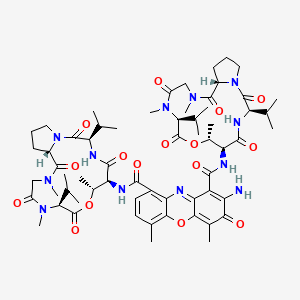
Dactinomycin
"A compound composed of a two CYCLIC PEPTIDES attached to a phenoxazine that is derived from STREPTOMYCES parvullus. It binds to DNA and inhibits RNA synthesis (transcription), with chain elongation more sensitive than initiation, termination, or release. As a result of impaired mRNA production, protein synthesis also declines after dactinomycin therapy. (From AMA Drug Evaluations Annual, 1993, p2015)" (MeSH 2013)
Found this page useful?
 Web Resources: Dactinomycin
Web Resources: Dactinomycin Latest Research Publications
Latest Research PublicationsWeb Resources: Dactinomycin (6 links)
Cancer Research UK
Macmillan Cancer Support
MedlinePlus.gov
NHS Evidence
PubChem - Substances
Irish Cancer Society
Latest Research Publications
This list of publications is regularly updated (Source: PubMed).
Song Y, Park IS, Kim J, Seo HR
Actinomycin D inhibits the expression of the cystine/glutamate transporter xCT via attenuation of CD133 synthesis in CD133
Chem Biol Interact. 2019; 309:108713 [PubMed] Related Publications
Actinomycin D inhibits the expression of the cystine/glutamate transporter xCT via attenuation of CD133 synthesis in CD133
Chem Biol Interact. 2019; 309:108713 [PubMed] Related Publications
Liver cancer is one of the most frequently occurring types of cancer with high mortality rate. Hepatocellular carcinoma (HCC) frequently metastasizes to lung, portal vein, and portal lymph nodes and most HCCs show strong resistance to conventional anticancer drugs. Cancer stem cells (CSCs) are considered to be responsible for resistance to therapies. Hence, recent advancements in the use of liver cancer stem cells (LCSCs) are rapidly gaining recognition as an efficient and organized means for developing antitumor agents. We aimed to use a non-target-based high-throughput screening (HTS) approach to specifically target α-fetoprotein (AFP)
Kang HL, Zhao Q, Yang SL, Duan W
Efficacy of Combination Therapy with Actinomycin D and Methotrexate in the Treatment of Low-Risk Gestational Trophoblastic Neoplasia.
Chemotherapy. 2019; 64(1):42-47 [PubMed] Related Publications
Efficacy of Combination Therapy with Actinomycin D and Methotrexate in the Treatment of Low-Risk Gestational Trophoblastic Neoplasia.
Chemotherapy. 2019; 64(1):42-47 [PubMed] Related Publications
OBJECTIVES: We aimed to identify an optimal regimen for low-risk gestational trophoblastic neoplasia (LR-GTN) providing reduction in dosage and toxicity/side effects, enhancement of therapeutic efficacy, and a shorter treatment duration.
METHODS: A total of 149 LR-GTN patients were enrolled in the affiliated Beijing Maternity Hospital of Capital Medical University from January 2014 to January 2017 and randomly divided into 3 groups with 50 cases in the methotrexate (MTX) group, 49 in actinomycin D (ACT-D) group, and 50 in ACT-D+MTX group. Follow-up recorded symptoms, physical and bimanual gynecological examinations, routine blood test, serum β-HCG level, liver and renal functions, electrolytes, electrocardiogram before each treatment course, and pelvic and abdominal B-mode ultrasound or pelvic/abdominal/chest computed tomography.
RESULTS: Serum complete remission (SCR) was 96.0, 87.8, and 83.7% for the ACT-D+MTX, ACT-D, and MTX groups, respectively, with SCR being highest in the ACT-D+MTX group, statistically higher than in the MTX group. Vomiting was the only side effect differing significantly by chemotherapy regimen, with a distinctly higher incidence in the ACT-D+MTX group compared with the MTX group (p = 0.028). The reduction rate of serum β-HCG in the ACT-D+MTX group was significantly greater than in the other 2 groups.
CONCLUSION: Combined ACT-D+MTX chemotherapy achieved overall better efficacy and showed less toxicity than ACT-D or MTX alone, and thus can be prioritized for the treatment of LR-GTN.
METHODS: A total of 149 LR-GTN patients were enrolled in the affiliated Beijing Maternity Hospital of Capital Medical University from January 2014 to January 2017 and randomly divided into 3 groups with 50 cases in the methotrexate (MTX) group, 49 in actinomycin D (ACT-D) group, and 50 in ACT-D+MTX group. Follow-up recorded symptoms, physical and bimanual gynecological examinations, routine blood test, serum β-HCG level, liver and renal functions, electrolytes, electrocardiogram before each treatment course, and pelvic and abdominal B-mode ultrasound or pelvic/abdominal/chest computed tomography.
RESULTS: Serum complete remission (SCR) was 96.0, 87.8, and 83.7% for the ACT-D+MTX, ACT-D, and MTX groups, respectively, with SCR being highest in the ACT-D+MTX group, statistically higher than in the MTX group. Vomiting was the only side effect differing significantly by chemotherapy regimen, with a distinctly higher incidence in the ACT-D+MTX group compared with the MTX group (p = 0.028). The reduction rate of serum β-HCG in the ACT-D+MTX group was significantly greater than in the other 2 groups.
CONCLUSION: Combined ACT-D+MTX chemotherapy achieved overall better efficacy and showed less toxicity than ACT-D or MTX alone, and thus can be prioritized for the treatment of LR-GTN.
Lamture G, Crooks PA, Borrelli MJ
Actinomycin-D and dimethylamino-parthenolide synergism in treating human pancreatic cancer cells.
Drug Dev Res. 2018; 79(6):287-294 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Actinomycin-D and dimethylamino-parthenolide synergism in treating human pancreatic cancer cells.
Drug Dev Res. 2018; 79(6):287-294 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Preclinical Research & Development Pancreatic cancer is the third leading cause of death in the US with a poor 5-year survival rate of 8.5%. A novel anti-cancer drug, dimethylamino parthenolide (DMAPT), is the water-soluble analog of the natural sesquiterpene lactone, parthenolide. The putative modes of action of DMAPT are inhibition of the Nuclear chain factor kappa-light-chain enhancer of activated B cells (NFκB) pathway and depletion of glutathione levels; the latter causing cancer cells to be more susceptible to oxidative stress-induced cell death. Actinomycin-D (ActD) is a polypeptide antibiotic that binds to DNA, and inhibits RNA and protein synthesis by inhibiting RNA polymerase II. A phase 2 clinical trial indicated that ActD could be a potent drug against pancreatic cancer; however, it was not a favored drug due to toxicity issues. New drug entities and methods of drug delivery, used alone or in combination, are needed to treat pancreatic cancer more effectively. Thus, it was postulated that combining DMAPT and ActD would result in synergistic inhibition of Panc-1 pancreatic cancer cell growth because DMAPT's inhibition of NFκB would enhance induction of apoptosis by ActD, via phosphorylation of c-Jun, by minimizing NFκB inhibition of c-Jun phosphorylation. Combining these two drugs induced a higher level of cell death than each drug alone. A fixed drug ratio of DMAPT: ActD (1,200:1) was used. Data from metabolic (MTT) and colony formation assays were analyzed for synergism with CompuSyn software, which utilizes the Chou-Talalay equation. The analyses indicated synergism and moderate synergism at combination concentrations of DMAPT/ActD of 12/0.01 and 18/0.015 μM, respectively.
Mu X, Yin R, Wang D, et al.
Hepatic toxicity following actinomycin D chemotherapy in treatment of familial gestational trophoblastic neoplasia: A case report.
Medicine (Baltimore). 2018; 97(38):e12424 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Hepatic toxicity following actinomycin D chemotherapy in treatment of familial gestational trophoblastic neoplasia: A case report.
Medicine (Baltimore). 2018; 97(38):e12424 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
RATIONALE: Familial hydatidiform mole is extremely rare while familial gestational trophoblastic neoplasia (GTN) has never been reported. Inspired by 2 biological sisters with postmolar GTN and liver toxicity, we reviewed susceptible maternal-effect genes and explored the role of possible drug transporter genes in the development of GTN.
PATIENT CONCERNS: We reported one Chinese family where the two sisters developed postmolar GTN while experiencing fast remission and significant hepatic toxicity from actinomycin D chemotherapy.
DIAGNOSES: The index pregnancy was diagnosed with curettage. The following GTN was confirmed when there was a rise in beta-hCG for three consecutive weekly measurements over at least a period of 2 weeks. Computed tomography was used to identify lung metastasis. The elder sister was diagnosed with gestational trophoblastic neoplasia (III: 2) while the younger sister was diagnosed as III: 3 according to WHO scoring system.
INTERVENTIONS: Patients were treated with actinomycin D of 10 μg/kg intravenously for 5 days every 2 weeks. When hepatic toxicity was indicated, polyene phosphatidyl choline and magnesium isoglycyrrhizinate were prescribed.
OUTCOMES: Both patients responded extremely well to the 5-day actinomycin D regimen. Beta-hCG remained less than 2 mIU/ml after 5 cycles while computed tomography scan showed downsized pulmonary nodules. Both experienced significant rise in ALT and AST levels that could be ameliorated with corresponding medication. Monthly followed-up showed negative beta-hCG levels and normal liver enzyme levels.
LESSONS: We speculated that the known or unknown NLRP7 and KHDC3L mutations might be correlated with drug disposition in liver while liver drug transporters such as P-glycoprotein family that are also expressed in trophoblasts might be correlated to GTN susceptibility. Future genomic profiles of large samples alike using next generation sequencing are needed to confirm our hypothesis and discover yet unknown genes.
PATIENT CONCERNS: We reported one Chinese family where the two sisters developed postmolar GTN while experiencing fast remission and significant hepatic toxicity from actinomycin D chemotherapy.
DIAGNOSES: The index pregnancy was diagnosed with curettage. The following GTN was confirmed when there was a rise in beta-hCG for three consecutive weekly measurements over at least a period of 2 weeks. Computed tomography was used to identify lung metastasis. The elder sister was diagnosed with gestational trophoblastic neoplasia (III: 2) while the younger sister was diagnosed as III: 3 according to WHO scoring system.
INTERVENTIONS: Patients were treated with actinomycin D of 10 μg/kg intravenously for 5 days every 2 weeks. When hepatic toxicity was indicated, polyene phosphatidyl choline and magnesium isoglycyrrhizinate were prescribed.
OUTCOMES: Both patients responded extremely well to the 5-day actinomycin D regimen. Beta-hCG remained less than 2 mIU/ml after 5 cycles while computed tomography scan showed downsized pulmonary nodules. Both experienced significant rise in ALT and AST levels that could be ameliorated with corresponding medication. Monthly followed-up showed negative beta-hCG levels and normal liver enzyme levels.
