphoma. 2010; 51(4):656-63 [PubMed] Related Publications
We aimed for the comparison of two protocols (OAP and COMP) as chemotherapy treatment in children with Hodgkin lymphoma (HL). A total of 119 children newly diagnosed with HD were divided to receive either the anthracycline-based OAP protocol or the alkylating-agent-based COMP protocol. Sixty patients received the OAP protocol and 59 patients received the COMP protocol. Complete response was achieved for 81.4% of patients treated with the COMP protocol versus 53.3% for those who received the OAP treatment. Toxic hepatitis or liver cell failure was recorded in 5% of patients treated with the COMP protocol. Complications were more frequent in those treated with the OAP protocol, as 6.8% developed heart failure and 20% showed toxic hepatitis or liver cell failure. The relapse rate was almost equal in both treatment arms. Patients treated with the COMP protocol achieved a better response and less toxicity but with similar survival to those given the OAP protocol.
Illerhaus G, Marks R, Müller F, et al.
High-dose methotrexate combined with procarbazine and CCNU for primary CNS lymphoma in the elderly: results of a prospective pilot and phase II study.
Ann Oncol. 2009; 20(2):319-25 [PubMed] Related Publications
High-dose methotrexate combined with procarbazine and CCNU for primary CNS lymphoma in the elderly: results of a prospective pilot and phase II study.
Ann Oncol. 2009; 20(2):319-25 [PubMed] Related Publications
BACKGROUND: To improve survival of elderly patients with primary central nervous system lymphoma (PCNSL), we conducted a phase II study with high-dose methotrexate (MTX) combined with procarbazine and CCNU. To reduce neurotoxicity, whole-brain irradiation was reserved for patients not responding to chemotherapy.
PATIENTS AND METHODS: High-dose MTX was applied on days 1, 15, and 30, procarbazine on days 1-10, and CCNU on day 1. Study treatment comprised up to three 45-day cycles. There was no lower limit of Karnofsky performance status (KPS).
RESULTS: Thirty patients with PCNSL (n = 29) or primary ocular lymphoma (n = 1) were included (median age 70 years, range 57-79 years). The median initial KPS was 60% (range 30%-90%). Best documented response in 27 assessable patients were 12 of 27 (44.4%) complete remissions, 7 of 27 (25.9%) partial remissions, and 8 of 27 (29.6%) disease progressions. Two patients died of probable treatment-related causes. With a median follow-up of 78 months (range 34-105), the 5-year overall survival is 33%. Eight of 30 patients (26.7%) are currently alive and well, six without signs of leukoencephalopathy.
CONCLUSION: The combination of high-dose MTX with procarbazine and CCNU is feasible and effective and results in a low rate of leukoencephalopathy. Comorbidity and toxicity remain of concern when treating PCNSL in elderly patients.
PATIENTS AND METHODS: High-dose MTX was applied on days 1, 15, and 30, procarbazine on days 1-10, and CCNU on day 1. Study treatment comprised up to three 45-day cycles. There was no lower limit of Karnofsky performance status (KPS).
RESULTS: Thirty patients with PCNSL (n = 29) or primary ocular lymphoma (n = 1) were included (median age 70 years, range 57-79 years). The median initial KPS was 60% (range 30%-90%). Best documented response in 27 assessable patients were 12 of 27 (44.4%) complete remissions, 7 of 27 (25.9%) partial remissions, and 8 of 27 (29.6%) disease progressions. Two patients died of probable treatment-related causes. With a median follow-up of 78 months (range 34-105), the 5-year overall survival is 33%. Eight of 30 patients (26.7%) are currently alive and well, six without signs of leukoencephalopathy.
CONCLUSION: The combination of high-dose MTX with procarbazine and CCNU is feasible and effective and results in a low rate of leukoencephalopathy. Comorbidity and toxicity remain of concern when treating PCNSL in elderly patients.
Huang F, Kavan P, Guiot MC, et al.
When temozolomide alone fails: adding procarbazine in salvage therapy of glioma.
Can J Neurol Sci. 2008; 35(2):192-7 [PubMed] Related Publications
When temozolomide alone fails: adding procarbazine in salvage therapy of glioma.
Can J Neurol Sci. 2008; 35(2):192-7 [PubMed] Related Publications
BACKGROUND: Since temozolomide (TMZ) entry into routine practice in the first-line management of glial tumors, post-TMZ recurrences present a growing challenge. Without standard chemotherapy for TMZ failure, care in such palliative settings requires consideration not only of efficacy but of toxicity and convenience.