LESSONS: We speculated that the known or unknown NLRP7 and KHDC3L mutations might be correlated with drug disposition in liver while liver drug transporters such as P-glycoprotein family that are also expressed in trophoblasts might be correlated to GTN susceptibility. Future genomic profiles of large samples alike using next generation sequencing are needed to confirm our hypothesis and discover yet unknown genes.
Kim HY, Veal GJ, Zhou F, Boddy AV
The role of solute carrier (SLC) transporters in actinomycin D pharmacokinetics in paediatric cancer patients.
Eur J Clin Pharmacol. 2018; 74(12):1575-1584 [PubMed] Related Publications
The role of solute carrier (SLC) transporters in actinomycin D pharmacokinetics in paediatric cancer patients.
Eur J Clin Pharmacol. 2018; 74(12):1575-1584 [PubMed] Related Publications
BACKGROUND: Actinomycin D is used for treatment of paediatric cancers; however, a large inter-patient pharmacokinetic (PK) variability and hepatotoxicity are significant limitations to its use and warrant further investigation. Elimination of actinomycin D may be mediated by transporters, as the drug does not seem to undergo significant metabolism. We investigated the role of solute carrier (SLC) transporters in actinomycin D PK.
METHODS: Fourteen key SLCs were screened through probe substrate uptake inhibition by actinomycin D in HEK293 cells. Uptake of actinomycin D was further studied in candidate SLCs by measuring intracellular actinomycin D using a validated LCMS assay. Pharmacogenetic analysis was conducted for 60 patients (Clinical trial: NCT00900354), who were genotyped for SNPs for OAT4 and PEPT2.
RESULTS: OAT4, OCT2, OCT3 and PEPT2 showed significantly lower probe substrate uptake (mean ± SD 75.0 ± 3.5% (p < 0.0001), 74.8 ± 11.2% (p = 0.001), 81.2 ± 14.0% (p = 0.0083) and 70.7 ± 5.7% (p = 0.0188)) compared to that of control. Intracellular accumulation of actinomycin D was greater compared to vector control in OAT4-transfected cells by 1.5- and 1.4-fold at 10 min (p = 0.01) and 20 min (p = 0.03), and in PEPT2-transfected cells by 1.5- and 1.7-fold at 10 min (p = 0.047) and 20 min (p = 0.043), respectively. Subsequent clinical study did not find a significant association between OAT4 rs11231809 and PEPT2 rs2257212 genotypes, and actinomycin D PK parameters such as clearance (CL) and volume of distribution (V
CONCLUSION: Transport of actinomycin D was mediated by OAT4 and PEPT2 in vitro. There was a lack of clinical significance of OAT4 and PEPT2 genotypes as predictors of actinomycin D disposition in paediatric cancer patients.
METHODS: Fourteen key SLCs were screened through probe substrate uptake inhibition by actinomycin D in HEK293 cells. Uptake of actinomycin D was further studied in candidate SLCs by measuring intracellular actinomycin D using a validated LCMS assay. Pharmacogenetic analysis was conducted for 60 patients (Clinical trial: NCT00900354), who were genotyped for SNPs for OAT4 and PEPT2.
RESULTS: OAT4, OCT2, OCT3 and PEPT2 showed significantly lower probe substrate uptake (mean ± SD 75.0 ± 3.5% (p < 0.0001), 74.8 ± 11.2% (p = 0.001), 81.2 ± 14.0% (p = 0.0083) and 70.7 ± 5.7% (p = 0.0188)) compared to that of control. Intracellular accumulation of actinomycin D was greater compared to vector control in OAT4-transfected cells by 1.5- and 1.4-fold at 10 min (p = 0.01) and 20 min (p = 0.03), and in PEPT2-transfected cells by 1.5- and 1.7-fold at 10 min (p = 0.047) and 20 min (p = 0.043), respectively. Subsequent clinical study did not find a significant association between OAT4 rs11231809 and PEPT2 rs2257212 genotypes, and actinomycin D PK parameters such as clearance (CL) and volume of distribution (V
CONCLUSION: Transport of actinomycin D was mediated by OAT4 and PEPT2 in vitro. There was a lack of clinical significance of OAT4 and PEPT2 genotypes as predictors of actinomycin D disposition in paediatric cancer patients.
Mu X, Song L, Li Q, et al.
Comparison of pulsed actinomycin D and 5-day actinomycin D as first-line chemotherapy for low-risk gestational trophoblastic neoplasia.
Int J Gynaecol Obstet. 2018; 143(2):225-231 [PubMed] Related Publications
Comparison of pulsed actinomycin D and 5-day actinomycin D as first-line chemotherapy for low-risk gestational trophoblastic neoplasia.
Int J Gynaecol Obstet. 2018; 143(2):225-231 [PubMed] Related Publications
OBJECTIVE: To compare the treatment outcome and cost-effectiveness of pulsed actinomycin D (Act-D) and 5-day Act-D in patients with low-risk gestational trophoblastic neoplasia (GTN).
METHOD: The present retrospective study included patients with low-risk GTN who received pulsed Act-D or 5-day Act-D as first-line chemotherapy at West China Second Hospital, Chengdu, China, between January 1, 2016, and December 31, 2017. Complete remission rates, mean number of treatment courses, and adverse events were compared, and a cost-effectiveness analysis was performed.
RESULTS: The study included 34 patients treated with pulsed Act-D and 26 patients treated with 5-day Act-D. Overall complete remission was observed in 21 (62%) patients in the pulsed Act-D group and 19 (73%) patients in the 5-day Act-D group (P=0.355); the mean number of treatment courses were 5.1 and 5.3, respectively (P=0.686). When Act-D failed, patients in each group required 4.9 and 4.6 courses, respectively, of a multi-agent regimen (P=0.545). No major adverse events were observed but moderate adverse events were more frequent in the pulsed Act-D group (P=0.011). The 5-day Act-D regimen was more expensive compared with pulsed Act-D regimen (US$7504.33 vs $5541.79), with an incremental cost-effectiveness ratio of $64 557.08 per avoidance of treatment failure.
CONCLUSION: Pulsed Act-D was more cost-effective than 5-day Act-D and could be preferred when considering Act-D as chemotherapy for low-risk GTN.
METHOD: The present retrospective study included patients with low-risk GTN who received pulsed Act-D or 5-day Act-D as first-line chemotherapy at West China Second Hospital, Chengdu, China, between January 1, 2016, and December 31, 2017. Complete remission rates, mean number of treatment courses, and adverse events were compared, and a cost-effectiveness analysis was performed.
RESULTS: The study included 34 patients treated with pulsed Act-D and 26 patients treated with 5-day Act-D. Overall complete remission was observed in 21 (62%) patients in the pulsed Act-D group and 19 (73%) patients in the 5-day Act-D group (P=0.355); the mean number of treatment courses were 5.1 and 5.3, respectively (P=0.686). When Act-D failed, patients in each group required 4.9 and 4.6 courses, respectively, of a multi-agent regimen (P=0.545). No major adverse events were observed but moderate adverse events were more frequent in the pulsed Act-D group (P=0.011). The 5-day Act-D regimen was more expensive compared with pulsed Act-D regimen (US$7504.33 vs $5541.79), with an incremental cost-effectiveness ratio of $64 557.08 per avoidance of treatment failure.
CONCLUSION: Pulsed Act-D was more cost-effective than 5-day Act-D and could be preferred when considering Act-D as chemotherapy for low-risk GTN.
Li L, Wan X, Feng F, et al.
Pulse actinomycin D as first-line treatment of low-risk post-molar non-choriocarcinoma gestational trophoblastic neoplasia.
BMC Cancer. 2018; 18(1):585 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Pulse actinomycin D as first-line treatment of low-risk post-molar non-choriocarcinoma gestational trophoblastic neoplasia.
BMC Cancer. 2018; 18(1):585 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
BACKGROUND: Little data exists predicting the resistance to actinomycin D (Act-D) single-agent for gestational trophoblastic neoplasia (GTN). The objective was to determine the overall success of pulse Act-D and the factors predictive of resistance to pulse Act-D in the treatment of low-risk, non-choriocarcinoma post-molar GTN.
METHODS: From January 2013 to October 2016, according to the FIGO criteria for the diagnosis of post-molar disease and the FIGO risk-factor scoring system for GTN, a total of 135 patients with post-molar non-choriocarcinoma GTN who were chemotherapy-naive with a FIGO score < 7 were treated with single-agent pulse Act-D as a first-line regimen, in Peking Union Medical College Hospital. The pulse Act-D regimen is defined as 1.25 mg/m
RESULTS: Ninety-six of 135 patients (71.1%) achieved complete remission after first-line chemotherapy of pulse Act-D. In multivariate analysis, existing invasive uterine lesions observed by pre-chemotherapy transvaginal ultrasound (odds ratio [OR] 7.5, 95% confidence intervals [CI] 2.7-20.8), FIGO score ≥ 5 (OR 15.2, 95% CI 1.5-156.1) and pre-chemotherapy levels of β-hCG ≥ 4000 IU/L (OR 3.1, 95% CI 1.2-8.3) were independent high-risk factors predicting resistance to pulse Act-D as single-agent chemotherapy. During follow-up, no relapse, treatment-associated serious adverse events, or death occurred.
CONCLUSIONS: As first-line chemotherapy, pulse Act-D was effective and tolerable for patients with low-risk post-molar non-choriocarcinoma. Existing invasive uterine lesions observed by pre-chemotherapy transvaginal ultrasound, a FIGO score ≥ 5, and pre-chemotherapy levels of β-hCG ≥ 4000 IU/L were independent factors for resistance to pulse Act-D.
METHODS: From January 2013 to October 2016, according to the FIGO criteria for the diagnosis of post-molar disease and the FIGO risk-factor scoring system for GTN, a total of 135 patients with post-molar non-choriocarcinoma GTN who were chemotherapy-naive with a FIGO score < 7 were treated with single-agent pulse Act-D as a first-line regimen, in Peking Union Medical College Hospital. The pulse Act-D regimen is defined as 1.25 mg/m
RESULTS: Ninety-six of 135 patients (71.1%) achieved complete remission after first-line chemotherapy of pulse Act-D. In multivariate analysis, existing invasive uterine lesions observed by pre-chemotherapy transvaginal ultrasound (odds ratio [OR] 7.5, 95% confidence intervals [CI] 2.7-20.8), FIGO score ≥ 5 (OR 15.2, 95% CI 1.5-156.1) and pre-chemotherapy levels of β-hCG ≥ 4000 IU/L (OR 3.1, 95% CI 1.2-8.3) were independent high-risk factors predicting resistance to pulse Act-D as single-agent chemotherapy. During follow-up, no relapse, treatment-associated serious adverse events, or death occurred.
CONCLUSIONS: As first-line chemotherapy, pulse Act-D was effective and tolerable for patients with low-risk post-molar non-choriocarcinoma. Existing invasive uterine lesions observed by pre-chemotherapy transvaginal ultrasound, a FIGO score ≥ 5, and pre-chemotherapy levels of β-hCG ≥ 4000 IU/L were independent factors for resistance to pulse Act-D.
Prouvot C, Golfier F, Massardier J, et al.
Efficacy and Safety of Second-Line 5-Day Dactinomycin in Case of Methotrexate Failure for Gestational Trophoblastic Neoplasia.
Int J Gynecol Cancer. 2018; 28(5):1038-1044 [PubMed] Related Publications
Efficacy and Safety of Second-Line 5-Day Dactinomycin in Case of Methotrexate Failure for Gestational Trophoblastic Neoplasia.
Int J Gynecol Cancer. 2018; 28(5):1038-1044 [PubMed] Related Publications
OBJECTIVE: The objective of this study was to evaluate the characteristics and outcomes of patients treated for gestational trophoblastic neoplasia (GTN) with second-line 5-day dactinomycin after failed first-line 8-day methotrexate.
METHODS: From 1999 to 2017, patients with methotrexate resistant GTN treated with second line dactinomycin were identified at the French Trophoblastic Disease Reference Center. Using univariate and multivariate analysis, we identified significant predictive factors of second line dactinomycin failure.
RESULTS: A total of 877 GTN patients were treated with first-line 8-day methotrexate, of which 103 required second-line 5-day dactinomycin for methotrexate failure. Complete response was observed in 78 patients (75.7% [95% confidence interval, 66.3-83.6]; P < 0.0001), whereas 25 needed third-line treatment, 13 for dactinomycin resistance and 12 for post-dactinomycin relapse. Overall survival of patients treated with dactinomycin was 100%. An interval of greater than or equal to 7 months between antecedent pregnancy termination and methotrexate initiation was a predictive factor significantly associated with second-line dactinomycin failure in multivariate analysis (exact odds ratio, 9.17 [95% confidence interval, 1.98-50.70]; P = 0.0029). No grades 4 and 5 adverse effects were experienced and the most common toxicity being grade 1 nausea (14.6%).
CONCLUSION: Given a 75.7% complete response rate in methotrexate failed low-risk GTN patients treated with second-line dactinomycin and an overall survival rate of 100% after third-line treatment, the use of dactinomycin should be favored as second-line, regardless of human chorionic gonadotropin level at the time of dactinomycin initiation. However, an interval between the termination of the antecedent pregnancy and methotrexate initiation longer than 6 months should encourage considering alternative therapeutic strategies.
METHODS: From 1999 to 2017, patients with methotrexate resistant GTN treated with second line dactinomycin were identified at the French Trophoblastic Disease Reference Center. Using univariate and multivariate analysis, we identified significant predictive factors of second line dactinomycin failure.
RESULTS: A total of 877 GTN patients were treated with first-line 8-day methotrexate, of which 103 required second-line 5-day dactinomycin for methotrexate failure. Complete response was observed in 78 patients (75.7% [95% confidence interval, 66.3-83.6]; P < 0.0001), whereas 25 needed third-line treatment, 13 for dactinomycin resistance and 12 for post-dactinomycin relapse. Overall survival of patients treated with dactinomycin was 100%. An interval of greater than or equal to 7 months between antecedent pregnancy termination and methotrexate initiation was a predictive factor significantly associated with second-line dactinomycin failure in multivariate analysis (exact odds ratio, 9.17 [95% confidence interval, 1.98-50.70]; P = 0.0029). No grades 4 and 5 adverse effects were experienced and the most common toxicity being grade 1 nausea (14.6%).
CONCLUSION: Given a 75.7% complete response rate in methotrexate failed low-risk GTN patients treated with second-line dactinomycin and an overall survival rate of 100% after third-line treatment, the use of dactinomycin should be favored as second-line, regardless of human chorionic gonadotropin level at the time of dactinomycin initiation. However, an interval between the termination of the antecedent pregnancy and methotrexate initiation longer than 6 months should encourage considering alternative therapeutic strategies.
Luchsinger C, Aguilar M, Burgos PV, et al.
Functional disruption of the Golgi apparatus protein ARF1 sensitizes MDA-MB-231 breast cancer cells to the antitumor drugs Actinomycin D and Vinblastine through ERK and AKT signaling.
PLoS One. 2018; 13(4):e0195401 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Functional disruption of the Golgi apparatus protein ARF1 sensitizes MDA-MB-231 breast cancer cells to the antitumor drugs Actinomycin D and Vinblastine through ERK and AKT signaling.
PLoS One. 2018; 13(4):e0195401 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Increasing evidence indicates that the Golgi apparatus plays active roles in cancer, but a comprehensive understanding of its functions in the oncogenic transformation has not yet emerged. At the same time, the Golgi is becoming well recognized as a hub that integrates its functions of protein and lipid biosynthesis to signal transduction for cell proliferation and migration in cancer cells. Nevertheless, the active function of the Golgi apparatus in cancer cells has not been fully evaluated as a target for combined treatment. Here, we analyzed the effect of perturbing the Golgi apparatus on the sensitivity of the MDA-MB-231 breast cancer cell line to the drugs Actinomycin D and Vinblastine. We disrupted the function of ARF1, a protein necessary for the homeostasis of the Golgi apparatus. We found that the expression of the ARF1-Q71L mutant increased the sensitivity of MDA-MB-231 cells to both Actinomycin D and Vinblastine, resulting in decreased cell proliferation and cell migration, as well as in increased apoptosis. Likewise, the combined treatment of cells with Actinomycin D or Vinblastine and Brefeldin A or Golgicide A, two disrupting agents of the ARF1 function, resulted in similar effects on cell proliferation, cell migration and apoptosis. Interestingly, each combined treatment had distinct effects on ERK1/2 and AKT signaling, as indicated by the decreased levels of either phospho-ERK1/2 or phospho-AKT. Our results suggest that disruption of Golgi function could be used as a strategy for the sensitization of cancer cells to chemotherapy.
Wang Y, Xia C, Lv Y, et al.
Crosstalk Influence between P38MAPK and Autophagy on Mitochondria-Mediated Apoptosis Induced by Anti-Fas Antibody/Actinomycin D in Human Hepatoma Bel-7402 Cells.
Molecules. 2017; 22(10) [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Crosstalk Influence between P38MAPK and Autophagy on Mitochondria-Mediated Apoptosis Induced by Anti-Fas Antibody/Actinomycin D in Human Hepatoma Bel-7402 Cells.
Molecules. 2017; 22(10) [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Our previous study indicated that anti-Fas antibody/actinomycin D (AF/AD) induced apoptosis of human hepatocellular carcinoma Bel-7402 cells; however, crosstalk influence between P38MAPK and autophagy on mitochondria-mediated apoptosis induced by AF/AD in Bel-7402 cells remains unclear. Therefore, effect of AF/AD on apoptosis, autophagy, phosphorylated-P38MAPK (p-P38MAPK), and membrane potential (ΔΨm) with or without the P38MAPK inhibitor SB203580 or the autophagy inhibitor 3-methyladenine (3-MA) in Bel-7402 cells was investigated in the present study. The results showed that AF/AD resulted in induction of apoptosis concomitant with autophagy, upregulation of p-P38MAPK and autophagy-associated gene proteins (Atg5-Atg12 protein complex, Atg7, Atg10, Beclin-1, LC3 I, and LC3 II), and downregulation of ΔΨm in Bel-7402 cells. In contrast, SB203580 attenuated the effects of AF/AD in Bel-7402 cells. Furthermore, the findings also demonstrated that 3-MA inhibited the impact of AF/AD on autophagy, Atg5-Atg12 protein complex, Atg7, Atg10, Beclin-1, LC3 I, LC3 II, and ΔΨm, and promoted the influence of AF/AD on apoptosis and p-P38MAPK in Bel-7402 cells. Taken together, we conclude that crosstalk between P38MAPK and autophagy regulates mitochondria-mediated apoptosis induced by AF/AD in Bel-7402 cells.
Wang Q, Fu J, Hu L, et al.
Prophylactic chemotherapy for hydatidiform mole to prevent gestational trophoblastic neoplasia.
Cochrane Database Syst Rev. 2017; 9:CD007289 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Prophylactic chemotherapy for hydatidiform mole to prevent gestational trophoblastic neoplasia.
Cochrane Database Syst Rev. 2017; 9:CD007289 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
BACKGROUND: This is an update of the original Cochrane Review published in Cochrane Library, Issue 10, 2012.Hydatidiform mole (HM), also called a molar pregnancy, is characterised by an overgrowth of foetal chorionic tissue within the uterus. HMs may be partial (PM) or complete (CM) depending on their gross appearance, histopathology and karyotype. PMs usually have a triploid karyotype, derived from maternal and paternal origins, whereas CMs are diploid and have paternal origins only. Most women with HM can be cured by evacuation of retained products of conception (ERPC) and their fertility preserved. However, in some women the growth persists and develops into gestational trophoblastic neoplasia (GTN), a malignant form of the disease that requires treatment with chemotherapy. CMs have a higher rate of malignant transformation than PMs. It may be possible to reduce the risk of GTN in women with HM by administering prophylactic chemotherapy (P-Chem). However, P-Chem given before or after evacuation of HM to prevent malignant sequelae remains controversial, as the risks and benefits of this practice are unclear.
OBJECTIVES: To evaluate the effectiveness and safety of P-Chem to prevent GTN in women with a molar pregnancy. To investigate whether any subgroup of women with HM may benefit more from P-Chem than others.
SEARCH METHODS: For the original review we performed electronic searches in the Cochrane Gynaecological Cancer Specialised Register, the Cochrane Central Register of Controlled Trials (CENTRAL, Issue 2, 2012), MEDLINE (1946 to February week 4, 2012) and Embase (1980 to 2012, week 9). We developed the search strategy using free text and MeSH. For this update we searched the Cochrane Central Register of Controlled Trials (CENTRAL, Issue 5, 2017), MEDLINE (February 2012 to June week 1, 2017) and Embase (February 2012 to 2017, week 23). We also handsearched reference lists of relevant literature to identify additional studies and searched trial registries.
SELECTION CRITERIA: We included randomised controlled trials (RCTs) of P-Chem for HM.
DATA COLLECTION AND ANALYSIS: Two review authors independently assessed studies for inclusion in the review and extracted data using a specifically designed data collection form. Meta-analyses were performed by pooling data from individual trials using Review Manager 5 (RevMan 5) software in line with standard methodological procedures expected by Cochrane methodology.
MAIN RESULTS: The searches identified 161 records; after de-duplication and title and abstract screening 90 full-text articles were retrieved. From these we included three RCTs with a combined total of 613 participants. One study compared prophylactic dactinomycin to no prophylaxis (60 participants); the other two studies compared prophylactic methotrexate to no prophylaxis (420 and 133 participants). All participants were diagnosed with CMs. We considered the latter two studies to be of poor methodological quality.P-Chem reduced the risk of GTN occurring in women following a CM (3 studies, 550 participants; risk ratio (RR) 0.37, 95% confidence interval (CI) 0.24 to 0.57; I² = 0%; P < 0.00001; low-quality evidence). However, owing to the poor quality (high risk of bias) of two of the included studies, we performed sensitivity analyses excluding these two studies. This left only one small study of high-risk women to contribute data for this primary outcome (59 participants; RR 0.28, 95% CI 0.10 to 0.73; P = 0.01); therefore we consider this evidence to be of low quality.The time to diagnosis was longer in the P-Chem group than the control group (2 studies, 33 participants; mean difference (MD) 28.72, 95% CI 13.19 to 44.24; P = 0.0003; low-quality evidence); and the P-Chem group required more courses to cure subsequent GTN (1 poor-quality study, 14 participants; MD 1.10, 95% CI 0.52 to 1.68; P = 0.0002; very low quality evidence).There were insufficient data to perform meta-analyses for toxicity, overall survival, drug resistance and reproductive outcomes.