METHODS: At our institution, a combination regimen has been used: oral alkylating agents procarbazine (PCB) (100-150 mg/m2/day) and TMZ (150-200 mg/m2/day) administered on days 1-5 of a 28-day cycle. This treatment has been initiated upon radiological and/or clinical disease progression, and continued until evidence of further progression or toxicity. We retrospectively reviewed our experence with this regimen.
RESULTS: Since November 2004, 17 patients (median age 53) were treated for histologically confirmed glioma (glioblastoma multiforme (GBM), N = 12; Grade 3 glioma, N = 3; Grade 2 glioma, N = 2) after a median of 2 recurrences. TMZ was previously given either as adjuvant therapy (post-chemoradiotherapy maintenance in 8 of 13 cases) or as salvage monotherapy (4 cases). Of 16 evaluable cases, 14 (13 high grade tumors) showed O-6-methylguanine-DNA methyltransferase (MGMT) promoter methylation. Two patients achieved partial response and one had complete response by RECIST criteria. Disease progressed after a median of 4 cycles (range 1 to 11+), with an actuarial progression-free survival of 42% after 6 cycles. Grade 3/4 toxicity was rare, and no dose reductions were needed. One patient discontinued treatment due to procarbazine hypersensitivity.
CONCLUSION: Combination PCB-TMZ is well-tolerated, with modest activity in TMZ-exposed glioma.
METHODS: At our institution, a combination regimen has been used: oral alkylating agents procarbazine (PCB) (100-150 mg/m2/day) and TMZ (150-200 mg/m2/day) administered on days 1-5 of a 28-day cycle. This treatment has been initiated upon radiological and/or clinical disease progression, and continued until evidence of further progression or toxicity. We retrospectively reviewed our experence with this regimen.
RESULTS: Since November 2004, 17 patients (median age 53) were treated for histologically confirmed glioma (glioblastoma multiforme (GBM), N = 12; Grade 3 glioma, N = 3; Grade 2 glioma, N = 2) after a median of 2 recurrences. TMZ was previously given either as adjuvant therapy (post-chemoradiotherapy maintenance in 8 of 13 cases) or as salvage monotherapy (4 cases). Of 16 evaluable cases, 14 (13 high grade tumors) showed O-6-methylguanine-DNA methyltransferase (MGMT) promoter methylation. Two patients achieved partial response and one had complete response by RECIST criteria. Disease progressed after a median of 4 cycles (range 1 to 11+), with an actuarial progression-free survival of 42% after 6 cycles. Grade 3/4 toxicity was rare, and no dose reductions were needed. One patient discontinued treatment due to procarbazine hypersensitivity.
CONCLUSION: Combination PCB-TMZ is well-tolerated, with modest activity in TMZ-exposed glioma.
Goerne R, Bogdahn U, Hau P
Procarbazine--a traditional drug in the treatment of malignant gliomas.
Curr Med Chem. 2008; 15(14):1376-87 [PubMed] Related Publications
Procarbazine--a traditional drug in the treatment of malignant gliomas.
Curr Med Chem. 2008; 15(14):1376-87 [PubMed] Related Publications
The methylhydrazine derivative Procarbazine (PCZ) as monotherapy or in combination with CCNU and vincristine (PCV) was evaluated in a vast number of clinical trials and is still used in patients with high-grade and low-grade gliomas. The compound is an antineoplastic agent with multiple sites of action. It inhibits incorporation of small DNA precursors, as well as RNA and protein synthesis. PCZ can also directly damage DNA through an alkylation reaction. The drug is not cross-resistant with other mustard-type alkylating agents. As PCZ was in almost all trials used in a combination with CCNU and Vincristin, the efficacy can only be evaluated in the view of the PCV regimen. The published data suggest a role of PCV as a salvage regimen, especially in oligodendroglial tumors; however, well designed studies with high evidence are rare in all entities. This article summarizes the existing data with the goal to define the role of PCZ/PCV in modern neurooncology.
Grossman SA, Carson KA, Batchelor TT, et al.
The effect of enzyme-inducing antiseizure drugs on the pharmacokinetics and tolerability of procarbazine hydrochloride.
Clin Cancer Res. 2006; 12(17):5174-81 [PubMed] Related Publications
The effect of enzyme-inducing antiseizure drugs on the pharmacokinetics and tolerability of procarbazine hydrochloride.