AUTHORS' CONCLUSIONS: P-Chem may reduce the risk of progression to GTN in women with CMs who are at a high risk of malignant transformation; however, current evidence in favour of P-Chem is limited by the poor methodological quality and small size of the included studies. As P-Chem may increase drug resistance, delays treatment of GTN and may expose women toxic side effects, this practice cannot currently be recommended.
OBJECTIVES: To evaluate the effectiveness and safety of P-Chem to prevent GTN in women with a molar pregnancy. To investigate whether any subgroup of women with HM may benefit more from P-Chem than others.
SEARCH METHODS: For the original review we performed electronic searches in the Cochrane Gynaecological Cancer Specialised Register, the Cochrane Central Register of Controlled Trials (CENTRAL, Issue 2, 2012), MEDLINE (1946 to February week 4, 2012) and Embase (1980 to 2012, week 9). We developed the search strategy using free text and MeSH. For this update we searched the Cochrane Central Register of Controlled Trials (CENTRAL, Issue 5, 2017), MEDLINE (February 2012 to June week 1, 2017) and Embase (February 2012 to 2017, week 23). We also handsearched reference lists of relevant literature to identify additional studies and searched trial registries.
SELECTION CRITERIA: We included randomised controlled trials (RCTs) of P-Chem for HM.
DATA COLLECTION AND ANALYSIS: Two review authors independently assessed studies for inclusion in the review and extracted data using a specifically designed data collection form. Meta-analyses were performed by pooling data from individual trials using Review Manager 5 (RevMan 5) software in line with standard methodological procedures expected by Cochrane methodology.
MAIN RESULTS: The searches identified 161 records; after de-duplication and title and abstract screening 90 full-text articles were retrieved. From these we included three RCTs with a combined total of 613 participants. One study compared prophylactic dactinomycin to no prophylaxis (60 participants); the other two studies compared prophylactic methotrexate to no prophylaxis (420 and 133 participants). All participants were diagnosed with CMs. We considered the latter two studies to be of poor methodological quality.P-Chem reduced the risk of GTN occurring in women following a CM (3 studies, 550 participants; risk ratio (RR) 0.37, 95% confidence interval (CI) 0.24 to 0.57; I² = 0%; P < 0.00001; low-quality evidence). However, owing to the poor quality (high risk of bias) of two of the included studies, we performed sensitivity analyses excluding these two studies. This left only one small study of high-risk women to contribute data for this primary outcome (59 participants; RR 0.28, 95% CI 0.10 to 0.73; P = 0.01); therefore we consider this evidence to be of low quality.The time to diagnosis was longer in the P-Chem group than the control group (2 studies, 33 participants; mean difference (MD) 28.72, 95% CI 13.19 to 44.24; P = 0.0003; low-quality evidence); and the P-Chem group required more courses to cure subsequent GTN (1 poor-quality study, 14 participants; MD 1.10, 95% CI 0.52 to 1.68; P = 0.0002; very low quality evidence).There were insufficient data to perform meta-analyses for toxicity, overall survival, drug resistance and reproductive outcomes.
AUTHORS' CONCLUSIONS: P-Chem may reduce the risk of progression to GTN in women with CMs who are at a high risk of malignant transformation; however, current evidence in favour of P-Chem is limited by the poor methodological quality and small size of the included studies. As P-Chem may increase drug resistance, delays treatment of GTN and may expose women toxic side effects, this practice cannot currently be recommended.
Farhane Z, Bonnier F, Byrne HJ
An in vitro study of the interaction of the chemotherapeutic drug Actinomycin D with lung cancer cell lines using Raman micro-spectroscopy.
J Biophotonics. 2018; 11(1) [PubMed] Related Publications
An in vitro study of the interaction of the chemotherapeutic drug Actinomycin D with lung cancer cell lines using Raman micro-spectroscopy.
J Biophotonics. 2018; 11(1) [PubMed] Related Publications
The applications of Raman microspectroscopy have been extended in recent years into the field of clinical medicine, and specifically in cancer research, as a non-invasive diagnostic method in vivo and ex vivo, and the field of pharmaceutical development as a label-free predictive technique for new drug mechanisms of action in vitro. To further illustrate its potential for such applications, it is important to establish its capability to fingerprint drug mechanisms of action and different cellular reactions. In this study, cytotoxicity assays were employed to establish the toxicity profiles for 48 and 72 hours exposure of lung cancer cell lines, A549 and Calu-1, after exposure to Actinomycin D (ACT) and Raman micro-spectroscopy was used to track its mechanism of action at subcellular level and subsequent cellular responses. Multivariate data analysis was used to elucidate the spectroscopic signatures associated with ACT chemical binding and cellular resistances. Results show that the ACT uptake and mechanism of action are similar in the 2 cell lines, while A549 cells exhibits spectral signatures of resistance to apoptosis related to its higher chemoresistance to the anticancer drug ACT. The observations are discussed in comparison to previous studies of the similar anthracyclic chemotherapeutic agent Doxorubicin. A, Preprocessed Raman spectrum of ACT stock solution dissolved in sterile water and mean spectrum with SD of (B) nucleolus, (C) nucleus and (D) cytoplasm of A549 cell lines after 48 hours exposure to the corresponding IC
Liang Y, Yang Z, Xu ZG, Ma L
Toxic epidermal necrolysis after dactinomycin and vincristine combination chemotherapy for nephroblastoma.
J Zhejiang Univ Sci B. 2017; 18(7):649-652 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Toxic epidermal necrolysis after dactinomycin and vincristine combination chemotherapy for nephroblastoma.
J Zhejiang Univ Sci B. 2017; 18(7):649-652 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
In this study, we describe a 2-year-old boy patient with nephroblastoma who has developed toxic epidermal necrolysis (TEN) associated with the combination chemotherapy administration of dactinomycin and vincristine. A skin biopsy confirmed the diagnosis of TEN, and with methylprednisolone pulse therapy, intravenous immunoglobulin (IVIG), and supportive care, the patient improved significantly.
Schmidt C, Schubert NA, Brabetz S, et al.
Preclinical drug screen reveals topotecan, actinomycin D, and volasertib as potential new therapeutic candidates for ETMR brain tumor patients.
Neuro Oncol. 2017; 19(12):1607-1617 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Preclinical drug screen reveals topotecan, actinomycin D, and volasertib as potential new therapeutic candidates for ETMR brain tumor patients.
Neuro Oncol. 2017; 19(12):1607-1617 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Background: Embryonal tumor with multilayered rosettes (ETMR) is a rare and aggressive embryonal brain tumor that solely occurs in infants and young children and has only recently been recognized as a separate brain tumor entity in the World Health Organization classification for CNS tumors. Patients have a very dismal prognosis with a median survival of 12 months upon diagnosis despite aggressive treatment. The aim of this study was to develop novel treatment regimens in a preclinical drug screen in order to inform potentially more active clinical trial protocols.
Methods: We have carried out an in vitro and in vivo drug screen using the ETMR cell line BT183 and its xenograft model. Furthermore, we have generated the first patient-derived xenograft (PDX) model for ETMR and evaluated our top drug candidates in an in vitro drug screen using this model.
Results: BT183 cells are very sensitive to the topoisomerase inhibitors topotecan and doxorubicin, to the epigenetic agents decitabine and panobinostat, to actinomycin D, and to targeted drugs such as the polo-like kinase 1 (PLK1) inhibitor volasertib, the aurora kinase A inhibitor alisertib, and the mammalian target of rapamycin (mTOR) inhibitor MLN0128. In xenograft mice, monotherapy with topotecan, volasertib, and actinomycin D led to a temporary response in tumor growth and a significant increase in survival. Finally, using multi-agent treatment regimens of topotecan or doxorubicin combined with methotrexate and vincristine, the response in tumor growth and survival was further increased compared with mice receiving single treatments.
Conclusions: We have identified several promising candidates for combination therapies in future clinical trials for ETMR patients.
Methods: We have carried out an in vitro and in vivo drug screen using the ETMR cell line BT183 and its xenograft model. Furthermore, we have generated the first patient-derived xenograft (PDX) model for ETMR and evaluated our top drug candidates in an in vitro drug screen using this model.
Results: BT183 cells are very sensitive to the topoisomerase inhibitors topotecan and doxorubicin, to the epigenetic agents decitabine and panobinostat, to actinomycin D, and to targeted drugs such as the polo-like kinase 1 (PLK1) inhibitor volasertib, the aurora kinase A inhibitor alisertib, and the mammalian target of rapamycin (mTOR) inhibitor MLN0128. In xenograft mice, monotherapy with topotecan, volasertib, and actinomycin D led to a temporary response in tumor growth and a significant increase in survival. Finally, using multi-agent treatment regimens of topotecan or doxorubicin combined with methotrexate and vincristine, the response in tumor growth and survival was further increased compared with mice receiving single treatments.
Conclusions: We have identified several promising candidates for combination therapies in future clinical trials for ETMR patients.
Das T, Nair RR, Green R, et al.
Actinomycin D Down-regulates SOX2 Expression and Induces Death in Breast Cancer Stem Cells.
Anticancer Res. 2017; 37(4):1655-1663 [PubMed] Related Publications
Actinomycin D Down-regulates SOX2 Expression and Induces Death in Breast Cancer Stem Cells.
Anticancer Res. 2017; 37(4):1655-1663 [PubMed] Related Publications
BACKGROUND/AIM: One of the major hurdles in the treatment of breast cancers is the inability of anti-cancer drugs to eliminate the breast cancer stem cells (BCSCs) population, which leads to disease relapse. The dearth in anti-cancer drugs that target BCSCs can be attributed to the absence of in vitro screening models that can not only recapitulate the tumor microenvironment consisting of BCSCs but also preserve the 3-dimensional (3D) architecture of in vivo tumors.
MATERIALS AND METHODS: In our present study, we have developed a 3D cell culture system that shows: (i) enrichment of BCSCs, (ii) increased drug resistance, and (iii) generation of hypoxic conditions similar to tumors.
RESULTS: Using this model, we were able to screen a FDA-approved diversity set and identify as well as validate actinomycin D as a potential anti-breast cancer agent. Interestingly, we show that actinomycin D specifically targets and down-regulates the expression of the stem cell transcription factor, Sox-2. Additionally, down-regulation of Sox-2 leads to depletion of the stem-cell population resulting in the inability of breast cancer cells to initiate tumor progression.
CONCLUSION: This study demonstrates the utility of an in vivo-like 3D cell culture system for the identification and validation of anti-cancer agents that will have a better probability of success in the clinic.
MATERIALS AND METHODS: In our present study, we have developed a 3D cell culture system that shows: (i) enrichment of BCSCs, (ii) increased drug resistance, and (iii) generation of hypoxic conditions similar to tumors.
RESULTS: Using this model, we were able to screen a FDA-approved diversity set and identify as well as validate actinomycin D as a potential anti-breast cancer agent. Interestingly, we show that actinomycin D specifically targets and down-regulates the expression of the stem cell transcription factor, Sox-2. Additionally, down-regulation of Sox-2 leads to depletion of the stem-cell population resulting in the inability of breast cancer cells to initiate tumor progression.
CONCLUSION: This study demonstrates the utility of an in vivo-like 3D cell culture system for the identification and validation of anti-cancer agents that will have a better probability of success in the clinic.
Verhoef L, Baartz D, Morrison S, et al.
Outcomes of women diagnosed and treated for low-risk gestational trophoblastic neoplasia at the Queensland Trophoblast Centre (QTC).
Aust N Z J Obstet Gynaecol. 2017; 57(4):458-463 [PubMed] Related Publications
Outcomes of women diagnosed and treated for low-risk gestational trophoblastic neoplasia at the Queensland Trophoblast Centre (QTC).
Aust N Z J Obstet Gynaecol. 2017; 57(4):458-463 [PubMed] Related Publications
BACKGROUND: Gestational trophoblastic neoplasia (GTN) is classified as a highly curable group of pregnancy-related malignancies; however, approximately 15% will be persistent and require chemotherapy. Up to 25% of these women will develop resistance and 2% will develop disease relapse after initial chemotherapy. Despite the need for further chemotherapy in these women, cure rates are high.
OBJECTIVE: To evaluate the outcomes of women diagnosed with low-risk GTN, assessing the type of treatment, the number of chemotherapy cycles received, development of resistance or disease relapse, survival, and to assess the feasibility of changing to a new drug regimen.
METHODS: From March 2012 until February 2015, a retrospective study was conducted and 38 cases with low-risk GTN were reviewed. The number of cycles, type of treatment received, duration of treatment, development of resistance and disease relapse, and adverse side effects were analysed.
RESULTS: The median duration of follow-up was 12 months. Disease-free survival was 100% and primary complete remission rates were achieved in 85.3% of patients who were treated with actinomycin D and 25% patients who were treated with methotrexate (MTX). A change in chemotherapy was required for nine patients. One patient developed disease relapse. Nausea, fatigue and constipation were the most frequent adverse events reported with actinomycin D. All women were cured of their disease.
CONCLUSION: All women were successfully treated and achieved complete remission. Changing from MTX to actinomycin D as first-line chemotherapy for women with low-risk GTN was feasible and safe.
OBJECTIVE: To evaluate the outcomes of women diagnosed with low-risk GTN, assessing the type of treatment, the number of chemotherapy cycles received, development of resistance or disease relapse, survival, and to assess the feasibility of changing to a new drug regimen.
METHODS: From March 2012 until February 2015, a retrospective study was conducted and 38 cases with low-risk GTN were reviewed. The number of cycles, type of treatment received, duration of treatment, development of resistance and disease relapse, and adverse side effects were analysed.
RESULTS: The median duration of follow-up was 12 months. Disease-free survival was 100% and primary complete remission rates were achieved in 85.3% of patients who were treated with actinomycin D and 25% patients who were treated with methotrexate (MTX). A change in chemotherapy was required for nine patients. One patient developed disease relapse. Nausea, fatigue and constipation were the most frequent adverse events reported with actinomycin D. All women were cured of their disease.
CONCLUSION: All women were successfully treated and achieved complete remission. Changing from MTX to actinomycin D as first-line chemotherapy for women with low-risk GTN was feasible and safe.
Yoshihara H, Yoshimoto Y, Hosoya Y, et al.
Infantile fibrosarcoma treated with postoperative vincristine and dactinomycin.
Pediatr Int. 2017; 59(3):371-374 [PubMed] Related Publications
Infantile fibrosarcoma treated with postoperative vincristine and dactinomycin.
Pediatr Int. 2017; 59(3):371-374 [PubMed] Related Publications
Infantile fibrosarcoma is a non-rhabdomyosarcoma soft-tissue sarcoma that occurs in infancy and which has a relatively good prognosis. A vincristine and dactinomycin (VA) regimen has been shown to be effective, although the duration of chemotherapy has not been well defined. We describe the case of a 4-month-old boy with a mass at the left dorsum of the foot who was diagnosed with infantile fibrosarcoma after resection of the tumor, the margin of which was macroscopically positive. VA treatment was carried out with careful monitoring of response and adverse effects. Pancytopenia was seen during the second cycle, and therapy was reduced thereafter. The treatment was continued for 38 weeks (12 cycles). There was no functional impairment, and no evidence of recurrence at 18 months after therapy.
Xu Y, Zhao Y, Xu Y, et al.
Blocking inhibition to YAP by ActinomycinD enhances anti-tumor efficacy of Corosolic acid in treating liver cancer.
Cell Signal. 2017; 29:209-217 [PubMed] Related Publications
Blocking inhibition to YAP by ActinomycinD enhances anti-tumor efficacy of Corosolic acid in treating liver cancer.
Cell Signal. 2017; 29:209-217 [PubMed] Related Publications
Chemotherapy is critical for the treatment of liver cancer. Despite the pro-apoptotic effects of corosolic acid (CA) have been revealed, the methods to enhance its efficacy are unclear. The aim of this study is to investigate the target that might reduce CA efficacy and figure out the way to conquer it. We found reduction of Yes-associated protein (YAP) might be a critical event that suppresses efficacy of CA. Treatment of CA accelerated degradation of YAP via enhancing its phosphorylation by LATS1. Moreover, we found CA boosts βTrCP-dependent Ubiquitination of YAP. Interestingly, the protein stability of βTrCP per se could be enhanced by CA. Notably, ActionomycinD (AD) strengthened CA-induced apoptosis of liver cancer cells via elevating YAP while down-regulating βTrCP. Importantly, combined treatment of CA and AD had much more obvious influences against transformative phenotypes of liver cancer cells than those under treatment of CA alone. Combined usage of AD successfully reduced IC50 value of CA. In summary, we have first uncovered that suppression of YAP might reduce efficacy of CA to treat liver cancer, combined treatment of AD and CA might solve this problem.
Lee YJ, Park JY, Kim DY, et al.
Comparing and evaluating the efficacy of methotrexate and actinomycin D as first-line single chemotherapy agents in low risk gestational trophoblastic disease.
J Gynecol Oncol. 2017; 28(2):e8 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Comparing and evaluating the efficacy of methotrexate and actinomycin D as first-line single chemotherapy agents in low risk gestational trophoblastic disease.
J Gynecol Oncol. 2017; 28(2):e8 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
OBJECTIVE: The aim of this study was to compare responses to single-agent chemotherapies and evaluate the predictive factors of resistance in low risk (LR) gestational trophoblastic disease (GTD). The chemotherapy agents included methotrexate (MTX) and actinomycin D (ACT-D).
METHODS: We conducted a retrospective study of 126 patients with GTD who were treated between 2000 and 2013. A total of 71 patients with LR GTD were treated with MTX (8-day regimen or weekly regimen, n=53) or ACT-D (bi-weekly pulsed regimen or 5-day regimen, n=18). The successful treatment group and the failed treatment group were compared and analyzed to identify prognostic factors.
RESULTS: The complete response rates were 83.3% for ACT-D and 62.2% for MTX, with no statistically significant difference. There was no severe adverse effect reported for either group. Longer interval durations from the index pregnancy (>2 months, p=0.040) and larger tumor size (>3 cm, p=0.020) were more common in non-responders than in responders; these results were statistically significant.
CONCLUSION: Based on our results, ACT-D may be a better option than MTX as a first-line single chemotherapy agent for LR GTD. The bi-weekly pulsed ACT-D regimen had minimal, or at least the same, toxicities compared with MTX. However, due to the lack of strong supporting evidence, it cannot be conclusively stated that this is the best single agent for first-line chemotherapy in LR GTD patients. Further larger controlled trials will be necessary to establish the best guidelines for GTD treatment.
METHODS: We conducted a retrospective study of 126 patients with GTD who were treated between 2000 and 2013. A total of 71 patients with LR GTD were treated with MTX (8-day regimen or weekly regimen, n=53) or ACT-D (bi-weekly pulsed regimen or 5-day regimen, n=18). The successful treatment group and the failed treatment group were compared and analyzed to identify prognostic factors.
RESULTS: The complete response rates were 83.3% for ACT-D and 62.2% for MTX, with no statistically significant difference. There was no severe adverse effect reported for either group. Longer interval durations from the index pregnancy (>2 months, p=0.040) and larger tumor size (>3 cm, p=0.020) were more common in non-responders than in responders; these results were statistically significant.
CONCLUSION: Based on our results, ACT-D may be a better option than MTX as a first-line single chemotherapy agent for LR GTD. The bi-weekly pulsed ACT-D regimen had minimal, or at least the same, toxicities compared with MTX. However, due to the lack of strong supporting evidence, it cannot be conclusively stated that this is the best single agent for first-line chemotherapy in LR GTD patients. Further larger controlled trials will be necessary to establish the best guidelines for GTD treatment.
Miller CR, Chappell NP, Sledge C, et al.
Are different methotrexate regimens as first line therapy for low risk gestational trophoblastic neoplasia more cost effective than the dactinomycin regimen used in GOG 0174?
Gynecol Oncol. 2017; 144(1):125-129 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Are different methotrexate regimens as first line therapy for low risk gestational trophoblastic neoplasia more cost effective than the dactinomycin regimen used in GOG 0174?
Gynecol Oncol. 2017; 144(1):125-129 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
OBJECTIVES: Gynecologic Oncology Group (GOG) 0174 compared weekly intramuscular methotrexate (MTX) with biweekly pulsed intravenous dactinomycin (Act-D) as single-agent chemotherapy for low-risk gestational trophoblastic neoplasia (GTN). Act-D had a higher rate of initial complete response (CR) (70% vs. 53%, p=0.01), but multi-day regimens of MTX have higher historic success rates. We assessed the cost-effectiveness of Act-D vs. MTX per GOG 0174 and explored multi-day MTX regimens.
METHODS: A cost effectiveness decision model was constructed with data from GOG 0174. Outcome was cost per first-line treatment success expressed in terms of incremental cost-effectiveness ratio (ICER). Front-line failures were assumed to receive cross-over single agent therapy, second line failures; multi-agent chemotherapy. GOG 0174 had no quality of life (QOL) evaluation, so equal QOL (utility 1.0) was assumed but varied in sensitivity analysis. A second exploratory model included 5-day and 8-day MTX regimens.
RESULTS: Act-D ($18,505) was more expensive compared to weekly MTX ($8950) with an ICER of $56,215 per first-line treatment success compared to weekly MTX. Small decreases in QOL dramatically increased the ICER during sensitivity analysis. Models with multi-day MTX regimens were also more cost-effective than Act-D. If effectiveness was redefined as avoidance of multi-agent chemotherapy, weekly MTX was more effective.