Clin Cancer Res. 2006; 12(17):5174-81 [PubMed] Related Publications
PURPOSE: Procarbazine hydrochloride (PCB) is one of the few anticancer drugs with activity against high-grade gliomas. This study was conducted to determine if the maximum tolerated dose and pharmacokinetics of PCB are affected by the concurrent use of enzyme-inducing antiseizure drugs (EIASD).
EXPERIMENTAL DESIGN: Adults with recurrent high-grade glioma were divided into cohorts who were (+) and were not (-) taking EIASDs. PCB was given orally for 5 consecutive days each month. Six patients were evaluated at each dose level beginning with 200 mg/m2/d and escalated using the modified continual reassessment method. Toxicity and response were assessed. Pharmacokinetic studies were done with a new electrospray ionization mass spectrometry assay.
RESULTS: Forty-nine patients were evaluated. The maximum tolerated dose was 393 mg/m2/d for the +EIASD group and the highest dose evaluated in -EIASD patients was 334 mg/m2/d. Myelosuppression was the primary dose-limiting toxicity. Significant hepatic dysfunction occurred in three patients in the +EIASD cohort. Four partial responses (8%) and no complete responses were observed. PCB exhibited linear pharmacokinetics with no significant differences between the two cohorts. A marked increase in peak PCB levels was noted on day 5 relative to day 1, which was not attributable to drug accumulation.
CONCLUSIONS: This study suggests that (a) EIASD use does not significantly affect the pharmacokinetics of PCB; (b) changes in the peak plasma concentration of PCB, consistent with decreased apparent oral clearance due to autoinhibition of hepatic metabolism, occur with daily dosing; and (c) severe hepatic dysfunction may accompany this administration schedule.
EXPERIMENTAL DESIGN: Adults with recurrent high-grade glioma were divided into cohorts who were (+) and were not (-) taking EIASDs. PCB was given orally for 5 consecutive days each month. Six patients were evaluated at each dose level beginning with 200 mg/m2/d and escalated using the modified continual reassessment method. Toxicity and response were assessed. Pharmacokinetic studies were done with a new electrospray ionization mass spectrometry assay.
RESULTS: Forty-nine patients were evaluated. The maximum tolerated dose was 393 mg/m2/d for the +EIASD group and the highest dose evaluated in -EIASD patients was 334 mg/m2/d. Myelosuppression was the primary dose-limiting toxicity. Significant hepatic dysfunction occurred in three patients in the +EIASD cohort. Four partial responses (8%) and no complete responses were observed. PCB exhibited linear pharmacokinetics with no significant differences between the two cohorts. A marked increase in peak PCB levels was noted on day 5 relative to day 1, which was not attributable to drug accumulation.
CONCLUSIONS: This study suggests that (a) EIASD use does not significantly affect the pharmacokinetics of PCB; (b) changes in the peak plasma concentration of PCB, consistent with decreased apparent oral clearance due to autoinhibition of hepatic metabolism, occur with daily dosing; and (c) severe hepatic dysfunction may accompany this administration schedule.
Chaar BT, Salem P, Petruska PJ
Procarbazine for non-Hodgkin's lymphoma.
Leuk Lymphoma. 2006; 47(4):637-40 [PubMed] Related Publications
Procarbazine for non-Hodgkin's lymphoma.
Leuk Lymphoma. 2006; 47(4):637-40 [PubMed] Related Publications
Procarbazine hydrochloride is an oral alkylating agent with activity against lymphoma. It is most commonly used in the treatment of Hodgkin's disease. The use of procarbazine-containing chemotherapeutic regimens in non-Hodgkin's lymphoma fell out of favor with the advent of CHOP. We report two patients with relapsed and/or refractory follicular lymphoma that achieved a complete and durable remission with a prolonged course of daily procarbazine.
Cornetta K, Croop J, Dropcho E, et al.
A pilot study of dose-intensified procarbazine, CCNU, vincristine for poor prognosis brain tumors utilizing fibronectin-assisted, retroviral-mediated modification of CD34+ peripheral blood cells with O6-methylguanine DNA methyltransferase.
Cancer Gene Ther. 2006; 13(9):886-95 [PubMed] Related Publications
A pilot study of dose-intensified procarbazine, CCNU, vincristine for poor prognosis brain tumors utilizing fibronectin-assisted, retroviral-mediated modification of CD34+ peripheral blood cells with O6-methylguanine DNA methyltransferase.
Cancer Gene Ther. 2006; 13(9):886-95 [PubMed] Related Publications
Administration of chemotherapy is often limited by myelosuppression. Expression of drug-resistance genes in hematopoietic cells has been proposed as a means to decrease the toxicity of cytotoxic agents. In this pilot study, we utilized a retroviral vector expressing methylguanine DNA methyltransferase (MGMT) to transduce hematopoietic progenitors, which were subsequently used in the setting of alkylator therapy (procarbazine, CCNU, vincristine (PCV)) for poor prognosis brain tumors. Granulocyte colony-stimulating factor (G-CSF)-mobilized peripheral blood progenitor cells were collected by apheresis and enriched for CD34+ expression. Nine subjects were infused with CD34+-enriched cells treated in a transduction procedure involving a 4-day exposure to cytokines with vector exposure on days 3 and 4. No major adverse event was related to the gene therapy procedure. Importantly, the engraftment kinetics of the treated product was similar to unmanipulated peripheral blood stem cells, suggesting that the ex vivo manipulation did not significantly reduce engrafting progenitor cell function. Gene-transduced cells were detected in all subjects. Although the level and duration was limited, patients receiving cells transduced using fibronectin 'preloaded' with virus supernatant appeared to show improved in vivo marking frequency. These findings demonstrate the feasibility and safety of utilizing MGMT-transduced CD34+ peripheral blood progenitor cells in the setting of chemotherapy.
Di Renzo N, Brugiatelli M, Montanini A, et al.
Vinorelbine, gemcitabine, procarbazine and prednisone (ViGePP) as salvage therapy in relapsed or refractory aggressive non-Hodgkin's lymphoma (NHL): results of a phase II study conducted by the Gruppo Italiano per lo Studio dei Linfomi.
Leuk Lymphoma. 2006; 47(3):473-9 [PubMed] Related Publications
Vinorelbine, gemcitabine, procarbazine and prednisone (ViGePP) as salvage therapy in relapsed or refractory aggressive non-Hodgkin's lymphoma (NHL): results of a phase II study conducted by the Gruppo Italiano per lo Studio dei Linfomi.
Leuk Lymphoma. 2006; 47(3):473-9 [PubMed] Related Publications
Patients with aggressive NHL who fail initial treatment or subsequently relapse have a very poor outcome and less than 20-25% achieve a prolonged disease-free interval with salvage therapies. To improve the outcome of patients with refractory aggressive NHL not suitable for High Dose Therapy (HDT) and Autologous Stem Cell Transplant (ASCT), the efficacy of a combination of gemcitabine, vinorelbine, procarbazine and prednisone (ViGePP) were tested. Between November 1999 and September 2002, 69 patients with relapsed or refractory aggressive NHL were treated with ViGePP regimen, every 4 weeks up to six courses. At the end of planned chemotherapy patients could receive additional radiotherapy on residual masses or on sites of previously bulky disease. Sixty-six patients were available for evaluation of study end-points. Thirty patients were refractory to therapy and 36 patients had relapsed after remission obtained with previous therapy. At the end of therapy, complete remission (CR) rate was 23%, 3-year relapse free survival rate was 40% and 3-year overall survival rate was 25% for the whole series (29% and 20% for relapsed and refractory patients, respectively). Patients achieving CR with ViGePP had a significantly better survival as compared with the remaining ones (p = 0.0003). ViGePP as used in the present setting has demonstrated a promising activity, comparable to other conventional dose regimens. Although CR was achieved only in a minority of patients, this was durable in a significant proportion of them. This regimen should be tested in less heavily pre-treated patients and probably in combination with new active agents such Rituximab. Further developments of this combination are warranted.
Preiss R, Baumann F, Regenthal R, Matthias M
Plasma kinetics of procarbazine and azo-procarbazine in humans.
Anticancer Drugs. 2006; 17(1):75-80 [PubMed] Related Publications
Plasma kinetics of procarbazine and azo-procarbazine in humans.
Anticancer Drugs. 2006; 17(1):75-80 [PubMed] Related Publications
The plasma kinetics of procarbazine (PCB) and its major metabolite azo-procarbazine (azo-PCB) were systematically investigated in humans for the first time. Eight therapy-refractory tumor patients with normal liver and renal function were given a single oral dose of 300 mg PCB hydrochloride as a drinking solution under fasting conditions. With the exception of the single i.v. administration of 10 mg ondansetron hydrochloride immediately before the administration of PCB, the patients were free of any co-medication 4 weeks before and during the study. PCB and azo-PCB were determined by a specially developed HPLC-UV method. PCB was absorbed very rapidly. Mean maximum plasma concentration was 12.5 min. A high elimination rate of PCB from plasma was found. The mean apparent oral systemic clearance and the plasma elimination half-life were estimated at 35.8 l/min and 9.2 min, respectively. Considerable amounts of azo-PCB are found in the plasma of the eight tumor patients. The mean Cmax and AUC ratios of azo-PCB/PCB were estimated at 5.5 and 45.2. Azo-PCB is formed very rapidly from PCB, but eliminated much more slowly from plasma than PCB. Considerable interindividual differences in the conversion rate of azo-PCB to its further metabolites were observed which should have consequences for the individual tumor therapeutic efficiency of PCB. No toxic side-effects or symptoms such as nausea or vomiting were observed during the entire study.