CONCLUSIONS: With a complete cure rate for low-risk GTN regardless of initial agent, our model supports provider hesitation toward first line Act-D for low risk GTN. While Act-D is more effective for first line treatment success, it is more costly, and does not decrease rate of multi-agent chemotherapy use.
METHODS: A cost effectiveness decision model was constructed with data from GOG 0174. Outcome was cost per first-line treatment success expressed in terms of incremental cost-effectiveness ratio (ICER). Front-line failures were assumed to receive cross-over single agent therapy, second line failures; multi-agent chemotherapy. GOG 0174 had no quality of life (QOL) evaluation, so equal QOL (utility 1.0) was assumed but varied in sensitivity analysis. A second exploratory model included 5-day and 8-day MTX regimens.
RESULTS: Act-D ($18,505) was more expensive compared to weekly MTX ($8950) with an ICER of $56,215 per first-line treatment success compared to weekly MTX. Small decreases in QOL dramatically increased the ICER during sensitivity analysis. Models with multi-day MTX regimens were also more cost-effective than Act-D. If effectiveness was redefined as avoidance of multi-agent chemotherapy, weekly MTX was more effective.
CONCLUSIONS: With a complete cure rate for low-risk GTN regardless of initial agent, our model supports provider hesitation toward first line Act-D for low risk GTN. While Act-D is more effective for first line treatment success, it is more costly, and does not decrease rate of multi-agent chemotherapy use.
Winter MC, Tidy JA, Hills A, et al.
Risk adapted single-agent dactinomycin or carboplatin for second-line treatment of methotrexate resistant low-risk gestational trophoblastic neoplasia.
Gynecol Oncol. 2016; 143(3):565-570 [PubMed] Related Publications
Risk adapted single-agent dactinomycin or carboplatin for second-line treatment of methotrexate resistant low-risk gestational trophoblastic neoplasia.
Gynecol Oncol. 2016; 143(3):565-570 [PubMed] Related Publications
OBJECTIVE: To evaluate the outcome of patients treated with second-line chemotherapy for methotrexate-resistant low-risk GTN at the Sheffield Centre, UK between 2001 and 2015, including the novel use of single-agent carboplatin as a strategy to reduce exposure to combination chemotherapy.
METHODS: 392 low-risk GTN patients were treated with first-line methotrexate. The selection of chemotherapy regimen following methotrexate-resistance depended on the volume of residual disease as indicated by the serum hCG value at the time, with patients switching to either single-agent dactinomycin at an hCG level<150IU/L from 2001-2010 and <300IU/L since 2010, or to combination treatment with etoposide/dactinomycin (EA) above these thresholds. In order to reduce exposure to more toxic combination chemotherapy regimens, our treatment policy was revised in 2011, with the recommendation of single-agent carboplatin as an alternative to EA at hCG levels >300IU/L.
RESULTS: 136 (35%) of 392 received second-line chemotherapy following methotrexate-resistance. 59 patients received single-agent dactinomycin with 53 (90%) patients achieving complete hCG response, 3 patients requiring combination chemotherapy or surgery, and 3 patients subsequently spontaneously resolving. 56 patients received EA chemotherapy with hCG complete response in 50 (89%) patients, and the remaining 6 patients were cured with further multi-agent chemotherapy or surgery. With carboplatin, 17/21 (81%) achieved an overall complete hCG response rate, with 4 patients requiring third-line EA. Carboplatin was well tolerated with no significant alopecia; myelosuppression was the most significant toxicity. Overall survival for all patients was 100%.
CONCLUSION: These data show the continued excellent outcomes for methotrexate-resistant low-risk patients treated with single-agent dactinomycin or EA. Our experience with carboplatin is promising and provides an alternative regimen for methotrexate-resistant low-risk disease that avoids alopecia and in-patient treatment.
METHODS: 392 low-risk GTN patients were treated with first-line methotrexate. The selection of chemotherapy regimen following methotrexate-resistance depended on the volume of residual disease as indicated by the serum hCG value at the time, with patients switching to either single-agent dactinomycin at an hCG level<150IU/L from 2001-2010 and <300IU/L since 2010, or to combination treatment with etoposide/dactinomycin (EA) above these thresholds. In order to reduce exposure to more toxic combination chemotherapy regimens, our treatment policy was revised in 2011, with the recommendation of single-agent carboplatin as an alternative to EA at hCG levels >300IU/L.
RESULTS: 136 (35%) of 392 received second-line chemotherapy following methotrexate-resistance. 59 patients received single-agent dactinomycin with 53 (90%) patients achieving complete hCG response, 3 patients requiring combination chemotherapy or surgery, and 3 patients subsequently spontaneously resolving. 56 patients received EA chemotherapy with hCG complete response in 50 (89%) patients, and the remaining 6 patients were cured with further multi-agent chemotherapy or surgery. With carboplatin, 17/21 (81%) achieved an overall complete hCG response rate, with 4 patients requiring third-line EA. Carboplatin was well tolerated with no significant alopecia; myelosuppression was the most significant toxicity. Overall survival for all patients was 100%.
CONCLUSION: These data show the continued excellent outcomes for methotrexate-resistant low-risk patients treated with single-agent dactinomycin or EA. Our experience with carboplatin is promising and provides an alternative regimen for methotrexate-resistant low-risk disease that avoids alopecia and in-patient treatment.
Liu XF, Xiang L, Zhou Q, et al.
Actinomycin D enhances killing of cancer cells by immunotoxin RG7787 through activation of the extrinsic pathway of apoptosis.
Proc Natl Acad Sci U S A. 2016; 113(38):10666-71 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Actinomycin D enhances killing of cancer cells by immunotoxin RG7787 through activation of the extrinsic pathway of apoptosis.
Proc Natl Acad Sci U S A. 2016; 113(38):10666-71 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
RG7787 is a mesothelin-targeted immunotoxin designed to have low-immunogenicity, high-cytotoxic activity and fewer side effects. RG7787 kills many types of mesothelin-expressing cancer cells lines and causes tumor regressions in mice. Safety and immunogenicity of RG7787 is now being assessed in a phase I trial. To enhance the antitumor activity of RG7787, we screened for clinically used drugs that can synergize with RG7787. Actinomycin D is a potent transcription inhibitor that is used for treating several cancers. We report here that actinomycin D and RG7787 act synergistically to kill many mesothelin-positive cancer cell lines and produce major regressions of pancreatic and stomach cancer xenografts. Analyses of RNA expression show that RG7787 or actinomycin D alone and together increase levels of TNF/TNFR family members and NF-κB-regulated genes. Western blots revealed the combination changed apoptotic protein levels and enhanced cleavage of Caspases and PARP.
Tzaridis T, Milde T, Pajtler KW, et al.
Low-dose Actinomycin-D treatment re-establishes the tumoursuppressive function of P53 in RELA-positive ependymoma.
Oncotarget. 2016; 7(38):61860-61873 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Low-dose Actinomycin-D treatment re-establishes the tumoursuppressive function of P53 in RELA-positive ependymoma.
Oncotarget. 2016; 7(38):61860-61873 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Ependymomas in children can arise throughout all compartments of the central nervous system (CNS). Highly malignant paediatric ependymoma subtypes are Group A tumours of the posterior fossa (PF-EPN-A) and RELA-fusion positive (ST-EPN-RELA) tumours in the supratentorial compartment. It was repeatedly reported in smaller series that accumulation of p53 is frequently observed in ependymomas and that immunohistochemical staining correlates with poor clinical outcome, while TP53 mutations are rare. Our TP53 mutation analysis of 130 primary ependymomas identified a mutation rate of only 3%. Immunohistochemical analysis of 398 ependymomas confirmed previous results correlating the accumulation of p53 with inferior outcome. Among the p53-positive ependymomas, the vast majority exhibited a RELA fusion leading to the hypothesis that p53 inactivation might be linked to RELA positivity.In order to assess the potential of p53 reactivation through MDM2 inhibition in ependymoma, we evaluated the effects of Actinomycin-D and Nutlin-3 treatment in two preclinical ependymoma models representing the high-risk subtypes PF-EPN-A and ST-EPN-RELA. The IC-50 of the agent as determined by metabolic activity assays was in the lower nano-molar range (0.2-0.7 nM). Transcriptome analyses of high-dose (100 nM), low-dose (5 nM) and non-treated cells revealed re-expression of p53 dependent genes including p53 upregulated modulator of apoptosis (PUMA) after low-dose treatment. At the protein level, we validated the Actinomycin-D induced upregulation of PUMA, and of p53 interaction partners MDM2 and p21. Proapoptotic effects of low-dose application of the agent were confirmed by flow cytometry. Thus, Actinomycin-D could constitute a promising therapeutic option for ST-EPN-RELA ependymoma patients, whose tumours frequently exhibit p53 inactivation.
Lertkhachonsuk R, Wairachpanich V
Treatment Outcomes of Gestational Trophoblastic Neoplasia in King Chulalongkorn Memorial Hospital over Two Decades.
J Reprod Med. 2016 May-Jun; 61(5-6):238-42 [PubMed] Related Publications
Treatment Outcomes of Gestational Trophoblastic Neoplasia in King Chulalongkorn Memorial Hospital over Two Decades.
J Reprod Med. 2016 May-Jun; 61(5-6):238-42 [PubMed] Related Publications
OBJECTIVE: To evaluate changes in treatment outcomes and epidemiologic profiles of gestational trophoblastic neoplasia (GTN) patients over a 20-year period.
STUDY DESIGN: This retrospective study recruited all GTN patients who were treated at King Chulalongkorn Memorial Hospital during the period January 1994-December 2013. Clinical data were collected. Statistical analyses were performed, with p values < 0.05 considered statistically significant.
RESULTS: There were 183 GTN cases during the study period, resulting in an incidence of 1.03 cases per 1,000 deliveries. Fifty-five cases (30.1%) were diagnosed as GTN following nonmolar pregnancy, and 128 cases were identified as postmolar GTN. A total of 113 cases were diagnosed as stage I, 12 as stage II, 40 as stage III, and 17 as stage IV; 125 cases (68.3%) were clas- sified as low risk, and 57 cases (31.1%) as high risk. Actinomycin D was the most frequently used first-line single-agent chemotherapy (98 cases), and VAC regimen was the most frequently used combination chemotherapy (24 cases). EMACO regimen was the most frequently used second-line chemotherapy (11 cases). The median number of chemotherapy courses was 4.5 courses in the first decade and 6 courses in the second decade of our study (p = 0.005). Median duration of treatment was 72 days (range, 7-491 days). Overall remission rate was 82.6%, with rates of 76% in the first decade and 90.8% in the second decade of the study (p=0.03).
CONCLUSION: Incidence of high-risk GTN increased over the course of the study period at our national referral hospital. Improvement in patient outcomes was observed, being directly associated with improved targeted chemotherapy regimens.
STUDY DESIGN: This retrospective study recruited all GTN patients who were treated at King Chulalongkorn Memorial Hospital during the period January 1994-December 2013. Clinical data were collected. Statistical analyses were performed, with p values < 0.05 considered statistically significant.