Bang SM, Cheong JW, Yang WI, Hahn JS
An unusual case of spontaneous remission of Hodgkin's disease after a single cycle of COPP-ABV chemotherapy followed by infectious complications.
Yonsei Med J. 2005; 46(3):425-30 [PubMed] Free Access to Full Article Related Publications
An unusual case of spontaneous remission of Hodgkin's disease after a single cycle of COPP-ABV chemotherapy followed by infectious complications.
Yonsei Med J. 2005; 46(3):425-30 [PubMed] Free Access to Full Article Related Publications
Advanced Hodgkin's disease is usually treated with six or more cycles of combination chemotherapy. Spontaneous regression of the cancer is very rarely reported in patients with Hodgkin's disease. We present an unusual case of a patient with Hodgkin's disease who experienced complete remission with a single cycle of chemotherapy, followed by pneumonia. The case was a 36-year-old man diagnosed with stage IVB mixed cellularity Hodgkin's disease in November 2000. After treatment with one cycle of COPP-ABV (cyclophosphamide, vincristine, procarbazine, prednisone, doxorubicin, bleomycin, and vinblastine) chemotherapy without bleomycin, the patient developed interstitial pneumonia and was cared in the intensive care unit (ICU) for two months. Follow-up chest computerized tomography (CT), performed during the course of ICU care, revealed markedly improved mediastinal lymphomatous lesions. Furthermore, follow-up whole body CT and 18-fluorodeoxyglucose positron emission tomography showed complete disappearance of the lymphomatous lesions. Four years later, the patient is well and without relapse. This report is followed by a short review of the literature on spontaneous regression of Hodgkin's disease. To the best of our knowledge, this is the first case report of spontaneous remission of Hodgkin's disease in Korea.
Macdonald DR, Kiebert G, Prados M, et al.
Benefit of temozolomide compared to procarbazine in treatment of glioblastoma multiforme at first relapse: effect on neurological functioning, performance status, and health related quality of life.
Cancer Invest. 2005; 23(2):138-44 [PubMed] Related Publications
Benefit of temozolomide compared to procarbazine in treatment of glioblastoma multiforme at first relapse: effect on neurological functioning, performance status, and health related quality of life.
Cancer Invest. 2005; 23(2):138-44 [PubMed] Related Publications
Since high-grade malignant gliomas can seldom be treated curatively, the main aim of first line therapy is to improve progression free survival (PFS), to reduce morbidity, and to preserve, if not restore neurological functions and the capacity to perform daily activities. Focusing on a single clinical efficacy parameter in clinical trials may provide a potentially biased result, as for patients the overall result of treatment entails a more complex picture of weighing and balancing gains and losses on different outcome measures. In this paper we address different clinical outcomes measures separately and we illustrate the value of multiple outcome measures using the results of a recent clinical trial comparing temozolomide with procarbazine in the treatment of Glioblastoma Multiforme. Compared with procarbazine, temozolomide not only prolonged PFS, but also maintained neurological functioning and performance status for a longer period of time, and also improved health-related quality of life (HRQL). All these statistically significant outcomes demonstrate a remarkable consistency. In addition, temozolomide showed a trend of extending overall survival over procarbazine.
Tang BN, Sadeghi N, Branle F, et al.
Semi-quantification of methionine uptake and flair signal for the evaluation of chemotherapy in low-grade oligodendroglioma.
J Neurooncol. 2005; 71(2):161-8 [PubMed] Related Publications
Semi-quantification of methionine uptake and flair signal for the evaluation of chemotherapy in low-grade oligodendroglioma.
J Neurooncol. 2005; 71(2):161-8 [PubMed] Related Publications
UNLABELLED: 11C-Methionine (MET) is a useful positron emission tomography (PET) tracer for the evaluation of low-grade gliomas. Among these tumors, a high percentage of low-grade oligodendrogliomas (ODG) are sensitive to chemotherapy with procarbazine, CCNU, and vincristine (PCV). We aimed at: (1) objectively assessing ODG response to PCV by a metabolic index (the Activity Volume Index or AVI) generated from an automated semi-quantification of PET with MET (PET-MET); (2) comparing AVI and quantitative magnetic resonance imaging (MRI) measurements of response to PCV.
METHODS: seven patients with ODG were followed for a period of 19.9+/-6.6 months after the completion of PCV chemotherapy. Regions of interest (ROI) were generated by covering all voxels with count values above a threshold level set at 120% of the mean cerebellar activity. On each slice, ROI volume and mean count values were calculated. AVI was calculated as the sum over all ROI of tumor volumex(tumor mean count/cerebellum count). Tumor volume measurements on MRI, were based on signal abnormalities visually detected on fluid-attenuated inversion recovery (FLAIR) sequences.
RESULTS: PCV therapy was associated with a drastic decrease in AVI (mean+/-SD, cm3): AVI post-PCV=0.80+/-1.45 vs. AVI prior PCV=12.94+/-11.46 (P=0.03). Likewise, we observed a decrease in tumor volume estimated from the FLAIR signal (31.37+/-11.99 post-PCV vs. 67.95+/-39.96 prior PCV, P=0.03) although AVI decrease after PCV was significantly more pronounced (P=0.015).
CONCLUSION: This study, based on limited number of patients and follow-up period indicates that AVI may be a sensitive and observer-independent method applicable to the assessment of ODG responsiveness to PCV treatment and may offer a major added value to both clinical assessment and MRI evaluation of chemotherapeutic outcomes.
METHODS: seven patients with ODG were followed for a period of 19.9+/-6.6 months after the completion of PCV chemotherapy. Regions of interest (ROI) were generated by covering all voxels with count values above a threshold level set at 120% of the mean cerebellar activity. On each slice, ROI volume and mean count values were calculated. AVI was calculated as the sum over all ROI of tumor volumex(tumor mean count/cerebellum count). Tumor volume measurements on MRI, were based on signal abnormalities visually detected on fluid-attenuated inversion recovery (FLAIR) sequences.
RESULTS: PCV therapy was associated with a drastic decrease in AVI (mean+/-SD, cm3): AVI post-PCV=0.80+/-1.45 vs. AVI prior PCV=12.94+/-11.46 (P=0.03). Likewise, we observed a decrease in tumor volume estimated from the FLAIR signal (31.37+/-11.99 post-PCV vs. 67.95+/-39.96 prior PCV, P=0.03) although AVI decrease after PCV was significantly more pronounced (P=0.015).
CONCLUSION: This study, based on limited number of patients and follow-up period indicates that AVI may be a sensitive and observer-independent method applicable to the assessment of ODG responsiveness to PCV treatment and may offer a major added value to both clinical assessment and MRI evaluation of chemotherapeutic outcomes.
Renschler MF
The emerging role of reactive oxygen species in cancer therapy.
Eur J Cancer. 2004; 40(13):1934-40 [PubMed] Related Publications
The emerging role of reactive oxygen species in cancer therapy.
Eur J Cancer. 2004; 40(13):1934-40 [PubMed] Related Publications
The generation of reactive oxygen species (ROS) can be exploited therapeutically in the treatment of cancer. One of the first drugs to be developed that generates ROS was procarbazine. It is oxidised readily in an oxic environment to its azo derivative, generating ROS. Forty years ago, Berneis reported a synergistic effect in DNA degradation when procarbazine was combined with radiation; this was confirmed in preclinical in vivo modes. Early uncontrolled clinical trials suggested an enhancement of the radiation effect with procarbazine, but two randomised trials failed to confirm this. The role of ROS in cancer treatments and in the development of resistance to chemotherapy is now better understood. The possibility of exploiting ROS as a cancer treatment is re-emerging as a promising therapeutic option with the development of agents such as buthionine sulfoximine and motexafin gadolinium.
Massoud M, Armand JP, Ribrag V
Procarbazine in haematology: an old drug with a new life?
Eur J Cancer. 2004; 40(13):1924-7 [PubMed] Related Publications
Procarbazine in haematology: an old drug with a new life?