RESULTS: There were 183 GTN cases during the study period, resulting in an incidence of 1.03 cases per 1,000 deliveries. Fifty-five cases (30.1%) were diagnosed as GTN following nonmolar pregnancy, and 128 cases were identified as postmolar GTN. A total of 113 cases were diagnosed as stage I, 12 as stage II, 40 as stage III, and 17 as stage IV; 125 cases (68.3%) were clas- sified as low risk, and 57 cases (31.1%) as high risk. Actinomycin D was the most frequently used first-line single-agent chemotherapy (98 cases), and VAC regimen was the most frequently used combination chemotherapy (24 cases). EMACO regimen was the most frequently used second-line chemotherapy (11 cases). The median number of chemotherapy courses was 4.5 courses in the first decade and 6 courses in the second decade of our study (p = 0.005). Median duration of treatment was 72 days (range, 7-491 days). Overall remission rate was 82.6%, with rates of 76% in the first decade and 90.8% in the second decade of the study (p=0.03).
CONCLUSION: Incidence of high-risk GTN increased over the course of the study period at our national referral hospital. Improvement in patient outcomes was observed, being directly associated with improved targeted chemotherapy regimens.
Lertkhachonsuk AA, Hanvoravongchai P
Comparison of Cost-Effectiveness Between Actinomycin D Versus Methotrexate-Folinic Acid in the Treatment of Low-Risk Gestational Trophoblastic Neoplasia.
J Reprod Med. 2016 May-Jun; 61(5-6):230-4 [PubMed] Related Publications
Comparison of Cost-Effectiveness Between Actinomycin D Versus Methotrexate-Folinic Acid in the Treatment of Low-Risk Gestational Trophoblastic Neoplasia.
J Reprod Med. 2016 May-Jun; 61(5-6):230-4 [PubMed] Related Publications
OBJECTIVE: To compare the cost-effectiveness between actinomycin D (Act-D) and methotrexate-folinic acid (MTX-FA) in the treatment of low-risk gestational trophoblastic neoplasia (GTN) in the Thai population.
STUDY DESIGN: A comparative cost-effectiveness analysis was performed from a societal perspective. A decision tree model was developed comparing 2 alternative treatment options: initial 5-day Act-D and 8-day MTX-FA. Treatment would be switched to another regimen in case of resistance. The outcome of interest is number of days to remission. Clinical data was obtained from our previous study in which Act-D demonstrated 100% remission rates as compared to 73.6% for MTX-FA. Cost of treatment data, which includes chemotherapeutics, accessory medications, laboratory tests, and hospital fees, was obtained from a university hospital. Patient-related travel cost and opportunity cost due to absence from work were also included. All costs were calculated to 2015 base year.
RESULT: Costs per treatment cycle were $308.01 and $227.20 US dollars (USD) for 5-day Act-D and 8-day MTX-FA, respectively. Expected time toward treatment completion for Act-D was 12.6 days shorter than for MTX-FA. Expected costs toward remission for initial treatment with Act-D and MTX-FA were $1,078.04 and $1,064.56 USD, respectively, i.e., an incremental cost effectiveness ratio (ICER) of $1.07 USD/day of earlier treatment completion. After sensitivity analysis, remission rate of lower than 72% would make initial treatment with MTX-FA more expensive than with Act-D.
CONCLUSION: Treatment costs of low-risk GTN are almost equal between the 2 treatment options with different time to remission. Initial treatment with MTX-FA is slightly less expensive, but there is longer time to remission. The ICER of initial treatment with Act-D over MTX-FA is $1.07 USD/day of earlier treatment completion.
STUDY DESIGN: A comparative cost-effectiveness analysis was performed from a societal perspective. A decision tree model was developed comparing 2 alternative treatment options: initial 5-day Act-D and 8-day MTX-FA. Treatment would be switched to another regimen in case of resistance. The outcome of interest is number of days to remission. Clinical data was obtained from our previous study in which Act-D demonstrated 100% remission rates as compared to 73.6% for MTX-FA. Cost of treatment data, which includes chemotherapeutics, accessory medications, laboratory tests, and hospital fees, was obtained from a university hospital. Patient-related travel cost and opportunity cost due to absence from work were also included. All costs were calculated to 2015 base year.
RESULT: Costs per treatment cycle were $308.01 and $227.20 US dollars (USD) for 5-day Act-D and 8-day MTX-FA, respectively. Expected time toward treatment completion for Act-D was 12.6 days shorter than for MTX-FA. Expected costs toward remission for initial treatment with Act-D and MTX-FA were $1,078.04 and $1,064.56 USD, respectively, i.e., an incremental cost effectiveness ratio (ICER) of $1.07 USD/day of earlier treatment completion. After sensitivity analysis, remission rate of lower than 72% would make initial treatment with MTX-FA more expensive than with Act-D.
CONCLUSION: Treatment costs of low-risk GTN are almost equal between the 2 treatment options with different time to remission. Initial treatment with MTX-FA is slightly less expensive, but there is longer time to remission. The ICER of initial treatment with Act-D over MTX-FA is $1.07 USD/day of earlier treatment completion.
Prindaville B, Horii KA, Canty KM
Radiation Recall Dermatitis Secondary to Dactinomycin.
Pediatr Dermatol. 2016; 33(5):e278-9 [PubMed] Related Publications
Radiation Recall Dermatitis Secondary to Dactinomycin.
Pediatr Dermatol. 2016; 33(5):e278-9 [PubMed] Related Publications
Radiation recall dermatitis (RRD) is an uncommon reaction typically triggered by the use of chemotherapeutic agents in the months after treatment with radiation therapy. It usually presents as dermatitis in the irradiated field with prominent intertriginous involvement, and because internal involvement occurs in up to one-third of cases, early recognition is important. RRD has rarely been reported in the pediatric literature. We report the case of a 15-month-old boy with RRD to dactinomycin.
Lawrie TA, Alazzam M, Tidy J, et al.
First-line chemotherapy in low-risk gestational trophoblastic neoplasia.
Cochrane Database Syst Rev. 2016; (6):CD007102 [PubMed] Related Publications
First-line chemotherapy in low-risk gestational trophoblastic neoplasia.
Cochrane Database Syst Rev. 2016; (6):CD007102 [PubMed] Related Publications
BACKGROUND: This is the second update of a Cochrane review that was first published in 2009, Issue 1, . Gestational trophoblastic neoplasia (GTN) is a rare but curable disease arising in the fetal chorion during pregnancy. Most women with low-risk GTN will be cured by evacuation of the uterus with or without single-agent chemotherapy. However, chemotherapy regimens vary between treatment centres worldwide and the comparable benefits and risks of these different regimens are unclear.
OBJECTIVES: To determine the efficacy and safety of first-line chemotherapy in the treatment of low-risk GTN.
SEARCH METHODS: We electronically searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and Embase in September 2008, February 2012, and January 2016. In addition, we searched online trial registers for protocols and ongoing trials.
SELECTION CRITERIA: For the original review, we included randomised controlled trials (RCTs), quasi-RCTs and non-RCTs that compared first-line chemotherapy for the treatment of low-risk GTN. For this updated versions of the review, we included only RCTs.
DATA COLLECTION AND ANALYSIS: Two review authors independently assessed studies for inclusion and extracted data to a pre-designed data extraction form. Meta-analysis was performed using the random-effects model.
MAIN RESULTS: We included seven RCTs (667 women) in this updated review. Most studies were at a low or moderate risk of bias and all compared methotrexate with actinomycin D. Three studies compared weekly intramuscular (IM) methotrexate with bi-weekly pulsed intravenous (IV) actinomycin D (393 women), one study compared five-day IM methotrexate with bi-weekly pulsed IV actinomycin D (75 women), one study compared eight-day IM methotrexate-folinic acid (MTX-FA) with five-day IV actinomycin D (49 women), and one study compared eight-day IM MTX-FA with bi-weekly pulsed IV actinomycin D. One study contributed no data. Moderate-certainty evidence indicates that actinomycin D is probably more likely to lead to primary cure than methotrexate (risk ratio (RR) 0.65, 95% confidence interval (CI) 0.57 to 0.75; six trials, 577 participants; I(2) = 26%), and first-line methotrexate treatment is probably more likely to fail than actinomycin D treatment (RR 3.55, 95% CI 1.81 to 6.95; six trials, 577 participants; I(2) = 61%; moderate-certainty evidence) Low-certainty evidence suggests that there may be little or no difference between methotrexate and actinomycin D treatment with respect to nausea (four studies, 466 women; RR 0.61, 95% CI 0.29 to 1.26) or any of the other individual side-effects reported, although data for all of these outcomes were insufficient and too inconsistent to be conclusive. Low-certainty evidence suggests that there may be little or no difference in the risk of severe adverse events (SAEs) between the groups overall (five studies, 515 women; RR 0.35, 95% CI 0.08 to 1.66; I² = 60%); however, the direction of effect favours methotrexate and more evidence is needed. Furthermore, evidence from subgroup analyses suggests that actinomycin D may be associated with a greater risk of SAEs than methotrexate (low-certainty evidence). We found no evidence on the effect of these treatments on future fertility.
AUTHORS' CONCLUSIONS: Actinomycin D is probably more likely to achieve a primary cure in women with low-risk GTN, and less likely to result in treatment failure, than a methotrexate regimen. There may be little or no difference between the pulsed actinomycin D regimen and the methotrexate regimen with regard to side-effects. However, actinomycin D may be associated with a greater risk of severe adverse events (SAEs) than a methotrexate regimen. Higher-certainty evidence is still needed on treating low-risk GTN and the four ongoing trials are likely to make a significant contribution to this field. Given the variety of treatment regimens, findings from these trials could facilitate a network meta-analysis in the next version of this review to help women and clinicians determine the best treatment options for low-risk GTN.
OBJECTIVES: To determine the efficacy and safety of first-line chemotherapy in the treatment of low-risk GTN.
SEARCH METHODS: We electronically searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and Embase in September 2008, February 2012, and January 2016. In addition, we searched online trial registers for protocols and ongoing trials.
SELECTION CRITERIA: For the original review, we included randomised controlled trials (RCTs), quasi-RCTs and non-RCTs that compared first-line chemotherapy for the treatment of low-risk GTN. For this updated versions of the review, we included only RCTs.
DATA COLLECTION AND ANALYSIS: Two review authors independently assessed studies for inclusion and extracted data to a pre-designed data extraction form. Meta-analysis was performed using the random-effects model.