Eur J Cancer. 2004; 40(13):1924-7 [PubMed] Related Publications
Procarbazine (PCB) was developed in the 1960s and was rapidly recognised as an active agent in lymphoid malignancies. PCB was one of the four drugs combined in mechlorethamine, vincristine, PCB, prednisolone (MOPP), one of the first combination chemotherapy regimens to show that advanced-stage disease could be cured in humans. During the last few decades, comprehensive studies have clarified cellular pathways involved in the modes of action of PCB and its drug resistance mechanisms. However, late toxicities, especially secondary leukaemias and sterility, led to its withdrawal from combination regimens used to treat Hodgkin's lymphomas (HLs). PCB was recently reintroduced in dose-intensified regimens and yielded impressive results. These new regimens (bleomycin, etoposide, doxorubicin, vincristine, PCB, and prednisone (BEACOPP) or escalated BEACOPP) are now being investigated versus the classic ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) or ABVD-like combination chemotherapy regimens in the treatment of HLs.
Bordallo MA, Guimarães MM, Pessoa CH, et al.
Decreased serum inhibin B/FSH ratio as a marker of Sertoli cell function in male survivors after chemotherapy in childhood and adolescence.
J Pediatr Endocrinol Metab. 2004; 17(6):879-87 [PubMed] Related Publications
Decreased serum inhibin B/FSH ratio as a marker of Sertoli cell function in male survivors after chemotherapy in childhood and adolescence.
J Pediatr Endocrinol Metab. 2004; 17(6):879-87 [PubMed] Related Publications
OBJECTIVE: Inhibin B produced by Sertoli cells may be an important marker of seminiferous tubule function in patients treated with chemotherapy (CT). The aim of this study was to evaluate the inhibin B/FSH ratio to detect male gonadal dysfunction in cancer survivors treated in childhood and adolescence.
PATIENTS: Twenty-one male patients (group A) treated with 6-10 courses of CT for Hodgkin's disease during childhood and adolescence were examined 3-11 years after the conclusion of treatment. Twenty healthy young men (18-23 years old) were used as controls (group B).
METHODS: Serum samples for the determination of inhibin B, follicle-stimulating hormone (FSH), luteinizing hormone (LH), testosterone (T), sex hormone-binding globulin (SHBG) and semen for analysis were collected.
RESULTS: The median testicular volume of patients of group A was lower than those of group B (p = 0.001) and a positive correlation was found between testicular size and sperm count (r = -0.5, p = 0.01). Semen analysis revealed azoospermia in 11 patients, severe oligospermia in four and normal sperm count in three. No significant difference was found in the median of T, LH, SHBG, inhibin B concentrations and T/LH ratio between the groups. Serum inhibin B was correlated with the serum FSH levels (r = -0.5, p = 0.02). Median FSH was significantly higher (p = 0.0001), and median inhibin B/FSH ratio was significantly lower in group A than in controls (p = 0.0002), but the inhibin B/FSH ratio was higher in the patients with normal sperm count than in those with oligospermia (p = 0.00004).
CONCLUSIONS: These results show that the cytotoxic effects of CT cause severe damage to the germinal epithelium with subtle effects on Sertoli cells. To assess Sertoli cell function in men with primary testicular damage after treatment with CT in childhood and adolescence, the inhibin B level needs to be interpreted in the context of the circulating FSH, especially when normal FSH levels are observed.
PATIENTS: Twenty-one male patients (group A) treated with 6-10 courses of CT for Hodgkin's disease during childhood and adolescence were examined 3-11 years after the conclusion of treatment. Twenty healthy young men (18-23 years old) were used as controls (group B).
METHODS: Serum samples for the determination of inhibin B, follicle-stimulating hormone (FSH), luteinizing hormone (LH), testosterone (T), sex hormone-binding globulin (SHBG) and semen for analysis were collected.
RESULTS: The median testicular volume of patients of group A was lower than those of group B (p = 0.001) and a positive correlation was found between testicular size and sperm count (r = -0.5, p = 0.01). Semen analysis revealed azoospermia in 11 patients, severe oligospermia in four and normal sperm count in three. No significant difference was found in the median of T, LH, SHBG, inhibin B concentrations and T/LH ratio between the groups. Serum inhibin B was correlated with the serum FSH levels (r = -0.5, p = 0.02). Median FSH was significantly higher (p = 0.0001), and median inhibin B/FSH ratio was significantly lower in group A than in controls (p = 0.0002), but the inhibin B/FSH ratio was higher in the patients with normal sperm count than in those with oligospermia (p = 0.00004).
CONCLUSIONS: These results show that the cytotoxic effects of CT cause severe damage to the germinal epithelium with subtle effects on Sertoli cells. To assess Sertoli cell function in men with primary testicular damage after treatment with CT in childhood and adolescence, the inhibin B level needs to be interpreted in the context of the circulating FSH, especially when normal FSH levels are observed.
Shibui S,
Randomized controlled trial on malignant brain tumors--activities of the Japan Clinical Oncology Group-Brain Tumor Study Group.
Neurol Med Chir (Tokyo). 2004; 44(4):220-1 [PubMed] Related Publications
Randomized controlled trial on malignant brain tumors--activities of the Japan Clinical Oncology Group-Brain Tumor Study Group.
Neurol Med Chir (Tokyo). 2004; 44(4):220-1 [PubMed] Related Publications
The Japan Clinical Oncology Group (JCOG)-Brain Tumor Study Group was organized with the support of the Health and Labour Sciences Research Grants of the Ministry of Health, Labour and Welfare. The group is now preparing a multi-institutional randomized controlled phase II/III study of chemoradiotherapy using ACNU versus procarbazine and ACNU for astrocytoma grades 3 and 4. The overall survival and response rates will be compared between the patients treated with ACNU and those treated with ACNU plus procarbazine. This study, under the surveillance of the JCOG, aims to set a standard protocol for treating patients with malignant glioma. Moreover, the study will establish a proper methodology for performing randomized studies in the field of neuro-oncology.
Hakvoort-Cammel FG, Buitendijk S, van den Heuvel-Eibrink M, Hählen K
Treatment of pediatric Hodgkin disease avoiding radiotherapy: excellent outcome with the Rotterdam-HD-84-protocol.
Pediatr Blood Cancer. 2004; 43(1):8-16 [PubMed] Related Publications
Treatment of pediatric Hodgkin disease avoiding radiotherapy: excellent outcome with the Rotterdam-HD-84-protocol.
Pediatr Blood Cancer. 2004; 43(1):8-16 [PubMed] Related Publications
BACKGROUND: To reduce radiotherapy (XRT) induced toxicity of treatment of children with Hodgkin disease (HD) while maintaining a high cure rate, we introduced a risk-adapted protocol consisting of chemotherapy (CT) alone in 1984.
PROCEDURE: The outcome of 46 children treated for HD from 1984 until 2000 according to the Rotterdam-HD-84-protocol was determined. Children with stage I-IIA disease (n = 23), were treated with six courses of epirubicin, bleomycin, vinblastine, and dacarbazine (EBVD). Children with stage IIB-IV disease (n = 23), were treated with three to five alternating cycles of EBVD and mechlorethamine, vincristine, procarbazine, and prednisone (MOPP).
RESULTS: At a median follow-up time of 8.6 years (range 2.6-18.3 years), the 10-year overall survival (OS) is 95% and the event-free survival (EFS) 91%. In 5/46 patients XRT was administered because of residual mediastinal mass. Four children relapsed, two of them died. Up until now only one patient developed hypothyroidism; no symptomatic cardiac or pulmonary dysfunction, no second malignancy has been diagnosed.
CONCLUSIONS: Risk-adapted treatment consisting of CT alone is highly efficacious for children with HD and toxicity is low. XRT was administered in only a small minority of children with HD. CT should be the first choice for HD in children and XRT should preferably be used for those with refractory or histologically proven residual disease or relapse.
PROCEDURE: The outcome of 46 children treated for HD from 1984 until 2000 according to the Rotterdam-HD-84-protocol was determined. Children with stage I-IIA disease (n = 23), were treated with six courses of epirubicin, bleomycin, vinblastine, and dacarbazine (EBVD). Children with stage IIB-IV disease (n = 23), were treated with three to five alternating cycles of EBVD and mechlorethamine, vincristine, procarbazine, and prednisone (MOPP).
RESULTS: At a median follow-up time of 8.6 years (range 2.6-18.3 years), the 10-year overall survival (OS) is 95% and the event-free survival (EFS) 91%. In 5/46 patients XRT was administered because of residual mediastinal mass. Four children relapsed, two of them died. Up until now only one patient developed hypothyroidism; no symptomatic cardiac or pulmonary dysfunction, no second malignancy has been diagnosed.
CONCLUSIONS: Risk-adapted treatment consisting of CT alone is highly efficacious for children with HD and toxicity is low. XRT was administered in only a small minority of children with HD. CT should be the first choice for HD in children and XRT should preferably be used for those with refractory or histologically proven residual disease or relapse.


 Cancer Screening and Early Detection
Cancer Screening and Early Detection