MAIN RESULTS: We included seven RCTs (667 women) in this updated review. Most studies were at a low or moderate risk of bias and all compared methotrexate with actinomycin D. Three studies compared weekly intramuscular (IM) methotrexate with bi-weekly pulsed intravenous (IV) actinomycin D (393 women), one study compared five-day IM methotrexate with bi-weekly pulsed IV actinomycin D (75 women), one study compared eight-day IM methotrexate-folinic acid (MTX-FA) with five-day IV actinomycin D (49 women), and one study compared eight-day IM MTX-FA with bi-weekly pulsed IV actinomycin D. One study contributed no data. Moderate-certainty evidence indicates that actinomycin D is probably more likely to lead to primary cure than methotrexate (risk ratio (RR) 0.65, 95% confidence interval (CI) 0.57 to 0.75; six trials, 577 participants; I(2) = 26%), and first-line methotrexate treatment is probably more likely to fail than actinomycin D treatment (RR 3.55, 95% CI 1.81 to 6.95; six trials, 577 participants; I(2) = 61%; moderate-certainty evidence) Low-certainty evidence suggests that there may be little or no difference between methotrexate and actinomycin D treatment with respect to nausea (four studies, 466 women; RR 0.61, 95% CI 0.29 to 1.26) or any of the other individual side-effects reported, although data for all of these outcomes were insufficient and too inconsistent to be conclusive. Low-certainty evidence suggests that there may be little or no difference in the risk of severe adverse events (SAEs) between the groups overall (five studies, 515 women; RR 0.35, 95% CI 0.08 to 1.66; I² = 60%); however, the direction of effect favours methotrexate and more evidence is needed. Furthermore, evidence from subgroup analyses suggests that actinomycin D may be associated with a greater risk of SAEs than methotrexate (low-certainty evidence). We found no evidence on the effect of these treatments on future fertility.
AUTHORS' CONCLUSIONS: Actinomycin D is probably more likely to achieve a primary cure in women with low-risk GTN, and less likely to result in treatment failure, than a methotrexate regimen. There may be little or no difference between the pulsed actinomycin D regimen and the methotrexate regimen with regard to side-effects. However, actinomycin D may be associated with a greater risk of severe adverse events (SAEs) than a methotrexate regimen. Higher-certainty evidence is still needed on treating low-risk GTN and the four ongoing trials are likely to make a significant contribution to this field. Given the variety of treatment regimens, findings from these trials could facilitate a network meta-analysis in the next version of this review to help women and clinicians determine the best treatment options for low-risk GTN.
Wang Y, Miao JW, Wang T, et al.
Comparison of MACT and 5Fu+ACT-D chemotherapy regimens in the treatment of low-risk gestational trophoblastic neoplasia.
J Chemother. 2016; 28(2):135-9 [PubMed] Related Publications
Comparison of MACT and 5Fu+ACT-D chemotherapy regimens in the treatment of low-risk gestational trophoblastic neoplasia.
J Chemother. 2016; 28(2):135-9 [PubMed] Related Publications
The study aimed to compare the efficacy of methotrexate (MTX) cervical injections + actinomycin-D (ACT-D)(MACT) and 5-fluorouracil (5-Fu) + actinomycin-D (5-Fu plus ACT-D) chemotherapy regimens for low-risk gestational trophoblastic neoplasia (LR-GTN). Clinical data from 66 LR-GTN patients, admitted to the Beijing Obstetrics and Gynecology Hospital from January 2010 to April 2012, were analysed retrospectively. In total, 32 patients were treated with a MACT therapeutic regimen and the remaining 34 with a 5Fu + ACT-D therapeutic regimen. Complete remission rates (CR), duration of treatment, hospital stay and toxicity effects were compared. There was no statistical difference in CR for the MACT (90.63%) or the 5-Fu plus ACT-D (100%) therapeutic regimens (p = 0.0676) or in the duration of treatment [MACT (3.50) or 5-Fu plus ACT-D (3.71; p = 0.2021)]. Moreover, the hospital stay in the 5-Fu plus ACT-D group (32.88 days) was significantly longer than for the MACT group (22.09 days; p < 0.001). Furthermore, the degree of myelosuppression, nausea and vomiting, diarrhoea, stomatitis and alopecia was more severe in the 5Fu + ACT-D group (p < 0.01). However, there was no statistical difference in the severity of liver function damage between the two groups. A shorter hospital stay, lower hospitalization cost and slightly more toxic effects were observed in LR-GTN patients treated with the MACT therapeutic regimen. We suggest that the MACT regimen should be used as first-line chemotherapy for LR-GTN.
Yarandi F, Mousavi A, Abbaslu F, et al.
Five-Day Intravascular Methotrexate Versus Biweekly Actinomycin-D in the Treatment of Low-Risk Gestational Trophoblastic Neoplasia: A Clinical Randomized Trial.
Int J Gynecol Cancer. 2016; 26(5):971-6 [PubMed] Related Publications
Five-Day Intravascular Methotrexate Versus Biweekly Actinomycin-D in the Treatment of Low-Risk Gestational Trophoblastic Neoplasia: A Clinical Randomized Trial.
Int J Gynecol Cancer. 2016; 26(5):971-6 [PubMed] Related Publications
OBJECTIVES: Methotrexate (MTX) and Actinomycin-D (Act-D) are effective drugs used in the treatment of low-risk gestational trophoblastic neoplasia (LRGTNs). The aim of the present study was to compare intravenous (IV) MTX and IV Act-D in the treatment of LRGTNs.
MATERIALS AND METHODS: Sixty-two patients with LRGTN were enrolled in a prospective randomized clinical trial between 2010 and 2013 in Moheb e Yas Hospital, Tehran University of Medical Sciences. Primary treatment regimens were IV MTX, 0.4 mg/kg daily for 5 days every 14 days (25 mg maximum daily dose), and IV Act-D, 1.25 mg/m (2 mg maximum dose) every 14 days.
RESULTS: Thirty-two and 30 patients were enrolled to MTX and Act-D groups, respectively. Complete remission after receiving first-line chemotherapy was achieved in 79% of all cases, 80% in the Act-D group and 78.1% in the MTX group.Twenty percent of the Act-D patients and 21.9% of the MTX patients showed resistance to the first-line chemotherapy, of which 16.7% and 15.6% responded completely to the second-line monotherapy, respectively. Multiple drug therapy was needed in 3.3% of the Act-D group and 6.3% of the MTX group.We did not find any correlation between treatment response and beta-human chorionic gonadotropin level, uterine mass size, lung metastasis, antecedent pregnancy, and duration from diagnosis to treatment. Adverse effects were not statistically different between the 2 groups.
CONCLUSIONS: Single-agent chemotherapy in the treatment of LRGTNs resulted in an overall complete remission rate of 79%, 80% in the Act-D group and 78.1% in MTX group, with no statistically significant difference. Whereas this study represents an important step in comparing single-agent treatments, comparison of other regimens will be required to determine the optimal single-agent therapy.
MATERIALS AND METHODS: Sixty-two patients with LRGTN were enrolled in a prospective randomized clinical trial between 2010 and 2013 in Moheb e Yas Hospital, Tehran University of Medical Sciences. Primary treatment regimens were IV MTX, 0.4 mg/kg daily for 5 days every 14 days (25 mg maximum daily dose), and IV Act-D, 1.25 mg/m (2 mg maximum dose) every 14 days.
RESULTS: Thirty-two and 30 patients were enrolled to MTX and Act-D groups, respectively. Complete remission after receiving first-line chemotherapy was achieved in 79% of all cases, 80% in the Act-D group and 78.1% in the MTX group.Twenty percent of the Act-D patients and 21.9% of the MTX patients showed resistance to the first-line chemotherapy, of which 16.7% and 15.6% responded completely to the second-line monotherapy, respectively. Multiple drug therapy was needed in 3.3% of the Act-D group and 6.3% of the MTX group.We did not find any correlation between treatment response and beta-human chorionic gonadotropin level, uterine mass size, lung metastasis, antecedent pregnancy, and duration from diagnosis to treatment. Adverse effects were not statistically different between the 2 groups.
CONCLUSIONS: Single-agent chemotherapy in the treatment of LRGTNs resulted in an overall complete remission rate of 79%, 80% in the Act-D group and 78.1% in MTX group, with no statistically significant difference. Whereas this study represents an important step in comparing single-agent treatments, comparison of other regimens will be required to determine the optimal single-agent therapy.
Mikami Y, Nagai T, Gomi Y, et al.
Methotrexate and actinomycin D chemotherapy in a patient with porphyria: a case report.
J Med Case Rep. 2016; 10:9 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
Methotrexate and actinomycin D chemotherapy in a patient with porphyria: a case report.
J Med Case Rep. 2016; 10:9 [PubMed] Article available free on PMC after 17/09/2019 Related Publications
BACKGROUND: Despite their broadly recommended use as chemotherapeutic agents, the porphyrogenicity of methotrexate and actinomycin D have not been confirmed. Accordingly, it is not known whether these agents are safe for use in patients with porphyria.
CASE PRESENTATION: In this report, we present a case of an invasive mole with lung metastasis in a 49-year-old Japanese woman who had previously been diagnosed with acute intermittent porphyria at 27 years of age but had no recent history of acute intermittent porphyria attacks. Her serum human chorionic gonadotropin level was elevated 1 month after hysterectomy, and she was referred to our center for chemotherapy. After she received 100 mg of methotrexate, drug eruptions were observed starting on day 3 and grew progressively worse. Erythema and mucosal erosion spread throughout her body, whereupon she was administered prednisolone. In addition, our patient experienced febrile neutropenia and required granulocyte colony- stimulating factor treatment. No changes in our patient's urinary coproporphyrin or uroporphyrin levels were detected during this entire episode. Methotrexate was replaced by actinomycin D (0.5 mg/body intravenously on days 1-5 every 2 weeks). After five uneventful cycles of actinomycin D, our patient achieved and maintained a normal serum human chorionic gonadotropin level for 3 years.
CONCLUSIONS: Methotrexate and actinomycin D did not induce acute porphyric attacks in this patient with acute intermittent porphyria; however, severe adverse effects were noted with methotrexate. Although further investigation is required, our data suggest that these agents are nonporphyrinogenic and can therefore be used to treat patients with comorbid porphyria.
CASE PRESENTATION: In this report, we present a case of an invasive mole with lung metastasis in a 49-year-old Japanese woman who had previously been diagnosed with acute intermittent porphyria at 27 years of age but had no recent history of acute intermittent porphyria attacks. Her serum human chorionic gonadotropin level was elevated 1 month after hysterectomy, and she was referred to our center for chemotherapy. After she received 100 mg of methotrexate, drug eruptions were observed starting on day 3 and grew progressively worse. Erythema and mucosal erosion spread throughout her body, whereupon she was administered prednisolone. In addition, our patient experienced febrile neutropenia and required granulocyte colony- stimulating factor treatment. No changes in our patient's urinary coproporphyrin or uroporphyrin levels were detected during this entire episode. Methotrexate was replaced by actinomycin D (0.5 mg/body intravenously on days 1-5 every 2 weeks). After five uneventful cycles of actinomycin D, our patient achieved and maintained a normal serum human chorionic gonadotropin level for 3 years.
CONCLUSIONS: Methotrexate and actinomycin D did not induce acute porphyric attacks in this patient with acute intermittent porphyria; however, severe adverse effects were noted with methotrexate. Although further investigation is required, our data suggest that these agents are nonporphyrinogenic and can therefore be used to treat patients with comorbid porphyria.



 Liver Cancer
Liver Cancer